Introduction
The eyelids are important for adequate tear film distribution across the ocular surface, tear drainage, protection of ocular surfaces, and cosmesis. The eyelids also contain glands that secrete substances responsible for lubricating the ocular surface.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Skin/Subcutaneous Tissue
The eyelid skin is unique because it has no subcutaneous fat and is thus the thinnest layer of skin on the body. The skin overlying the tarsus tends to be firmly attached to the underlying tissue; whereas, the skin above the tarsal plate, in the upper lid, and below the tarsal plate, in the lower lid, overlying the orbital septum is loosely attached to underlying tissue giving rise to a potential space for fluid to collect in the setting of trauma or edema.
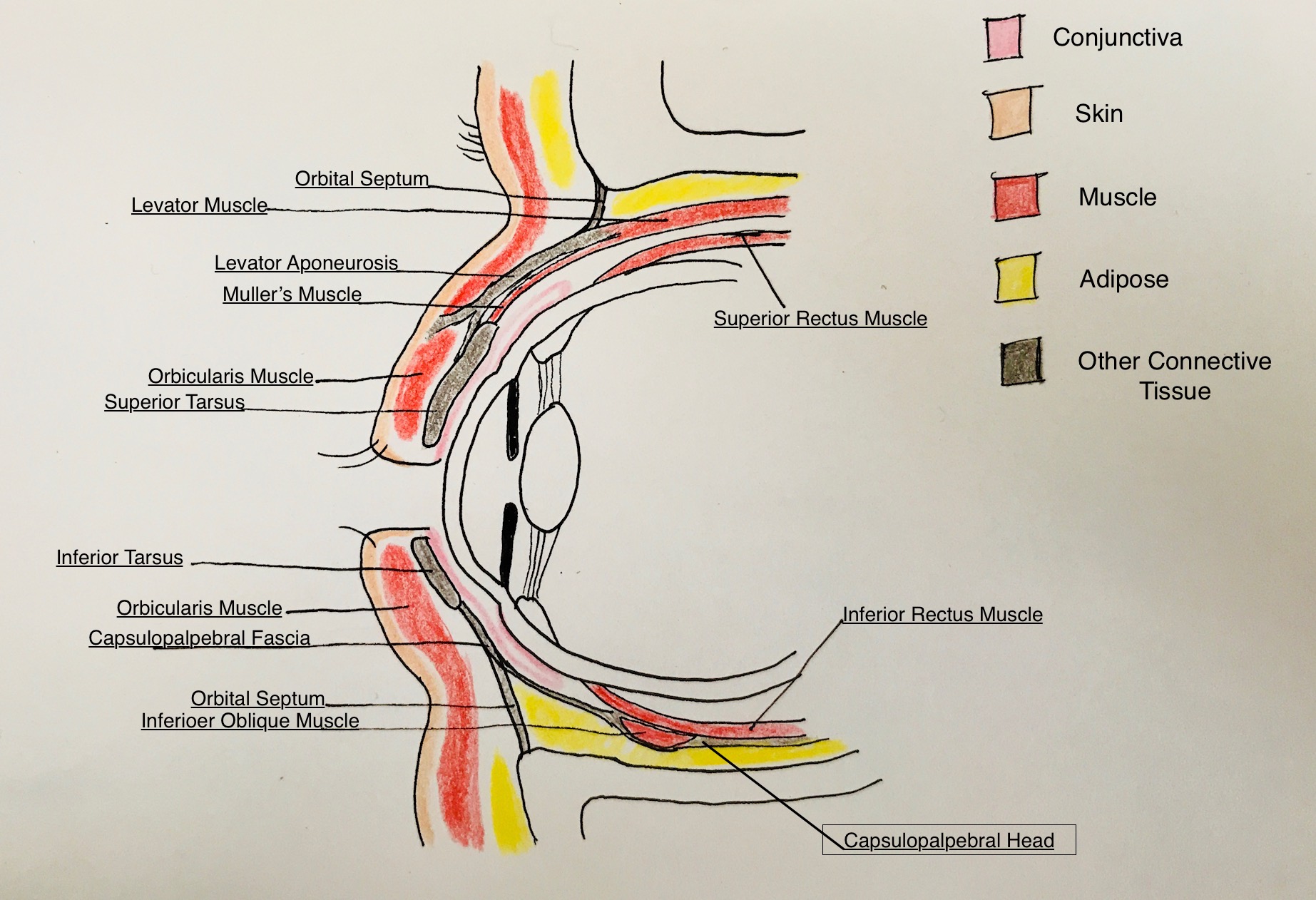
Orbital Septum
A thin, fibrous connective tissue layer separates anterior eyelid structures from intra-orbital structures. The superior orbital septum connects the periosteum of the superior orbital rim to the levator aponeurosis above the superior tarsal border (though this has racial variance). The inferior orbital septum connects the periosteum of the inferior orbital rim to the capsulopalpebral fascia just below the inferior tarsal border.
Orbital Fat
Orbital fat is located immediately posterior to the orbital septum and anterior to the levator aponeurosis in the upper lid and capsulopalpebral fascia of the lower lid. In the upper lid, there are two discrete nasal and central fat pads. In the lower eyelid, there are three fat pads: nasal, central, and temporal. Thin fibrous capsules surround the pads. The inferior oblique muscle runs in between the medial and central fat pad in the lower eyelid and is an important anatomical landmark during eyelid and orbital surgery.
Tarsus
The tarsal plates serve as the main structural component of the eyelids. They are made of dense connective tissue and contain the Meibomian glands and eyelash follicles. There are approximately 30 meibomian glands in the upper eyelid and 20 meibomian glands in the lower eyelid. There are approximately 100 eyelashes in the upper lid in 2 to 3 rows. There are approximately 50 eyelashes in the lower eyelid. The tarsal plate of the upper eyelid is 10 mm to 12 mm vertically in the center of the eyelid, and the tarsal plate of the lower eyelid is up to 4 mm vertically in the central eyelid. Both upper and lower tarsal plates are approximately 29 mm in horizontally length. Both tarsal plates have rigid attachments to the periosteum via the medial and lateral canthal tendons. Along with the Meibomian glands that run in a row parallel to the lid margin and posterior to the lash line, the glands of Zeis and Moll are associated with eyelash hair follicles and secrete lipid and modified sweat respectively.
Conjunctiva
This non-keratinizing squamous epithelium lines the inner surface of the eyelids and continues to cover the anterior surface of the globe where it terminates at the edge of the cornea. The conjunctiva contains mucin-secreting goblet cells and accessory lacrimal glands that assist in keeping ocular tissues lubricated.
In the nasolacrimal system (not represented in the illustration) both the upper eyelid and the lower eyelid have small openings on the surface of the eyelid margin near the medial canthus called puncta. The puncta lead to a drainage channel called the canaliculus, the superior and inferior of which merge medially to form the common canaliculus. The canaliculi travel 2 mm inferiorly (lower lid) or superiorly (upper lid) from the punctum, then turn 90 degrees medially and travel 8 mm to 10 mm before reaching the common canaliculus. The common canaliculus then drains into the lacrimal sac which in turn drains to the nose underneath the inferior turbinate via the nasolacrimal duct. [1]
Embryology
The eyelid is derived from secondary mesenchyme and surface ectoderm. Secondary mesenchyme is produced when the cranial neural crest cells invade the mesoderm. The surface ectoderm gives rise to the eyelid skin epithelium, conjunctival, hair follicles and accessory glands. The mesenchyme gives rise to the tarsal plate, the muscles in the eyelid and the orbital septum. The eyelid begins to form during week 6 of gestation and continues to develop until nearly complete at 36 weeks. The stages of development are formation, fusion, development, separation, and maturation.[2]
Blood Supply and Lymphatics
The upper eyelid gets most of its blood supply from the internal carotid artery. Blood flows from the internal carotid artery to the ophthalmic artery to the superior marginal arcade that traverses the lid just superior to the upper eyelid margin posterior to the orbicularis muscle and anterior to the tarsal plate.
The inferior eyelid gets the majority of its blood from the external carotid artery. Blood flows from the external carotid artery to the facial artery to the angular artery and then to the inferior marginal artery. The upper and lower eyelids have rich vascular supply and have many anastomoses between the upper and lower lid circulations.
The medial parts of the upper and lower eyelids have lymph circulation that drains to the submandibular lymph nodes. The lateral parts of the upper and lower eyelids drain to the pre-auricular lymph nodes.
Nerves
The sensation of the upper eyelid is provided by the ophthalmic branch of cranial nerve V. The sensation of the lower eyelid is provided by the maxillary branch of cranial nerve V.
Cranial nerve III, as well as sympathetic innervation, innervates the eyelid retractors. Cranial nerve VII innervates the orbicularis muscle responsible for protracting (closing) the eyelids. [3]
Muscles
Protractors
Directly under the upper and lower eyelid skin is the orbicularis oculi muscle. This is the main protractor muscle (closure) of the eyelid. The orbicularis oculi muscle is a large, thin, circular muscle that is divided into pretarsal, preseptal, and orbital segments. The pretarsal and preseptal segments are responsible for involuntary eyelid closure (blinking). The orbital segment is primarily responsible for voluntary/forced eyelid closure.
Retractors
Upper Eyelid
The levator muscle originates in the apex of the orbit, travels forward over the eyeball, and splits into two unique structures: the levator aponeurosis anteriorly and the superior tarsal muscle (Muller's muscle) posteriorly. The split occurs superiorly at the Whitnall ligament and inferiorly at the Lockwood ligament.
The levator aponeurosis continues inferiorly and splits into an anterior and posterior portion near the upper tarsal border. The anterior portion of the levator aponeurosis inserts into the pretarsal orbicularis and skin to form the upper eyelid crease. The posterior portion of the aponeurosis inserts into the upper anterior surface of the tarsal plate.
Muller's muscle extends from the undersurface of the levator aponeurosis at the level of the Whitnall ligament and inserts along the upper eyelid superior tarsal margin. It is a sympathetically innervated retractor muscle of the upper eyelid and provides approximately 2mm of eyelid elevation.
Lower Eyelid
The capsulopalpebral fascia is analogous to the levator aponeurosis in the upper eyelid. Its fibers originate from attachments to the inferior rectus muscle. It extends forward, envelops the inferior oblique muscle, forms the Lockwood ligament, and continues anteriorly, attaching to the orbital septum and inferior conjunctival fornix before finally inserting on the inferior tarsal border.
The inferior tarsal muscle is analogous to the Muller's muscle in the upper eyelid. This muscle is poorly developed and runs posterior to the capsulopalpebral fascia of the lower eyelid. [4]
Physiologic Variants
Asian populations tend to have a lower eyelid crease than Caucasian populations. This is because the orbital septum in Asian eyelids fuses with the levator aponeurosis closer to the eyelid margin; whereas, the orbital septum in Caucasians fuses with the levator aponeurosis closer to the superior border of the tarsal plate.
Surgical Considerations
Many surgical procedures can be done on eyelids to address a variety of eyelid conditions. One of the most common eyelid surgeries performed on adults is to correct dermatochalasis of the eyelids. This is called a blepharoplasty and consists of surgically removing eyelid skin along the eyelid crease for improved cosmesis or for therapeutic purposed to improve the superior visual field that is being occluded from hanging eyelid skin.[5]
Clinical Significance
Many different types of conditions can affect the eyelids. An example of a common condition is when the glands that produce oil in the eyelid can become obstructed or infected and cause a painful, inflamed nodule on the eyelid. If the nodule is infected, it is called a hordeolum. If the nodule is a sterile collection of debris from an obstructed gland it is called a chalazion. Another common condition that can affect the eyelids is known as blepharitis. This is when the eyelid margin becomes inflamed and irritated.
Media
References
Tong J, Lopez MJ, Patel BC. Anatomy, Head and Neck: Eye Orbicularis Oculi Muscle. StatPearls. 2024 Jan:(): [PubMed PMID: 28722936]
Tawfik HA, Abdulhafez MH, Fouad YA, Dutton JJ. Embryologic and Fetal Development of the Human Eyelid. Ophthalmic plastic and reconstructive surgery. 2016 Nov/Dec:32(6):407-414 [PubMed PMID: 27124372]
Choi Y, Kang HG, Nam YS, Kang JG, Kim IB. Facial Nerve Supply to the Orbicularis Oculi around the Lower Eyelid: Anatomy and Its Clinical Implications. Plastic and reconstructive surgery. 2017 Aug:140(2):261-271. doi: 10.1097/PRS.0000000000003543. Epub [PubMed PMID: 28746270]
Ludwig PE, Aslam S, Czyz CN. Anatomy, Head and Neck: Eye Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 29262013]
Chang EI, Esmaeli B, Butler CE. Eyelid Reconstruction. Plastic and reconstructive surgery. 2017 Nov:140(5):724e-735e. doi: 10.1097/PRS.0000000000003820. Epub [PubMed PMID: 29068942]