Introduction
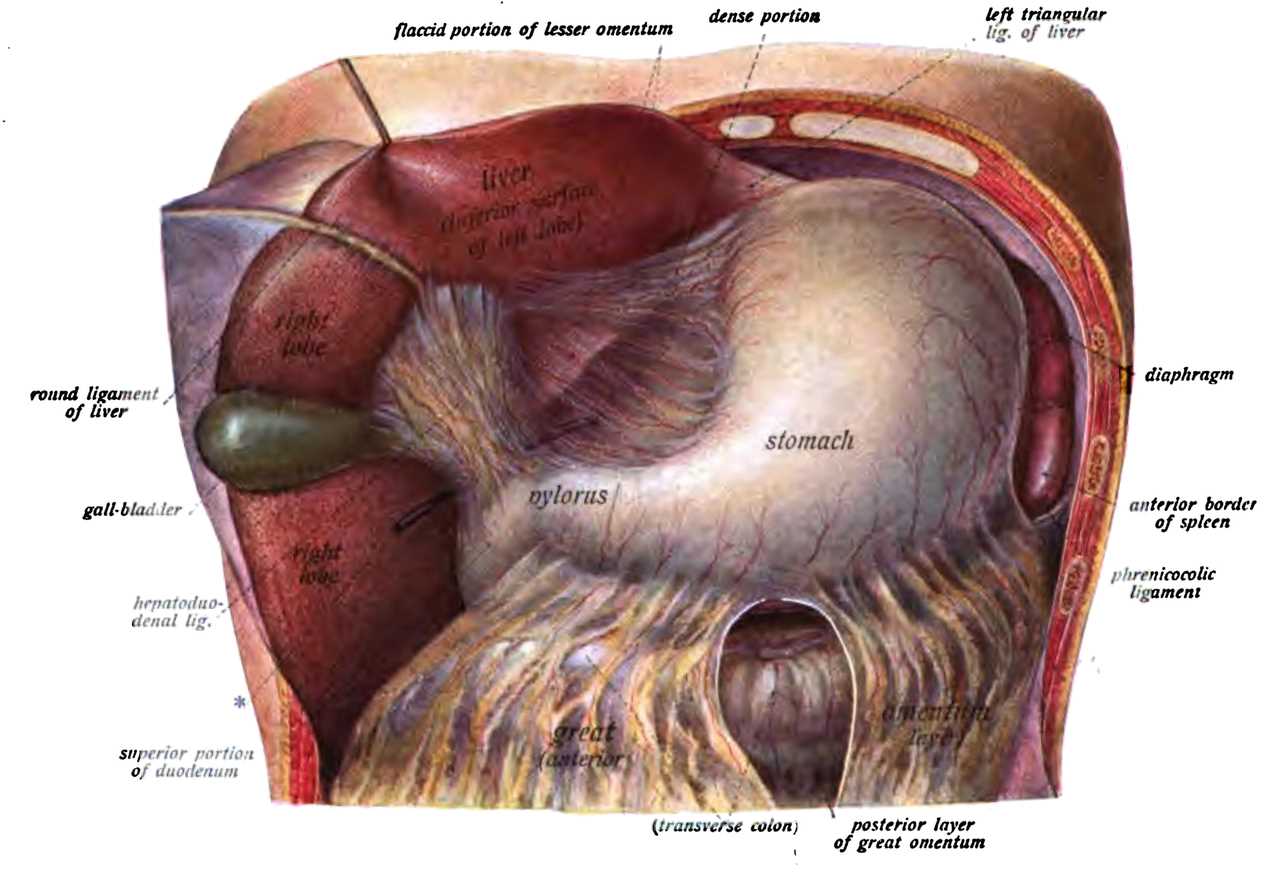
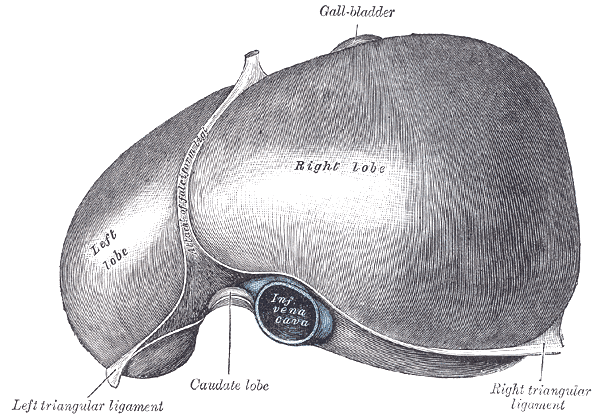
The liver is found inferior to the diaphragm and occupies most of the abdomen's right upper quadrant (RUQ). It is mostly intraperitoneal, from the fifth intercostal space in the midclavicular line to the right costal margin. The superior posterior aspect of the liver contains a bare area where the diaphragm and inferior vena cava are found (see Image. The Liver). The rest of the liver is covered by the visceral peritoneum, which meets the diaphragm at the border of the bare area, forming the coronary ligament. The inferior liver is closely associated with the gallbladder and right kidney (see Image. Inferior Surface of the Liver). Another ligament of mention is the Falciform ligament, which splits the liver into anatomic left and right along the anterior aspect. The falciform ligament's free-form edge contains the liver's round ligament, which is the remnant of the embryonic umbilical vein. Anatomically, the liver has 4 lobes: right, left, caudate, and quadrate. The caudate lobe is demarcated medially by the ligamentum venosum, posteriorly by the inferior vena cava, and anteriorly by the porta hepatis (see Image. Posterior and Inferior Surfaces of the Liver). The ligamentum venosum is the remnant of the embryonic ductus venosus. The quadrate lobe is anterior to the porta hepatis and lateral to the round ligament of the liver and is closely associated with the gallbladder. However, these anatomic lobes do not correlate to the boundaries of the 8 functional sub-divisions of the liver, which are divided according to the blood supply.[1][2][3]
The functional unit of the liver is the lobule. Liver lobules are collections of hepatocytes in a hexagonal shape, with the center being a central vein. Within the lobules, the hepatocytes are arranged in cords, and in between the cords is a vascular space with a thin fenestrated endothelium and a discontinuous membrane called a sinusoid. These sinusoids contain Kupffer cells, the resident macrophage of the liver, and stellate cells, which are hepatic lipocytes. At the vertices of the hexagon is a triad of a bile duct branch, a portal vein branch, and a hepatic artery branch, referred to as a portal triad. Blood flows from the portal vein branch and hepatic artery branch across the lobule and finally into the central vein, a branch of the hepatic vein. An alternative organization of hepatocytes places the line between 2 triads at the center of a rhomboid, with the ends being central veins. This arrangement is called the portal acinus and helps describe the functional zones of the liver. Zone 1 hepatocytes immediately surround the portal tracts and are primarily involved in oxidative energy metabolism. Zone 3 hepatocytes immediately surround the central veins and are the primary location for the biotransformation of drugs. Zone 2 hepatocytes lie between zones 1 and 3 and have mixed functionality.
The liver protects the body from toxic substances absorbed from the gastrointestinal (GI) tract by processing and metabolism within the lobule. The cytochrome P-450 enzyme system catabolizes phase-I reactions, while phase-II reactions conjugate substances with substrates such as glucuronide, glutathione, and sulfate.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Anatomically, the liver has 4 lobes: right, left, caudate, and quadrate (see Image. Liver Anatomy). The quadrate lobe is located on the inferior surface of the right lobe. The caudate lobe is located between the left and right lobes in an anterior and superior location.
The liver is the largest gland in the body and is ideally located to receive absorbed nutrients and detoxify absorbed drugs and other noxious substances. It serves as both an exocrine organ and an endocrine organ. The exocrine functionality of the liver is mainly in the synthesis and excretion of bile salts into the common hepatic duct, as well as the conjugation of bilirubin and excretion into the gut. The endocrine functions of the liver include involvement in glycemic control via insulin and glucagon. The liver synthesizes important proteins such as fibrinogen, albumin, prothrombin, and other amino acids and modifies proteins into enzymes and peptide hormones. The liver participates in fatty acid metabolism and synthesizes lipoproteins, cholesterol, and phospholipids. Additionally, it is involved in the metabolism of carbohydrates, which includes storing glycogen and gluconeogenesis. It also is involved in the metabolism of lactic acid and converts ammonia to urea. The liver stores vitamins and minerals such as iron. In summary, the liver is an important mediator from the gut to the blood and plays a vital role in the metabolism of macronutrients, hormones, components of blood plasma, and exocrine and endocrine substances.
Embryology
The liver, gallbladder, and biliary system arise from a ventral proliferation of endoderm that grows into mesoderm from the caudal part of the foregut. This outgrowth happens in the fourth week of embryonic growth and is called the hepatic diverticulum or liver bud. The endoderm of the liver bud differentiates into hepatocytes, while the mesoderm becomes connective tissue and blood vessels. It is important to remember that the liver has a hematopoietic role throughout the fetal period.
Blood Supply and Lymphatics
The liver receives a dual blood supply, with 75% to 80% of the blood volume coming from the portal vein and 20% to 25% from the hepatic artery. The portal vein is formed from the superior mesenteric and splenic veins posterior to the neck of the pancreas. It is joined by the proper hepatic artery, a branch of the celiac trunk, and the common bile duct to form the portal triad, enclosed in the hepatoduodenal ligament. Within the portal triad and associated branches, the bile leaves the liver in the bile ducts while the portal vein and hepatic artery are delivering blood to the liver; this creates countercurrent flow, which allows for the optimized exchange of electrolytes, bile acids, and other compounds.
Venous drainage of the liver occurs primarily via the left, right, and middle hepatic veins. The left hepatic vein accounts for 20.7% of the venous drainage and primarily drains the left lobe of the liver. The middle hepatic vein accounts for 32.7% of hepatic drainage and drains the middle portions of the left and right lobes of the liver. The right hepatic vein accounts for 39.6% of drainage and drains the lateral portion of the right lobe of the liver. The caudate lobe of the liver drains into the middle hepatic vein in most cases. In some cases, it drains directly into the retrohepatic portion of the inferior vena cava.[4][5]
Nerves
The hepatic plexus innervates the liver. This plexus consists of sympathetic fibers from the celiac plexus and parasympathetic fibers from the anterior and posterior vagal trunks. The hepatic plexus accompanies the vessels and biliary ducts within the portal triad.
Physiologic Variants
Partial liver transplants can be made, primarily by harvesting the right lobe of the liver. Care must be taken to account for possible variations in the anatomy of the liver. Common variations include absent main-right portal vein (14.5%) and multiple bile duct abnormalities. Patients with portal vein abnormalities are highly likely to have multiple bile ducts (88.9%).[6]
Surgical Considerations
Surgical treatment of portal hypertension secondary to liver damage or portal vein thrombosis is achieved using a trans-hepatic portosystemic shunt (TIPS) procedure. This procedure involves connecting the portal vein, which brings blood into the liver, and the inferior vena cava, which drains blood out of the liver. This provides a method by which blood can bypass the damaged hepatic system to alleviate portal venous congestion.[7][8]
Clinical Significance
The liver can be involved in many pathologies, so only a few of the most common conditions are mentioned. When the liver's exocrine function is impaired, either by physical blockage of the bile ducts, hepatocyte damage, or dysfunction of conjugation, bilirubin concentration rises in the blood. This manifests as a yellowing of the skin and sclera, called jaundice, and can be associated with itching, mental status changes, edema, and spider vessels.
The liver is highly vascular and is the main site for portocaval anastomosis. Patients with portal hypertension often exhibit signs of venous congestion at points of portocaval anastomoses. This can lead to esophageal varices, rectal hemorrhoids, and caput medusae.
Budd-Chiari syndrome is the blockage of hepatic venous drainage caused by thrombosis of 1 or more major hepatic veins. This condition should be considered in patients with hypercoagulable states that present with signs of portal hypertension, such as ascites, jaundice, or varices. Patients with right heart failure may also present with these signs due to back-up of blood through the inferior vena cava, but these patients are not considered to have Budd-Chiari syndrome. The diagnosis of Budd-Chiari syndrome is made with ultrasound or MRI.[9][10]
Media
(Click Image to Enlarge)
The Liver. The superior surface of the liver.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
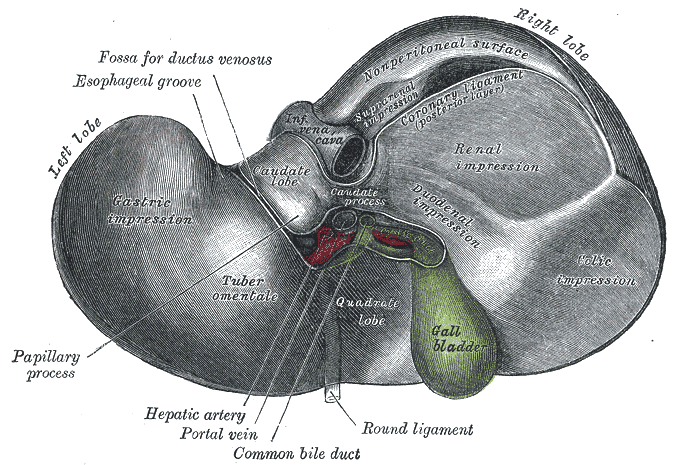
Inferior Surface of the Liver. The inferior surface of the liver, including the gall bladder, hepatic artery, portal vein, and common bile duct, is shown in this image.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
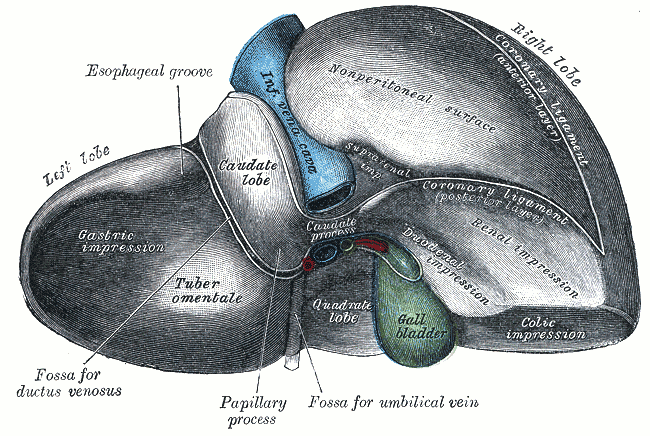
Posterior and Inferior Surfaces of the Liver. The posterior and inferior surfaces of the liver are shown in this image.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Alessandrino F, Ivanovic AM, Souza D, Chaoui AS, Djokic-Kovac J, Mortele KJ. The hepatoduodenal ligament revisited: cross-sectional imaging spectrum of non-neoplastic conditions. Abdominal radiology (New York). 2019 Apr:44(4):1269-1294. doi: 10.1007/s00261-018-1829-0. Epub [PubMed PMID: 30448917]
Level 2 (mid-level) evidenceNota CL, Hagendoorn J, Fong Y. ASO Author Reflections: The Role of Robotic Surgery in Liver Resection. Annals of surgical oncology. 2019 Feb:26(2):591-592. doi: 10.1245/s10434-018-7082-5. Epub 2018 Dec 11 [PubMed PMID: 30539495]
Abdel-Misih SR, Bloomston M. Liver anatomy. The Surgical clinics of North America. 2010 Aug:90(4):643-53. doi: 10.1016/j.suc.2010.04.017. Epub [PubMed PMID: 20637938]
Tani K,Shindoh J,Akamatsu N,Arita J,Kaneko J,Sakamoto Y,Hasegawa K,Kokudo N, Venous drainage map of the liver for complex hepatobiliary surgery and liver transplantation. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2016 Dec; [PubMed PMID: 27665239]
Ortale JR, Borges Keiralla LC. Anatomy of the portal branches and the hepatic veins in the caudate lobe of the liver. Surgical and radiologic anatomy : SRA. 2004 Oct:26(5):384-91 [PubMed PMID: 15300411]
Bageacu S, Abdelaal A, Ficarelli S, Elmeteini M, Boillot O. Anatomy of the right liver lobe: a surgical analysis in 124 consecutive living donors. Clinical transplantation. 2011 Jul-Aug:25(4):E447-54. doi: 10.1111/j.1399-0012.2011.01466.x. Epub 2011 Apr 26 [PubMed PMID: 21518003]
Level 2 (mid-level) evidenceStrunk H, Marinova M. Transjugular Intrahepatic Portosystemic Shunt (TIPS): Pathophysiologic Basics, Actual Indications and Results with Review of the Literature. RoFo : Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 2018 Aug:190(8):701-711. doi: 10.1055/a-0628-7347. Epub 2018 Jul 25 [PubMed PMID: 30045395]
Song T, Rössle M, He F, Liu F, Guo X, Qi X. Transjugular intrahepatic portosystemic shunt for hepatorenal syndrome: A systematic review and meta-analysis. Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver. 2018 Apr:50(4):323-330. doi: 10.1016/j.dld.2018.01.123. Epub 2018 Feb 17 [PubMed PMID: 29422242]
Level 2 (mid-level) evidenceVan Wettere M, Bruno O, Rautou PE, Vilgrain V, Ronot M. Diagnosis of Budd-Chiari syndrome. Abdominal radiology (New York). 2018 Aug:43(8):1896-1907. doi: 10.1007/s00261-017-1447-2. Epub [PubMed PMID: 29285598]
Grus T, Lambert L, Grusová G, Banerjee R, Burgetová A. Budd-Chiari Syndrome. Prague medical report. 2017:118(2-3):69-80. doi: 10.14712/23362936.2017.6. Epub [PubMed PMID: 28922103]