Anatomy, Bony Pelvis and Lower Limb: Thigh Femoral Nerve
Anatomy, Bony Pelvis and Lower Limb: Thigh Femoral Nerve
Introduction
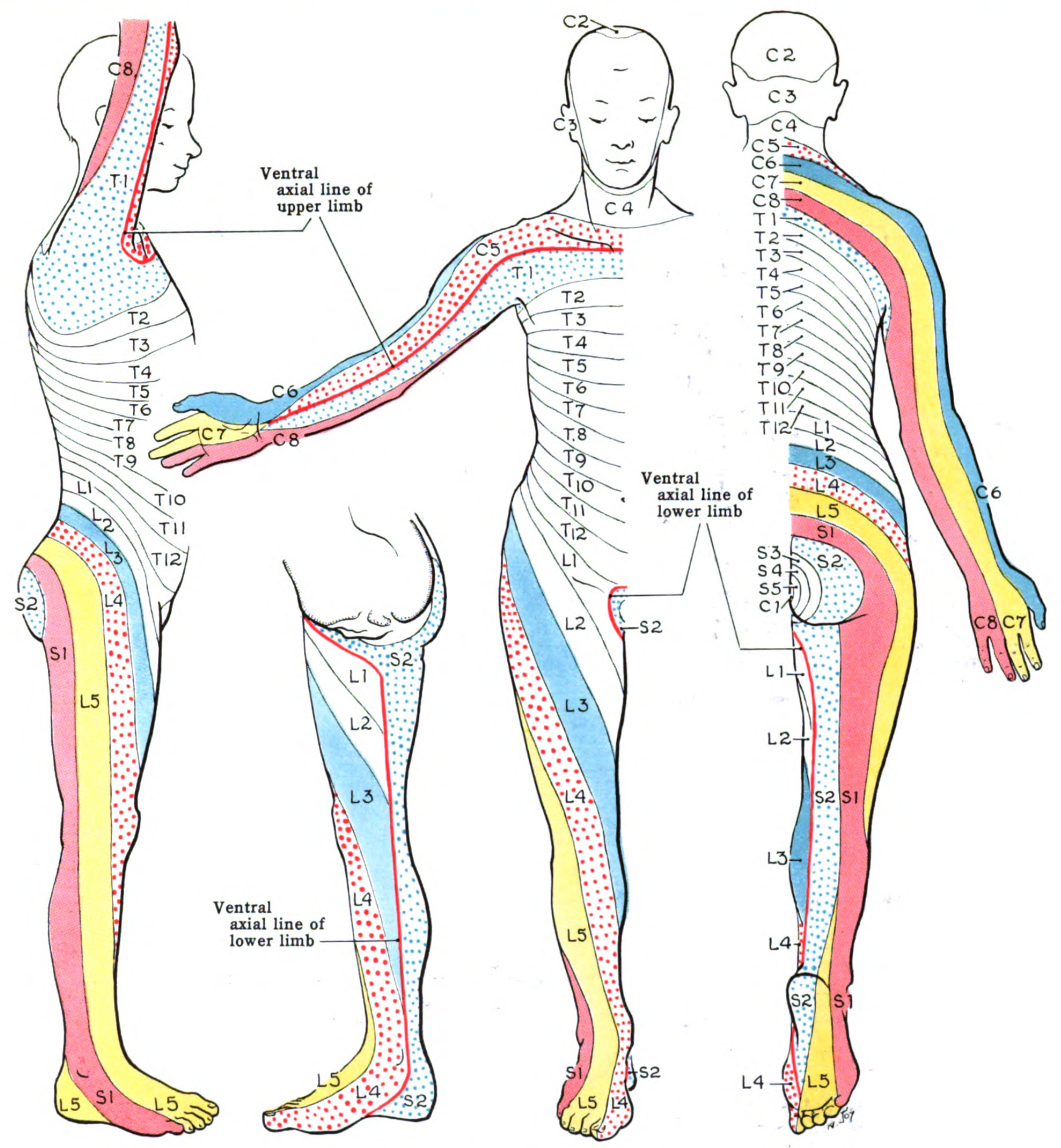
The femoral nerve is the largest nerve of the lumbar plexus. It forms from the dorsal divisions of the L2-L4 ventral rami.[1] It has a role in motor and sensory processing in the lower limbs. As a result, it controls the major hip flexor muscles, as well as knee extension muscles. It also controls sensation over the anterior and medial thigh and the medial leg down to the hallux (big toe). Therefore, it has several branches as it originates in the lumbar spine, down into the pelvis, and further down into the lower limbs.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
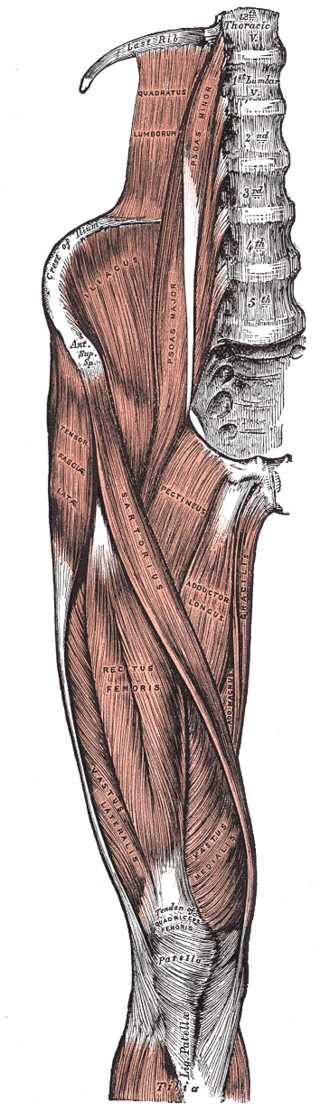
In the Abdomen
The femoral nerve begins its course in the abdomen by passing through the psoas major muscle. It then traverses laterally to the distal part of the psoas major muscle, and finally, it is "sandwiched" between the iliacus muscle and the psoas major muscle.[2] The iliacus muscle lies inferior to the femoral nerve, and the psoas major muscle is superior to the femoral nerve. The femoral nerve supplies the iliacus muscle. Because the psoas major muscle is located medial to the union of the ventral rami to form the femoral nerve, the psoas major is innervated by the ventral rami of L2-L4. These muscles will flex the thigh at the hip. Weakness of the iliopsoas muscle will cause difficulty in flexing the thigh to go upstairs.
In the Pelvis
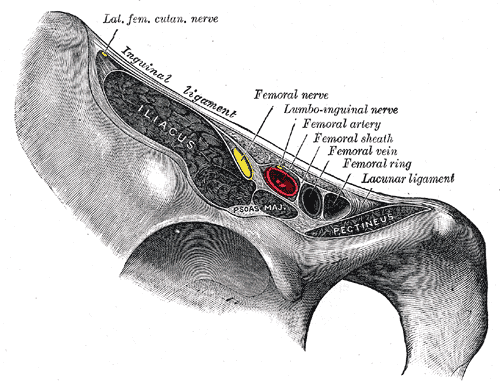
The femoral nerve then enters the thigh. To do so, it must enter the femoral triangle by running inferior to the inguinal ligament. The femoral triangle is formed by three structures: sartorius (laterally), adductor longus (medially), and the inguinal ligament (superiorly).[3] The contents of the femoral triangle include the femoral nerve, femoral artery, femoral vein, femoral canal, and lymphatic vessels (in order from most lateral to medial).[4] A memory aid to remember the order of the structures is NAVEL from lateral to medial. N = femoral nerve; A = femoral artery; V = femoral vein; EL = empty space with lymphatics (femoral canal with lymph node of Cloquet). About 4 cm below the inguinal ligament, the femoral nerve then divides into anterior and posterior divisions. The two divisions of the femoral nerve are distinguishable because the lateral femoral cutaneous artery splits them.[5]
Anterior Division
The anterior division of the femoral nerve has four terminal branches, two motor and two sensory. The motor branches are the nerve to the pectineus and the nerve to the sartorius. These muscles help to flex the thigh at the hip as well. The pectineus muscle is a
The sensory branches of the anterior division are the medial cutaneous nerve of the thigh and the intermediate cutaneous nerve of the thigh. These nerves are collectively responsible for the anteromedial sensory innervation of the thigh.
Posterior Division
The posterior division of the femoral nerve has a sensory nerve, four motor branches, and nerves to the hip and knee joints (articular branches). The sensory nerve is called the saphenous nerve and is the largest cutaneous branch of the femoral nerve. It is responsible for sensory innervation along the anteromedial and posteromedial aspects of the leg into the medial foot.[6] The femoral nerve becomes the saphenous nerve when it passes through the adductor canal. It continues to travel along the medial aspect of the tibia until about halfway down the tibia, where it finally divides into two branches. One branch is more posterior and ends at the ankle. The other branch is more anterior and continues along the medial aspect of the foot and terminates at the hallux.
The four motor branches of the posterior division of the femoral nerve are nerves to the rectus femoris, vastus medialis, vastus intermedius, and vastus lateralis. These muscles are the principal extensors of the leg at the knee and collectively form the quadriceps femoris muscle.
Lastly, branches from the posterior division of the femoral nerve also supply the knee and hip joints, termed articular joint nerves. The nerve to the rectus femoris supplies the hip, while all three nerves supply the knee joint as well as innervating the vastus medialis, vastus intermedius, and vastus lateralis. The articular nerves innervate the fibrous capsule, ligaments, and synovial membranes of the joints, following Hilton's law. Hilton's law is named for the English surgeon Dr. John Hilton, who noted that the nerve innervating the muscles which act on a joint also innervates the joint itself and often the skin over the joint as well.[7]
Blood Supply and Lymphatics
The femoral nerve travels with the femoral artery, vein, and lymphatics in the femoral triangle. The femoral artery and some of its branches supply the femoral nerve and its branches with oxygenated blood to maintain its function.
Nerves
Branches to the psoas major from L2-L4. These technically do not belong to the femoral nerve because they arise before the ventral rami of L2, L3, and L4 unite to form the femoral nerve
The nerve to the iliacus
Anterior Division
- Motor:
- The nerve to the sartorius
- The nerve to the pectineus
- Sensory:
- The medial cutaneous nerve of the thigh
- The intermediate cutaneous nerve of the thigh
Posterior Division
- Motor:
- The nerve to the rectus femoris
- The nerve to the vastus medialis
- The nerve to the vastus lateralis
- The nerve to the vastus intermedius
- Articular:
- Hip - supplied by the nerve to the rectus femoris
- Knee - supplied by the nerve to the vastus medialis, nerve to the vastus intermedius, and the nerve to the vastus lateralis
- Sensory:
- Saphenous nerve
- Infrapatellar branches to the knee
Muscles
Psoas major - The principal flexor of the thigh at the hip. It has a role in maintaining the body in an erect posture during standing. It arises laterally from the T12-L5 vertebrae. It inserts with the iliacus onto the lesser trochanter of the femur.
Iliacus - Another principal flexor of the thigh at the hip. It arises from the iliac fossa and crest and the ala of the sacrum. It Inserts with the psoas major onto the lesser trochanter of the femur.
Sartorius - Flexes, abducts, and laterally rotates the thigh at the hip. It can also flex and medially rotate the leg at the knee. It can also flex the leg at the knee joint. The sartorius arises from the anterior superior iliac spine. It inserts onto the medial surface of the tibia. At its insertion, the tendon of the sartorius joins with that of the gracilis and semitendinosus to form the pes anserinus (Latin - goose's foot). A goose's foot has three toes joined by a web. The sartorius is named from the Latin word for tailor - sartor. Tailors sit on the floor with the thigh abducted and medially rotated at the hip and the leg flexed at the knee.
Pectineus - Flexes and adducts the thigh at the hip. It arises from the superior ramus of the pubic bone. It inserts into the pectineal line of the femur. Pecten is a Latin word for a comb, so named because the parallel fibers of the muscle at its insertion resemble the teeth of a comb.
Physiologic Variants
In a case study in Karnataka, India, researchers observed that in a 65-year-old male cadaver, the left femoral nerve had split in the abdomen when coming off the L2-L4 nerve roots. It then rejoined to form the femoral nerve just proximal to the inguinal canal.[8]
Surgical Considerations
Surgeons use the femoral artery for arterial access in many procedures, including aortic aneurysm repairs.[9] It is essential to identify the femoral nerve before doing such a procedure, as damage to the nerve can result in loss of function of any of the muscles innervated by the femoral nerve.
Researchers have found the branches to the rectus femoris to range between 1 and 4 branches, with the most common innervation pattern being two branches. As a result, it is important to be aware and identify the possible variants and landmarks of the different possible branches.[10]
When the great saphenous nerve is removed for use in cardiac bypass procedures, the saphenous nerve is also commonly removed, resulting in anesthesia over the medial leg as far distally as the medial malleolus. One should forewarn the patient, so they do not become frightened by the sudden appearance of loss of feeling in the distribution of the saphenous nerve.
Clinical Significance
Radiculopathy and Loss of Reflexes
Radicular pain is irritation or inflammation of a nerve root. This is usually due to disc herniation. The symptoms include pain that travels in a dermatomal fashion. Motor deficits, as well as sensory deficits, can occur due to disc herniations.[11] If a disc herniation occurs on the L4 spinal nerve root, one can also lose their patellar reflex because reflexes include an afferent and efferent limb, which are affected in radicular pain.
Femoral Hernia
Femoral hernias are less likely to occur than inguinal hernias; however, they are more likely to occur in elderly females. They are protrusions of abdominal contents through a weakening in the femoral canal. They create a bulge in the groin area and can lead to strangulation and necrosis of abdominal contents if not treated. Because the hernia sac is located in the femoral canal, the femoral vein will be located lateral to the hernia sac.[12]
Psoas Abscess/Hematoma
Any infection or hematoma can cause a mass effect injury near the psoas muscle or iliacus muscle. Due to the relationship of these muscles to the femoral nerve, the growing abscess or hematoma can begin to compress the femoral nerve. This can lead to nerve injury, potentially affecting motor or sensory innervation from the femoral nerve.[13]
Femoral and Saphenous Nerve Blocks
Femoral nerve blocks are common in the management of hip pain in hip fracture patients; this is because they avoid the side effects and addictive properties of opioids. The pericapsular nerve group (PENG) blocks target articular branches of the femoral nerve to alleviate pain in the hip.[14]
Femoral Nerve Damage
- The most common etiology is direct, sharp trauma.
- A compressive etiology can damage the nerve due to ischemia, such as hematoma or tumor.
- Iatrogenic injuries have been reported following intraabdominal operations and hip surgeries due to prolonged compression, retraction, or stretching of the nerve.[15]
- Proximal interlocking screw placement through femoral IM nailing can be a risk factor for iatrogenic injury of the femoral nerve.
- Although uncommon, femoral nerve neuropathy has been reported in complex anterior and posterior spinal surgery.[16]
Clinically, patients will have quadriceps wasting, loss of knee extension, and to a lesser extent, hip flexion due to the involvement of the iliacus and pectineus muscles. On the sensory side, there will be a loss of sensation over the anterior and medial thigh due to the involvement of the anterior and medial cutaneous nerves of the thigh. Furthermore, loss of sensation will occur over the medial aspect of the lower leg and foot due to the involvement of the saphenous nerve. Although the prognosis in most cases is satisfactory, some cases necessitate nerve repair or grafting, and some cases cause permanent residual neurologic deficits.
Femoral Neuropathy in Obstetric Patients Undergoing Vaginal Delivery
Femoral neuropathies may occur during vaginal delivery. Commonly, patients are put in the dorsal lithotomy position, in which the thigh is flexed at the hip, and the leg is flexed at the knee. This position compresses the femoral nerve against the inguinal ligament, compromising the blood supply to the nerve. At the end of the delivery, the patient attempts to stand and falls to the floor because the quadriceps femoris muscle is not functional due to the loss of its innervation by the femoral nerve. The quadriceps femoris muscle inserts onto the patella. The patellar ligament attaches to the tibial tuberosity. When the quadriceps femoris muscle contracts, it extends the leg at the knee. This action is crucial to prevent the leg from buckling. Thus, if one is assisting the patient in arising from a gurney after delivery, one must be able to catch the patient if she falls due to femoral neuropathy.[17]
An interesting variation is seen in patients who experience signs and symptoms that indicate femoral neuropathy. However, they also have other signs demonstrating this is not a true femoral neuropathy. For example, the patient appears to have not only femoral neuropathy but also a foot drop. The presence of foot drop indicates that this patient does not have a true femoral neuropathy but rather a lumbosacral plexopathy. This condition is also associated with a difficult delivery.[17]
Femoral Neuropathy caused by Surgical Treatment of the Fracture of the Patella
The surgical repair of a patellar fracture can cause femoral neuropathy.[18]
Testing the Femoral Nerve
The femoral nerve can be tested by the following procedure. The patient is placed in a prone position. The leg is flexed at the knee, and the examiner raises the leg (Reverse Lasegue test). Hyperextension of the hip with the leg flexed at the knee causes stretching of the femoral nerve with consequent pain.
Testing the Patellar Tendon Reflex
The patellar tendon reflex is tested by tapping the patellar tendon with a reflex hammer, causing a reflex contraction of the quadriceps femoris muscle. This reflex involves the femoral nerve and the L2-L4 ventral primary rami. The muscle spindle fibers of the quadriceps femoris are stimulated by tapping the patellar tendon. They cause activation of sensory axons that have their cell bodies in the dorsal root ganglia from L2-L4 because they are innervated by the femoral nerve. The central processes of the cells of the dorsal root ganglia enter the spinal cord by the dorsal roots and then pass to the alpha-motor neurons of the ventral horn of the spinal cord. Stimulation of these neurons, whose axons are located in the femoral nerve, causes contraction of the quadriceps femoris muscle. This reflex is involved in maintaining tone in the quadriceps femoris muscle. The activity in this circuit can be modulated by neurons from higher influences.
Reasons for performing a patellar tendon reflex
Decreased Patellar Tendon Reflex. Diseases of the lower motor neurons connecting the ventral horn of the spinal cord to the quadriceps femoris muscle may take several forms. For example, poliomyelitis is an infection by a virus that attacks and kills the alpha-motor neurons of the spinal cord. This can result in paralysis and death of the lower limb muscles, including the quadriceps femoris muscle. In this case, the result is a lower motor neuron syndrome. Damage to the femoral nerve (femoral neuropathy) from various causes ranging from trauma to poliomyelitis to a spinal cord injury will cause decreased or absent patellar tendon reflexes (hyporeflexia).
Increased patellar tendon reflexes may be seen in cerebrovascular accidents (strokes). Here the neurons that run in the pathway from the motor cortex to the corticospinal tracts to the alpha-motor neurons are damaged or destroyed. This causes weakness (paresis) or frank paralysis (plegia). In addition, there are suppressor fibers that run with the lateral corticospinal tracts to the alpha-motor neurons. These neurons suppress the patellar tendon reflex. In the presence of a brain injury due to trauma or stroke, the loss of the suppressor neurons causes hyperreflexia (increased deep tendon reflexes).[19][20]
Other Issues
Diabetes mellitus can cause peripheral neuropathies. One of the more common variants is termed diabetic lumbosacral radiculoplexus neuropathy. In this case, the patient appears to have femoral neuropathy but has other signs and symptoms that indicate that this is not a true femoral neuropathy, even though it has signs and symptoms consistent with a femoral neuropathy. As with the case above of vaginal delivery, the other symptoms are not consistent with true femoral neuropathy.[21][22][23][24]
Media
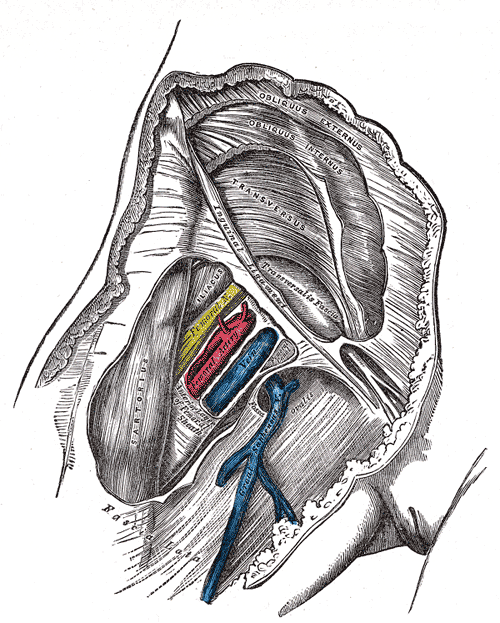
(Click Image to Enlarge)
Right Hip and Femoral Muscles, Anterior View. This illustration shows the tensor fasciae latae, thoracic vertebrae, quadratus lumborum, psoas minor and major, crest of ilium, anterior superior iliac spine, iliacus, sartorius, pectineus, adductor longus, gracilis, adductor magnus, rectus femoris, vastus lateralis and medialis, tibia, patella, and quadriceps tendon.
Henry Vandyke Carter, Public domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
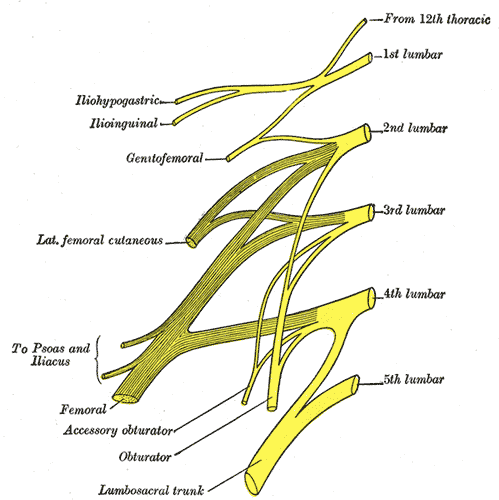
Nerve Roots L2-L4 Jointo Form the Femoral Nerve
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Wong TL, Kikuta S, Iwanaga J, Tubbs RS. A multiply split femoral nerve and psoas quartus muscle. Anatomy & cell biology. 2019 Jun:52(2):208-210. doi: 10.5115/acb.2019.52.2.208. Epub 2019 Jun 30 [PubMed PMID: 31338239]
Jakubowicz M. Topography of the femoral nerve in relation to components of the iliopsoas muscle in human fetuses. Folia morphologica. 1991:50(1-2):91-101 [PubMed PMID: 1844583]
Basinger H, Hogg JP. Anatomy, Abdomen and Pelvis: Femoral Triangle. StatPearls. 2023 Jan:(): [PubMed PMID: 31082184]
Clar DT, Bordoni B. Anatomy, Abdomen and Pelvis: Femoral Region. StatPearls. 2023 Jan:(): [PubMed PMID: 30860736]
Orebaugh SL. The femoral nerve and its relationship to the lateral circumflex femoral artery. Anesthesia and analgesia. 2006 Jun:102(6):1859-62 [PubMed PMID: 16717338]
Mathew K, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Saphenous Nerve, Artery, and Vein. StatPearls. 2023 Jan:(): [PubMed PMID: 31082089]
Hébert-Blouin MN, Tubbs RS, Carmichael SW, Spinner RJ. Hilton's law revisited. Clinical anatomy (New York, N.Y.). 2014 May:27(4):548-55. doi: 10.1002/ca.22348. Epub 2013 Nov 22 [PubMed PMID: 24272922]
Ashwini LS, Somayaji SN, Rao M, Marpalli S. Preinguinal Splitting and Reunion of Femoral Nerve Entrapping the Fleshy Fibres of Iliacus Muscle - A Case Report. Journal of clinical and diagnostic research : JCDR. 2017 Apr:11(4):AD01-AD02. doi: 10.7860/JCDR/2017/24214.9685. Epub 2017 Apr 1 [PubMed PMID: 28571125]
Level 3 (low-level) evidenceAvraham E, Natour M, Obaid W, Karmeli R. Superficial femoral artery access for endovascular aortic repair. Journal of vascular surgery. 2020 May:71(5):1538-1545. doi: 10.1016/j.jvs.2019.07.081. Epub 2019 Nov 4 [PubMed PMID: 31699510]
Plante D, Janelle N, Angers-Goulet M, Corbeil P, Takech MA, Belzile EL. Anatomical variants of the rectus femoris motor innervation. Journal of hip preservation surgery. 2019 Jul:6(2):170-176. doi: 10.1093/jhps/hnz026. Epub 2019 Jun 20 [PubMed PMID: 31660203]
Alexander CE, Varacallo M. Lumbosacral Radiculopathy. StatPearls. 2023 Jan:(): [PubMed PMID: 28613587]
Goethals A, Azmat CE, Adams CT. Femoral Hernia. StatPearls. 2023 Jan:(): [PubMed PMID: 30571070]
Lorei MP, Hershman EB. Peripheral nerve injuries in athletes. Treatment and prevention. Sports medicine (Auckland, N.Z.). 1993 Aug:16(2):130-47 [PubMed PMID: 8378668]
Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A. Pericapsular Nerve Group (PENG) Block for Hip Fracture. Regional anesthesia and pain medicine. 2018 Nov:43(8):859-863. doi: 10.1097/AAP.0000000000000847. Epub [PubMed PMID: 30063657]
Hudson AR, Hunter GA, Waddell JP. Iatrogenic femoral nerve injuries. Canadian journal of surgery. Journal canadien de chirurgie. 1979 Jan:22(1):62-6 [PubMed PMID: 445241]
Level 3 (low-level) evidenceNaroji S, Belin LJ, Maltenfort MG, Vaccaro AR, Schwartz D, Harrop JS, Weinstein M. Vulnerability of the femoral nerve during complex anterior and posterior spinal surgery. The journal of spinal cord medicine. 2009:32(4):432-5 [PubMed PMID: 19777866]
Level 3 (low-level) evidenceBlack AC, Williams SE, Holt JA, Jackson M, Hawks K, Munakomi S. Foot Drop in Obstetrics. StatPearls. 2023 Jan:(): [PubMed PMID: 35881745]
Lee SH, Lee TJ, Woo MS, Kwon DG. Femoral nerve palsy with patella fracture. Knee surgery & related research. 2013 Dec:25(4):230-2. doi: 10.5792/ksrr.2013.25.4.230. Epub 2013 Nov 29 [PubMed PMID: 24369003]
Chandrasekhar A, Abu Osman NA, Tham LK, Lim KS, Wan Abas WA. Influence of age on patellar tendon reflex response. PloS one. 2013:8(11):e80799. doi: 10.1371/journal.pone.0080799. Epub 2013 Nov 18 [PubMed PMID: 24260483]
Steineman BD, Karra P, Park K. Assessment of Patellar Tendon Reflex Responses Using Second-Order System Characteristics. Applied bionics and biomechanics. 2016:2016():7172948. doi: 10.1155/2016/7172948. Epub 2016 Feb 14 [PubMed PMID: 27041981]
Glenn MD, Jabari D. Diabetic Lumbosacral Radiculoplexus Neuropathy (Diabetic Amyotrophy). Neurologic clinics. 2020 Aug:38(3):553-564. doi: 10.1016/j.ncl.2020.03.010. Epub [PubMed PMID: 32703468]
Llewelyn D, Llewelyn JG. Diabetic amyotrophy: a painful radiculoplexus neuropathy. Practical neurology. 2019 Apr:19(2):164-167. doi: 10.1136/practneurol-2018-002105. Epub 2018 Dec 8 [PubMed PMID: 30530723]
Bhanushali MJ, Muley SA. Diabetic and non-diabetic lumbosacral radiculoplexus neuropathy. Neurology India. 2008 Oct-Dec:56(4):420-5 [PubMed PMID: 19127036]
Younger DS. Diabetic lumbosacral radiculoplexus neuropathy: a postmortem studied patient and review of the literature. Journal of neurology. 2011 Jul:258(7):1364-7. doi: 10.1007/s00415-011-5938-8. Epub 2011 Feb 17 [PubMed PMID: 21327851]
Level 3 (low-level) evidence