Introduction
Floppy eyelid syndrome (FES) is considered a common and under-diagnosed eyelid syndrome. FES is characterized by a loose or “floppy” eyelid that easily contorts or everts without spontaneously returning to its normal shape. Typical presenting symptoms include tearing, irritation, photosensitivity, and foreign body sensation in the eye. Signs include swelling, discharge, and papillary conjunctivitis. Despite these often-common signs and symptoms, FES remains a poorly defined eyelid disorder. First described in 1984, FES was first seen in a group of mostly men with high BMI who presented with eyelid laxity and papillary conjunctivitis.[1]
Other terms, such as “lax eyelid syndrome” (LES), have been used.[2][3] There is a distinction between these terms, as LES refers to known causes of eyelid laxity. These include “paralytic LES” (cranial nerve VII palsy), mechanical forces that disrupt the lateral canthal ligament, or involutional changes of the lateral canthal ligament or canthus unrelated to mechanical forces. When eyelid laxity presents as an isolated condition apart from other ocular surface diseases (OSD) or papillary conjunctivitis, it is termed “lax eyelid condition” (LAC).[4]
FES is a term used to describe a subset of patients within the larger classification of LES, predominantly men of middle age with high BMIs presenting with papillary conjunctivitis. Additionally, there is a strong correlation between the prevalence of patients with FES and obstructive sleep apnea (OSA).[5][6][7]
Therefore, the terms FES, LES, and LAC should not be used interchangeably. A careful history of past medical and ocular diseases, risk factors, time of presentation, and presenting signs and symptoms can aid in properly diagnosing floppy eyelid syndrome.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Different theories have been postulated regarding the etiology of floppy eyelid syndrome. Culbertson and Ostler hypothesized that the loss of tarsal elasticity combined with nocturnal lagophthalmos resulted in a spontaneous eversion of the upper eyelid overnight. Parunovic suggested that mechanical stress may cause the upregulation of elastolytic enzymes and cause elastic fiber degradation and subsequent tarsal laxity.[8]
Meanwhile, Schwartz et al. theorized that a poor interface between the loose eyelids and the epi-bulbar surface could cause injury to the eyelid and laxity. Lastly, multiple studies have suggested that elastin is the main culprit in FES. Histopathologic studies have shown that not only is there a decrease in the amount of elastin in the tarsal plate, but the elastin fibers are also abnormal in these patients. The features of abnormal elastin have been documented in human connective tissue disorders such as Marfan syndrome, Ehlers-Danlos syndrome, pseudoxanthoma elasticum, and more.[9]
Epidemiology
The prevalence of floppy eyelid syndrome in the general population ranges from 3.5 to 15.8%. However, diagnostic and definitional challenges likely underestimate the true prevalence of FES. Trends in the demographic groups seem to indicate a greater prevalence of FES in men of middle age with high BMIs. However, recent data suggests that the prevalence in women could be comparable to men's.[10] FES is not a syndrome exclusive to adult patients, as studies have shown that FES can occur as early as childhood.[11]
Pathophysiology
The pathophysiology of floppy eyelid syndrome is poorly understood. There are speculations about the underlying mechanisms based on associations from previous studies. These theories remain inconclusive as further studies investigating these mechanisms are warranted. Current evidence suggests genetic inheritance predispositions and anomalies, changes in the elastin structure of the tarsal plates and tendon ligaments, and overexpression of matrix metalloproteinases (MMPs) and proteases are the main factors in the pathogenesis of FES.[1][12][13]
Some studies have suggested that there may be an associated X-linked pattern of inheritance that could explain the high occurrence of FES in males. Other genetic anomalies in the COL5A1 and COLA52 type V collagen genes seen in Ehlers-Danlos may be associated with FES, as early studies demonstrated comorbidity between connective tissue disorders and FES.[9]
Most notably, there is a strong association between FES and OSA that researchers have tried to explain.[7][14] The most likely explanation lies in the premise that patients with OSA experience moments of hypoxia leading to increased oxidative stress and production of reactive oxygen species, leading to increased production of MMPs. Several studies have shown increased levels of metalloproteinases in patients with FES. Metalloproteinases are responsible for the enzymatic breakdown of elastin, leading to loss of tarsal elasticity and laxity of the lateral canthal tendon tissues.
Histopathology
Floppy eyelid syndrome is characterized by decreased levels of elastin fibers in the tarsus on light microscopy and immunohistochemical staining. Collagen types I and III are comparable to patients without FES.[15] The common presenting sign on inspection of the conjunctiva is prominent papillary changes of the conjunctival epithelium accompanied by chronic non-granulomatous inflammation underlying the lamina propria. The loss of (exposed) goblet cells and the loss of meibomian glands in the tarsal plate is also a common finding.[16]
Inflammation of the adjacent lamina propria is typically confined to this space and does not extend into the tarsus.[12] These findings are consistent with a documented history of chronic eye rubbing in FES patients.
Evaluation of elastin fibers within the tarsal collagen using Verhoeff’s modified elastin has demonstrated a prominent decrease in elastin fibers between the acini. The endomysium and perimysium of the pretarsal orbicularis muscle can also demonstrate decreased levels of elastic fibers. Despite the persistent reductions in elastin fibers, the ultrastructure of tarsal collagen remains mostly unchanged.[13]
History and Physical
Patients typically present with nonspecific symptoms of ocular irritation and discomfort. A wide range of complaints can be elicited on questioning, including tearing, redness, photosensitivity, foreign body sensation, mucoid discharge, dryness, and eyelid swelling. The patient may also notice a worsening of these symptoms in the morning.[4]
Examination reveals easy upper eyelid eversion and horizontal laxity. A great majority of patients will also demonstrate palpebral papillary conjunctivitis.[15] Other ocular findings associated with FES include punctate erosions, keratitis, corneal abrasions, keratoconus, blepharitis, dermatochalasis, and eyelid malposition. Both keratoconus and FES are associated with heavy eye rubbing.[17]
Evaluation
Patients presenting with ocular irritation and discomfort symptoms should be assessed for floppy eyelid syndrome, particularly if these are chronic and resistant to medical management. The examination of these patients is comprehensive and includes a thorough ophthalmological exam focusing on testing the eyelid laxity of the patient and screening for OSA.
Different methods have been developed to evaluate and quantify upper lid laxity in FES patients, but no gold standard exists. McNabb’s approach, commonly regarded as the most reproducible technique, is easily performed in the clinic. The examiner distracts or vertically pulls the upper eyelid by placing a thumb on its outer one-third and brings it superiorly and laterally. The maximum difference between the upper eyelid’s resting position and maximal displacement is measured. A difference ranging between 15 to 25 mm strongly suggests floppy eyelids.
Alternatively, in their upper horizontal distraction test, Iyengar and Khan quantified the distance between the anterior corneal surface and the anteriorly displaced upper eyelid to diagnose FES.[18] A displacement averaging 17.09 mm was considered significant for this disease. Liu and Stasior measured the horizontal lid distraction distance, with a distance greater than 5mm and 6mm for the upper and lower lids, respectively, suggesting FES.[19]
Once diagnosed, the FES severity can be graded. One grading system, in particular, has been used in several clinical trials. In this method, the upper eyelid is distracted up as the patient is asked to look down. The amount of visible conjunctiva during this maneuver determines the severity of FES. If no conjunctiva is visible, the patient does not have FES and is assigned Grade 0. In mild FES, or Grade 1, less than one-third of the upper conjunctival is visible. In moderate FES, or Grade 2, one-third to one-half of the conjunctiva is observed. Lastly, more than half of the tarsal conjunctiva is visible in severe FES, or Grade 3.[4]
Another commonly employed grading system is based on the amount of horizontal lid distraction from the corneal surface. This amount is measured in millimeters and converted into a grading scale of 0 to 4. If less than 6 mm, this is considered a Grade 0, 6 to 8 mm a Grade 1, 9 to 11 mm Grade 2, 12 to 15 mm a Grade 3, and greater than 15 mm a Grade 4.
The evaluation of FES should also include a full ophthalmological evaluation. Consideration must be given to related conditions such as keratoconus and dry eye. Given the high association between obstructive sleep apnea and FES, patients must be screened for OSA as part of the FES evaluation. A clinician can easily accomplish this by utilizing the Epworth Sleepiness Scale, which provides a quick way to screen FES patients. In those patients with a score greater than 10, a polysomnography test is indicated to diagnose OSA. Similarly, patients diagnosed with sleep apnea must also be evaluated for FES.
Treatment / Management
Management of floppy eyelid syndrome can be divided into medical and surgical. The patient is first treated with a conservative approach, including artificial tears, nighttime ophthalmic ointment, eyelid taping, and shielding. If there is significant ocular inflammation, anti-inflammatory agents can be considered. Patients must treat underlying OSA with a CPAP machine, as properly managed OSA can improve the FES grade and dry eye symptoms. If a patient fails conservative treatment, surgical management can be considered. Various surgical techniques are currently employed for the correction of eyelid laxity. A lateral tarsal strip procedure can shorten the eyelid length and reduce laxity.[20] (B2)
While this technique was mostly employed for the lower eyelids, it has recently become an option for upper eyelid disease.[21] Other techniques include full-thickness wedge excision, canthal tendon plication, and even a simple lateral tarsorrhaphy.[22][23][24](B3)
Differential Diagnosis
- Blepharitis
- Ectropion
- Dermatochalasis
- Giant papillary conjunctivitis
- Atopic keratoconjunctivitis
- Superior limbic keratoconjunctivitis
- Allergic conjunctivitis
- Involutional ptosis
- Contact lens complication
Prognosis
When treated, FES is a manageable condition with minimal risk of complications and reduction of symptomatic complaints for patients. Untreated FES in patients may result in sight-threatening conditions, including dry eye and other ocular surface diseases. Patients with concomitant OSA and FES have seen improvement in both OSA symptoms and symptoms and FES and other dry eye conditions. Some studies have demonstrated full resolution of FES in patients who strictly adhered to CPAP therapy.[25][26]
Not all patients may be responsive to conservative management of FES and will require corrective surgery.[15] In the case of patients who undergo lateral tarsal strip procedures, studies have shown up to 91% of patients reporting improved symptoms and up to 98% of patients achieving long-term success. Other procedures, such as full and modified full-thickness wedge excision (FTWE and MTWE, respectively) and canthal tendon plication, have reported similar success rates.[15][27] However, recent studies suggest long-term outcomes are favored for patients undergoing medial and lateral canthal plication (MC/LC) over FTWE.[28]
Complications
Untreated FES can lead to chronic irritation and inflammation of the ocular surface. Patients can present with keratitis, recurrent corneal erosions, and even vascularization and scarring of the corneal surface. In severe cases, corneal ulceration and perforation have been observed.[29]
Deterrence and Patient Education
Better outcomes are likely if patients are educated on the following:
- Avoid rubbing the eyelid, as this can exacerbate eyelid laxity.
- Adherence to treatment, including topical ointments, eyelid shields, and eyelid taping at night.
- A sleeping position that does not disturb the eyelid during the night. This most likely involves avoiding sleeping on the side or face down on the pillow.[30]
- Adherence to CPAP therapy might reverse FES in patients on CPAP for OSA.[26]
Enhancing Healthcare Team Outcomes
The interprofessional healthcare team for patients with floppy eyelid syndrome potentially includes a team of optometrists, ophthalmologists, PCPs, sleep medicine specialists, and nursing staff. Further medical education on diagnosing and early recognizing FES is essential to avoid sight-threatening conditions. Educating PCPs on the strong association between OSA and FES could facilitate a timely referral to the eye doctor if the PCP team suspects OSA or if a sleep medicine specialist diagnoses OSA.
Media
(Click Image to Enlarge)

Causes of Epiphora. The conditions that can cause epiphora include herpes zoster with keratitis (A), lacrimal mucocele (B), corneal calcific keratopathy (C), floppy eyelid syndrome (D), kissing puncta syndrome (E), and pemphigoid disease with trichiasis and obliteration of puncta (F).
Contributed by BCK Patel, MD, FRCS
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
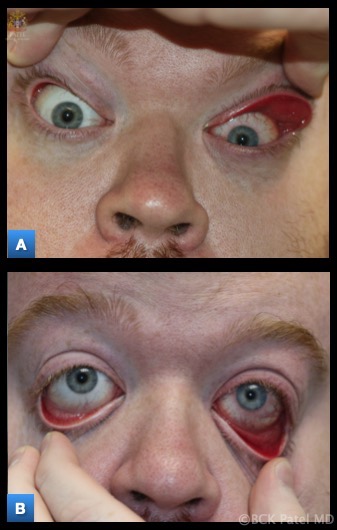
Floppy Eyelid Syndrome: Marked laxity of the upper and lower eyelids, which is usually asymmetric, with the side the patient sleeps on worse. There is easy eversion of the upper and lower eyelids with associated papillary conjunctivitis, discharge, tearing, redness, foreign body sensation, mucoid discharge, and decreased vision. Contributed by Prof. Bhupendra C. K. Patel MD, FRCS
(Click Image to Enlarge)

Floppy Eyelid Syndrome: the findings of eyelid laxity are almost always asymmetric, with the side that the patient sleeps on being worse, as illustrated here. Most patients are males with obesity (with a BMI > 30 kg/m2), and sleep apnea. Sleep apnea is present in more than 50% of patients witht the floppy eyelid syndrome. Contributed by Prof. Bhupendra C. K. Patel MD, FRCS
References
Culbertson WW, Ostler HB. The floppy eyelid syndrome. American journal of ophthalmology. 1981 Oct:92(4):568-75 [PubMed PMID: 7294118]
Level 3 (low-level) evidenceFowler AM, Dutton JJ. Floppy eyelid syndrome as a subset of lax eyelid conditions: relationships and clinical relevance (an ASOPRS thesis). Ophthalmic plastic and reconstructive surgery. 2010 May-Jun:26(3):195-204. doi: 10.1097/IOP.0b013e3181b9e37e. Epub [PubMed PMID: 20489546]
Level 2 (mid-level) evidenceSward M, Kirk C, Kumar S, Nasir N, Adams W, Bouchard C. Lax eyelid syndrome (LES), obstructive sleep apnea (OSA), and ocular surface inflammation. The ocular surface. 2018 Jul:16(3):331-336. doi: 10.1016/j.jtos.2018.04.003. Epub 2018 May 3 [PubMed PMID: 29729418]
De Gregorio A, Cerini A, Scala A, Lambiase A, Pedrotti E, Morselli S. Floppy eyelid, an under-diagnosed syndrome: a review of demographics, pathogenesis, and treatment. Therapeutic advances in ophthalmology. 2021 Jan-Dec:13():25158414211059247. doi: 10.1177/25158414211059247. Epub 2021 Dec 5 [PubMed PMID: 35187400]
Level 3 (low-level) evidenceBeis PG, Brozou CG, Gourgoulianis KI, Pastaka C, Chatzoulis DZ, Tsironi EE. The floppy eyelid syndrome: evaluating lid laxity and its correlation to sleep apnea syndrome and body mass index. ISRN ophthalmology. 2012:2012():650892. doi: 10.5402/2012/650892. Epub 2012 Jun 20 [PubMed PMID: 24558590]
Pedrotti E, Demasi CL, Bruni E, Bosello F, Di Sarro PP, Passilongo M, Fasolo A, Gennaro N, De Gregorio A, Ferrari M, Marchini G. Prevalence and risk factors of eye diseases in adult patients with obstructive sleep apnoea: results from the SLE.E.P.Y cohort study. BMJ open. 2017 Oct 22:7(10):e016142. doi: 10.1136/bmjopen-2017-016142. Epub 2017 Oct 22 [PubMed PMID: 29061607]
Bulloch G, Seth I, Alphonse S, Sathe A, Jennings M, Sultan D, Rahmeh R, McNab AA. Prevalence of Obstructive Sleep Apnea With Floppy Eyelid Syndrome: A Systematic Review and Meta-analysis. Ophthalmic plastic and reconstructive surgery. 2022 Oct 28:():. doi: 10.1097/IOP.0000000000002298. Epub 2022 Oct 28 [PubMed PMID: 36700854]
Level 1 (high-level) evidenceParunović A. Floppy eyelid syndrome. The British journal of ophthalmology. 1983 Apr:67(4):264-6 [PubMed PMID: 6830745]
Level 3 (low-level) evidenceSegev F, Héon E, Cole WG, Wenstrup RJ, Young F, Slomovic AR, Rootman DS, Whitaker-Menezes D, Chervoneva I, Birk DE. Structural abnormalities of the cornea and lid resulting from collagen V mutations. Investigative ophthalmology & visual science. 2006 Feb:47(2):565-73 [PubMed PMID: 16431952]
Level 3 (low-level) evidencePaciuc M, Mier ME. A woman with the floppy eyelid syndrome. American journal of ophthalmology. 1982 Feb:93(2):255-6 [PubMed PMID: 7065101]
Level 3 (low-level) evidenceRao LG, Bhandary SV, Devi AR, Gangadharan S. Floppy eyelid syndrome in an infant. Indian journal of ophthalmology. 2006 Sep:54(3):217-8 [PubMed PMID: 16921233]
Level 3 (low-level) evidenceNetland PA, Sugrue SP, Albert DM, Shore JW. Histopathologic features of the floppy eyelid syndrome. Involvement of tarsal elastin. Ophthalmology. 1994 Jan:101(1):174-81 [PubMed PMID: 8302552]
Schlötzer-Schrehardt U, Stojkovic M, Hofmann-Rummelt C, Cursiefen C, Kruse FE, Holbach LM. The Pathogenesis of floppy eyelid syndrome: involvement of matrix metalloproteinases in elastic fiber degradation. Ophthalmology. 2005 Apr:112(4):694-704 [PubMed PMID: 15808264]
Level 2 (mid-level) evidenceLeibovitch I, Selva D. Floppy eyelid syndrome: clinical features and the association with obstructive sleep apnea. Sleep medicine. 2006 Mar:7(2):117-22 [PubMed PMID: 16458600]
Salinas R, Puig M, Fry CL, Johnson DA, Kheirkhah A. Floppy eyelid syndrome: A comprehensive review. The ocular surface. 2020 Jan:18(1):31-39. doi: 10.1016/j.jtos.2019.10.002. Epub 2019 Oct 5 [PubMed PMID: 31593763]
Liu S, Li S, Li M, Zeng S, Chen B, Zhang L. Evaluation of the Ocular Surface and Meibomian Gland in Obstructive Sleep Apnea Hypopnea Syndrome. Frontiers in medicine. 2022:9():832954. doi: 10.3389/fmed.2022.832954. Epub 2022 Feb 9 [PubMed PMID: 35223929]
Donnenfeld ED, Perry HD, Gibralter RP, Ingraham HJ, Udell IJ. Keratoconus associated with floppy eyelid syndrome. Ophthalmology. 1991 Nov:98(11):1674-8 [PubMed PMID: 1800928]
Level 3 (low-level) evidenceIyengar SS, Khan JA. Quantifying upper eyelid laxity in symptomatic floppy eyelid syndrome by measurement of anterior eyelid distraction. Ophthalmic plastic and reconstructive surgery. 2007 May-Jun:23(3):255 [PubMed PMID: 17519685]
Level 3 (low-level) evidenceLiu D, Stasior OG. Lower-eyelid distractor. Plastic and reconstructive surgery. 1984 Jan:73(1):137-9 [PubMed PMID: 6691064]
Burkat CN, Lemke BN. Acquired lax eyelid syndrome: an unrecognized cause of the chronically irritated eye. Ophthalmic plastic and reconstructive surgery. 2005 Jan:21(1):52-8 [PubMed PMID: 15677953]
Level 2 (mid-level) evidenceViana GAP, Sant'Anna AE, Righetti F, Osaki M. Floppy eyelid syndrome. Plastic and reconstructive surgery. 2008 May:121(5):333e-334e. doi: 10.1097/PRS.0b013e31816b1147. Epub [PubMed PMID: 18453947]
Phillips ME, Fowler BT, Dryden SC, Fleming JC. Canthal V-plasty for Floppy Eyelid Surgery. Plastic and reconstructive surgery. Global open. 2019 Oct:7(10):e2464. doi: 10.1097/GOX.0000000000002464. Epub 2019 Oct 29 [PubMed PMID: 31772892]
Scholten E, Marck KW, Grond AJ. Surgical correction of floppy eyelids. British journal of plastic surgery. 1998 Apr:51(3):264-6 [PubMed PMID: 9664895]
Level 3 (low-level) evidenceDutton JJ. Surgical management of floppy eyelid syndrome. American journal of ophthalmology. 1985 May 15:99(5):557-60 [PubMed PMID: 4003492]
Level 3 (low-level) evidenceChokroverty S, Bhat S. "Droopy eyelid" syndrome in obstructive sleep apnea: reversal after CPAP treatment. Sleep medicine. 2021 May:81():285-287. doi: 10.1016/j.sleep.2021.02.042. Epub 2021 Feb 27 [PubMed PMID: 33743474]
McNab AA. Reversal of floppy eyelid syndrome with treatment of obstructive sleep apnoea. Clinical & experimental ophthalmology. 2000 Apr:28(2):125-6 [PubMed PMID: 10933776]
Level 3 (low-level) evidenceMedel R, Alonso T, Vela JI, Calatayud M, Bisbe L, García-Arumí J. Conjunctival cytology in floppy eyelid syndrome: objective assessment of the outcome of surgery. The British journal of ophthalmology. 2009 Apr:93(4):513-7. doi: 10.1136/bjo.2008.144287. Epub 2008 Dec 5 [PubMed PMID: 19060014]
Ezra DG, Beaconsfield M, Sira M, Bunce C, Shah-Desai S, Verity DH, Uddin J, Collin R. Long-term outcomes of surgical approaches to the treatment of floppy eyelid syndrome. Ophthalmology. 2010 Apr:117(4):839-46. doi: 10.1016/j.ophtha.2009.09.009. Epub 2010 Jan 25 [PubMed PMID: 20097426]
Level 2 (mid-level) evidenceDin N, Vasquez-Perez A, Ezra DG, Tuft SJ. Serious corneal complications and undiagnosed floppy eyelid syndrome; A case series and a 10-year retrospective review. Journal of current ophthalmology. 2019 Jun:31(2):225-228. doi: 10.1016/j.joco.2019.03.003. Epub 2019 Apr 8 [PubMed PMID: 31317105]
Level 2 (mid-level) evidenceTing RJE, Singh N, Ling M, Spencer SK, Khan MA, Desai A, Agar A, Francis IC. Assessment of Obstructive Sleep Apnoea and Sleeping Laterality by Evaluating Upper Eyelid Distraction: A Prospective, Comparative Polysomnographic Study. Cureus. 2020 Aug 5:12(8):e9566. doi: 10.7759/cureus.9566. Epub 2020 Aug 5 [PubMed PMID: 32905542]
Level 2 (mid-level) evidence
