Introduction
The spinothalamic tract (STT) is a sensory tract that carries nociceptive, temperature, crude touch, and pressure from our skin to the somatosensory area of the thalamus. It is responsible for our quick withdraw reaction to a painful stimulus such as touching the stove burner. The spinothalamic tract is composed of two adjacent pathways: anterior and lateral. The anterior spinothalamic tract carries sensory input about crude touch. The lateral spinothalamic tract carries information about pain and temperature. These two divisions of the spinothalamic tract run next to each other indistinctly. Thus, they can be considered one pathway. The spinothalamic tract is part of the anterolateral system, which also encompasses the spinoreticulothalamic tract (SRTT) and the spinotectal tract (SpTT). Three types of sensory fibers are associated with the spinothalamic tract: type III fibers, unmyelinated c-fibers, and myelinated A-delta fibers. Peripheral receptors having associations with the spinothalamic tract pathway are nociceptors, thermal receptors, and thermal nociceptors. Nociceptors are associated with A-delta and type III fibers, which are small, lightly myelinated axons for the transmission of fast, sharp pain. Thermal receptors and thermal nociceptors are associated with A-delta and C fibers, which are small, unmyelinated axons that conduction the transmission of slow-burning pain.[1][2]
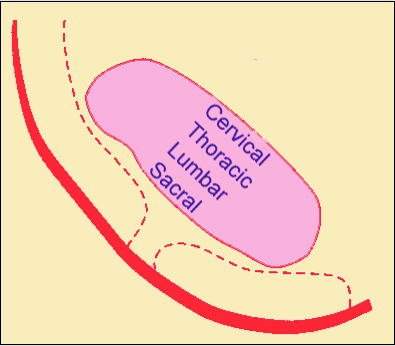
The pathway of the spinothalamic tract to the cerebral cortex starts with the dorsal root ganglions, which are composed of pseudounipolar neurons with the peripheral (distal) and central (proximal) axonal processes. These dorsal root ganglia lie adjacent to the spinal cord and represent the first-order neuron of the spinothalamic tract pathway. The axons of the central process of the first-order neurons enter the spinal cord through the lateral dorsal root entry zone to enter the Lissauer tract and synapses with second-order neurons in the substantia gelatinosa, located in the grey matter of the spinal cord. The axons of the second-order neurons cross over the spinal cord to the opposite side two segments above the level of entry via the anterior white commissure, unlike the posterior medial lemniscus pathway, which decussates in the brainstem. The decussating second-neuron fibers enter the anterolateral portion of the spinal cord and then enter the brainstem as the spinal lemniscus. The spinothalamic tract ascends in the ventrolateral aspect of the spinal white matter over the length of the spinal cord. The anterolateral system in the rostral medulla runs between the inferior olivary nucleus and the nucleus of the spinal trigeminal tract, whereas, in the pons and midbrain, the anterolateral system runs dorsolaterally to the medial lemniscus. The spinothalamic tract of the anterolateral system terminates in the ventral posterolateral nucleus (VPL) of the thalamus, the third-order neurons of this pathway. From the thalamus, axons of VPL neurons project out of the thalamus laterally and course somatotopically through the internal capsule's posterior limb of the and terminate in the postcentral gyrus primary somatosensory. In the spinal cord, the spinothalamic tract pathway has a certain somatotopic organization. The medial part of the track receives cervical input while the lateral part receives sacral input. Other pathways, such as cortical spinal tract and posterior medial lemniscus pathway, have a reversed somatotopy in comparison to the spinothalamic tract.[3][4][5][6]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The main function of the spinothalamic tract is to carry pain and temperature via the lateral part of the pathway and crude touch via the anterior part. The spinothalamic tract pathway is an imperative sensory pathway in human survival because it enables one to move away from noxious stimuli by carrying pain and temperature information from the skin to the thalamus where it is processed and transmitted to the primary sensory cortex. The primary sensory cortex communicates with the primary motor cortex, which lies close to it, to generate rapid movement in response to potentially harmful stimuli. Furthermore, the spinothalamic tract has a role in responding to pruritogens, causing us to itch. Interestingly, itching suppresses the spinothalamic tract neuron response to the histamine effect.
Clinical Significance
The spinothalamic tract is especially important when dealing with any kind of spinal cord injury. The spinothalamic tract is an anterolateral pathway. Since it is on the same side of the body, a lesion on this side of the body will cause a deficit of anything controlled below that point. Several spinal cord syndromes have spinothalamic tract involvement. Spinothalamic tract deficit leads to loss of pain and temperature sensations on one side of the body at about two levels below the lesion but on the contralateral side. An example of spinal cord syndrome with such findings is Brown-Sequard syndrome, also known as a hemicord syndrome, which compromises multiple tracts of the spinal cord, including the spinothalamic tract. However, bilateral loss of pain and temperature in a dermatomal fashion can be present in syringomyelia where the anterior white commissure becomes obliterated due to cavitation in the central spinal cord. Similar clinical presentations to syringomyelia also present in acute central cervical cord syndrome.[7][8][9]
In addition to trauma and cavitation, the spinothalamic tract can be compromised due to vascular issues as well. One example is anterior spinal artery syndrome, which is caused by infarction of the anterior spinal artery territory. Patients with anterior spinal artery syndrome present with pain and temperature loss bilaterally below the level of the lesion. However, vibratory and proprioceptive senses are preserved due to posterior column sparing. Lateral medullary syndrome caused by occlusion of posterior inferior cerebellar artery affects the spinothalamic tract as STT runs in the lateral aspect of the medulla, resulting in loss of pain and temperature sensations over the entire contralateral side of the body as well as on the ipsilateral face due to the spinal trigeminal tract involvement. Similarly, lateral pontine syndrome caused by the anterior inferior cerebellar artery can impact the spinothalamic tract giving a clinical picture that resembles that of lateral medullary syndrome. In lateral medullary and pontine syndrome, however, cranial nerve deficits and cerebellar findings coexist with STT deficit findings as well as Horner syndrome.
A lesion localized to a ventral posterolateral in the thalamus will lead to an initial loss of all sensations from the contralateral side of the body, including pain. Over time, the patient may experience pain in all, or part, of the contralateral side of the body; this is referred to as thalamic pain syndrome (Déjérine-Roussy syndrome). This phenomenon of sensing the pain on the opposite side of the body can be detrimental to both the patient and practitioner. If the lesion is not obvious, the sensation and location described by patients can lead physicians to think that the pain is more psychological rather than physical. Practitioners need to keep this phenomenon in mind when evaluating patients for pain management.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Navarro-Orozco D, Bollu PC. Neuroanatomy, Medial Lemniscus (Reils Band, Reils Ribbon). StatPearls. 2024 Jan:(): [PubMed PMID: 30252296]
Lemons ML. Locate the Lesion: A Project-Based Learning Case that Stimulates Comprehension and Application of Neuroanatomy. Journal of undergraduate neuroscience education : JUNE : a publication of FUN, Faculty for Undergraduate Neuroscience. 2017 Spring:15(2):C7-C10 [PubMed PMID: 28690440]
Level 3 (low-level) evidenceMense SS. [Functional neuroanatomy for pain stimuli. Reception, transmission, and processing]. Schmerz (Berlin, Germany). 2004 Jun:18(3):225-37 [PubMed PMID: 15221425]
Bohotin C, Scholsem M, Bohotin V, Franzen R, Schoenen J. Vagus nerve stimulation attenuates heat- and formalin-induced pain in rats. Neuroscience letters. 2003 Nov 13:351(2):79-82 [PubMed PMID: 14583386]
Level 3 (low-level) evidenceWillis WD, Westlund KN. Neuroanatomy of the pain system and of the pathways that modulate pain. Journal of clinical neurophysiology : official publication of the American Electroencephalographic Society. 1997 Jan:14(1):2-31 [PubMed PMID: 9013357]
Level 3 (low-level) evidenceBurstein R, Dado RJ, Cliffer KD, Giesler GJ Jr. Physiological characterization of spinohypothalamic tract neurons in the lumbar enlargement of rats. Journal of neurophysiology. 1991 Jul:66(1):261-84 [PubMed PMID: 1655994]
Level 3 (low-level) evidenceSaito H. The location and characteristics of the thermal sudomotor pathways in the human brainstem: A reappraisal. Autonomic neuroscience : basic & clinical. 2019 Mar:217():80-90. doi: 10.1016/j.autneu.2019.01.006. Epub 2019 Jan 28 [PubMed PMID: 30744906]
Kunam VK, Velayudhan V, Chaudhry ZA, Bobinski M, Smoker WRK, Reede DL. Incomplete Cord Syndromes: Clinical and Imaging Review. Radiographics : a review publication of the Radiological Society of North America, Inc. 2018 Jul-Aug:38(4):1201-1222. doi: 10.1148/rg.2018170178. Epub [PubMed PMID: 29995620]
Diaz E, Morales H. Spinal Cord Anatomy and Clinical Syndromes. Seminars in ultrasound, CT, and MR. 2016 Oct:37(5):360-71. doi: 10.1053/j.sult.2016.05.002. Epub 2016 May 6 [PubMed PMID: 27616310]