Introduction
The Hippocratic Oath instructs physicians and other medical providers to first, “do no harm”. Similarly, the three ethical principles laid forth in the Belmont Report ask providers to prioritize respect for persons, beneficence, and justice in their daily practice. While is it critical for providers of medical care to uphold these tenets, frequently situations arise where it is impossible to fulfill all. Medical providers are tasked with multiple roles simultaneously - healer, patient advocate, protector of hospital staff, guardian of public health, citizen, and a humanist and spiritual being. Providers must be prepared for the situation that places these roles and priorities at odds. This article will discuss relevant definitions, delve further into the ethical principles introduced above, and prepare medical providers for how to approach these complex patient encounters with the intent of maximizing benefit for all and protecting the provider(s) involved.
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
Relevant Definitions
In any academic conversation, it is critical to ensure that all participants understand the shared lexicon. This is even more important concerning the topic of competency and capacity - an ethically and legally charged subject, that if not understood or executed properly can contribute to patient harm and legal action against medical providers.
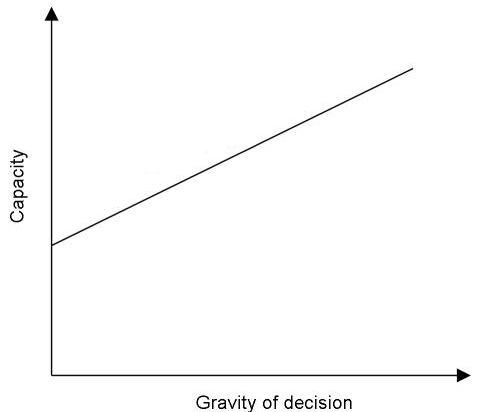
Capacity is defined as "a functional determination that an individual is or is not capable of making a medical decision within a given situation" [1]. This is relative to the baseline abilities of the patient, pertains only to the current situation, and takes into consideration the severity of the possible consequences.
Competency is defined as “the ability of an individual to participate in legal proceedings”. Legal competence is presumed - to disprove an individual's competence requires a hearing and presentation of evidence. Competence is determined by a judge [1][2][3]. This legal determination is never determined by medical providers. Because this determination is not made by providers we will not use this term further in this article.
A Tort is defined as "an act, or omission of an act, that results in injury or harm to an individual. This is a volitional act done with intent to cause harm or suffering" [4].
Informed Consent is defined as "the systematic approach to patient education and medical decision-making regarding a particular treatment or procedure" [5]. This is both an ethical and legal imperative in modern medicine and requires a discussion of the nature of the procedure, the risks and benefits, the reasonable alternatives, and an assessment of the patient's understanding of these items [5]. Refer to separate StatPearls articles on this topic.
A Medical Provider is, in the context of this article, limited to licensed physicians (MD, DO), physician assistants, and advanced degree nurse practitioners. This term is herein limited because these are the medical professionals who are legally permitted to assess and document mental capacity for medical decision-making.
Ethical Principles Involved
When graduating from medical school, all new physicians recite the Hippocratic Oath. The Oath, regarded as one of the earliest expressions of medical ethics in the Western World, instructs physicians 1) to use medical education for the benefit of all, 2) to abstain from intentional wrongdoing or harm to patients, and 3) to hold secret the information learned about patients. Over the years, these instructions have been reduced to the common aphorism of "first do no harm".
The Belmont Report of 1976 builds from this principle of “first do no harm” and gives physicians an ethical basis from which to build their clinical practice. Spurred by incidents of unethical medical practice (e.g. The Tuskegee Syphilis Study), the Belmont Report explains and extends three fundamental ethical principles that the practitioner must use as a guide to the ethical practice of medical practice [6]. These principles are:
1. Respect for Persons: The root ethical principle here counsels the practitioner to uphold and allow for patient autonomy. This includes allowing all appropriate patients the opportunity for informed consent before receiving medical treatment or undergoing procedures.
2. Beneficence: This term is the modern equivalent for Hippocrates' concept of "do no harm". In practice, the ethical issue addressed examines the risk/benefit ratio of the proposed medical treatment, while simultaneously 1) maximizing patient benefit and 2) minimizing harm or discomfort. This involves both making decisions to benefit the patient, as well as taking affirmative steps to prevent or remove harm from the patient. What is beneficial for the patient is highly personal and multi-faceted, and involves consideration of the patient's medical prognosis as well as multiple subjective factors, such as goals of care, quality of life, financial considerations, family input, etc. 3. Justice: The overarching philosophy of this principle instructs the practitioner to ensure fair end equitable distribution of medical resources regardless of demographics, insurance status, socioeconomic status, mental disability, etc. Keep in mind that "physician paternalism" (here defined as "the policy of restricting the freedom and responsibility of patients against their will, and defended by a claim that the person interfered with will be better off or protected from harm") is not in service of these ethical principles. Coercion into the course of action that the provider thinks is best neither respects patient autonomy nor upholds the principle of beneficence. Truly bringing these principles into daily practice involves taking the time to communicate your findings and recommendations to the patient, actively listening to their questions and concerns, and making a shared decision. Ultimately, this decision may not agree with what the provider thinks is best. Supporting that decision, if appropriate, is part of practicing respect for patient autonomy.
Clinical Significance
Why Is This Important To Clinical Practice?
Despite our overall goal to uphold the ethical principles described in the Belmont Report, this is not always possible. Although physicians and other practitioners indeed provide medical care for patients, practitioners have many other roles; e.g. as a protector of hospital staff, as a guardian of public health, as a citizen, and as a humanist and spiritual being in his/her own right. Some situations arise in daily clinical practice that creates conflict between these roles and complicates the ethics of the day-to-day decision-making of medical practice. For example, imagine that you have diagnosed a patient with active tuberculosis, but he refuses treatment. In your role as a practitioner, you engage in a conversation with him about his declination of treatment and decide that the patient possesses the capacity to decline. You are therefore ethically bound to respect this patient's autonomy to make his own medical decisions but are also bound to protect and serve the health of the overall community concerning the risk of infectious contagion. How do you weigh these competing interests? What legal repercussions may you face if you prioritize one over the other?
Consider another case. You are caring for a young man brought in by police after he was found wandering on a road with no shoes. In the ED, he is agitated and combative with staff. You decide on clinical grounds that he will require a full workup including IV placement, labs, and imaging but he is adamantly screaming that he "wants to leave" and tries to strike any provider who comes near him. Can you place an IV against his will? Can you restrain or sedate him against his will? Again, what steps do you need to take to ensure you are legally protected?
Recall that a tort is an act, or omission of an act, that results in injury or harm to an individual. Specifically concerning the illustration above, the common law tort of "assault" involves "an act or omission causing an individual to experience reasonable fear or apprehension of an immediate battery." Here battery is legally defined as "harmful or offensive contact". Does the placement of the IV constitute a battery? Likewise, the tort of "false imprisonment" involves an act/omission that results in an individual "being confined or bound in a defined space with no possibility of escape." Does the act of restraining and sedating the patient constitute false imprisonment?
The question then reduces to a query of how medical providers may protect both their patients and themselves amidst this swarm of conflicting ethical principles, disagreeing roles, and risk for legal action. The answer in part lies in a complete and thorough assessment of a patient’s capacity for medical decision-making. This assessment is the foundation on which medical providers may gain legal protection when acting against a patient's immediate wishes in the service of the well-being of the patient, the staff, or the overall public.
In the context of the case above, until a capacity assessment is completed, placing an IV against this patient's will constitutes the tort of battery. Placing him on a hold constitutes the tort of false imprisonment. Chemically or physically restraining him equates to the tort of battery and false imprisonment [7]. Therefore, an assessment of decision-making capacity MUST be performed before acting without a patient's consent.
When To Access Capacity?
Evaluation of decision-making capacity should be involved in every patient interaction. The depth of this evaluation may vary on a case-by-case basis, depending on 1) the acuity of the illness, 2) the patient's age and functional status, 3) the patient's or family's goals for care, 4) the clinical environment or 5) any number of other factors. Remember that an assessment of capacity is valid only within the time, place, and situation in which the evaluation took place [8]. It is therefore a snapshot in time, and cannot be applied to any other time or situation. For example, a patient with a history of dementia does not automatically lack capacity. At the time of the capacity assessment, they may be lucid and able to participate meaningfully in the discussion, thus potentially indicating a capacity for decision-making in the present moment. However, two weeks in the future, the same patient may be disoriented to such a degree that the individual is subsequently found by examination to lack capacity. Similarly, an intoxicated patient may be temporarily impaired until the individual is sober, and may, upon achieving clinical sobriety, be able to make reasonable and sound medical decisions.
Some specific triggers to further investigate a patient’s decision-making capacity include [2][9][10][9]:
- Inability to voice a decision
- Blanket acceptance or refusal of care
- Absence of questions about the treatment being offered or provided
- Excessive or inconsistent reasons for refusing care
- New inability to perform activities of daily living
- Hyperactivity, disruptive behavior, or agitation
- Labile emotions or effect
- Hallucinations
- Clinical intoxication
The salient point for the reader is that some manner of assessment of a patient's medical-decision making skills should be part of every patient encounter, and should be scaled to the degree of illness severity and mental impairment. The initial capacity evaluation need not be more than a standard patient examination, e.g. a general appearance, level of consciousness, orientation to self/time/situation, observation of behavior and affect, and an effort to ascertain the patient's ability to understand and comprehend medical information. If there are concerning findings on this initial impression, a more thorough examination should be performed.
How To Access Capacity?
Recall that as defined above, capacity is a functional determination that an individual is or is not capable of making a medical decision within a given situation. This is relative to the baseline abilities of the patient, pertains only to the current situation, and takes into consideration the severity of the possible consequences [11]. This is an exam that providers in psychiatry, psychology, and primary care may be quite familiar with and comfortable performing. Providers in other fields may have more limited experience with this assessment. Ideally, it should be practiced regularly, so that it can be executed quickly and properly when necessary. This process has been described as a "complex calculation involving a patient's mental status, cognitive ability, culture, education, health literacy, and ability to articulate the issues of concern” [12].
Because of legal issues regarding licensure, this assessment is not an appropriate job for nurses, nursing assistants, technicians, or other support staff. Often, psychiatrists are felt to be the experts of this assessment, and they can be involved in particularly complex situations that require expert opinion. However, these providers are not always readily available for an instant consultation. Therefore, and particularly in the emergency department setting, a rapid assessment of capacity may be immediately required due to the high acuity of physical or mental illness. Thus, any licensed physician, physician assistant, or nurse practitioner can and should be able to assess and determine capacity.
The foundation of this assessment is the mental status exam (MSE); one cannot determine capacity without this.
A thorough mental status exam should include evaluation of the following [13]:
1. Appearance and general behavior: Body habitus, grooming and hygiene, eye contact, distinguishing features, overall behavior
2. Motor activity: Posture, movements, facial expressions, psychomotor agitation or retardation
3. Speech: Quantity, rate, volume, fluency, and the ability for other’s to understand the language used
4. Mood: Defined as the individual's subjective experience of the patient's inner emotional state. Consider asking, "how would you describe your mood?"
5. Affect: Your objective observation of the behaviors suggesting the patient's inner emotional state
6. Thought process: Flow and form of thought
7. Thought content: Content of the patient’s thoughts, i.e. obsessions, delusions, phobias, suicidal or homicidal ideation
8. Perceptual disturbances: Hallucinations
9. Sensorium: Level of consciousness and stability of consciousness
10. Cognition: Attentiveness, ability to concentrate, short-term memory. This may be permanently or temporarily impaired by a medical condition such as dementia, delirium, intoxication, etc [14].
11. Insight: The patient's understanding of his/her illness and required treatments.
12. Judgment: Patient's ability to recognize and comprehend the consequences of actions and decisions
A complete understanding of an individual's mental status or at least as complete as the patient's clinical condition will allow, is imperative for an accurate determination of their capacity to make medical decisions. This exam provides the foundation on which to build an argument for or against a patient’s capacity.
In the medical environment, a patient proves capacity by demonstrating the following [2]:
- Understanding of information relevant to the decision in question
- Ability to weigh risks and benefits, and to assess alternative options
- Communicate clearly with medical providers about the decision in question, and verbalize the ultimate decision
- Consistency of logic and decision-making throughout the encounter
Consider again the case from above - the young man brought in agitated and combative after being found wandering in a road without shoes. Documentation of his mental status exam one might observe and document the following:
1. Appearance and general behavior: Disheveled appearing, malodorous, feet and lower legs are covered in dirt, appears agitated
2. Motor activity: Writhing in bed and trying to pull off pulse ox and monitor leads
3. Speech: Slurred and difficult to understand, yelling loudly, speech is pressured and rapid
4. Mood: “Let me out of here, I need to leave”
5. Affect: Expansive, hostile
6. Thought process: Tangential, jumps from topic-to-topic without linear process
7. Thought content: Obsessive about wanting to leave, appears to have an intense fear about someone "coming after him"
8. Perceptual disturbances: Appears internally stimulated
9. Sensorium: Heightened level of alertness, hyper-vigilant
10. Cognition: Poor attention, unable to participate in a linear conversation
11. Insight: Extremely poor - unable to relay understanding of his abnormal mental status
12. Judgment: Extremely poor - unable to communicate an understanding of the consequences of his desire to leave the ER before examination and testing
Based on this mental status exam, it would be reasonable and appropriate to determine that this patient does not have the capacity to make sound or logical medical decisions. Of the four criteria for capacity listed above, he has demonstrated none. A patient who lacks decision-making capacity can neither refuse nor consent to treatment [7]. Once this absence of capacity has been determined and documented, the medical provider is legally permitted to perform sedation, restraint, venipuncture, and other testing or treatment as determined to be appropriate.
Enhancing Healthcare Team Outcomes
Regarding documentation; a safe rule to follow is the ubiquitous adage, “if it’s not documented, it didn’t happen”. These situations are high-risk from a medico-legal perspective and providers should document accordingly. Emergency department providers have been shown to have suboptimal documentation habits, particularly in high-risk scenarios [15]. Taking several minutes immediately after performing the mental status exam and capacity determination to thoroughly document the exam and capacity determination is essential and should be prioritized. Remember that unless and until a complete capacity assessment has been performed and documented, performing procedures and treatments without patient consent is both unethical and illegal.
Media
(Click Image to Enlarge)
References
Darby RR, Dickerson BC. Dementia, Decision Making, and Capacity. Harvard review of psychiatry. 2017 Nov/Dec:25(6):270-278. doi: 10.1097/HRP.0000000000000163. Epub [PubMed PMID: 29117022]
Mitchell MA. Assessing Patient Decision-Making Capacity: It's About the Thought Process. Journal of emergency nursing. 2015 Jul:41(4):307-12. doi: 10.1016/j.jen.2014.10.014. Epub 2015 Jan 10 [PubMed PMID: 25583426]
Level 3 (low-level) evidenceAppelbaum PS. Clinical practice. Assessment of patients' competence to consent to treatment. The New England journal of medicine. 2007 Nov 1:357(18):1834-40 [PubMed PMID: 17978292]
Derse AR. Law and ethics in emergency medicine. Emergency medicine clinics of North America. 1999 May:17(2):307-25, ix [PubMed PMID: 10429630]
Moskop JC. Informed consent in the emergency department. Emergency medicine clinics of North America. 1999 May:17(2):327-40, ix-x [PubMed PMID: 10429631]
Level 3 (low-level) evidenceDepartment of Health, Education, and Welfare, National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont Report. Ethical principles and guidelines for the protection of human subjects of research. The Journal of the American College of Dentists. 2014 Summer:81(3):4-13 [PubMed PMID: 25951677]
Clark MA, Abbott JT, Adyanthaya T. Ethics seminars: a best-practice approach to navigating the against-medical-advice discharge. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2014 Sep:21(9):1050-7. doi: 10.1111/acem.12461. Epub [PubMed PMID: 25269588]
Kahn JH. Confidentiality and Capacity. Emergency medicine clinics of North America. 2020 May:38(2):283-296. doi: 10.1016/j.emc.2020.01.003. Epub [PubMed PMID: 32336325]
Jones RC, Holden T. A guide to assessing decision-making capacity. Cleveland Clinic journal of medicine. 2004 Dec:71(12):971-5 [PubMed PMID: 15641525]
Pachet A, Allan L, Erskine L. Assessment of fluctuating decision-making capacity in individuals with communication barriers: a case study. Topics in stroke rehabilitation. 2012 Jan-Feb:19(1):75-85. doi: 10.1310/tsr1901-75. Epub [PubMed PMID: 22306631]
Level 3 (low-level) evidenceNelson J, Venkat A, Davenport M. Responding to the refusal of care in the emergency department. Narrative inquiry in bioethics. 2014 Spring:4(1):75-80. doi: 10.1353/nib.2014.0008. Epub [PubMed PMID: 24748262]
Level 3 (low-level) evidenceGoldfrank LR, Wittman I. Capacity? Informed Consent; Informed Discharge? Uncertainty! Annals of emergency medicine. 2017 Nov:70(5):704-706. doi: 10.1016/j.annemergmed.2017.05.009. Epub 2017 Jun 26 [PubMed PMID: 28662910]
Snyderman D, Rovner B. Mental status exam in primary care: a review. American family physician. 2009 Oct 15:80(8):809-14 [PubMed PMID: 19835342]
Larkin GL, Marco CA, Abbott JT. Emergency determination of decision-making capacity: balancing autonomy and beneficence in the emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2001 Mar:8(3):282-4 [PubMed PMID: 11229953]
Schaefer MR, Monico EP. Documentation proficiency of patients who leave the emergency department against medical advice. Connecticut medicine. 2013 Sep:77(8):461-6 [PubMed PMID: 24156173]
Level 2 (mid-level) evidence