Introduction
Dead bag syndrome is a rare cause of spontaneous intraocular lens (IOL) dislocation late after cataract surgery. A distinctive characteristic of dead bag syndrome is the presence of a clear capsule many years postoperatively. Predisposing factors include conditions associated with progressive zonular weakening, such as pseudoexfoliation, uveitis, myopia, connective tissue disorders, a history of vitrectomy, and ocular trauma.[1][2] However, the etiology of dead bag syndrome is still unclear.
Dead bag syndrome was first identified in the early 2000s and described by Dr. Samuel Masket, who reported IOL dislocation cases where the capsular bag was diaphanous and floppy, unequipped to support the IOL.[3] Patients with dead bag syndrome often present with visual disturbances due to IOL dislocation from the inability to screen for dead bag syndrome. Subluxation may occur either through a defect in the bag's periphery or an in-the-bag dislocation. In contrast to early IOL dislocation, which results from inadequate IOL fixation, dead bag syndrome is suspected to result from zonular weakness that develops as a late postoperative complication.[4][5] Late IOL dislocation occurs at least 3 months after cataract surgery, with reported occurrence between 6 and 12 years after surgery.[6]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The exact etiology of dead bag syndrome remains unknown. Current hypotheses revolve around trophic effects between the capsular basement membrane and lens epithelial cells (LECs) comprising the lens capsule. In nonpathologic conditions, the lens capsule is an uninterrupted basement membrane secreted by lens epithelial and fiber cells. To maintain its integrity, the capsule thickens over time due to the deposition of extracellular matrix and capsular components at the basal ends of the cortical lens fibers and LECs.[7][8] LECs are important for capsular development, but whether the condition's etiology arises from the basement membrane or the LECs is unclear.
Leading hypotheses include the following:
- A problem lies within the capsule, initiating a cycle of LEC damage and capsular degradation.[9][10]
- The problem lies within the LECs, causing degeneration that damages the capsule.
- Late postoperative zonular failure is related to capsule splitting or delamination occurring at the level of zonular attachments.[11]
This syndrome and IOL material or design do not appear to be associated.[12] Capsular structures that provide IOL stability and integrity require further investigation.
Epidemiology
Dead bag syndrome is a rare and poorly understood condition. Thus, few epidemiologic factors have been identified. However, predisposing factors include conditions associated with progressive zonular weakening, such as pseudoexfoliation, uveitis, myopia, connective tissue disorders, history of vitrectomy, and ocular trauma. These factors are not unique to dead bag syndrome but are also linked with other conditions causing zonular weakening. The frequency of dead bag syndrome across different sexes and age groups remains undetermined due to its rarity.
Pathophysiology
The currently proposed mechanism underlying dead bag syndrome is the absence or scarcity of LECs, potentially from prior capsular damage or LEC removal from polishing the capsule during cataract surgery. LEC scarcity may play a role in the pathophysiology of dead bag syndrome. However, the association between this condition and capsular polishing during cataract surgery has not been established. Supporting evidence includes the occurrence of dead bag syndrome being documented in cases where surgeons did not practice LEC removal. In addition, capsular polishing cannot remove all LECs and cannot reach the capsular bag equator, as this region is not readily visible.[13]
Histopathology
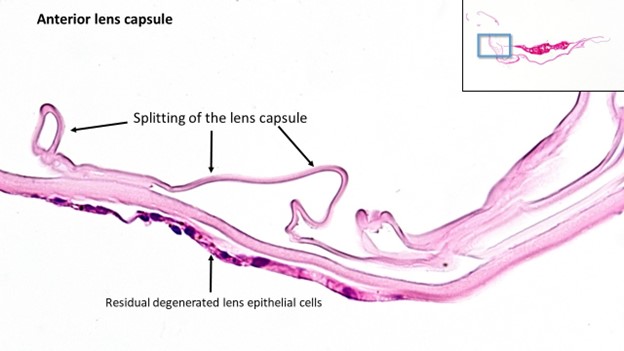
Dead bag syndrome differs from other causes of lens subluxation because it lacks capsular evidence of fibrosis or opacification. Histopathological findings from suspected cases show little to no LECs in the capsule. Additional findings include degradation signs, such as capsular thinning or splitting at zonular attachment sites, resulting in weak zonular support (see Image. Lens Capsule Splitting). Werner et al hypothesized that late postoperative zonular failure relates to capsule splitting or delamination at the zonular attachments. These features are considered characteristic of the pathology's late stages.
History and Physical
Dead bag syndrome is a disease spectrum most evident once it has progressed several years after cataract surgery. The condition's clinical progression and early manifestations have not been formally established. Consequently, clinicians cannot recognize patients in the perioperative or postoperative period who are likely to develop dead bag syndrome.
Difficulty in early recognition often leads to dead bag syndrome presenting with visual disturbances due to IOL dislocation. Patients may remain unaware of the condition if the IOL dislocation does not compromise central vision.
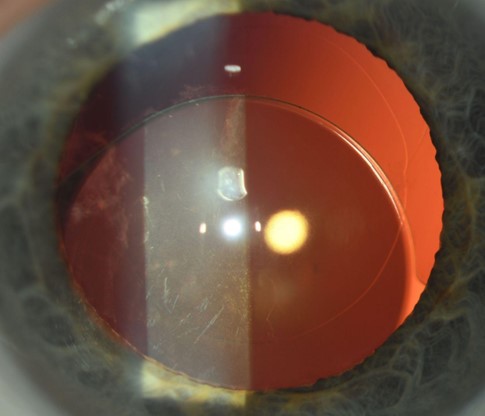
The capsular bag may appear dilated and diaphanous with clear anterior and posterior capsules without evidence of fibrosis or opacification on slit-lamp examination. Late postoperative evaluation may often show lens subluxation (see Image. Lens Dislocation).
Evaluation
A detailed medical, ocular, and surgical history should be obtained from the patient. Visual acuity, intraocular pressures, and pupillary examination should be performed. A comprehensive slit-lamp and fundus examination should be performed with a 90-diopter lens to assess the capsular bag. The degree of subluxation should be noted, as this clinical sign guides management. If the clinician prefers diagnostic testing, an anterior segment optical coherence tomography or an ultrasound biomicroscopy may be performed to assess the degree of subluxation of the lens and capsule.
Treatment / Management
Several unanswered questions remain regarding the clinical progression and etiology of dead bag syndrome. Therefore, the pathophysiology of dead bag syndrome results in complicated scenarios that often lead to improvisation in surgical technique and management. Based on the assessment of capsular integrity, IOL type, and biometric characteristics, surgical interventions include IOL rescue and repositioning or IOL-bag complex exchange.[14][15] Cases with mild subluxation require adherence to close follow-up. Meanwhile, cases with severe subluxation may necessitate exchanging a 1-piece IOL for a 3-piece IOL that allows for techniques such as sutureless Yamane transscleral fixation, glued or transscleral sutured posterior chamber IOL fixation. Anterior vitrectomy is recommended to thoroughly remove capsular remnants and is essential to prevent any inflammatory response.[16][17]
Differential Diagnosis
Other common causes of late IOL dislocation include true exfoliation syndrome and pseudoexfoliation syndrome.
True Exfoliation Syndrome
This condition typically affects older patients who have had significant exposure to high heat or infrared radiation. Therefore, the causative factor is due to age-related degeneration. Slit-lamp findings include thin capsule delamination, typically without zonular instability. Histopathological findings include lens capsule splitting, delamination, or schisis with varying amounts of LECs.[18][19]
Pseudoexfoliation Syndrome
Pseudoexfoliation is an age-related condition with a strong genetic component involving dysregulated tissue expression of the lysyl oxidase 1 gene. This condition is characterized by the deposition of fibrillar material in the anterior segment with or without the presence of a capsular contraction and rarely capsular phimosis. Histopathological findings often include fibrous metaplasia of anterior LECs or Soemmerring formation.[20][21]
Prognosis
The prognosis of dead bag syndrome depends on the level of zonular support. Currently, long-term data are insufficient to provide an explicit prognosis for patients with this condition.
Complications
The primary complication of dead bag syndrome is lens dislocation, which can lead to visual disturbances and decreased visual acuity. Dislocations can lead to retinal detachment, bleeding, and inflammation that can result in corneal or macular edema in some cases.
Deterrence and Patient Education
Surgeons may consider including this pathology in the informed consent process if a patient possesses various factors predisposing to its development. Awareness of dead bag syndrome should prompt cataract surgeons to reassess the diagnosis and treatment of patients with late IOL dislocations. Continuity of care and adherence to close follow-up must be emphasized to patients with an established diagnosis to prevent complications from dead bag syndrome. Patients should be aware of any visual disturbances they may experience after cataract surgery. Patients are encouraged to undergo comprehensive ophthalmic examinations to assess and screen for IOL and capsule positioning changes.
Enhancing Healthcare Team Outcomes
Effective communication among team members is crucial for managing dead bag syndrome. Ophthalmologists and optometrists must promptly recognize the symptoms and clinical signs of the condition. A detailed history of visual symptoms must be obtained before examination. Open and clear communication facilitates rapid diagnosis and treatment decisions, preventing errors and ensuring a coordinated response.
Ethical considerations guide care decisions. Informed consent is essential to respect patient autonomy and ensure beneficence and nonmaleficence. Patient preferences are central to decisions, promoting shared decision-making. Education and training keep the team updated on best practices. Ongoing professional development ensures that healthcare practitioners are equipped to manage dead bag syndrome. A patient-centered approach places the patient's well-being and preferences at the forefront of all decisions. An interprofessional healthcare team ensures a comprehensive response, minimizes complications, and prioritizes patient safety and care quality in managing dead bag syndrome.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Subasi S, Yuksel N, Karabas VL, Yilmaz Tugan B. Late in-the-bag spontaneous IOL dislocation: risk factors and surgical outcomes. International journal of ophthalmology. 2019:12(6):954-960. doi: 10.18240/ijo.2019.06.12. Epub 2019 Jun 18 [PubMed PMID: 31236352]
Werner L. The dead bag syndrome. Journal of cataract and refractive surgery. 2022 May 1:48(5):517-518. doi: 10.1097/j.jcrs.0000000000000930. Epub [PubMed PMID: 35703837]
Culp C, Qu P, Jones J, Fram N, Ogawa G, Masket S, Mamalis N, Werner L. Clinical and histopathological findings in the dead bag syndrome. Journal of cataract and refractive surgery. 2022 Feb 1:48(2):177-184. doi: 10.1097/j.jcrs.0000000000000742. Epub [PubMed PMID: 34261985]
Ascaso FJ, Huerva V, Grzybowski A. Epidemiology, Etiology, and Prevention of Late IOL-Capsular Bag Complex Dislocation: Review of the Literature. Journal of ophthalmology. 2015:2015():805706. doi: 10.1155/2015/805706. Epub 2015 Dec 21 [PubMed PMID: 26798506]
McKellar MJ, Elder MJ. The early complications of cataract surgery: is routine review of patients 1 week after cataract extraction necessary? Ophthalmology. 2001 May:108(5):930-5 [PubMed PMID: 11320024]
Kristianslund O, Dalby M, Drolsum L. Late in-the-bag intraocular lens dislocation. Journal of cataract and refractive surgery. 2021 Jul 1:47(7):942-954. doi: 10.1097/j.jcrs.0000000000000605. Epub [PubMed PMID: 33750091]
Yan Q, Blake D, Clark JI, Sage EH. Expression of the matricellular protein SPARC in murine lens: SPARC is necessary for the structural integrity of the capsular basement membrane. The journal of histochemistry and cytochemistry : official journal of the Histochemistry Society. 2003 Apr:51(4):503-11 [PubMed PMID: 12642629]
Liu W, Huang D, Guo R, Ji J. Pathological Changes of the Anterior Lens Capsule. Journal of ophthalmology. 2021:2021():9951032. doi: 10.1155/2021/9951032. Epub 2021 May 4 [PubMed PMID: 34055399]
Shentu XC, Zhu YN, Gao YH, Zhao SJ, Tang YL. Electron microscopic investigation of anterior lens capsule in an individual with true exfoliation. International journal of ophthalmology. 2013:6(4):553-6. doi: 10.3980/j.issn.2222-3959.2013.04.27. Epub 2013 Aug 18 [PubMed PMID: 23991396]
Thakur A, Bansal M, Challa D, Malhotra C, Jain AK. Dead bag syndrome-in the capsular bag subluxated intraocular lens centration and refixation: A new technique. Indian journal of ophthalmology. 2023 Oct:71(10):3412-3414. doi: 10.4103/IJO.IJO_1061_23. Epub [PubMed PMID: 37787245]
Danysh BP, Duncan MK. The lens capsule. Experimental eye research. 2009 Feb:88(2):151-64. doi: 10.1016/j.exer.2008.08.002. Epub 2008 Aug 16 [PubMed PMID: 18773892]
Sumioka T, Werner L, Yasuda S, Okada Y, Mamalis N, Ishikawa N, Saika S. Immunohistochemical findings of lens capsules obtained from patients with dead bag syndrome. Journal of cataract and refractive surgery. 2024 Aug 1:50(8):862-867. doi: 10.1097/j.jcrs.0000000000001472. Epub [PubMed PMID: 38711217]
Darian-Smith E, Safran SG, Coroneo MT. Comment on: Clinical and histopathological findings in the dead bag syndrome. Journal of cataract and refractive surgery. 2022 Jul 1:48(7):871-872. doi: 10.1097/j.jcrs.0000000000000960. Epub [PubMed PMID: 35514046]
Level 3 (low-level) evidenceCooke CA, Lum DJ, Wheeldon CE, Teoh H, McGhee CN. Surgical approach, histopathology, and pathogenesis in cataract associated with true lens exfoliation. Journal of cataract and refractive surgery. 2007 Apr:33(4):735-8 [PubMed PMID: 17397753]
Wong AL, Chan TC, Fong AH, Lam BN, Yuen HK. Clinical characteristics and surgical outcomes of phacoemulsification in true exfoliation syndrome. Journal of cataract and refractive surgery. 2014 Jan:40(1):82-6. doi: 10.1016/j.jcrs.2013.06.022. Epub 2013 Nov 14 [PubMed PMID: 24238944]
Darian-Smith E, Safran SG, Coroneo MT. Lens Epithelial Cell Removal in Routine Phacoemulsification: Is It Worth the Bother? American journal of ophthalmology. 2022 Jul:239():1-10. doi: 10.1016/j.ajo.2022.01.013. Epub 2022 Jan 23 [PubMed PMID: 35081415]
Fernández-Buenaga R, Alio JL, Pérez-Ardoy AL, Larrosa-Quesada A, Pinilla-Cortés L, Barraquer R, Alio JL 2nd, Muñoz-Negrete FJ. Late in-the-bag intraocular lens dislocation requiring explantation: risk factors and outcomes. Eye (London, England). 2013 Jul:27(7):795-801; quiz 802. doi: 10.1038/eye.2013.95. Epub 2013 Jun 14 [PubMed PMID: 23764989]
Senthilkumar VA, Krishna MS, Krishnadas R. True exfoliation with double delamination of the anterior lens capsule. Indian journal of ophthalmology. 2020 May:68(5):919. doi: 10.4103/ijo.IJO_1631_19. Epub [PubMed PMID: 32317488]
Karp CL, Fazio JR, Culbertson WW, Green WR. True exfoliation of the lens capsule. Archives of ophthalmology (Chicago, Ill. : 1960). 1999 Aug:117(8):1078-80 [PubMed PMID: 10448754]
Olawoye OO, Pasquale LR, Ritch R. Exfoliation syndrome in sub-Saharan Africa. International ophthalmology. 2014 Oct:34(5):1165-73. doi: 10.1007/s10792-014-9953-5. Epub 2014 May 21 [PubMed PMID: 24844849]
Liu E, Cole S, Werner L, Hengerer F, Mamalis N, Kohnen T. Pathologic evidence of pseudoexfoliation in cases of in-the-bag intraocular lens subluxation or dislocation. Journal of cataract and refractive surgery. 2015 May:41(5):929-35. doi: 10.1016/j.jcrs.2014.08.037. Epub 2015 Apr 29 [PubMed PMID: 25935341]
Level 3 (low-level) evidence