Introduction
Airway management is of paramount importance in the operating room and critical care settings. Patients who are in respiratory distress or require general anesthesia typically need an advanced airway such as an endotracheal tube (ETT) or laryngeal mask airway (LMA) so that ventilatory support can be given. Failure to secure the airway during intubation can lead to catastrophic, possibly fatal, outcomes for the patient. Several assessment tools have been devised for the proceduralist to use to anticipate challenges during airway management.[1]
In this article, we will focus on the Mallampati score, a simple and quick tool to help the proceduralist evaluate the patient’s airway anatomy to assess the likelihood of challenges during airway manipulation.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The purpose of the human airway is to allow airflow during spontaneous and mechanical ventilation. It is divided into two main portions: the upper and lower airways. The upper airway includes the nasopharynx, oropharynx, and hypopharynx. The lower airway consists of the trachea, bronchi, bronchioles, and alveoli. The upper and lower airways are divided by the larynx, which is a key portion involved in sound production. The larynx includes two fundamental structures, namely the epiglottis and vocal cords.[2]
During endotracheal intubation, the proceduralist aims to pass the endotracheal tube through the upper airway and vocal cords into the trachea. When attempting an orotracheal approach to intubation, the endotracheal tube must pass through the structures in the oropharynx, including the base of the tongue, the palatine tonsils, tonsillar pillars, and uvula. If these structures are relatively large, the proceduralist may experience difficulty in laryngoscopy or intubation.
The Mallampati score is one assessment to describe the relative size of the base of the tongue compared to the oropharyngeal opening in hopes of predicting the difficult airway.
Indications
The Mallampati score should be used in circumstances when a patient requires any type of anesthesia or is to be intubated. This will enable the proceduralist to prepare for airway anatomy challenges in advance of securing the airway.
Contraindications
There are no absolute contraindications for this assessment tool. However, the score's usefulness can be diminished if the patient cannot fully cooperate with the exam.
Personnel
This tool is useful for physicians and advanced practice providers who commonly intubate patients.
Preparation
Induction of anesthesia is a crucial time when a patient is given sedation medications that decrease respiratory drive. After induction of anesthesia, the proceduralist must be able to ventilate the patient either through a mask or by placing an advanced airway (ETT or LMA) to maintain oxygenation and ventilation. While the overall majority of patients are relatively easy to mask, ventilate and intubate, about 1 to 5% of patients are difficult to mask, ventilate, and 5% of patients are difficult to intubate.[3][4][5][6]
According to the ASA Practice Guidelines, difficult mask ventilation is the inability to ventilate (as confirmed by end-tidal carbon dioxide). Difficult intubation requires multiple attempts or if tracheal intubation fails after multiple attempts.[7]
According to one closed claim analysis, 67% of difficult airway claims arose during the induction of anesthesia. Therefore the ability to predict and prepare for a patient who will be difficult to mask, ventilate or intubate can help avoid these adverse outcomes.[8]
Technique or Treatment
Over time, many different risk factors have been proposed with the intent of helping the proceduralist predict and prepare for challenges that may arise during the induction of anesthesia. One such tool is the Mallampati score. In 1983, Dr. Seshagiri Mallampati, an anesthesiologist, hypothesized that the size of the base of the tongue relative to the oropharyngeal cavity could predict difficult intubation.[9]
A relatively large tongue would mask the palatoglossal and palatopharyngeal arches and the uvula, while a relatively small tongue would not. To test this hypothesis, he enrolled 210 healthy adults undergoing direct laryngoscopy to undergo preoperative evaluation of the relative size of the tongue.
Each patient was seated and asked to open their mouth and maximally protrude the tongue without phonation. Patients were divided into one of three classes based on visible structures. These classes were:
- Class I - fully visualize the faucial pillars, soft palate, and uvula.
- Class II - full visualization of the faucial pillars and soft palate. Unable to visualize the uvula as it is obscured by the base of the tongue
- Class III - Only the soft palate could be visualized
Dr. Mallampati categorized difficult intubation as an intubation attempt that provided less than adequate exposure of the glottis during direct laryngoscopy. He found a significant correlation between this clinical sign (now better known as the Mallampati Score) and the intubation difficulty.[10]
Just two years after this publication, another team of Samson and Young added a fourth classification (now known as class IV) in which neither the faucial pillars, uvula, or soft palate could be visualized. On a larger scale, these researchers found that in all seven cases of difficult intubation among obstetric patients, each was either Mallampati class III or IV.[11]
In 1998, class 0 was introduced to describe the infrequent observation of any part of the epiglottis on a pharyngoscopic view. They claimed in all cases, endotracheal intubation was easy.[12][13] Based on these studies, Mallampati scoring became commonplace to use as a quick method of assessing and preparing for possible difficult intubation.
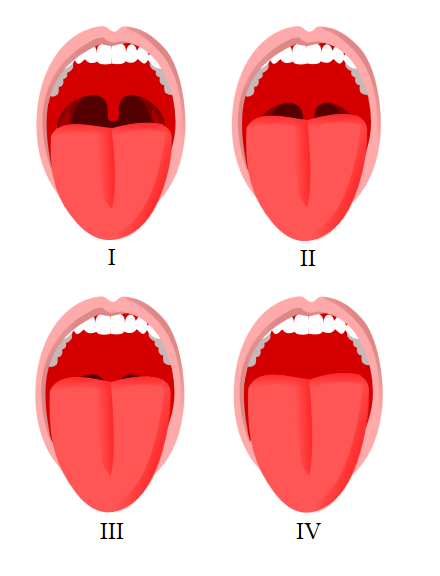
The modified Mallampati score used routinely today is as follows:
- Class 0: Any part of the epiglottis is visible
- Class I: soft palate, uvula, and pillars are visible
- Class II: soft palate and uvula are visible
- Class III: only the soft palate and base of the uvula are visible
- Class IV: only the hard palate is visible
To properly assess a patient's Mallampati score, the patient is seated in the upright position and opens their mouth while maximally protruding their tongue. Classically this exam is done without phonation.
Clinical Significance
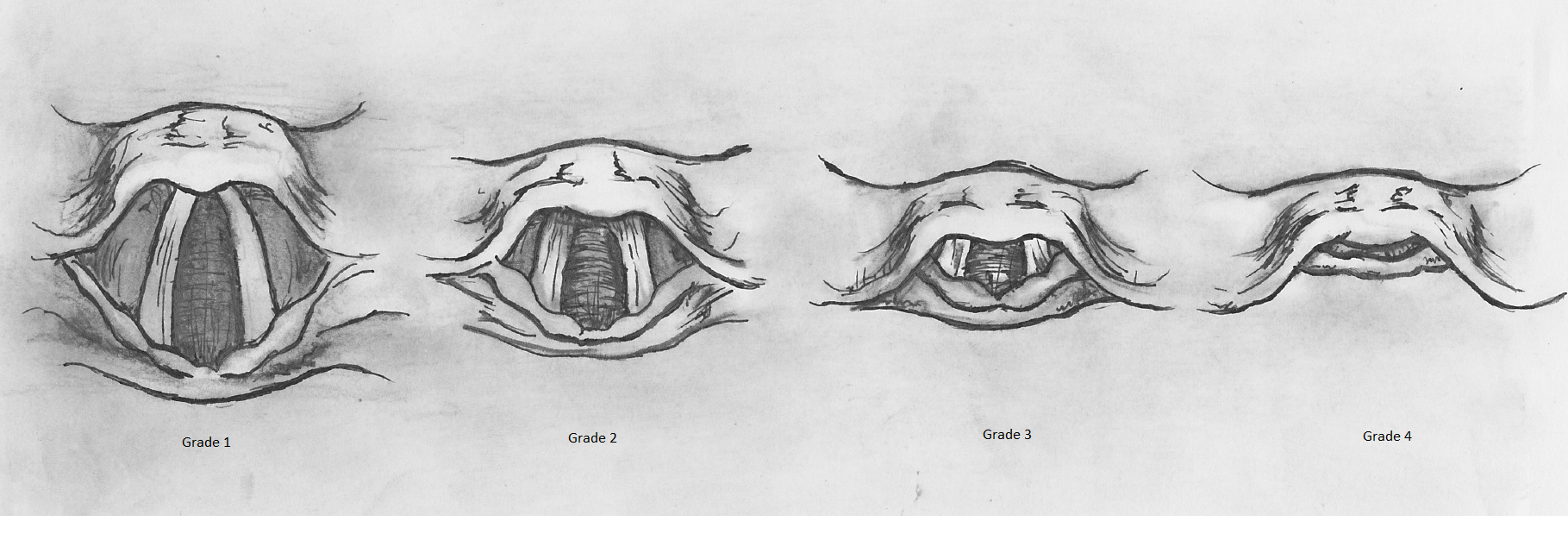
After its introduction in the 1980s, the Mallampati scoring system quickly became a routine preoperative physical exam to predict the difficult airway. Early studies concluded that Class III and IV could predict difficult intubation based on the laryngeal views as described in the original study.[10][11] However, the laryngeal views in Mallampati’s original study were inconsistent with the Cormack-Lehane grading system (described one year after his proposed sign), which is now most commonly used.[14]
One group argued that many of the views deemed ‘difficult’ by Mallampati could now be considered good based on this grading system. When placed in this context, they argue the positive predictive value is only 33.3% making the Mallampati scoring a poor predictor of difficult intubation.[15] Another study found that Mallampati class III only had a 22% positive predictive value.[16] A recent meta-analysis agrees that when used alone, Mallampati tests are limited in predicting the difficult airway.[17]
A 2016 Cochrane meta-analysis found the sensitivity and specificity of the modified Mallampati test in predicting difficult tracheal intubation to be 0.51 and 0.87. Therefore, the Mallampati test is a poor independent screening tool as it misses nearly half of all difficult airways but is fairly specific for ruling out a difficult airway.[18]
There are several other known risk factors associated with difficult endotracheal intubation, including a thick neck (>40 cm), limited neck mobility, small mouth opening (<3 finger breadths), short TMD (<6 cm), limited mandibular protrusion, and a history of a difficult airway. The proceduralist should consider all these factors when planning to intubate a patient. A routine preoperative exam includes assessment and documentation of many of these risk factors to help stratify patients to predict the difficult airway.
Mask ventilation is also a key element of airway management. The inability to ventilate a patient can lead to profound negative patient outcomes and mask ventilation is a significant branch point in the difficult airway algorithm between the emergent and non-emergent pathways. Therefore, the ability to predict and prepare for a patient who may be challenging to mask ventilate is important.
Several risk factors have been studied to predict difficult mask ventilation. Some of these include advanced age (>55 years), obesity (BMI >30kg/m^2), presence of a beard, lack of teeth, history of obstructive sleep apnea (OSA)/snoring, male sex, limited mandibular protrusion, short thyromental distance (TMD <6 cm), and Mallampati class 3 or 4. A large meta-analysis found that the Mallampati score had very low sensitivity in predicting difficult mask ventilation, to be 0.17.[3] Therefore, similar to predicting the difficult airway, the Mallampati score is a poor screening tool to predict difficult mask ventilation.
Of note, it has been observed that the Mallampati score can change during pregnancy. One study found that among a cohort of 242 pregnant patients, there was a 34% increase in the number of Mallampati grade IV cases at 38 weeks gestation compared to the same patients at 12 weeks gestation. The common belief behind this increase is that edema and fluid retention during pregnancy leads to higher scores.[19] Overall, the difficulty of intubation is not significantly greater in the pregnant population.[20] However, as pregnancy progresses, there can be a significant increase in Mallampati score in the same patient.
Obstructive sleep apnea (OSA) has also been correlated with Mallampati scores. OSA is the most common sleep-related breathing disorder. Relaxation of upper airway structures during sleep leads to upper airway occlusion. The Mallampati score has been proven to be an independent risk factor in predicting the presence and severity of OSA. For every one-point increase in the Mallampati score, there is a two-fold increase in the odds of having OSA. For every one-point increase in the Mallampati score, the apnea-hypopnea index increases on average by more than five events per hour.[21] Therefore, assessing a patient’s Mallampati score before polysomnography may be useful in the clinic setting to predict OSA.
Overall, several methods, including the Mallampati scoring system, have been proposed to predict whether a patient will have a difficult airway or will be difficult to mask ventilate. Through this literature review, the Mallampati score by itself is not sensitive in predicting difficult mask ventilation or intubation. Therefore, it is not recommended to be used on its own to help the proceduralist predict difficult airway management but rather as one of many clinical signs to aid in airway management decisions. The ability to predict the difficult airway continues to be challenging. One recent study found that 93% of difficult intubations were unanticipated, and 94% of difficult mask ventilation were unanticipated.[22] Therefore the proceduralist must be constantly vigilant and prepared for unanticipated difficult airway management in all circumstances.
Enhancing Healthcare Team Outcomes
Knowledge of risk factors for difficult mask ventilation and difficult intubation can help physicians and advanced practitioners who routinely perform endotracheal intubation prepare for and successfully secure the difficult airway. Involving other healthcare team members such as additional physicians, nurse anesthetists, anesthesia assistants, nursing staff, and respiratory therapists, when appropriate, can help aid the proceduralist in successful mask ventilation and/or endotracheal intubation.
When intubation is needed on a patient known to be difficult to intubate, the most experienced provider should make the initial attempt as multiple attempts can result in airway edema and decreases the likelihood of successful intubation. Successful oxygenation and ventilation can avoid adverse and potentially fatal outcomes.
Mallampati score, though a risk factor for difficult mask ventilation and endotracheal intubation, is not independently sufficient to predict the difficult airway.[18] [Level 1] Therefore, the Mallampati score should be combined with other known risk factors to best guide airway management.
Media
References
Mouri M, Krishnan S, Hendrix JM, Maani CV. Airway Assessment. StatPearls. 2025 Jan:(): [PubMed PMID: 29262092]
Ball M, Hossain M, Padalia D. Anatomy, Airway. StatPearls. 2025 Jan:(): [PubMed PMID: 29083624]
Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, Riou B. Prediction of difficult mask ventilation. Anesthesiology. 2000 May:92(5):1229-36 [PubMed PMID: 10781266]
Kheterpal S,Han R,Tremper KK,Shanks A,Tait AR,O'Reilly M,Ludwig TA, Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006 Nov; [PubMed PMID: 17065880]
Shiga T,Wajima Z,Inoue T,Sakamoto A, Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. Anesthesiology. 2005 Aug; [PubMed PMID: 16052126]
Level 1 (high-level) evidenceLundstrøm LH, Møller AM, Rosenstock C, Astrup G, Wetterslev J. High body mass index is a weak predictor for difficult and failed tracheal intubation: a cohort study of 91,332 consecutive patients scheduled for direct laryngoscopy registered in the Danish Anesthesia Database. Anesthesiology. 2009 Feb:110(2):266-74. doi: 10.1097/ALN.0b013e318194cac8. Epub [PubMed PMID: 19194154]
Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, Fiadjoe JE, Greif R, Klock PA, Mercier D, Myatra SN, O'Sullivan EP, Rosenblatt WH, Sorbello M, Tung A. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022 Jan 1:136(1):31-81. doi: 10.1097/ALN.0000000000004002. Epub [PubMed PMID: 34762729]
Level 1 (high-level) evidencePeterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW. Management of the difficult airway: a closed claims analysis. Anesthesiology. 2005 Jul:103(1):33-9 [PubMed PMID: 15983454]
Mallampati SR, Clinical sign to predict difficult tracheal intubation (hypothesis) Canadian Anaesthetists' Society journal. 1983 May; [PubMed PMID: 6336553]
Level 3 (low-level) evidenceMallampati SR,Gatt SP,Gugino LD,Desai SP,Waraksa B,Freiberger D,Liu PL, A clinical sign to predict difficult tracheal intubation: a prospective study. Canadian Anaesthetists' Society journal. 1985 Jul; [PubMed PMID: 4027773]
Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987 May:42(5):487-90 [PubMed PMID: 3592174]
Level 2 (mid-level) evidenceEzri T, Cohen I, Geva D, Szmuk P. Pharyngoscopic views. Anesthesia and analgesia. 1998 Sep:87(3):748 [PubMed PMID: 9728878]
Level 3 (low-level) evidenceEzri T, Warters RD, Szmuk P, Saad-Eddin H, Geva D, Katz J, Hagberg C. The incidence of class "zero" airway and the impact of Mallampati score, age, sex, and body mass index on prediction of laryngoscopy grade. Anesthesia and analgesia. 2001 Oct:93(4):1073-5, table of contents [PubMed PMID: 11574386]
Cormack RS,Lehane J, Difficult tracheal intubation in obstetrics. Anaesthesia. 1984 Nov; [PubMed PMID: 6507827]
O'Leary AM, Sandison MR, Roberts KW. History of anesthesia; Mallampati revisited: 20 years on. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2008 Apr:55(4):250-1. doi: 10.1007/BF03021512. Epub [PubMed PMID: 18378973]
Level 3 (low-level) evidenceTse JC, Rimm EB, Hussain A. Predicting difficult endotracheal intubation in surgical patients scheduled for general anesthesia: a prospective blind study. Anesthesia and analgesia. 1995 Aug:81(2):254-8 [PubMed PMID: 7618711]
Lee A, Fan LT, Gin T, Karmakar MK, Ngan Kee WD. A systematic review (meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesthesia and analgesia. 2006 Jun:102(6):1867-78 [PubMed PMID: 16717341]
Level 1 (high-level) evidenceRoth D,Pace NL,Lee A,Hovhannisyan K,Warenits AM,Arrich J,Herkner H, Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. The Cochrane database of systematic reviews. 2018 May 15; [PubMed PMID: 29761867]
Level 1 (high-level) evidencePilkington S, Carli F, Dakin MJ, Romney M, De Witt KA, Doré CJ, Cormack RS. Increase in Mallampati score during pregnancy. British journal of anaesthesia. 1995 Jun:74(6):638-42 [PubMed PMID: 7640115]
McDonnell NJ, Paech MJ, Clavisi OM, Scott KL, ANZCA Trials Group. Difficult and failed intubation in obstetric anaesthesia: an observational study of airway management and complications associated with general anaesthesia for caesarean section. International journal of obstetric anesthesia. 2008 Oct:17(4):292-7. doi: 10.1016/j.ijoa.2008.01.017. Epub 2008 Jul 9 [PubMed PMID: 18617389]
Level 2 (mid-level) evidenceNuckton TJ, Glidden DV, Browner WS, Claman DM. Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep. 2006 Jul:29(7):903-8 [PubMed PMID: 16895257]
Nørskov AK,Rosenstock CV,Wetterslev J,Astrup G,Afshari A,Lundstrøm LH, Diagnostic accuracy of anaesthesiologists' prediction of difficult airway management in daily clinical practice: a cohort study of 188 064 patients registered in the Danish Anaesthesia Database. Anaesthesia. 2015 Mar; [PubMed PMID: 25511370]
Level 2 (mid-level) evidence