Introduction
The craniocervical junction includes the occiput, C1 (atlas), and C2 (axis). C1, also known as the atlas, has a unique anatomy, located just inferior to the occiput, and connects the cranium to the cervical spine through the articulations with C2 (axis) and the occipital condyles. The occipito-atlantal and atlantoaxial articulations contribute significantly to flexion and rotation in the cervical spine, respectively, accounting for 50% of these movements. Due to their high degree of motion, these bony segments are the most commonly injured body parts in adults, particularly prone to fractures. Although C1 fractures rarely require surgery, they should be promptly identified and treated in all patients. Any fracture involving the atlas warrants a thorough examination of the ligamentous structures between C0 and C1 and C1 and C2.
The C1 (atlas) vertebra lacks a vertebral body and spinous process. Instead, it consists of anterior and posterior arches that encircle the spinal cord posteriorly and the odontoid process anteriorly. The lateral masses on either side join the arches, with their superior articular surfaces participating in the occipital-cervical joint and their inferior articular surfaces contributing to the highly mobile atlantoaxial joint. Stabilization of the atlantoaxial joint is achieved through the anterior atlantoaxial ligament (between the anterior ring of C1 and C2), the transverse ligament (posterior to the odontoid process), and the posterior atlantoaxial ligament (between the posterior ring of the atlas and C2). Among these, the transverse ligament plays the most significant role in C1-C2 articulation. C1 characteristically lacks a spinous process or vertebral body.[1] C1 behaves as an intercalated segment cradling the base of the occiput at the atlanto-occipital articulation, allowing almost 50% of flexion and extension movements at the neck.[2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
C1 fractures typically result from axial loading, often combined with flexion, extension, or rotation, leading to characteristic fracture patterns. This area is subject to high stresses from a large moment arm of the cranium. Low-energy trauma in older populations and high-impact trauma in young cohorts have been implicated in the pathogenesis of C1 fractures.[3][4]
Epidemiology
C1 fractures account for approximately 10% to 13% of all cervical spine fractures.[5][6] The annual incidence has shown a nearly 700% increase, estimated at 157 per million among older patients.[3] A bimodal distribution with peaks typically observed around ages 30 and 80 has been noted.[5][6] Most cases occur in individuals aged 50 or older.[3] With an aging population, the median age of involvement has been observed to increase annually by 2.6.[5] Only one-third of all C1 fractures are isolated,[4] with C2 being the most commonly associated injury.[7]
Pathophysiology
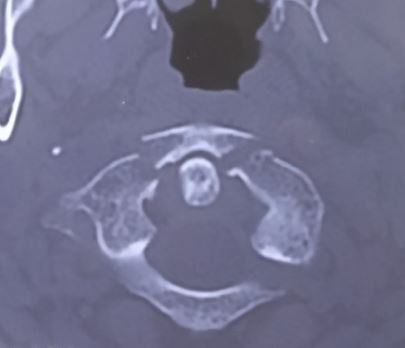
The classification of atlas ring fractures proposed by Gehweiler, with further subdivision of Gehweiler type 3b fractures as postulated by Dickman et al, is the most commonly utilized tool (see Images. C1 Arch Fracture and C1 Fracture).[8]
Gehweiler Classification System of C1 Fractures
The Gehweiler Classification categorizes C1 fractures into several types based on their anatomical location and characteristics, as mentioned below.
- Type 1: Fractures of the anterior arch of C1.
- Type 2: Fractures of the posterior arch of C1.
- Type 3: Fractures of both the anterior and posterior arches (Jefferson burst fracture).
- Type 3a: Ligamentous disruption.
- Type 3b: Bony avulsion with an intact transverse atlantal ligament (TAL).
- Type 4: Fractures of the lateral mass of the atlas.
- Type 5: Isolated fractures of the transverse process of the atlas.[4]
Dickman Classification System of Transverse Atlantal Ligament Injuries
The Dickman classification system categorizes TAL injuries into distinct types based on their nature and anatomical involvement, as mentioned below.
- Type 1: Intra-ligamentous rupture.
- Type 1a: Central lesion.
- Type 1b: Lesion close to the lateral mass.
- Type 2: Bony avulsion injuries.
- Type 2a: Isolated bony avulsion.
- Type 2b: Bony avulsion associated with lateral mass fractures.
Levine Classification System of C1 Fractures
The Levine classification system provides a structured approach to categorizing C1 fractures based on their specific patterns and locations, as mentioned below.
- Type 1: Involves an isolated bony apophysis (transverse process) fracture.
- Type 2: Involves an isolated posterior arch fracture.
- Type 3: Involves an isolated anterior arch fracture.
- Type 4: Represents a comminuted fracture of the lateral mass.
- Type 5: Describes a bilateral burst fracture (Jefferson fracture)
Notably, 50% of atlas fractures are associated with concomitant spine fractures, and there is a 40% association with axis fractures.
History and Physical
Most C1 fractures are caused by significant trauma, typically involving an axial load injury to the cranium, such as diving into shallow water, football tackles, or motor vehicle collisions resulting in blunt cranial trauma. However, certain patient populations, such as those with osteoporosis or neuromuscular diseases, may be at an increased risk with lower velocity mechanisms.
Any physical examination for cervical trauma should commence with assessing the ABCs—airway, breathing, and circulation. If tracheal intubation is necessary, it should be performed with manual in-line stabilization to prevent displacement of fractures or dislocations. A comprehensive neurological assessment should follow, beginning with the Glasgow Coma Scale (GCS).[9] Evaluation of all other traumatic injuries to organs should be prioritized according to the Advanced Trauma Life Support (ATLS) protocol.
The physical examination should be comprehensive, noting any axial neck pain or external signs of cervical spine trauma. A thorough neurological assessment should be conducted, including evaluation of cranial nerves and a complete sensory and motor examination of the upper and lower extremities. Additionally, a rectal exam and assessment of the bulbocavernosus reflex are recommended for patients showing signs of neurologic shock.
C1 fractures typically manifest with axial neck pain without initial signs of neurological dysfunction. However, due to their caudal location, cranial nerves in the medulla and pons are at risk when involved—cranial nerves VI to XII may result in their respective palsies. Fractures involving the C1/C2 transverse foramina may also lead to blunt vertebral artery injury, resulting in basilar insufficiency. Therefore, a comprehensive cranial neurological examination should be conducted.
Evaluation
Gehweiler type 3 classification of C1 fractures is the most commonly observed subtype of atlas fracture.[4]
The Rule of Spence demonstrates that lateral mass displacement (LMD) exceeding 6.9 mm on open-mouth radiographs correlates with TAL rupture.[10][11]. LMD greater than 8.1 mm exhibits high sensitivity and specificity for TAL injury.[12] Another significant indicator is the widening of the anterior atlanto-dental interval to more than 3 mm in adults and 5 mm in children on functional lateral x-rays.[11] In addition, a C1:C2 ratio of more than 1.10 on plain radiographs has been observed to have high sensitivity in detecting concurrent transverse ligament injury.[13]
Cohorts with associated spine injuries, an increased atlanto-dental interval, and lateral mass displacement are at high risk of vertebral artery injury.[14] Evaluating the vascular anatomy in relation to C1 is of paramount importance.[15] Fractures involving the transverse process and lateral mass pose a significant risk of injury to the artery.[11]
Treatment / Management
Management Strategies for C1 Fractures
The following are the management strategies that outline surgical and nonoperative approaches for C1 fractures:
- Surgery as a primary option.
- Surgery as a secondary option after failed initial nonoperative management.
- Surgery involving the C1 level, with the main indication being a concomitant cervical spine fracture.
- Nonoperative management with external immobilization.[7]
The concomitant subaxial cervical injuries mostly dictate the indication for surgery.[4]
Gehweiler type 1, 2, 3b, or 5 fractures are typically stable and managed nonsurgically with the Minerva cast, Halo brace, or collar for an average period of 8.5 weeks.[16][8](B2)
Progressive diastasis at the fracture segment, as well as articular subluxation due to the lengthening of the TAL, may occur.[17] Lateral displacement of the lateral mass with subluxation of the occipital condyle can occur, which should be assessed through periodic follow-up imaging.[4][7] To distinguish between stable and unstable type 3 injuries, evaluating the integrity of the TAL with magnetic resonance imaging (MRI) is essential.[7]
Unstable atlas fractures (type 3b) with a moderately dislocated ligamentous bony avulsion of the TAL and sagittal split type 4 fractures may be treated by atlas osteosynthesis only.[11][8] Gehweiler type 4 fractures are preferentially managed by occipito-cervical instrumentation.[8](B3)
C1 and subaxial instrumentations can be performed through:
- Lateral mass
- C2 pars screw (less risk of vertebral injury)
- Transarticular (Magerl technique)
- Transpedicular/Pars (Goel and Harms technique)
- Translaminar screws placements
C1 lateral mass-C2 translaminar and C1 lateral mass-C2/3 transarticular (C1LM-C2TL and C1LM-C2/3TACL) fixation provides satisfactory atlantoaxial stabilization, as C1LM-C2 pedicular screw (Goel and Harms technique) is often not feasible due to anatomical constraints.[18] Sectioning or neurectomy of the C2 nerve root provides better visualization and minimizes operative time and blood loss. Furthermore, subsequent occipital numbness has not been found to significantly affect the quality of life.[19](B2)
The key anatomic landmarks for C1 lateral mass screw placement are mentioned below.
- Harms: At the inferior border of the posterior arch of C1 and the midpoint of the C1 lateral mass.[19]
- Goel: At the center of the posterior surface of the lateral mass, 1 to 2 mm cranial to the C1-C2 facet.[20] (B3)
In Goel's method, the screws are angled approximately 15 degrees medially and approximately 30 degrees cranially. On the other hand, the Harms' method requires no angulation.[20] Currently, no clear consensus exists on the ideal angulation and location.[20]
Neuronavigation facilitates accuracy and minimizes radiation exposure. However, the navigation system is costly, and a learning curve is associated with setup and utilization.[20]
Computed tomography (CT) evaluates the accuracy of free-hand C1 lateral mass screw placement as mentioned below.
- Type I (ideal): Screw threads completely within the bone.
- Type II (safe): Less than half the diameter of the screw violates the surrounding cortex.
- Type III (unacceptable): Clear violation of the transverse foramen or spinal canal.[21]
In a study, 97.2% of screws were rated as type I or II.[21] Among the 10 screws that were rated as unacceptable, there were no known associated neurological or vascular injuries.
Anatomical landmarks, ideal trajectories, and screw lengths are the most important determinants for accurate instrumentation.[21] The occipitocervical inclination can be effectively restored with the assistance of 3-dimensional–printed models.[22][23][24] There has been no observed difference in the safety or accuracy between the free-hand and navigated techniques for C2 pedicle and C2 pars screws.[25](A1)
Posterior atlantoaxial or occipitocervical fusion is the primary surgical technique, typically resulting in a reduced range of motion in the upper cervical spine post-operatively.[10][26] Transoral anterior C1-ring osteosynthesis via systems such as Jefferson-fracture reduction plate (JeRP) connotes good bone union while preserving C1–C2 motion.[27][28][29] This system also improves the integrity of the C0-C1-C2 and secondary stabilizers comprising the alar ligaments, facet capsule, and neck musculature while restoring the C0-C2 height.[10](B3)
The JeRP system is primarily indicated for unstable C1 fractures (Gehweiler type I/III) with or without TAL injury (Dickman type II).[10] Similarly, posterior C1-ring osteosynthesis is superior to C1-C2 fixation fusion in improving neck pain and movements.[30] In addition, this has been shown to significantly reduce operative time, intraoperative blood loss, radiation dose, length of hospital stay, and economic burden.[30](A1)
Differential Diagnosis
In the pediatric population, it is crucial to differentiate fractures of the C1 vertebra from unfused ossification centers.[31] An immature atlas typically develops 3 ossification centers—one for the anterior ring and one for each posterior neural arch—which appear by 1 year of age. The connection between the anterior and posterior arches comprises neurocentral synchondrosis, which fuses by age 7. The posterior arch usually closes by age 3 in an individual. These unfused ossification centers can mimic fractures and should be considered whenever children are aged 6 or younger and present with cervical spine trauma.
Prognosis
The overall prognosis of C1 fractures is favorable, with conservative management and external immobilization typically providing adequate fracture healing. C1 fractures are associated with a very low incidence of neurological deficit, as the fracture fragments tend to be outwardly displaced rather than encroach on the neural canal. The spinal canal is also very spacious at this level. The prognosis and healing of these fractures are primarily determined by associated bony and ligament injuries, particularly involving the transverse ligament
Complications
Complications of Osteosynthesis
- Reducing fractures within a deep and narrow space during the transoral approach can be cumbersome.
- The end of the lateral mass screw may damage the posterior pharyngeal wall, increasing the risk of wound complications or causing postoperative dysphagia.[26]
Complications of Posterior Instrumentation
- Egress of cerebrospinal fluid following unintended durotomies
- Epidural and subdural cerebellar hematomas
- Injury to the vertebral artery and internal carotid artery
- Substantial bleeding from venous plexus between C1 and C2
- Venous air embolism
- Hardware complications and pseudoarthrosis [32]
Revision surgery was required in approximately 6% of cases, primarily due to surgical-site infection and instability.[4]
A study reported an all-cause 30-day mortality rate of 12.2%.[4] A higher Charlson Comorbidity Index and older age are associated with increased mortality, whereas a concomitant C2 fracture was associated with improved survival.[6]
Postoperative and Rehabilitation Care
After applying a halo device, regular x-rays are required to ensure the fracture is healing.[33] The halo is often required for 8 to 16 weeks, depending on the rate of healing. Once the halo is removed, a collar is placed, and the patient should be enrolled in a rehabilitation program to regain muscle strength.
Deterrence and Patient Education
Most C1 fractures are generally managed conservatively with some form of external immobilization. Patients should be aware of the need for regular follow-up as advised by medical personnel and the possibility of requiring surgical intervention if conservative treatment fails. Smoking can hinder fracture healing and should be strictly avoided. Strict compliance with the collar is also recommended to ensure proper fracture healing.
Enhancing Healthcare Team Outcomes
C1 fractures are relatively common following trauma and can affect patients of all ages. As these fractures can be life-threatening, therefore, all healthcare personnel in the emergency department or trauma team must be aware of their presentation and management. Although a neurosurgeon or orthopedic spine surgeon usually manages the primary pathology, the aftercare is generally performed by nursing staff and physiotherapists, operating as part of an interprofessional healthcare team.
When promptly treated, isolated C1 fractures generally have a favorable outcome. Small case series indicate favorable outcomes even after anterior plate fixation, with patients often returning to their pre-injury status. However, outcomes are more guarded for older adults and young males, who often suffer from multiorgan injuries and require intubation and admission to the intensive care unit. Even after discharge, some of these individuals may have residual neurological deficits.[34][35]
Media
References
Forbes J, Das JM. Anatomy, Head and Neck: Atlantoaxial Joint. StatPearls. 2024 Jan:(): [PubMed PMID: 33085418]
Kaiser JT, Reddy V, Launico MV, Lugo-Pico JG. Anatomy, Head and Neck: Cervical Vertebrae. StatPearls. 2024 Jan:(): [PubMed PMID: 30969556]
Lyons JG, Mian HM. Epidemiology of atlas fractures in the United States: A 20-year analysis. Journal of craniovertebral junction & spine. 2022 Jan-Mar:13(1):85-93. doi: 10.4103/jcvjs.jcvjs_164_21. Epub 2022 Mar 9 [PubMed PMID: 35386248]
Fiedler N, Spiegl UJA, Jarvers JS, Josten C, Heyde CE, Osterhoff G. Epidemiology and management of atlas fractures. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2020 Oct:29(10):2477-2483. doi: 10.1007/s00586-020-06317-7. Epub 2020 Jan 30 [PubMed PMID: 32002697]
Cloney MB, El-Tecle N, Dahdaleh NS. Traumatic atlas fracture patients comprise two subpopulations with distinct demographics and mechanisms of injury. Clinical neurology and neurosurgery. 2022 Oct:221():107414. doi: 10.1016/j.clineuro.2022.107414. Epub 2022 Aug 17 [PubMed PMID: 35987045]
Matthiessen C, Robinson Y. Epidemiology of atlas fractures--a national registry-based cohort study of 1,537 cases. The spine journal : official journal of the North American Spine Society. 2015 Nov 1:15(11):2332-7. doi: 10.1016/j.spinee.2015.06.052. Epub 2015 Jun 29 [PubMed PMID: 26133259]
Level 3 (low-level) evidenceYlönen H, Danner N, Jyrkkänen HK, Kämäräinen OP, Leinonen V, Huttunen J. Surgically Treated C1 Fractures: A Population-Based Study. World neurosurgery. 2021 Oct:154():e333-e342. doi: 10.1016/j.wneu.2021.07.046. Epub 2021 Jul 17 [PubMed PMID: 34284160]
Laubach M, Pishnamaz M, Scholz M, Spiegl U, Sellei RM, Herren C, Hildebrand F, Kobbe P. Interobserver reliability of the Gehweiler classification and treatment strategies of isolated atlas fractures: an internet-based multicenter survey among spine surgeons. European journal of trauma and emergency surgery : official publication of the European Trauma Society. 2022 Feb:48(1):601-611. doi: 10.1007/s00068-020-01494-y. Epub 2020 Sep 12 [PubMed PMID: 32918554]
Level 3 (low-level) evidenceJain S, Iverson LM. Glasgow Coma Scale. StatPearls. 2024 Jan:(): [PubMed PMID: 30020670]
Ma W, Xu N, Hu Y, Li G, Zhao L, Sun S, Jiang W, Liu G, Gu Y, Liu J. Unstable atlas fracture treatment by anterior plate C1-ring osteosynthesis using a transoral approach. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2013 Oct:22(10):2232-9. doi: 10.1007/s00586-013-2870-x. Epub 2013 Jun 18 [PubMed PMID: 23775293]
Level 3 (low-level) evidenceKandziora F, Scholz M, Pingel A, Schleicher P, Yildiz U, Kluger P, Pumberger M, Korge A, Schnake KJ, Spine Section of the German Society for Orthopaedics and Trauma. Treatment of Atlas Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global spine journal. 2018 Sep:8(2 Suppl):5S-11S. doi: 10.1177/2192568217726304. Epub 2018 Sep 7 [PubMed PMID: 30210964]
Eun J, Oh Y. The relationship between radiologic parameters and transverse atlantal ligament injury obtained from MRI scans in patients with an isolated atlas burst fracture: A retrospective observational study. Medicine. 2021 Dec 10:100(49):e28122. doi: 10.1097/MD.0000000000028122. Epub [PubMed PMID: 34889272]
Level 2 (mid-level) evidenceLin P, Chuang TC, Baker JF. C1:C2 ratio is a potential tool assessing atlas fracture displacement and transverse ligament injury. Journal of craniovertebral junction & spine. 2019 Jul-Sep:10(3):139-144. doi: 10.4103/jcvjs.JCVJS_59_19. Epub [PubMed PMID: 31772425]
Cloney M, Kim H, Riestenberg R, Dahdaleh NS. Risk Factors for Transverse Ligament Disruption and Vertebral Artery Injury Following an Atlas Fracture. World neurosurgery. 2021 Feb:146():e1345-e1350. doi: 10.1016/j.wneu.2020.11.172. Epub 2020 Dec 9 [PubMed PMID: 33309644]
Rusconi A, Peron S, Roccucci P, Stefini R. The internal carotid artery and the atlas: anatomical relationship and implications for C1 lateral mass fixation. Surgical and radiologic anatomy : SRA. 2021 Jan:43(1):87-92. doi: 10.1007/s00276-020-02537-0. Epub 2020 Jul 30 [PubMed PMID: 32734343]
Tomaszewski R, Sesia SB, Studer D, Rutz E, Mayr JM. Conservative treatment and outcome of upper cervical spine fractures in young children: A STROBE-compliant case series. Medicine. 2021 Apr 2:100(13):e25334. doi: 10.1097/MD.0000000000025334. Epub [PubMed PMID: 33787631]
Level 2 (mid-level) evidenceStarnoni D, Ecker T, Barges-Coll J. Navigation-Assisted Posterior Open Reduction and Internal Fixation in a C-CLAMP Fashion for an Isolated C1 Fracture. Journal of neurological surgery. Part B, Skull base. 2021 Feb:82(Suppl 1):S61-S62. doi: 10.1055/s-0040-1701692. Epub 2020 Mar 20 [PubMed PMID: 33692933]
Du YQ, Li T, Ma C, Qiao GY, Yin YH, Yu XG. Biomechanical evaluation of two alternative techniques to the Goel-Harms technique for atlantoaxial fixation: C1 lateral mass-C2 bicortical translaminar screw fixation and C1 lateral mass-C2/3 transarticular screw fixation. Journal of neurosurgery. Spine. 2020 Jan 17:32(5):682-688. doi: 10.3171/2019.11.SPINE191178. Epub 2020 Jan 17 [PubMed PMID: 31952043]
Level 2 (mid-level) evidenceConroy E, Laing A, Kenneally R, Poynton AR. C1 lateral mass screw-induced occipital neuralgia: a report of two cases. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2010 Mar:19(3):474-6. doi: 10.1007/s00586-009-1178-3. Epub 2009 Oct 25 [PubMed PMID: 19856190]
Level 3 (low-level) evidenceButt BB, Gagnet P, Piche J, Patel R, Park P, Aleem IS. Lateral mass screw placement in the atlas: description of a novel surgical technique, radiographic parameters, and review of the literature. Journal of spine surgery (Hong Kong). 2021 Sep:7(3):335-343. doi: 10.21037/jss-20-566. Epub [PubMed PMID: 34734138]
Hu Y, Kepler CK, Albert TJ, Yuan ZS, Ma WH, Gu YJ, Xu RM. Accuracy and complications associated with the freehand C-1 lateral mass screw fixation technique: a radiographic and clinical assessment. Journal of neurosurgery. Spine. 2013 Apr:18(4):372-7. doi: 10.3171/2013.1.SPINE12724. Epub 2013 Feb 1 [PubMed PMID: 23373564]
Rajasekaran S, Soundararajan DCR, Shetty AP, Kanna RM. Motion-Preserving Navigated Primary Internal Fixation of Unstable C1 Fractures. Asian spine journal. 2020 Aug:14(4):466-474. doi: 10.31616/asj.2019.0189. Epub 2020 Feb 14 [PubMed PMID: 32050311]
Barrenechea IJ, Márquez L, Bruna AE. Unilateral C1 split fracture osteosynthesis using a patient-specific three-dimensional-printed guide: Technique report. Journal of craniovertebral junction & spine. 2021 Oct-Dec:12(4):437-439. doi: 10.4103/jcvjs.jcvjs_76_21. Epub 2021 Dec 11 [PubMed PMID: 35068828]
Wu C, Deng JY, Li T, Zeng BF, Hu HG, Zhu YF, Wei Q. 3D-Printed Screw-Rod Auxiliary System for Unstable Atlas Fractures: A Retrospective Analysis. Orthopaedic surgery. 2021 May:13(3):1006-1015. doi: 10.1111/os.13015. Epub 2021 Apr 7 [PubMed PMID: 33826254]
Level 2 (mid-level) evidenceAzimi P, Yazdanian T, Benzel EC, Aghaei HN, Azhari S, Sadeghi S, Montazeri A. Accuracy and safety of C2 pedicle or pars screw placement: a systematic review and meta-analysis. Journal of orthopaedic surgery and research. 2020 Jul 20:15(1):272. doi: 10.1186/s13018-020-01798-0. Epub 2020 Jul 20 [PubMed PMID: 32690035]
Level 1 (high-level) evidenceZou X, Ouyang B, Ma X, Chen Y, Ge S, Zhang S, Ni L, Xia H, Wu Z. [Progress in treatment of unstable atlas fracture]. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi = Chinese journal of reparative and reconstructive surgery. 2020 Jun 15:34(6):793-796. doi: 10.7507/1002-1892.201909129. Epub [PubMed PMID: 32538574]
Zou X, Ouyang B, Wang B, Yang H, Ge S, Chen Y, Ni L, Zhang S, Xia H, Wu Z, Ma X. Motion-preserving treatment of unstable atlas fracture: transoral anterior C1-ring osteosynthesis using a laminoplasty plate. BMC musculoskeletal disorders. 2020 Aug 12:21(1):538. doi: 10.1186/s12891-020-03575-w. Epub 2020 Aug 12 [PubMed PMID: 32787814]
Tu Q, Chen H, Li Z, Chen Y, Xu A, Zhu C, Huang X, Ma X, Wang J, Zhang K, Yin Q, Xu J, Xia H. Anterior reduction and C1-ring osteosynthesis with Jefferson-fracture reduction plate (JeRP) via transoral approach for unstable atlas fractures. BMC musculoskeletal disorders. 2021 Aug 30:22(1):745. doi: 10.1186/s12891-021-04628-4. Epub 2021 Aug 30 [PubMed PMID: 34461878]
Shin JW, Suk KS, Kim HS, Yang JH, Kwon JW, Lee HM, Moon SH, Lee BH, Park SJ, Park SR, Kim SK. Direct Internal Fixation for Unstable Atlas Fractures. Yonsei medical journal. 2022 Mar:63(3):265-271. doi: 10.3349/ymj.2022.63.3.265. Epub [PubMed PMID: 35184429]
Yan L, Du J, Yang J, He B, Hao D, Zheng B, Yang X, Hui H, Liu T, Wang X, Guo H, Chen J, Wang S, Ma S, Dong S. C1-ring osteosynthesis versus C1-2 fixation fusion in the treatment of unstable atlas fractures: a multicenter, prospective, randomized controlled study with 5-year follow-up. Journal of neurosurgery. Spine. 2022 Aug 1:37(2):157-165. doi: 10.3171/2021.12.SPINE211063. Epub 2022 Feb 11 [PubMed PMID: 35148517]
Level 1 (high-level) evidenceJunewick JJ, Chin MS, Meesa IR, Ghori S, Boynton SJ, Luttenton CR. Ossification patterns of the atlas vertebra. AJR. American journal of roentgenology. 2011 Nov:197(5):1229-34. doi: 10.2214/AJR.10.5403. Epub [PubMed PMID: 22021519]
Macki M, Hamilton T, Pawloski J, Chang V. Occipital fixation techniques and complications. Journal of spine surgery (Hong Kong). 2020 Mar:6(1):145-155. doi: 10.21037/jss.2019.12.01. Epub [PubMed PMID: 32309653]
Koutsogiannis P, Weisbrod LJ, Dowling TJ. Halo Brace. StatPearls. 2024 Jan:(): [PubMed PMID: 32491478]
Bhimani AD, Chiu RG, Esfahani DR, Patel AS, Denyer S, Hobbs JG, Mehta AI. C1-C2 Fusion Versus Occipito-Cervical Fusion for High Cervical Fractures: A Multi-Institutional Database Analysis and Review of the Literature. World neurosurgery. 2018 Nov:119():e459-e466. doi: 10.1016/j.wneu.2018.07.182. Epub 2018 Jul 30 [PubMed PMID: 30071333]
Purvis TE, De la Garza-Ramos R, Abu-Bonsrah N, Goodwin CR, Groves ML, Ain MC, Sciubba DM. External fixation and surgical fusion for pediatric cervical spine injuries: Short-term outcomes. Clinical neurology and neurosurgery. 2018 May:168():18-23. doi: 10.1016/j.clineuro.2018.02.005. Epub 2018 Feb 5 [PubMed PMID: 29505977]