Introduction
Enophthalmos is defined as the posterior displacement of the globe in an anteroposterior plane within the orbit (see Image. Orbit, Anterior View). This is to be distinguished from hyperglobus, hypoglobus, esoglobus, and exoglobus.[1] The opposite of enophthalmos is proptosis, also termed exophthalmos, where the globe is displaced forward in an anteroposterior direction.
Clinically, the eye may appear sunken and have a deeper superior sulcus with either an upper eyelid retraction, upper eyelid ptosis, or, often, both, eyelid retraction with lagophthalmos as well as ptosis because of the three-dimensional change in the orbital tissues and the eyelid. Dryness may be the initial presenting symptom. Some patients will notice the asymmetry in their eye positions. It should be remembered that the normal position of the globe varies according to age, ethnic background, and sex. African orbits are shallower than White orbits, resulting in the appearance of relatively "proud eyes."
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Enophthalmos may be congenital or acquired and may be associated with systemic syndromes and local orbital disease.[2]
Etiology and Pathophysiology
Enophthalmos may be caused by one or more of the following anatomical and physiological factors:
- Enlargement of the orbit
- Reduction of the orbital contents
- Shrinkage or contracture of orbital contents
1. Enlargement of the Orbit
Enlargement of the orbit may be because of a defect in the orbital walls or a displacement of one or more of the orbital walls. Causes include:
- Orbital fractures: Orbital floor fractures are the most common cause of enophthalmos. Trauma is commonly seen during sports, motor vehicle accidents, fighting, and, less commonly, after endonasal surgery. An isolated blow-out fracture involves the expansion of the orbital cavity as the medial and inferior walls of the orbit fracture without the disruption of the orbital rim. This, in turn, causes herniation of the contents of the orbit (fat, muscle, globe) through the defect. The expansion of the orbital space results in enophthalmos. Maxillofacial injuries, including Le Fort II, III, and zygomaticomaxillary complex fractures (ZMC fractures), also involve the orbit and may also result in malpositioning of the globe. Isolated lateral wall and roof fractures do not usually cause significant enophthalmos. With orbital roof fractures, proptosis is more commonly seen. Extensive lateral wall fractures can result in enophthalmos. Indeed, manipulation of the lateral orbital wall and creating a surgical enophthalmos allows the surgeon to improve the proptosis seen in thyroid orbitopathy. Enophthalmos is not usually an immediate finding after orbital trauma as there is significant surrounding edema, intramuscular hematoma, chemosis, periorbital ecchymosis, and proptosis of the globe in the acute stage. Enophthalmos may only be visible 6 - 20 days after there is a resolution of swelling. Smaller fractures of the orbital floor (those less than 50% in size) are linked to a smaller incidence of post-traumatic enophthalmos. Large fractures (over 150mm²) are highly likely to present with enophthalmos and, therefore, can be used as predictors of enophthalmos severity.[3] Although most cases of enophthalmos will be evident within two weeks of trauma, in some patients, secondary orbital changes leading to progressively greater enophthalmos may occur over months.
- Maxillary sinus disease with outbowing of the orbital floor (also called the silent sinus syndrome or chronic maxillary sinus atelectasis): Silent sinus syndrome (SSS) usually occurs in the 30-60 age group. It is an insidious condition involving painless progressive unilateral enophthalmos, vertical diplopia with mild to moderate facial asymmetry, lagophthalmos, and hypoglobus.[4] A vacuum effect created by disruption of the drainage of the maxillary sinus into the middle meatus through a triggering event is thought to be the etiology of the silent sinus syndrome. As the fluid gathers within the maxillary sinus, it is slowly reabsorbed, creating a progressive negative pressure. This results in a downward force on the orbital floor.[5][6] The chronic nature of this process induces bony remodeling of the maxillary sinus that can be viewed on MRI or CT of the orbit, seen as opacification of the sinuses and bowing of the orbital floor. Although this is classically documented as a chronic process over the years, changes with maxillary antrum collapse have been shown to occur within a few months.[7][8] It is thought that lateralization of the middle turbinate may be responsible for the creation of negative pressure in the maxillary sinus with downward displacement of the orbital floor a result. Patients will develop enophthalmos without pain and will gradually worsen, sometimes with no history of sinus problems. Most patients respond to the creation of a middle meatal antrostomy, which improves the sinus aeration. The malposition of the globe (enophthalmos, hypoglobus) can be corrected subsequently with orbital floor volume augmentation, although both procedures may be performed at the same time.
- Missing or deficient sphenoidal wing secondary to neurofibromatosis: patients may present with enophthalmos or proptosis and will often have pulsations of the globe because of the communication between the orbit and the brain. Interpositional barrier grafts (bone, medpore, etc.) help resolve these problems.
- Age-related bony changes of the orbit: With age, there is an enlargement of the orbital cavity. The bony opening of the orbit expands horizontally and obliquely with associated enophthalmos. Expansion of the bony cavity results in enophthalmos and hypoglobus with an associated deep superior sulcus and skeletonization of the periorbital region. Such involutional changes are addressed with tissue repositioning and lipotransfer.
2. Reduction of Orbital Contents
- Age-related fat atrophy: Age-related changes are largely associated with lipoatrophy of the peri-ocular region and intra-orbital fat. These changes begin as young as age 20 years and may be associated with syndromes that affect the integrity of the ocular surface in the elderly.[9] The lack of orbital fat causes a loss of supportive elements in orbit, thereby causing posterior displacement of the globe. The temples and cheeks will show volume loss early. Lipofilling and liposculpting may be used to improve these changes. Some changes seen in the periorbital region have been given specific names because of a collection of findings. One variant is the Giant Fornix Syndrome [GFS]. GFS presents with gradually increasing weakness of the levator aponeurosis and deepening of the fornices, which can perpetuate persistent staphylococcal pseudomembranous conjunctivitis. The resulting infection, enophthalmos, and lagophthalmos can have determinantal effects on the ocular surface. Intensive topical lubrication with or without steroid treatment and antibiotics are required to manage the condition.[10] The Senile Sunken Eye Syndrome is so-named to specifically reflect the deepening of the superior sulcus due to lipoatrophy. The deep superior sulcus results in malposition of the upper eyelid, which may show ptosis or retraction (or both), with lagophthalmos. Patients will frequently have a corneal epithelial breakdown and may even have eyelid entropion.[11][[12]
- Orbital varix: orbital varices more often cause proptosis, but because of the expansion and shrinkage of the venous anomaly, enophthalmos may also develop. Varix fills with the Valsalva maneuver and causes proptosis. Orbital fat atrophy can result from repeated venous expansion and shrinkage. Patients may present with pressure, pain, or proptosis that varies with the position of the head. Some patients will notice symptoms when partaking in activities like playing instruments (trumpet) or in sports where there is a frequent positional change of the head (yoga, for example). An MRI may not show varix unless a scan is performed with the Valsalva maneuver. Ultrasound examination of the orbit will show a low-flow mass, which fills with the Valsalva maneuver. Hemorrhage in varix may result in pain and limitation of ocular movement. Vision loss is uncommon but can occur. When managing this condition, the resection of varices is usually not successful. Partial removal, coagulation, use of glues, and thrombosing agents like bleomycin may be needed.
- Radiotherapy: when radiation is administered to the head in childhood, as is done for the treatment of rhabdomyosarcoma or retinoblastoma, enophthalmos and loss of facial fat may occur. As many as a third of patients receiving radiotherapy in childhood will eventually develop these changes. There will be associated osseous hypoplasia together with atrophy or the orbital contents with resultant hemifacial changes that may require extensive reconstruction and lipotransfer. Bilateral facial radiotherapy will result in bilateral deformities, which can give an hourglass type of facial deformity. Besides enophthalmos, there will be loss of temporal fullness, atrophy of the temporalis muscle, deep superior sulci, and hypotelorism. Surgical intervention yields poor results because of the effects of radiotherapy on the tissues and the poor blood supply.
- Lipodystrophy: Lipodystrophy syndromes present with abnormal fat distribution. Many different syndromes are associated with lipodystrophy, congenital as well as acquired.[13] There may be excess fat or insufficient fat (lipoatrophy). Lipodystrophy syndromes can present with diabetes mellitus (insulin resistant), pancreatitis, hepatic cirrhosis, proteinuria, and renal failure. Enophthalmos and loss of facial fat are features that may be found in these syndromes. Specific treatment for enophthalmos associated with the lipodystrophy syndromes is rarely sought.
- Linear scleroderma: Localized scleroderma or morphea is an inflammatory autoimmune disease process that causes sclerosis of the skin and subcutaneous tissue.[14] The incidence of the disease is between 0.34 and 2.7 cases per 100,000 per year, tends to affect white females, and can start in early childhood.[14][15] Although there are many sub-types, those types which cause enophthalmos include morphea en coup de sabre (linear lesions on the frontoparietal scalp and forehead with the appearance as if struck by a sword) and progressive hemifacial atrophy (Parry-Romberg Syndrome) – both predominately affect the soft tissue of the head and neck. Patients report a progressive, painless enophthalmos and restrictions of upward gaze and subsequent diplopia.[16][17] Although there is no defined auto-antibody for linear scleroderma, those associated with rheumatic disease can be utilized: Anti-nuclear antibody (ANA), anti-topoisomerase antibody type of anti-nuclear autoantibodies (anti-Scl-70), and anti-histone antibodies (AHA).[18] They are used alongside the Localised Scleroderma Assessment tool (LoSCAT), which provides a score used to measure disease activity and damage.[19] The mainstay of treatment includes steroids, methotrexate, and psoralen-UVA photochemotherapy.[20]
- Parry-Romberg Syndrome/Hemifacial atrophy: Parry-Romberg syndrome [PRS] causes lipodystrophy of one-half of the face with the loss of fat in the dermal and subcutaneous tissues. It is seen mostly in females in the first two decades of life with slow progression. The skin becomes thinner and may become pigmented over time. The underlying muscles and bones are usually normal. Besides enophthalmos, the patient may present with ptosis, strabismus (restrictive type), coloboma, heterochromia, and uveitis. The exact cause is unknown, but unlike linear scleroderma, in Parry-Romberg syndrome, the elastic fibers are preserved. Ophthalmologists and general practitioners who witness signs of enophthalmos or facies with a deviation of the mouth to the affected side or eyelid alterations should consider early PRS.[12] Treatment includes fat transfer and soft tissue surgery.
- Orbital surgery: any kind of orbital surgery where there is the removal of normal or abnormal soft tissue will, by definition, result in orbital volume loss. These patients may present with enophthalmos, hypoglobus, or both. Iatrogenic enophthalmos may occur after orbital decompression. This was more often seen when aggressive removal of the orbital floor, the medial orbital wall, and lateral orbital wall were undertaken. The patient may end up with a sunken eye (often termed the sunken eye syndrome) resulting from enophthalmos and hypoglobus because of the expansion of the orbit and lack of appropriate support for the globe because of disruption of the Koornneef septae and fascial supporting structures in orbit.[21]
- Orbital trauma: even in the absence of orbital wall fractures, severe trauma, especially with hemorrhage and hematoma, can result in orbital fat loss and consequent enophthalmos.
- Drugs: Prostaglandin analogs, which are used to treat glaucoma, can affect fat cell metabolism resulting in fat loss with associated enophthalmos, deep superior sulci, and hollowing of the lower eyelid cheek junction with the inferior orbital rim prominence. There may be associated ptosis, inferior scleral show, prominence of eyelid vessels, and tightness of the eyelids. This has been termed prostaglandin-associated perirbitopathy (PAP). There is only a partial recovery after the prostaglandin analogs are stopped.
- HIV infection: HIV infection will cause bitemporal volume deficiency and enophthalmos. There is a generalized loss of subcutaneous fat in the face. There may be a marked loss of orbital fat. Patients receiving nucleoside treatment will experience these changes more often.
3. Shrinkage or Contracture of Orbital Contents
- Metastatic orbital disease: Orbital metastasis is a rare occurrence that accounts for 1 to 13% of orbital tumors.[22] The incidence may seem to be higher in recent years due to increased awareness, improved technology for detection, and diagnostics, e.g., fine-needle aspiration biopsy. Orbital metastases may arise from cancers of the prostate, lung, the gastrointestinal tract, skin, and the parotid gland. 53% of metastatic orbital lesions are from breast carcinoma. The literature indicates that the actual incidence of metastatic breast carcinoma to the orbits may be much higher because of smaller cancers, which may be present undetected in the orbits.[23] Patients may present with unilateral or bilateral metastatic disease with symptoms of limitation of ocular movements, double vision, proptosis or enophthalmos, and decreased vision.[24]
- Metastatic scirrhous breast cancer generally causes enophthalmos of the affected eye, as opposed to the classical space-occupying mass effect of most metastatic disease, and can often be the first clinical sign of breast carcinoma.[24][25] Fibrotic infiltration of the orbital soft tissue in scirrhous metastatic breast disease causes retraction with fibrosis of the orbital tissues. It is thought that the other mechanism involved is one of fat atrophy where the metastatic cells replace orbital fat and promote the deposition of collagen with resultant contraction of the soft tissue inducing atrophy and eventual necrosis. Breast metastatic disease should always be considered in middle-aged women who present with unilateral or bilateral enophthalmos in the absence of trauma or other diseases. An ophthalmic examination, examination of the breasts, and imaging of the orbits are obtained. MRI is the best modality for diagnosing metastatic breast carcinoma.[26]
- In an aging population and with improved imaging and more widespread use of imaging, orbital metastases are being increasingly recognized. In the presence of new enophthalmos, especially when there is a restrictive pattern of ocular motility reduction, it is important to consider metastatic disease as a possibility. A biopsy of the lesion is required to confirm a diagnosis, followed by PET/CT to investigate the locations of metastatic disease.[27]
- Trauma: severe trauma can cause injury to orbital vessels and fat with resultant loss of orbital volume even in the absence of any bony fractures.
- Fibrosis: Congenital fibrosis syndrome is a congenital disorder that is non-progressive. Patients present with restrictive ophthalmoplegia, strabismus, severe ptosis, and a chin-up position of the head. Most patients' eyes are fixed in downgaze, and they, therefore, have a chin-up position. The fibrosis of the extraocular muscles will also give the appearance of enophthalmos. Because these are bilateral conditions, the enophthalmos is not usually noticeable. Congenital fibrosis syndrome types 1 and 3 are autosomal dominant, and type 2 is autosomal recessive. The condition is caused by hypoplasia of the extraocular muscles, which is a result of the affliction of the oculomotor nerve. The decreased innervation of the extraocular muscles causes hypoplasia of the extraocular muscles. It is, therefore, not true fibrosis, as was initially thought. The ptosis is managed with frontalis slings, and strabismus surgery is performed to improve the head position of the child and improve eye alignment in the primary position.
Epidemiology
Enophthalmos reported in the literature largely affects males more than females, as the most common cause is related to trauma. In a retrospective study of 629 patients with orbital fractures, the male to female ratio was 5.7:1, with a mean of 37.2 years of age.[3]
History and Physical
Symptoms
The underlying etiology of enophthalmos usually determines the presenting symptoms. These symptoms can include:
- Facial asymmetry
- Double vision
- Dry eye
- Cosmetic complaints
- Droopy upper eyelid (ptosis)
- Difficulty focusing
- Deep superior sulcus[28]
Clinical Examination
In unilateral cases, the asymmetry of the orbits and globes may be obvious. The deep-set eye may show the associated deep sulcus, relative ptosis, lagophthalmos, and reduced palpebral fissure. Many patients will have associated hyperglobus, hypoglobus, esoglobus, or exoglobus.[1]
The best way to visually examine for relative enophthalmos is the chin-up position, also known as the dog's view or the lover's view (attributed to the French, but this may be apocryphal). See Image. Enophthalmos Examination.
Objective Measurement of Enophthalmos
The orbit is comprised of seven bones. The superior wall involves the lesser wing of the sphenoid and the orbital plate of the frontal bone. Both the zygomatic bone and the greater wing of the sphenoid form the lateral wall. The inferior wall is composed of three bones: the zygomatic, the maxilla, and the palatine bones. Finally, the medial wall is made of the sphenoid, the ethmoid, and the maxilla.[29] These seven bones form a protective housing for the globe which protrudes just beyond the orbital rim. Enophthalmos can be defined as a difference of 2mm or more in the anteroposterior axis between the two globes when measured from the lateral edge of the orbit to the maximum height of the corneal surface.[30] This definition assumes that one of the globes is in a normal position for the particular patient.
Clinical Measurement: Exophthalmometry
The clinical assessment of enophthalmos is measured with respect to the individual's orbital margins and is the degree of the anteroposterior position of the globe. A popular tool for clinical assessment is exophthalmometry. This allows the clinician to diagnose and monitor the changes in the globe position. Several different exophthalmometers are available, each with its advantages and disadvantages. See Image. Enophthalmos, Types of Exophthalmometers Used to Measure the Globe Position.
Hertel exophthalmometer: measures from the lateral orbital rim to the apex of the corneal surface. It is relatively easy to use in the clinical setting, but its use is dependent on the integrity of the lateral orbital rim, which is often lost in orbital-zygomatic fractures. It has also been found that inter-observer variation is high.[31]
Naugle exophthalmometer: is a similar, horizontally placed bar between two lateral canthi; it takes this a step further by using a 4-point fixation system, involving the superior and inferior orbital margins. Black markers along the length of the instrument aid in finding the midpoint of the pupils, thereby allowing the user to easily reposition the instrument for a serial of reproducible measurements. A study comparing Hertel and Naugle exophthalmometry found Naugle measurements to be more reliable in those who have suffered orbito-zygomatic fractures, where the lateral border of the orbit is disturbed, and the patient experience is more pleasant.[32]
A Leudde prism exophthalmometer: allows parallax error to be removed when observing both eyes to assess the degree of enophthalmos or exophthalmos. A parallax error occurs when the viewing angle changes between observers who do not view an object from an angle that is perpendicular to the object. The Leudde prism is used as a ruler and placed on the lateral orbital rim as a point of reference.
The Mourits exophthalmometer: combines the use of prisms placed along with a graduated metal frame (much like the Hertel instrument) and is thought to be a reliable tool when compared to Leudde and Hertel tools.[31]
Evaluation
Computed-Tomography (CT) and magnetic resonance imaging (MRI) are the two modalities most commonly used when assessing orbital diseases and trauma. CT imaging is best used when bony detail needs to be assessed. MRI is more useful for the assessment of soft tissue detail.
Computed tomography provides an excellent view of the contents of the orbit and allows for accurate measurements of the degree of enophthalmos without necessarily relying on a single reference point. The lateral orbital rim may still be used.[33] In the case of fractures, the nasal septum with the mirror image of the unaffected eye can be substituted to quantify enophthalmos or the styloid process can also act as a point of reference.[34] The change in volume of orbital contents can be accurately measured using CT and may be compared to the normal side. Axial scans are most useful in assessing the degree of enophthalmos and for serial comparisons.
Zhang et al demonstrated a statistically significant relationship using CT to measure orbital volume and the volume of herniated contents in orbital fractures to the degree of enophthalmos measured.[33] The sagittal and coronal reconstructions of the orbit can be very useful in the assessment of the orbital floor in maxillofacial trauma and essential for surgical planning.[35] CT imaging does expose the patient to radiation. Once a diagnosis is established and where specific soft tissue change does not need to be assessed (carcinoma, etc), exophthalmometry is the best tool for clinical follow-up. A systematic review of exophthalmometry by Nightengale et al. (they used the Mourtis exophthalmometer) suggested that exophthalmometry may be successfully used for long-term follow-up of patients and helps reduce repeated radiation exposure with CT scans.[36]
Treatment / Management
The treatment of enophthalmos starts with a good clinical workup of the patient, including a full medical and ocular history with the progression of symptoms (old photographs may prove useful). A full eye examination is performed with an assessment of visual fields, ocular movements, and any changes in visual acuity. In the case of trauma, this may be quite straightforward as a patient may experience proptosis, followed by increasing diplopia and enophthalmos over weeks after the initial insult.
Conservative management of traumatic injuries may be a choice in some patients who do not wish to undergo orbital surgery or in those where surgery is not indicated due to the size of the fracture (small), or the absence of significant clinical symptoms e.g. diplopia caused by post-traumatic enophthalmos.[37] An oculocardiac reflex is often an indication to operate in the acute phase. This reflex presents with persistent vomiting, bradycardia, and syncope in a pediatric population. It occurs due to trapped soft tissue (commonly the inferior rectus). It is recommended that surgery in the delayed setting occur within a 2-week window, as this is sufficient time for edema to resolve and for an accurate assessment of enophthalmos or diplopia to be made. The risk of developing the orbital compartment syndrome which is a sight-threatening complication is also reduced.[35]
Another indication is the cosmetic correction of enophthalmos, especially when it is apparent to visual assessment. The degree to which enophthalmos may be apparent varies by race, age, and underlying facial and orbital anatomy. Surgical management can be guided by CT scans using an 'enophthalmos estimate line': this virtual line is drawn between the most distal part of the fractured segment to the original position of the fracture segment.[38] This provides a prediction of enophthalmos a patient may experience over time. The surgical aim is near normal ocular motility and resolution of diplopia.[39] (B3)
Techniques include metal plates for fracture reduction or the placement of orbital floor implants to support its contents. More rarely, fat injections for globe support may be used. These techniques are also used to help those with the Silent Sinus Syndrome where endoscopic maxillary antrostomy and uncinectomy (clearing of the osteomeatal complex) are performed. This aims to increase the size of the opening to the maxillary sinus and promotes drainage of any accumulated fluids, thereby decompressing the sinus system. By establishing aeration of the sinus, the procedure may reduce enophthalmos by up to 2 mm.[40](B3)
Differential Diagnosis
True enophthalmos should be distinguished from the appearance of enophthalmos where there is no true anteroposterior change in the globe positions. This is often termed pseudoenophthalmos.[28][41] The differential diagnosis includes the following:
- Contralateral exophthalmos or proptosis may make the normal side look abnormal (enophthalmic).
- Facial asymmetry: Hemifacial microsomia, which may be congenital or facial asymmetry following trauma, can lead to the appearance of pseudoenophthalmos.
- Phthisis bulbi: Globe shrinkage secondary to an intraocular infection, trauma, or surgery will result in a reduced volume of the globe giving rise to a secondary appearance of a sunken globe and associated ptosis even though there may not be true axial posterior displacement of the globe. See Image. Enophthalmos, Phthisis Bulbs.
- Microphthalmos: Microphthalmos is a congenitally small eye where the globe volume is reduced without any associated ocular abnormalities. The corneal diameter will be smaller than the opposite eye. Microphthalmia may be seen in patients with hemifacial microsomia (see Image. Enophthalmos, Microphthalmos).
- Anisometropia: If one eye is more myopic, it will look bigger and, therefore, proptosis. Similarly, a more hypermetropic eye may look smaller and may give the impression of enophthalmos. 3 diopters of refraction result in a 1 mm difference in the axial length of the eye when refractive surgery has not been performed
- Horner syndrome: A lesion of the sympathetic pathway to the eye will result in ptosis, miosis, anhidrosis, and an appearance of enophthalmos. The paresis of the Muller's muscle, which is sympathetically innervated, results in ptosis and the lower eyelid may be elevated compared to the opposite side, resulting in the appearance of enophthalmos. Hertel measurements are usually normal.
- Ptosis: Congenital or acquired ptosis can result in a deeper superior sulcus giving the impression of enophthalmos.
- Post-enucleation socket syndrome (PESS), also known as the anophthalmic socket: Loss of an eye, may result in decreased orbital volume, ptosis, deep superior sulcus, lower lid laxity, and, sometimes, relative upper lid retraction. The prosthetic eye will give the appearance of being enophthalmic and may need volume restoration surgery together with eyelid surgery to give a more normal appearance.
Prognosis
The prognosis for patients with enophthalmos varies with etiology. The surgical treatment of the silent sinus syndrome or orbital fractures is generally performed in the younger age groups with a generally excellent outcome.[5] Following traumatic orbital repair, the cosmetic and functional outcomes are satisfactory. However, residual enophthalmos and limitation of ocular motility can remain, depending upon the extent of bony and soft tissue injury.[42][43] With orbital metastatic disease, the treatment of enophthalmos is rarely undertaken as the nature of the underlying primary tumor with the possibility of other tumors systemically will determine the prognosis. The 5-year survival rate in those who required orbital exenteration due to metastasis is 41.2% in a case series of 39 patients.[44]
Complications
Complications of surgical management of enophthalmos include:
- Facial asymmetry
- Residual diplopia/limitation of ocular motility
- Vision loss
- Entropion/ectropion
- Iatrogenic worsening of enophthalmos
Deterrence and Patient Education
Essential patient eduction in the presence of new enophthalmos includes advice on how vision may affect their day-to-day activities (driving, work, etc.) depending upon the effect of the enophthalmos on vision and on any double vision. In the presence of orbital fractures, the patient is advised not to blow the nose to avoid orbital emphysema.
Enhancing Healthcare Team Outcomes
Understanding the various causes of enophthalmos is invaluable in ensuring patients receive the correct care by the relevant specialist teams. Enophthalmos is detectable to casual examination by a physician if there is more than 2 mm of difference in the globe position. In social life, cosmetic concern usually arises only if there is a larger degree of enophthalmos. Because of the large number of underlying conditions that can cause enophthalmos, appropriate referral, examination, and assessment are vital.[45]
The care of patients with enophthalmos will require ophthalmologists (often to first clinically diagnose non-traumatic enophthalmos), oculoplastic surgeons, and maxillofacial surgeons to reconstruct orbital fractures and to improve the aesthetic and functional outcomes. Close interaction with radiologists is vital to assess the appropriate imaging and to allow for any surgical planning to be undertaken.[46] [Level 5]
Media
(Click Image to Enlarge)

Orbit, Anterior View. Shown in this illustration are the supraorbital notch, ethmoidal foramina, optic foramen, superior orbital fissure (hourglass configuration), greater wing of the sphenoid bone, zygomaticofacial foramen, inferior orbital fissure, infraorbital groove, zygomaticomaxillary suture, infraorbital foramen, infraorbital suture, posterior lacrimal crest, anterior lacrimal crest, frontomaxillary suture, and lamina papyracea. The walls of the orbit include the frontal bone superiorly; ethmoid, frontal, lacrimal, and sphenoid bones medially; maxilla, zygomatic, and palatine bones inferiorly; and zygomatic and sphenoid bones laterally.
Johannes Sobotta, MD, Public Domain, Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
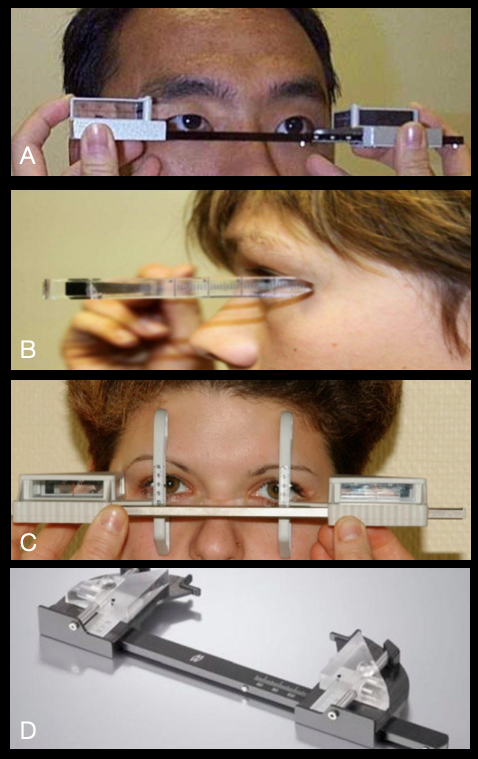
Enophthalmos, Types of Exophthalmometers Used to Measure the Globe Position. The different types of exophthalmometers that are used to measure the globe position are the Hertel exophthalmometer (A), the Leudde exophthalmometer (B), the Naugle exophthalmometer (C), and the Mourits exophthalmometer (D).
Contributed by BCK Patel, MD, FRCS
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Patel BC. In Praise of Precision: Esoglobus and Exoglobus. Ophthalmic plastic and reconstructive surgery. 2017 Jan/Feb:33(1):72-73. doi: 10.1097/IOP.0000000000000817. Epub [PubMed PMID: 27811634]
Erkoç MF, Öztoprak B, Gümüş C, Okur A. Exploration of orbital and orbital soft-tissue volume changes with gender and body parameters using magnetic resonance imaging. Experimental and therapeutic medicine. 2015 May:9(5):1991-1997 [PubMed PMID: 26136927]
Ahmad Nasir S, Ramli R, Abd Jabar N. Predictors of enophthalmos among adult patients with pure orbital blowout fractures. PloS one. 2018:13(10):e0204946. doi: 10.1371/journal.pone.0204946. Epub 2018 Oct 5 [PubMed PMID: 30289909]
Sheikhi M, Jalalian F. The silent sinus syndrome. Dental research journal. 2013 Mar:10(2):264-7 [PubMed PMID: 23946747]
Level 3 (low-level) evidenceArikan OK, Onaran Z, Muluk NB, Yilmazbaş P, Yazici I. Enophthalmos due to atelectasis of the maxillary sinus: silent sinus syndrome. The Journal of craniofacial surgery. 2009 Nov:20(6):2156-9. doi: 10.1097/SCS.0b013e3181bf0116. Epub [PubMed PMID: 19884840]
Level 3 (low-level) evidenceRapidis AD, Liarikos S, Ntountas J, Patel BC. The silent sinus syndrome: report of 2 cases. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2004 Aug:62(8):1028-33 [PubMed PMID: 15278871]
Level 3 (low-level) evidenceJacobs JM,Chou EL,Tagg NT, Rapid remodeling of the maxillary sinus in silent sinus syndrome. Orbit (Amsterdam, Netherlands). 2019 Apr; [PubMed PMID: 29742007]
Langer PD,Patel BC,Anderson RL, Silent sinus syndrome. Ophthalmology. 1994 Nov [PubMed PMID: 7800351]
Level 3 (low-level) evidenceAscher B, Coleman S, Alster T, Bauer U, Burgess C, Butterwick K, Donofrio L, Engelhard P, Goldman MP, Katz P, Vleggaar D. Full scope of effect of facial lipoatrophy: a framework of disease understanding. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2006 Aug:32(8):1058-69 [PubMed PMID: 16918569]
Level 3 (low-level) evidenceRose GE. The giant fornix syndrome: an unrecognized cause of chronic, relapsing, grossly purulent conjunctivitis. Ophthalmology. 2004 Aug:111(8):1539-45 [PubMed PMID: 15288985]
Level 3 (low-level) evidenceLiang L, Sheha H, Fu Y, Liu J, Tseng SC. Ocular surface morbidity in eyes with senile sunken upper eyelids. Ophthalmology. 2011 Dec:118(12):2487-92. doi: 10.1016/j.ophtha.2011.05.035. Epub 2011 Aug 27 [PubMed PMID: 21872934]
Level 3 (low-level) evidenceBucher F,Fricke J,Neugebauer A,Cursiefen C,Heindl LM, Ophthalmological manifestations of Parry-Romberg syndrome. Survey of ophthalmology. 2016 Nov - Dec; [PubMed PMID: 27045226]
Level 3 (low-level) evidenceFeingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R, New M, Purnell J, Sahay R, Shah AS, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, Akinci B, Gular MC, Oral EA. Lipodystrophy Syndromes: Presentation and Treatment. Endotext. 2000:(): [PubMed PMID: 29989768]
Bielsa Marsol I. Update on the classification and treatment of localized scleroderma. Actas dermo-sifiliograficas. 2013 Oct:104(8):654-66. doi: 10.1016/j.adengl.2012.10.012. Epub 2013 Aug 13 [PubMed PMID: 23948159]
George R, George A, Kumar TS. Update on Management of Morphea (Localized Scleroderma) in Children. Indian dermatology online journal. 2020 Mar-Apr:11(2):135-145. doi: 10.4103/idoj.IDOJ_284_19. Epub 2020 Mar 9 [PubMed PMID: 32477969]
Kapoor AG, Kumar SV, Bhagyalakshmi N. Localized scleroderma causing enophthalmos: A rare entity. Indian journal of ophthalmology. 2018 Nov:66(11):1611-1612. doi: 10.4103/ijo.IJO_303_18. Epub [PubMed PMID: 30355873]
Hock LE, Kontzialis M, Szewka AJ. Linear scleroderma en coup de sabre presenting with positional diplopia and enophthalmos. Neurology. 2016 Oct 18:87(16):1741-1742 [PubMed PMID: 27754909]
Khatri S, Torok KS, Mirizio E, Liu C, Astakhova K. Autoantibodies in Morphea: An Update. Frontiers in immunology. 2019:10():1487. doi: 10.3389/fimmu.2019.01487. Epub 2019 Jul 9 [PubMed PMID: 31354701]
Kelsey CE, Torok KS. The Localized Scleroderma Cutaneous Assessment Tool: responsiveness to change in a pediatric clinical population. Journal of the American Academy of Dermatology. 2013 Aug:69(2):214-20. doi: 10.1016/j.jaad.2013.02.007. Epub 2013 Apr 4 [PubMed PMID: 23562760]
Level 2 (mid-level) evidenceCareta MF, Romiti R. Localized scleroderma: clinical spectrum and therapeutic update. Anais brasileiros de dermatologia. 2015 Jan-Feb:90(1):62-73. doi: 10.1590/abd1806-4841.20152890. Epub [PubMed PMID: 25672301]
Koornneef L. Eyelid and orbital fascial attachments and their clinical significance. Eye (London, England). 1988:2 ( Pt 2)():130-4 [PubMed PMID: 3197870]
Novitskaya E, Rene C. Enophthalmos as a sign of metastatic breast carcinoma. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2013 Sep 17:185(13):1159. doi: 10.1503/cmaj.120726. Epub 2013 Mar 4 [PubMed PMID: 23460637]
Level 3 (low-level) evidenceShields JA, Shields CL, Brotman HK, Carvalho C, Perez N, Eagle RC Jr. Cancer metastatic to the orbit: the 2000 Robert M. Curts Lecture. Ophthalmic plastic and reconstructive surgery. 2001 Sep:17(5):346-54 [PubMed PMID: 11642491]
Level 2 (mid-level) evidenceAhmad SM,Esmaeli B, Metastatic tumors of the orbit and ocular adnexa. Current opinion in ophthalmology. 2007 Sep; [PubMed PMID: 17700235]
Level 3 (low-level) evidenceOrr CK, Cochran E, Shinder R. Metastatic Scirrhous Breast Carcinoma to Orbit Causing Enophthalmos. Ophthalmology. 2016 Jul:123(7):1529. doi: 10.1016/j.ophtha.2016.04.012. Epub [PubMed PMID: 27342331]
Homer N, Jakobiec FA, Stagner A, Cunnane ME, Freitag SK, Fay A, Yoon MK. Periocular breast carcinoma metastases: correlation of clinical, radiologic and histopathologic features. Clinical & experimental ophthalmology. 2017 Aug:45(6):606-612. doi: 10.1111/ceo.12926. Epub 2017 Mar 3 [PubMed PMID: 28181367]
Allen RC. Orbital Metastases: When to Suspect? When to biopsy? Middle East African journal of ophthalmology. 2018 Apr-Jun:25(2):60-64. doi: 10.4103/meajo.MEAJO_93_18. Epub [PubMed PMID: 30122850]
Hamedani M,Pournaras JA,Goldblum D, Diagnosis and management of enophthalmos. Survey of ophthalmology. 2007 Sep-Oct; [PubMed PMID: 17719369]
Level 3 (low-level) evidenceShumway CL, Motlagh M, Wade M. Anatomy, Head and Neck, Orbit Bones. StatPearls. 2024 Jan:(): [PubMed PMID: 30285385]
Bite U, Jackson IT, Forbes GS, Gehring DG. Orbital volume measurements in enophthalmos using three-dimensional CT imaging. Plastic and reconstructive surgery. 1985 Apr:75(4):502-8 [PubMed PMID: 3838589]
Delmas J, Loustau JM, Martin S, Bourmault L, Adenis JP, Robert PY. Comparative study of 3 exophthalmometers and computed tomographic biometry. European journal of ophthalmology. 2018 Mar:28(2):144-149. doi: 10.5301/ejo.5001049. Epub [PubMed PMID: 29108394]
Level 2 (mid-level) evidenceJeon HB,Kang DH,Oh SA,Gu JH, Comparative Study of Naugle and Hertel Exophthalmometry in Orbitozygomatic Fracture. The Journal of craniofacial surgery. 2016 Jan; [PubMed PMID: 26674913]
Level 2 (mid-level) evidenceZhang Z, Zhang Y, He Y, An J, Zwahlen RA. Correlation between volume of herniated orbital contents and the amount of enophthalmos in orbital floor and wall fractures. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2012 Jan:70(1):68-73. doi: 10.1016/j.joms.2011.02.036. Epub 2011 Jun 12 [PubMed PMID: 21664740]
Level 2 (mid-level) evidenceAfanasyeva DS, Gushchina MB, Gerasimov MY, Borzenok SA. Computed exophthalmometry is an accurate and reproducible method for the measuring of eyeballs' protrusion. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2018 Mar:46(3):461-465. doi: 10.1016/j.jcms.2017.12.024. Epub 2017 Dec 26 [PubMed PMID: 29325888]
Boyette JR, Pemberton JD, Bonilla-Velez J. Management of orbital fractures: challenges and solutions. Clinical ophthalmology (Auckland, N.Z.). 2015:9():2127-37. doi: 10.2147/OPTH.S80463. Epub 2015 Nov 17 [PubMed PMID: 26604678]
Nightingale CL,Shakib K, Analysis of contemporary tools for the measurement of enophthalmos: a PRISMA-driven systematic review. The British journal of oral [PubMed PMID: 31431316]
Level 1 (high-level) evidenceYoung SM, Kim YD, Kim SW, Jo HB, Lang SS, Cho K, Woo KI. Conservatively Treated Orbital Blowout Fractures: Spontaneous Radiologic Improvement. Ophthalmology. 2018 Jun:125(6):938-944. doi: 10.1016/j.ophtha.2017.12.015. Epub 2018 Feb 3 [PubMed PMID: 29398084]
Ramasamy A, Madhan B, Krishnan B. Comments on "A Straightforward Method of Predicting Enophthalmos in Blowout Fractures Using Enophthalmos Estimate Line". Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2017 Jun:75(6):1094. doi: 10.1016/j.joms.2017.01.045. Epub 2017 Mar 6 [PubMed PMID: 28279685]
Level 3 (low-level) evidenceMcRae M, Augustine HFM, Budning A, Antonyshyn O. Functional Outcomes of Late Posttraumatic Enophthalmos Correction. Plastic and reconstructive surgery. 2018 Aug:142(2):169e-178e. doi: 10.1097/PRS.0000000000004600. Epub [PubMed PMID: 30045183]
Thomas RD,Graham SM,Carter KD,Nerad JA, Management of the orbital floor in silent sinus syndrome. American journal of rhinology. 2003 Mar-Apr; [PubMed PMID: 12751704]
Level 3 (low-level) evidenceTripathy K, Chawla R, Temkar S, Sagar P, Kashyap S, Pushker N, Sharma YR. Phthisis Bulbi-a Clinicopathological Perspective. Seminars in ophthalmology. 2018:33(6):788-803. doi: 10.1080/08820538.2018.1477966. Epub 2018 Jun 14 [PubMed PMID: 29902388]
Level 3 (low-level) evidenceHazani R, Yaremchuk MJ. Correction of posttraumatic enophthalmos. Archives of plastic surgery. 2012 Jan:39(1):11-7. doi: 10.5999/aps.2012.39.1.11. Epub 2012 Jan 15 [PubMed PMID: 22783485]
Kim YH, Ha JH, Kim TG, Lee JH. Posttraumatic enophthalmos: injuries and outcomes. The Journal of craniofacial surgery. 2012 Jul:23(4):1005-9. doi: 10.1097/SCS.0b013e31824e6a1a. Epub [PubMed PMID: 22777457]
Level 2 (mid-level) evidenceAryasit O, Preechawai P, Hirunpat C, Horatanaruang O, Singha P. Factors related to survival outcomes following orbital exenteration: a retrospective, comparative, case series. BMC ophthalmology. 2018 Jul 28:18(1):186. doi: 10.1186/s12886-018-0850-y. Epub 2018 Jul 28 [PubMed PMID: 30055580]
Level 2 (mid-level) evidenceUgradar S, Lo C, Manoukian N, Putthirangsiwong B, Rootman D. The Degree of Posttraumatic Enophthalmos Detectable by Lay Observers. Facial plastic surgery : FPS. 2019 Jun:35(3):306-310. doi: 10.1055/s-0039-1688945. Epub 2019 May 17 [PubMed PMID: 31100769]
Kolk A, Pautke C, Schott V, Ventrella E, Wiener E, Ploder O, Horch HH, Neff A. Secondary post-traumatic enophthalmos: high-resolution magnetic resonance imaging compared with multislice computed tomography in postoperative orbital volume measurement. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2007 Oct:65(10):1926-34 [PubMed PMID: 17884517]


