Introduction
The atrioventricular (AV) node is a subendocardial structure located in the inferior-posterior right atrium. In an average adult, an AV node measures approximately 1 x 3 x 5 millimeters and sits within an anatomic region bordered posteriorly by the coronary sinus ostium, superiorly by the tendon of Todaro, and anteriorly by the septal tricuspid valve annulus. This anatomic region is also commonly referred to as the triangle of Koch. The blood supply to the AV node is from the AV nodal branch of the right coronary artery (90%) or the left circumflex artery (10%) depending on the right or left dominant blood supply to the heart. The first septal perforator of the left anterior descending artery also supplies blood to the AV node.[1][2][3][4][5][6][7]
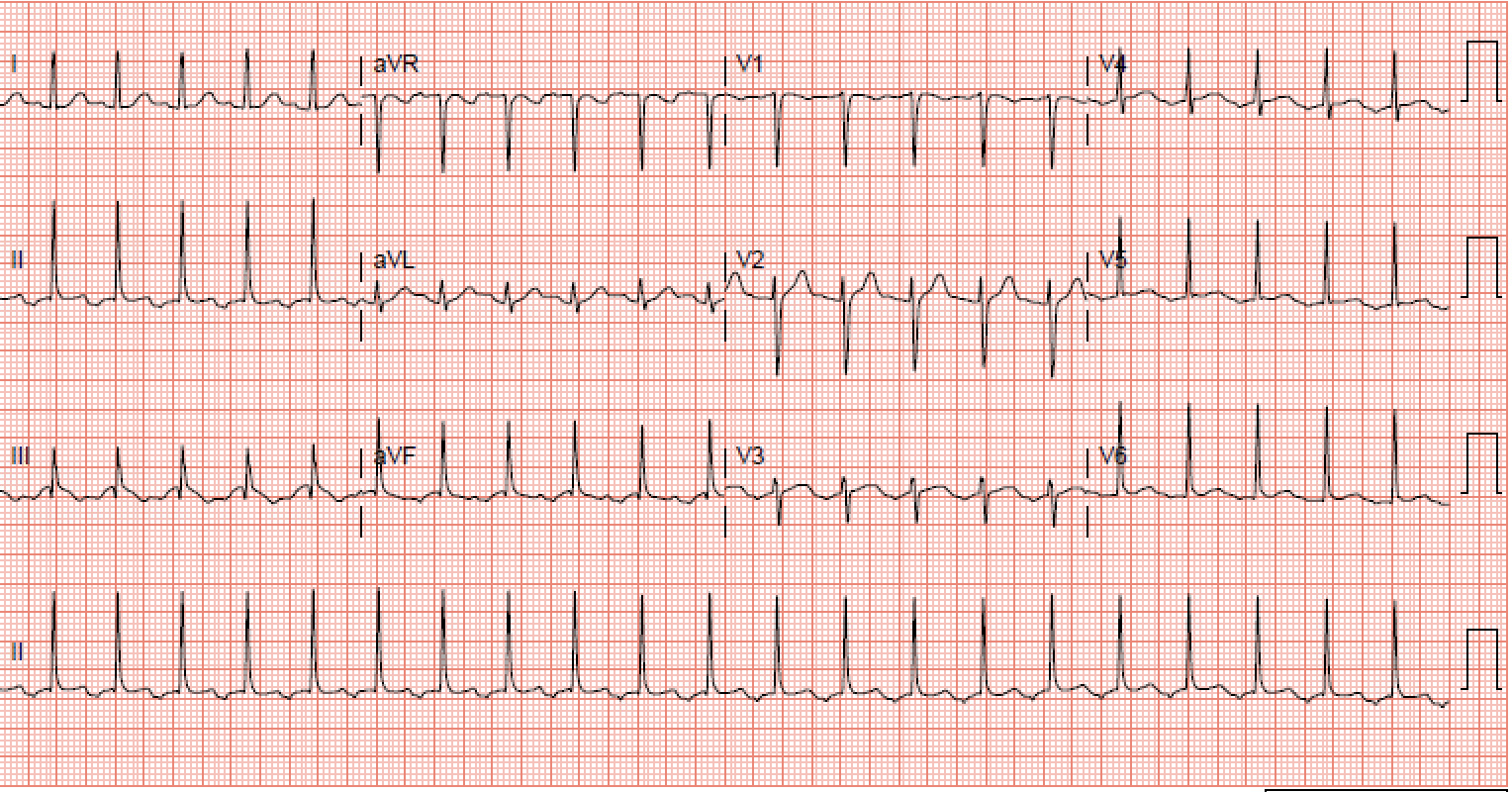
Atrioventricular nodal reentrant tachycardia (AVNRT) is a type of paroxysmal supraventricular tachycardia that results due to the presence of a reentry circuit within or adjacent to the AV node. The diagnosis of AVNRT requires visualization on an electrocardiogram (ECG). In most cases, an ECG will show heart rate between 140 and 280 beats per minute (bpm), and in the absence of aberrant conduction, a QRS complex of fewer than 120 milliseconds.[8][9][10] ECG criteria based on the reentrant circuits are as follows:
Slow-Fast AVNRT
- Pseudo-S wave in leads II, III, and AVF
- Pseudo-R' in lead V1.
Fast-Slow AVNRT
- P waves between the QRS and T waves (QRS-P-T complexes)
Slow-Slow AVNRT
- Late P waves after a QRS - often appears as atrial tachycardia
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Atrioventricular nodal reentry tachycardia is usually not prevalent in patients with structural heart disease. The anatomy of the reentrant circuit defines the type of AVNRT present. A slow-fast AVNRT accounts for 90% of AVNRTs with anterograde conduction by the slow AV nodal pathway and retrograde conduction by the fast AV nodal pathway. Fast-slow AVNRT represents approximately 5% to 10% of AVNRTs with anterograde conduction by the fast AV nodal pathway and retrograde conduction by the slow AV nodal pathway. Slow-slow AVNRTs account for 1% to 5% of AVNRTs with anterograde conduction by slow AV nodal pathways and retrograde conduction by slow atrial fibers.[10][11]
Epidemiology
The prevalence of atrioventricular nodal reentry tachycardia globally is similar to the United States. Close to 60% of the paroxysmal supraventricular tachycardia is AVNRT, with approximately two-thirds of that in women. A study found that the majority of patients presenting with symptoms due to AVNRT are in their twenties, but some patients might present with AVNRT in their seventh or eighth decade.[12]
Pathophysiology
A reentry circuit requires a difference in conduction velocity and refractory period. A fast conduction pathway has rapid conduction but a slow refractory period, whereas a slow conduction pathway has a rapid refractory period coupled with slow conduction.[10][13]
Histopathology
Despite being examined, it remains controversial whether fast and slow AV nodal conduction pathways share anatomical distinction or whether they represent functional diversity in the nodal structure.[14]
History and Physical
Patients with atrioventricular nodal reentrant tachycardia usually present with symptoms of dizziness, syncope, shortness of breath, intermittent palpitations, pain/discomfort in the neck, pain/discomfort in the chest, anxiety, and polyuria secondary atrial natriuretic factor secreted mainly by the heart atria in response to atrial stretch. Patients with AVNRT and a known history of coronary artery disease may present with a myocardial infarction secondary to the stress on the heart. Patients with AVNRT and a known history of heart failure may present with acute exacerbation and possibly reduced ejection fraction secondary to tachycardia-induced cardiomyopathy.[15]
Although syncope is an uncommon symptom in patients with AVNRT, it is typical in patients who have a heart rate above 170 bpm as less filling of the ventricles leads to the reduction in cardiac output and the decreased perfusion of the brain. Depression of the sinoatrial node secondary to tachycardia also may contribute to syncopal symptoms of patients who present with AVNRT.[16]
Patients with AVNRT usually present with a heart rate within the range of 140 to 280 bpm. If a patient has known heart failure or coronary artery disease, they may complain of chest pain. They also may have symptoms of heart failure such as tachypnea with wheezes or swelling in the lower extremities on physical exam. During a physical exam, a provider might be able to appreciate Cannon A waves as the atrium contracts in conjunction with the ventricular contractions against a closed tricuspid valve. Hypotension secondary to decreased ventricular filling also may be a significant physical exam finding in patients presenting with AVNRT.[17]
Evaluation
The most significant component of the assessment for a patient who presents with signs and symptoms of atrioventricular nodal reentrant tachycardia is a history and physical exam. These should include vital signs (respiratory rate, blood pressure, temperature, and heart rate) and an electrocardiogram. A patient presenting with AVNRT should undergo evaluation for any unknown underlying coronary artery disease or heart failure. During an assessment, the clinician should establish whether the patient is hemodynamically stable based mainly on his blood pressure, mental status, and respiratory rate. Initial evaluation of patients with AVNRT can include testing to access the patient's thyroid and pulmonary function, together with routine blood work and echocardiography.[18][19]
Treatment / Management
Management of patients presenting with atrioventricular nodal reentry tachycardia begins with an initial evaluation of their hemodynamic stability. Hemodynamically unstable patients present with tachycardia associated with hypotension, ischemic chest pain, altered mental status, respiratory failure, or shock. These patients need their AVNRT terminated electrically with an urgent electrical cardioversion. Hemodynamically stable patients should be treated first with vagal maneuvers to cease the rhythm acutely. If attempted twice and the patient remains in AVNRT, the clinicians should perform modified vagal exercises at least twice to terminate the arrhythmia. Once such maneuvers are unsuccessful or are inappropriate, intravenous (IV), it warrants medical therapy.[20][21][22](A1)
First-line medical therapy is IV adenosine, administered up to 18 mg given in increments of 6 mg in the absence of contraindications such as severe bronchospastic lung disease or severe coronary artery disease. In the event both vagal maneuvers and IV adenosine are unsuccessful or ruled inappropriate, IV non-dihydropyridine calcium channel blockers, IV beta-blockers, or IV digoxin are next in consideration. The selection of these IV medical agents is based upon the presence of concomitant factors, such as in patients with AVNRT and hypotension; IV digoxin may be appropriate as it lacks anti-hypertensive properties. Subsequently, in a patient who is actively wheezing secondary to a reactive airway, IV non-dihydropyridine calcium channel blockers should be used first.[23][24][25][26][27][28][29][30](A1)
IV adenosine terminates approximately 80% of AVNRT arrhythmias. Patients in whom medical treatment and Valsalva maneuvers fail or those who cannot tolerate medication due to its side effects might opt for catheter ablation as a one-time definitive cure. Catheter ablations in patients with AVNRT have a high success rate, reported to be as high as 95%. Prolonged medical therapy with Class III or IC antiarrhythmics such as flecainide, propafenone, amiodarone, dofetilide, or sotalol can be done in instances where the patient does not respond to calcium channel blockers or beta-blockers and refuses catheter ablation. The selection of these antiarrhythmics usually is based on patients' comorbidities and the drug side effect profiles.[31][32][33](B2)
Differential Diagnosis
Once a narrow QRS complex tachycardia is present on an electrocardiogram, and the rhythm becomes evaluated as regular, differential rhythms include the following[34]:
- Atrioventricular nodal reentrant tachycardia
- Atrioventricular reentrant tachycardia
- Intra-atrial reentrant tachycardia
- Sinoatrial nodal reentrant tachycardia
- Junctional ectopic tachycardia
- Atrial tachycardia
- Atrial flutter
- Sinus tachycardia
- Inappropriate sinus tachycardia
Prognosis
Prognosis is generally good when a healthcare provider promptly identifies the rhythm.
Complications
If not identified promptly, symptomatic complications such as syncope, fatigue, or dizziness can occur.
Deterrence and Patient Education
Educating patients at risk for this rhythm and making a closed-loop communication between them and their providers can help further improve the management of these rhythms.
Pearls and Other Issues
In rare instances, atrioventricular nodal reentry tachycardia can result in sudden cardiac arrest.[35]
Enhancing Healthcare Team Outcomes
An interprofessional team that provides an integrated approach in identifying that the patient is in atrioventricular nodal reentrant tachycardia and whether the patient is hemodynamically stable or not is integral towards managing patients with this arrhythmia. Upon establishing that the patient is hemodynamically stable, management decisions are possible through prompt communication between the physician, pharmacist, and nursing staff, which can significantly enhance healthcare team outcomes in patients with AVNRT. The clinician can consult with a board-certified cardiology pharmacist in selecting the most appropriate agent, verifying dosing parameters, and checking for interactions. Nursing will have a significant role as they will administer the drug chosen, and need to be aware of potential adverse event signs as well as assessing for therapeutic effectiveness. Once treated, if available, patient education is necessary, using resources familiar to the patient, including online resources and pamphlets. This interprofessional approach optimizes patient outcomes through open communication and collaborative effort. [Level 5]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
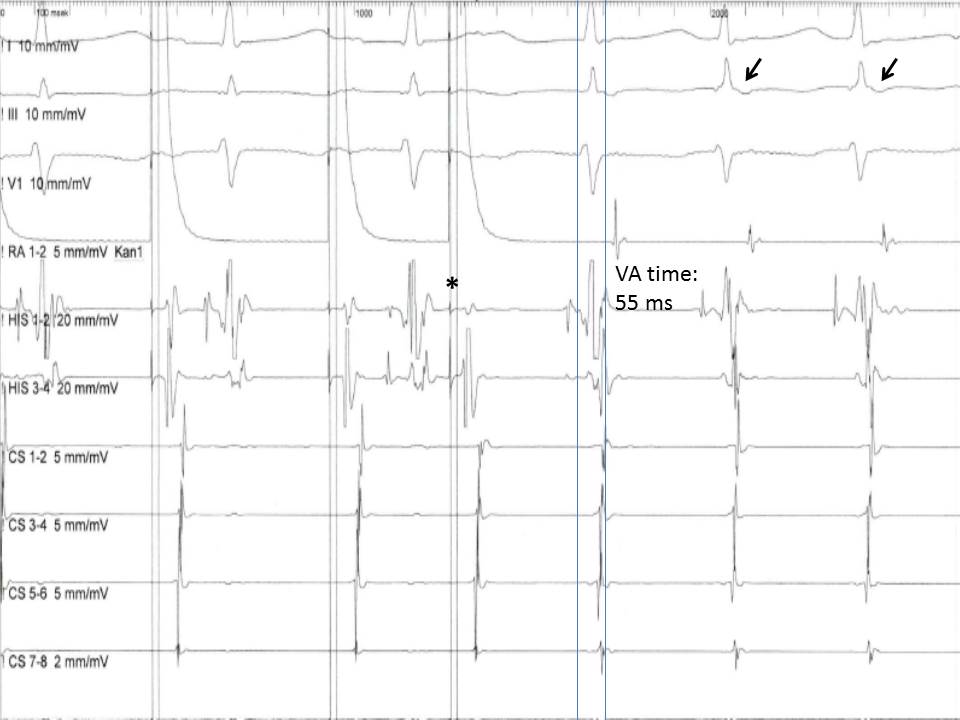
Induction of an Atrioventricular Nodal Reentry Tachycardia. This image shows the induction of an atrioventricular nodal reentry tachycardia (AVNRT) with a premature atrial extra stimulus (asterisk). Note the short ventriculoatrial time (<60 ms) in the His bundle recording and the retrograde P waves in the electrocardiogram leads (arrows).
Contributed by S Koulouris, MD
References
Inoue S, Becker AE. Koch's triangle sized up: anatomical landmarks in perspective of catheter ablation procedures. Pacing and clinical electrophysiology : PACE. 1998 Aug:21(8):1553-8 [PubMed PMID: 9725153]
Level 3 (low-level) evidenceSumitomo N, Tateno S, Nakamura Y, Ushinohama H, Taniguchi K, Ichikawa R, Fukuhara J, Abe O, Miyashita M, Kanamaru H, Ayusawa M, Harada K, Mugishima H. Clinical importance of Koch's triangle size in children: a study using 3-dimensional electroanatomical mapping. Circulation journal : official journal of the Japanese Circulation Society. 2007 Dec:71(12):1918-21 [PubMed PMID: 18037746]
Sánchez-Quintana D, Picazo-Angelín B, Cabrera A, Murillo M, Cabrera JA. Koch's triangle and the atrioventricular node in Ebstein's anomaly: implications for catheter ablation. Revista espanola de cardiologia. 2010 Jun:63(6):660-7 [PubMed PMID: 20515623]
Van der Hauwaert LG, Stroobandt R, Verhaeghe L. Arterial blood supply of the atrioventricular node and main bundle. British heart journal. 1972 Oct:34(10):1045-51 [PubMed PMID: 5086972]
Pejković B, Krajnc I, Anderhuber F, Kosutić D. Anatomical aspects of the arterial blood supply to the sinoatrial and atrioventricular nodes of the human heart. The Journal of international medical research. 2008 Jul-Aug:36(4):691-8 [PubMed PMID: 18652764]
Podziemski P, Zebrowski JJ. A simple model of the right atrium of the human heart with the sinoatrial and atrioventricular nodes included. Journal of clinical monitoring and computing. 2013 Aug:27(4):481-98. doi: 10.1007/s10877-013-9429-6. Epub 2013 Feb 22 [PubMed PMID: 23430363]
Saremi F, Abolhoda A, Ashikyan O, Milliken JC, Narula J, Gurudevan SV, Kaushal K, Raney A. Arterial supply to sinuatrial and atrioventricular nodes: imaging with multidetector CT. Radiology. 2008 Jan:246(1):99-107; discussion 108-9 [PubMed PMID: 18024438]
Level 2 (mid-level) evidenceDi Biase L, Gianni C, Bagliani G, Padeletti L. Arrhythmias Involving the Atrioventricular Junction. Cardiac electrophysiology clinics. 2017 Sep:9(3):435-452. doi: 10.1016/j.ccep.2017.05.004. Epub [PubMed PMID: 28838549]
Marzlin KM, Webner C. Atrioventricular Reentrant Tachycardia. AACN advanced critical care. 2017 Summer:28(2):223-228. doi: 10.4037/aacnacc2017151. Epub [PubMed PMID: 28592483]
Marzlin KM. Atrioventricular Nodal Reentrant Tachycardia. AACN advanced critical care. 2017 Spring:28(1):84-88. doi: 10.4037/aacnacc2017887. Epub [PubMed PMID: 28254859]
Yamaguchi T, Tsuchiya T, Nagamoto Y, Miyamoto K, Sadamatsu K, Tanioka Y, Kadokami T, Murotani K, Takahashi N. Anatomical and electrophysiological variations of Koch's triangle and the impact on the slow pathway ablation in patients with atrioventricular nodal reentrant tachycardia: a study using 3D mapping. Journal of interventional cardiac electrophysiology : an international journal of arrhythmias and pacing. 2013 Jun:37(1):111-20. doi: 10.1007/s10840-012-9769-z. Epub 2013 Feb 14 [PubMed PMID: 23408048]
Level 1 (high-level) evidenceLiuba I, Jönsson A, Säfström K, Walfridsson H. Gender-related differences in patients with atrioventricular nodal reentry tachycardia. The American journal of cardiology. 2006 Feb 1:97(3):384-8 [PubMed PMID: 16442401]
MOE GK, PRESTON JB, BURLINGTON H. Physiologic evidence for a dual A-V transmission system. Circulation research. 1956 Jul:4(4):357-75 [PubMed PMID: 13330177]
Abe H, Nagatomo T, Kobayashi H, Miura Y, Araki M, Kuroiwa A, Nakashima Y. Neurohumoral and hemodynamic mechanisms of diuresis during atrioventricular nodal reentrant tachycardia. Pacing and clinical electrophysiology : PACE. 1997 Nov:20(11):2783-8 [PubMed PMID: 9392809]
Ganz LI, Friedman PL. Supraventricular tachycardia. The New England journal of medicine. 1995 Jan 19:332(3):162-73 [PubMed PMID: 7800009]
Leitch JW, Klein GJ, Yee R, Leather RA, Kim YH. Syncope associated with supraventricular tachycardia. An expression of tachycardia rate or vasomotor response? Circulation. 1992 Mar:85(3):1064-71 [PubMed PMID: 1537103]
Goyal R, Zivin A, Souza J, Shaikh SA, Harvey M, Bogun F, Daoud E, Man KC, Strickberger SA, Morady F. Comparison of the ages of tachycardia onset in patients with atrioventricular nodal reentrant tachycardia and accessory pathway-mediated tachycardia. American heart journal. 1996 Oct:132(4):765-7 [PubMed PMID: 8831363]
Wood KA, Drew BJ, Scheinman MM. Frequency of disabling symptoms in supraventricular tachycardia. The American journal of cardiology. 1997 Jan 15:79(2):145-9 [PubMed PMID: 9193013]
Level 2 (mid-level) evidenceDoi A, Miyamoto K, Uno K, Nakata T, Tsuchihashi K, Shimamoto K. Studies on hemodynamic instability in paroxysmal supraventricular tachycardia: noninvasive evaluations by head-up tilt testing and power spectrum analysis on electrocardiographic RR variation. Pacing and clinical electrophysiology : PACE. 2000 Nov:23(11 Pt 1):1623-31 [PubMed PMID: 11138299]
Ferguson JD, DiMarco JP. Contemporary management of paroxysmal supraventricular tachycardia. Circulation. 2003 Mar 4:107(8):1096-9 [PubMed PMID: 12615783]
Level 3 (low-level) evidencePandya A, Lang E. Valsalva maneuver for termination of supraventricular tachycardia. Annals of emergency medicine. 2015 Jan:65(1):27-9. doi: 10.1016/j.annemergmed.2013.07.012. Epub 2013 Aug 7 [PubMed PMID: 23932719]
Alboni P, Tomasi C, Menozzi C, Bottoni N, Paparella N, Fucà G, Brignole M, Cappato R. Efficacy and safety of out-of-hospital self-administered single-dose oral drug treatment in the management of infrequent, well-tolerated paroxysmal supraventricular tachycardia. Journal of the American College of Cardiology. 2001 Feb:37(2):548-53 [PubMed PMID: 11216977]
Level 1 (high-level) evidenceGlatter KA, Cheng J, Dorostkar P, Modin G, Talwar S, Al-Nimri M, Lee RJ, Saxon LA, Lesh MD, Scheinman MM. Electrophysiologic effects of adenosine in patients with supraventricular tachycardia. Circulation. 1999 Mar 2:99(8):1034-40 [PubMed PMID: 10051297]
Level 2 (mid-level) evidenceRankin AC, Brooks R, Ruskin JN, McGovern BA. Adenosine and the treatment of supraventricular tachycardia. The American journal of medicine. 1992 Jun:92(6):655-64 [PubMed PMID: 1605147]
Page RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ, Estes NA 3rd, Field ME, Goldberger ZD, Hammill SC, Indik JH, Lindsay BD, Olshansky B, Russo AM, Shen WK, Tracy CM, Al-Khatib SM, Evidence Review Committee Chair‡. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2016 Apr 5:133(14):e506-74. doi: 10.1161/CIR.0000000000000311. Epub 2015 Sep 23 [PubMed PMID: 26399663]
Level 1 (high-level) evidenceCairns CB, Niemann JT. Intravenous adenosine in the emergency department management of paroxysmal supraventricular tachycardia. Annals of emergency medicine. 1991 Jul:20(7):717-21 [PubMed PMID: 2064090]
Margolis B, DeSilva RA, Lown B. Episodic drug treatment in the management of paroxysmal arrhythmias. The American journal of cardiology. 1980 Mar:45(3):621-6 [PubMed PMID: 7355758]
Level 3 (low-level) evidenceDougherty AH, Jackman WM, Naccarelli GV, Friday KJ, Dias VC. Acute conversion of paroxysmal supraventricular tachycardia with intravenous diltiazem. IV Diltiazem Study Group. The American journal of cardiology. 1992 Sep 1:70(6):587-92 [PubMed PMID: 1510006]
Level 1 (high-level) evidenceDiMarco JP, Sellers TD, Berne RM, West GA, Belardinelli L. Adenosine: electrophysiologic effects and therapeutic use for terminating paroxysmal supraventricular tachycardia. Circulation. 1983 Dec:68(6):1254-63 [PubMed PMID: 6640877]
Sung RJ, Elser B, McAllister RG Jr. Intravenous verapamil for termination of re-entrant supraventricular tachycardias: intracardiac studies correlated with plasma verapamil concentrations. Annals of internal medicine. 1980 Nov:93(5):682-9 [PubMed PMID: 7212475]
Level 1 (high-level) evidenceBagherzadeh A, Keshavarzi T, Farahani MM, Goodarzynejad H. Determinants of immediate success for catheter ablation of atrioventricular nodal reentry tachycardia in patients without junctional rhythm. Journal of interventional cardiac electrophysiology : an international journal of arrhythmias and pacing. 2014 Jan:39(1):19-23. doi: 10.1007/s10840-013-9839-x. Epub 2013 Oct 8 [PubMed PMID: 24101150]
Katritsis DG, Marine JE, Contreras FM, Fujii A, Latchamsetty R, Siontis KC, Katritsis GD, Zografos T, John RM, Epstein LM, Michaud GF, Anter E, Sepahpour A, Rowland E, Buxton AE, Calkins H, Morady F, Stevenson WG, Josephson ME. Catheter Ablation of Atypical Atrioventricular Nodal Reentrant Tachycardia. Circulation. 2016 Nov 22:134(21):1655-1663 [PubMed PMID: 27754882]
Chrispin J, Misra S, Marine JE, Rickard J, Barth A, Kolandaivelu A, Ashikaga H, Tandri H, Spragg DD, Crosson J, Berger RD, Tomaselli G, Calkins H, Sinha SK. Current management and clinical outcomes for catheter ablation of atrioventricular nodal re-entrant tachycardia. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2018 Apr 1:20(4):e51-e59. doi: 10.1093/europace/eux110. Epub [PubMed PMID: 28541507]
Level 2 (mid-level) evidenceSpector P, Reynolds MR, Calkins H, Sondhi M, Xu Y, Martin A, Williams CJ, Sledge I. Meta-analysis of ablation of atrial flutter and supraventricular tachycardia. The American journal of cardiology. 2009 Sep 1:104(5):671-7. doi: 10.1016/j.amjcard.2009.04.040. Epub [PubMed PMID: 19699343]
Level 1 (high-level) evidenceWang YS, Scheinman MM, Chien WW, Cohen TJ, Lesh MD, Griffin JC. Patients with supraventricular tachycardia presenting with aborted sudden death: incidence, mechanism and long-term follow-up. Journal of the American College of Cardiology. 1991 Dec:18(7):1711-9 [PubMed PMID: 1960318]
Level 2 (mid-level) evidence