Introduction
The splanchnic nerves are paired autonomic nerves containing visceral motor and sensory afferent fibers (see Image. Autonomic Nervous System). Five sets of splanchnic nerves travel on each side of the vertebral column: the cardiopulmonary, thoracic splanchnic, lumbar splanchnic, sacral splanchnic, and pelvic splanchnic nerves. Preganglionic spinal cord cell bodies give rise to the splanchnic nerves, though the cardiopulmonary splanchnic nerves arise from postganglionic cell bodies in the cervical and upper thoracic spinal trunk. All splanchnic nerves have sympathetic activity except for the pelvic splanchnic nerves, which carry parasympathetic fibers.
Splanchnicectomy or splanchnic denervation is a procedure that may be performed to alleviate intractable visceral pain. Splanchnic nerve involvement in visceral tumors can impact surgical planning and outcomes. Understanding the anatomy, physiology, and clinical variations of the splanchnic nerves is essential to diagnosing and managing autonomically driven conditions in the thoracic and abdominopelvic regions.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The splanchnic nerves contain both sensory and motor fibers.[1] The paired splanchnic nerves run parallel to each other and form 5 primary nerves that supply different thoracic and abdominopelvic organs.[2]
Cardiopulmonary Splanchnic Nerves
Structure
The cardiopulmonary splanchnic nerves arise from the C4 to T5 paravertebral ganglia. These nerves synapse with the plexuses innervating the thoracic visceral organs, including the heart, larynx, trachea, bronchi, and lungs.
Function
The cardiopulmonary splanchnic nerves carry sympathetic fibers to their destined visceral organs. Sympathetic stimulation of the heart increases the heart rate and contractility. In the pulmonary system, sympathetic impulses reduce airway resistance by dilating bronchi and bronchioles.
Thoracic Splanchnic Nerves
Structure
The thoracic splanchnic nerves arise from the lower thoracic sympathetic ganglia's medial branches.[3] The thoracic splanchnic nerves are organized into 3 pairs: the greater splanchnic, lesser splanchnic, and least splanchnic nerve pairs. All 3 thoracic splanchnic nerve pairs pass the diaphragmatic crura before traveling to their destinations.[4]
The greater splanchnic nerves receive branches from the T5 to T9 thoracic sympathetic ganglia. These nerves traverse the diaphragm and terminate in the superior preaortic ganglia, commonly called the "celiac ganglia." The postsynaptic fibers then supply the foregut organs as the celiac plexus. The afferent pathway of the greater splanchnic nerves uses the white communicating rami, ventral rami, and spinal nerves to relay sensory information into the spinothalamic tract. This nerve tract projects to the thalamus before ascending to the cerebrum.
The lesser splanchnic nerves arise from the T10 to T11 sympathetic trunk. These nerves lie lateral and inferior to the greater splanchnic nerves, synapsing with either the superior mesenteric or aorticorenal ganglia.
The least splanchnic nerves form from T12 sympathetic branches. These nerves communicate with the renal plexus near the renal arteries.[5][6]
Function
Greater splanchnic nerve stimulation has the following effects:
- Foregut inhibition: This action reduces upper gastrointestinal motility and secretory activity.
- Suppression of pancreatic enzyme secretion: Splanchnic nerve stimulation reduces digestive activity in the duodenum.
- Blood glucose elevation: Stimulating gluconeogenesis, glycogenolysis, and free glucose release increases blood glucose levels. Sympathetic control of pancreatic hormonal functions also increases blood glucose, particularly by inhibiting insulin secretion and stimulating glucagon release.
- Reduction of gallbladder motility: The greater splanchnic nerve inhibits gallbladder contraction and bile emptying.
- Chromaffin cell stimulation: This action enhances catecholamine secretion.
- Splenic pain transmission: Sensory nerves from an inflamed splenic capsule send afferent signals to the splanchnic nerves.
Stimulation of the lesser splanchnic nerves modulate midgut activity. Least splanchnic nerve stimulation enhances renin secretion, reduces renal blood flow, and increases renal tubular sodium absorption. The least splanchnic nerves also stimulate adrenal catecholamine secretion.
Lumbar Splanchnic Nerves
Structure
The lumbar splanchnic nerves form from the L1 to L4 sympathetic chain branches. These nerves course anteriorly toward the aortic plexus, synapsing in diffuse ganglia within the plexus. Postganglionic fibers then project to blood vessels, smooth muscles, and glands in this region. Lumbar splanchnic nerves indirectly connect to the superior hypogastric plexus via the aortic plexus.
The lumbar splanchnic nerves arise from the sympathetic trunk and join the celiac, inferior mesenteric, and superior hypogastric plexuses. The 1st lumbar splanchnic nerve arises from the 1st ganglion and synapses with the celiac, inferior mesenteric, and renal plexuses. The 2nd lumbar splanchnic nerve emerges from the 2nd ganglion and communicates with the intermesenteric plexus, also known as the inferior mesenteric plexus. The 3rd and 4th lumbar splanchnic nerves arise from the 3rd and 4th ganglia, respectively, and join the superior hypogastric plexuses.
Function
The lumbar splanchnic nerves provide sympathetic innervation to lower abdominal and pelvic organs, regulating glandular secretions, stimulating vasoconstriction, and inhibiting smooth muscle contraction in these regions.[7]
Sacral Splanchnic Nerves
Structure
The sacral splanchnic nerves are preganglionic sympathetic fibers arising from T10 to L2 neurons. These nerves synapse with the superior and inferior hypogastric plexus to reach the pelvic area. The fibers then traverse the aortic and inferior mesenteric plexuses to innervate the hindgut, pelvic vessels, and pelvic visceral organs.[8]
Function
The sacral splanchnic nerves provide visceral afferent and sympathetic innervation to the rectum and bladder. These nerves also supply the uterus and vagina in female individuals and the prostate and penis in male individuals.[9] Stimulation of these nerves produces the following actions:
- In the colon: Inhibition of smooth muscle contraction and glandular activity; vasoconstriction
- In the bladder: Detrusor muscle relaxation (though sympathetic stimulation has little effect on bladder emptying)
- In the male genitalia: Ductus deferens and seminal vesicle contraction; initiation of emission and ejaculation; detumescence
- In the female genitalia: Vasoconstriction, diminishing clitoral erection and vaginal lubrication
Visceral afferent fibers send sensory information to the spine.
Pelvic Splanchnic Nerves
Structure
Pelvic splanchnic nerves arise from the S2 to S4 ventral rami.[10] These fibers synapse with the intrinsic ganglia in the lower colon, rectum, and pelvic viscera. Radical pelvic surgery is associated with an increased risk of pelvic splanchnic nerve injury.
Function
Pelvic splanchnic nerves carry parasympathetic fibers. Stimulation of these nerves produces the following actions:
- In the colon: Emptying of the colon
- In the bladder: Emptying of the bladder
- In the male genitalia: Penile erection, final ejaculation through the urethra
- In the female genitalia: Increased vaginal secretions, clitoral erection, labia minora engorgement
These nerves also carry nociceptive afferents.
Embryology
During the 5th week of embryonic development, neural crest cells migrate along each side of the spinal cord and form paired ganglia dorsolateral to the aorta. The sympathetic trunks connect these segmentally organized sympathetic ganglia, forming chainlike structures on each side of the vertebral bodies. Some neural crest cells migrate ventrally to the aorta to form preaortic ganglionic neurons, including the celiac and mesenteric ganglia. Other neural crest cells give rise to terminal ganglia in sympathetic plexuses near the visceral organs.
The sympathetic trunks develop with the growth of the axons from the thoracolumbar lateral horn cell bodies. White rami communicantes connect spinal nerve roots with the paravertebral ganglia, where they can either synapse with postganglionic neurons on the same spinal level, ascend to superior ganglia, or descend to inferior ganglia. Other presynaptic fibers pass through the paravertebral ganglia without synapsing but terminate directly in the nerve plexuses.
Nerves
The table below summarizes information about the origin, destination, autonomic fiber type, and autonomic division of the splanchnic nerves.
Table. Splanchnic Nerves
| Splanchnic Nerves | Origin | Destination | Autonomic Fiber Type | Autonomic Division |
| Cardiopulmonary | C4-T5 paravertebral ganglia | Thoracic viscera | Postsynaptic | Sympathetic |
|
Thoracic |
|
|
Presynaptic | Sympathetic |
| Lumbar | L1-L4 sympathetic trunk |
Inferior mesenteric ganglia Intermesenteric and hypogastric plexus ganglia |
Presynaptic | Sympathetic |
| Sacral | T10 to L2 sympathetic trunk | Ganglia of the superior and inferior hypogastric plexuses | Presynaptic | Sympathetic |
| Pelvic | S2 to S4 ventral rami | Intrinsic ganglia of the descending and sigmoid colon, rectum, and pelvic visceral organs | Presynaptic | Parasympathetic |
Muscles
The splanchnic nerves control visceral muscles in different thoracic and abdominal regions.
- Cardiopulmonary: myocytes, smooth muscles in the large air passageways, lungs, and blood vessels
- Thoracic: smooth muscles in the foregut, midgut, and kidneys
- Lumbar, sacral, and pelvic: smooth muscles in the hindgut and pelvic viscera
The sympathetic influence on smooth muscles helps prepare the body for rapid responses to stress or environmental challenges. Parasympathetic stimulation does the opposite.
Physiologic Variants
The greater splanchnic nerves typically arise from the T5 to T9 roots, with other nerves joining these fibers along their course. However, the origin of the greater splanchnic nerves can involve regions as low as the T11 level in some individuals. Others may exhibit discontinuity of spinal contributions to this nerve pair, such that the fibers originate from spinal regions separated by at least 1 level.
Surgical Considerations
Key surgical considerations to keep in mind considering the splanchnic nerve are as follows:
- Subdiaphragmatic neuroadaptive surgical procedures may reduce chronic abdominal pain. A thorough understanding of the anatomical position and location of the thoracic splanchnic nerves is critical to this procedure's success.[11]
- Pelvic splanchnic nerve injury is a potential risk of cervical cancer surgery. These nerves can get inadvertently damaged during resection.[12] Intraoperative electrical stimulation of the pelvic splanchnic nerves may be performed to ensure anatomical and functional preservation before closing the surgical field. The possible sequelae of pelvic splanchnic nerve injury include loss of bowel control, constipation, sexual dysfunction, bladder atony, deranged bladder reflexes, and chronic abdominopelvic pain.[13]
Clinical Significance
Organization of the splanchnic nerves into different levels is useful in thoracic, abdominal, and retroperitoneal procedures. For example, chronic pain associated with chronic pancreatitis or unresectable pancreatic cancer may be managed by thoracoscopic splanchnicectomy, targeting the greater splanchnic nerves. This treatment reduces visceral pain afferent nerve firing in the pancreatic region. Chronic flank pain arising from conditions like autosomal-dominant polycystic kidney disease may also be managed with thoracic thoracoscopic splanchnicectomy, this time focusing on renal denervation.
Iatrogenic splanchnic nerve transection may result in orthostatic hypotension, as these nerves regulate smooth muscle contraction in the blood vessels. Loss of bowel control may arise from inadvertent lumbar, sacral, or pelvic splanchnic nerve injury.
Chronic abdominal pain may be managed with a splanchnic nerve block if a celiac plexus block fails. A splanchnic nerve block requires needle insertion in the anterolateral margin of the T12 vertebral body. The patient is placed in a prone position to visualize the thoracic spine, then the 12th rib, L1 spinous process, and T12 vertebral body are identified. Splanchnic nerve blocks provide better and longer-lasting pain relief than celiac plexus blocks.[14]
Diabetic neuropathy can cause thoracic and abdominopelvic complications, including sexual dysfunction, due to splanchnic nerve damage.
Media
(Click Image to Enlarge)
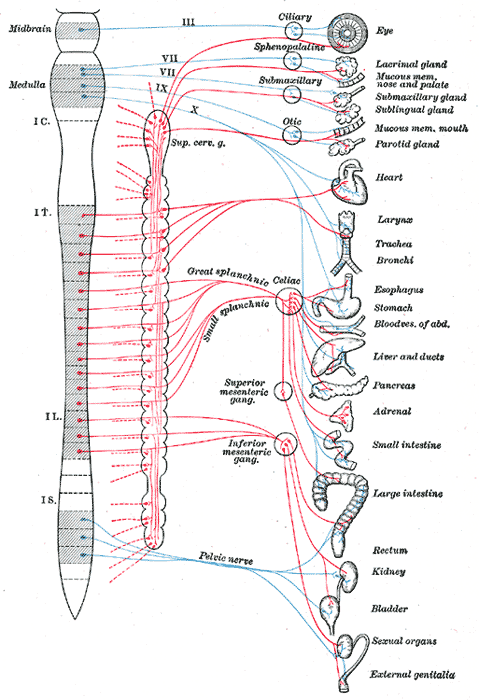
Autonomic Nervous System. This illustration shows the sympathetic and parasympathetic nervous system. Blue lines show the sacral or parasympathetic outflow. Red lines mark the thoracolumbar or sympathetic outflow. The pathways of the greater and small splanchnic and pelvic nerves are shown. The midbrain, medulla, and superior cervical, ciliary, sphenopalatine, submaxillary, otic, celiac, and superior and inferior mesenteric ganglia are also included in this illustration. The organs controlled by the autonomic nervous system are shown.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Kaiser JT, Lugo-Pico JG. Neuroanatomy, Spinal Nerves. StatPearls. 2024 Jan:(): [PubMed PMID: 31194375]
Waxenbaum JA, Reddy V, Varacallo M. Anatomy, Autonomic Nervous System. StatPearls. 2024 Jan:(): [PubMed PMID: 30969667]
Alshak MN, M Das J. Neuroanatomy, Sympathetic Nervous System. StatPearls. 2024 Jan:(): [PubMed PMID: 31194352]
Candal R, Reddy V, Samra NS. Anatomy, Abdomen and Pelvis: Celiac Ganglia. StatPearls. 2024 Jan:(): [PubMed PMID: 30844156]
Ehrhardt JD, Weber C, Carey FJ, Lopez-Ojeda W. Anatomy, Thorax, Greater Splanchnic Nerves. StatPearls. 2024 Jan:(): [PubMed PMID: 29763202]
Yang HJ, Gil YC, Lee WJ, Kim TJ, Lee HY. Anatomy of thoracic splanchnic nerves for surgical resection. Clinical anatomy (New York, N.Y.). 2008 Mar:21(2):171-7. doi: 10.1002/ca.20599. Epub [PubMed PMID: 18288763]
Jetti R, Kadiyala B, Bolla SR. Anatomy, Back, Lumbar Sympathetic Chain. StatPearls. 2024 Jan:(): [PubMed PMID: 30969736]
LeBouef T, Yaker Z, Whited L. Physiology, Autonomic Nervous System. StatPearls. 2024 Jan:(): [PubMed PMID: 30860751]
McEvoy A, Tetrokalashvili M. Anatomy, Abdomen and Pelvis: Female Pelvic Cavity. StatPearls. 2024 Jan:(): [PubMed PMID: 30860705]
Spence KT, Forro SD. Anatomy, Bony Pelvis and Lower Limb: Nerves. StatPearls. 2024 Jan:(): [PubMed PMID: 30335337]
Kommuru H, Jothi S, Bapuji P, Sree D L, Antony J. Thoracic part of sympathetic chain and its branching pattern variations in South Indian cadavers. Journal of clinical and diagnostic research : JCDR. 2014 Dec:8(12):AC09-12. doi: 10.7860/JCDR/2014/9274.5246. Epub 2014 Dec 5 [PubMed PMID: 25653929]
Park SB, Garg R, Singh P. Anatomy, Abdomen and Pelvis, Nerves. StatPearls. 2024 Jan:(): [PubMed PMID: 31194402]
Lemos N, Possover M. Laparoscopic approach to intrapelvic nerve entrapments. Journal of hip preservation surgery. 2015 Jul:2(2):92-8. doi: 10.1093/jhps/hnv030. Epub 2015 Jun 6 [PubMed PMID: 27011825]
Kapural L, Lee N, Badhey H, McRoberts WP, Jolly S. Splanchnic block at T11 provides a longer relief than celiac plexus block from nonmalignant, chronic abdominal pain. Pain management. 2019 Mar 1:9(2):115-121. doi: 10.2217/pmt-2018-0056. Epub 2019 Jan 25 [PubMed PMID: 30681022]