Introduction
Although tibia and fibula shaft fractures are amongst the most common long bone fractures, there is little literature citing the incidence of isolated fibula shaft fractures. One reason for this may be the treatment for the vast majority of isolated fibula shaft fractures is non-operative - this contrasts with the treatment of lateral malleolus fractures, which, although it is part of the fibula, technically, are categorized as ankle fractures and, therefore, have different treatment principles. The following article will focus on fractures of the fibula that are proximal to the ankle joint and the treatment of such fractures.
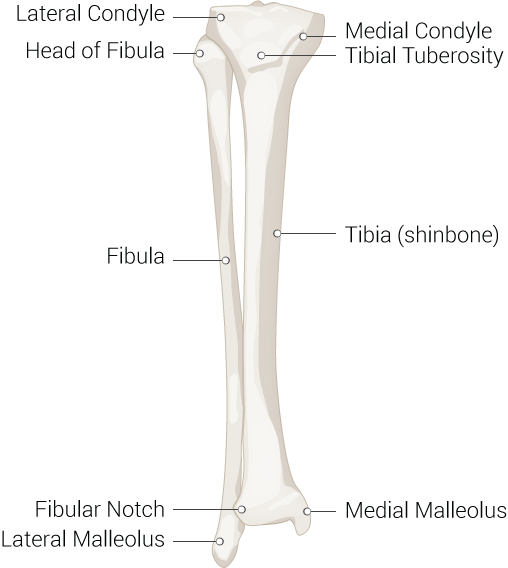
The fibula is one of the two long bones in the leg, and, in contrast to the tibia, is a non-weight bearing bone in terms of the shaft. Located posterolaterally to the tibia, it is much smaller and thinner. At its most proximal part, it is at the knee just posterior to the proximal tibia, running distally on the lateral side of the leg where it becomes the lateral malleolus at the level of the ankle.
The fibula and tibia connect via an interosseous membrane, which attaches to a ridge on the medial surface of the fibula. There is very limited mobility between this syndesmosis.
There are several distinct portions of the fibula in terms of structure, including the head, neck, shaft, and the distal end termed the lateral malleolus. This article focuses on the shaft of the fibula, which can be located between the neck of the fibula, the narrowed portion just distal to the fibular head, and the lateral malleolus, which in concert with the posterior and medial malleoli, form the ankle joint. Both the posterior and medial malleolus are part of the distal end of the tibia.
The fibular shaft is an origin for multiple muscles of the leg, including muscles of the anterior compartment (extensor digitorum longus, extensor hallucis longus, peroneus tertius), the lateral compartment (peroneus longus, peroneus brevis), the superficial posterior compartment (soleus), and the deep posterior compartment (tibialis posterior and flexor hallucis longus). The triangular shape of the fibula is dictated by the insertion points of the muscles on the shaft.
The superficial peroneal nerve innervates the musculature of the lateral compartment and is responsible for eversion and, to a much milder degree, plantarflexion of the foot. Damage to this nerve may result in deficits in those movements. The superficial peroneal nerve also gives sensation to the dorsum of the foot.
The deep peroneal nerve innervates the musculature of the anterior compartment and is responsible for the dorsiflexion of the foot and toes. A common result of damage to the deep peroneal nerve is drop foot, in which there is a loss of the capacity to dorsiflex the foot. The deep peroneal nerve is responsible for sensation over the first dorsal webspace.[1][2][3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
A truly isolated fracture of the fibula, one that has no other associated ligamentous or other bony injuries, are quite rare. They are typically the result of a direct injury to the leg, usually a fall or direct blow or blunt trauma like a sports injury or motor vehicle accident. Gunshot wounds are another mechanism from which an isolated fibula fracture can be sustained.[4]
Epidemiology
As stated earlier, isolated fractures of the fibula are quite rare, and not much literature exists on the frequency of their occurrence. While tibia fractures are most common in young males and elderly females, it is likely that most isolated fibula fractures are in the younger population, based on the injury responsible for these fractures. Young athletes, especially those involved in contact sports, and those individuals involved in motor vehicle accidents and pedestrian versus motor vehicle accidents, are likely at the highest risk.
History and Physical
A thorough history and physical are important to ensure a proper diagnosis. As stated earlier, isolated fibula shaft fractures are rare but, when they do occur, commonly are the result of direct trauma to the leg. A patient presenting with a history of recent trauma to the leg with tenderness to palpation, especially over the fibula on the lateral leg, should be considered capable of suffering fibula shaft fracture. It is also pertinent to examine the skin for any lacerations, abrasions, or bruising that would be consistent with trauma to the leg. The entire extremity should be examined for any signs of trauma, including range of motion of the joints above and below the area to rule out any potential intra-articular pathology. The quality of pain is likely to be acute and sharp, not longstanding, or have qualities more consistent with nerve pathology, like burning or shooting pain.
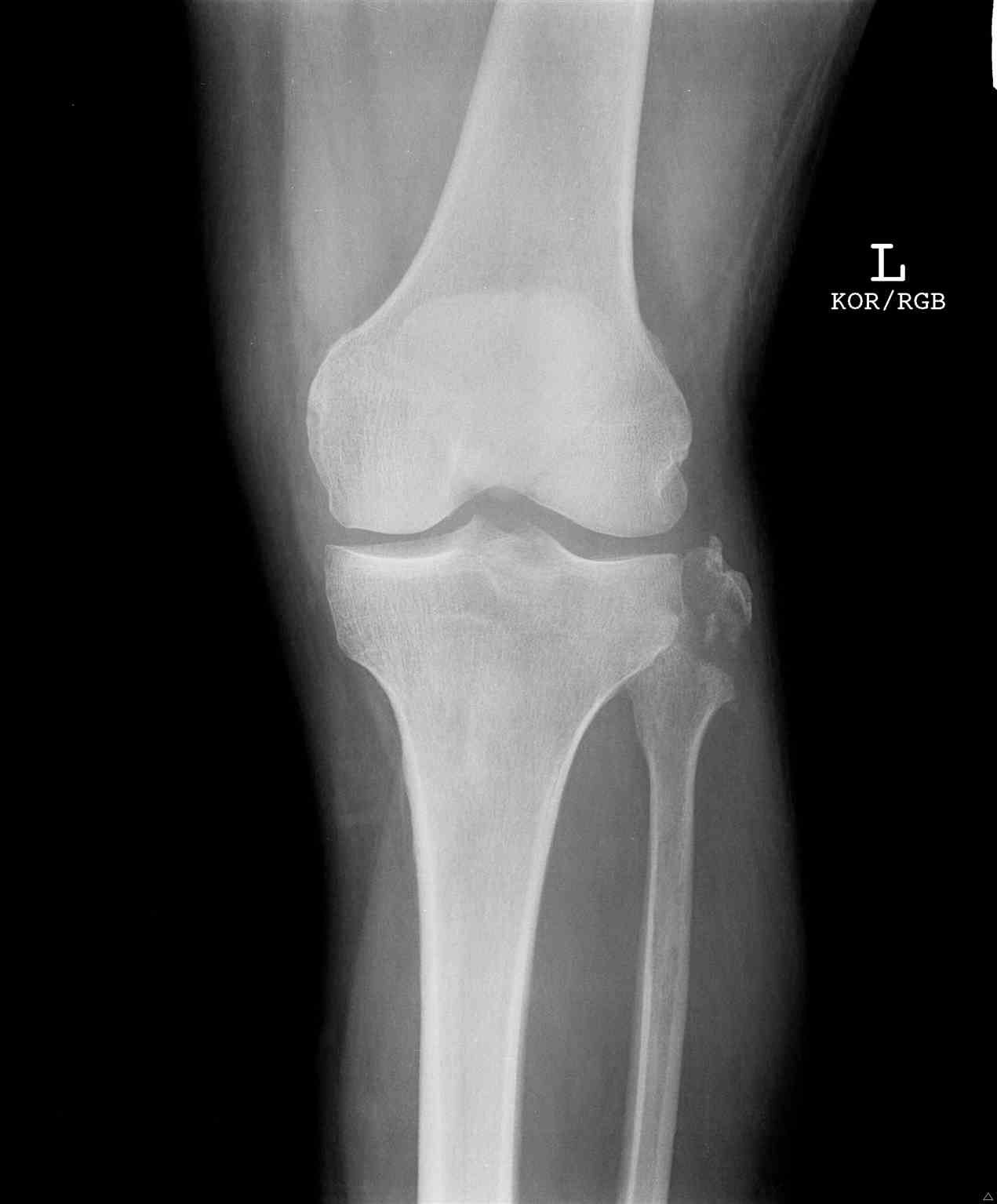
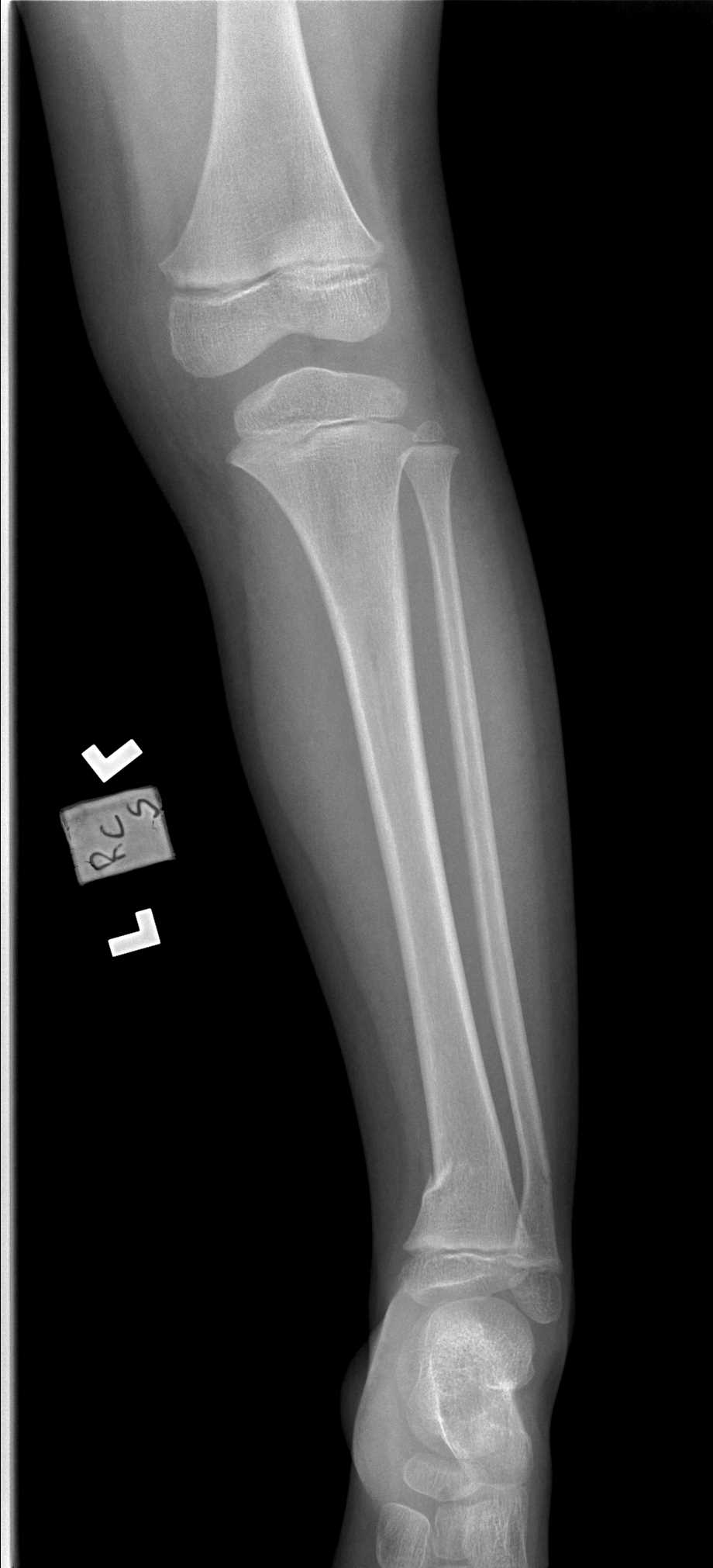
Evaluation
It is important to perform a thorough evaluation of isolated fibular shaft fractures to ensure they are, in fact, isolated. As in most orthopedic injury evaluations, it is good practice to check one joint above and below the injury. The knee should be checked for any ligamentous instability, and the ankle should be evaluated for any injury. Dedicated films of the knee and ankle are especially important to rule out other fractures in addition to lower-leg x rays. A fracture at the fibular neck without any other fractures in the rest of the fibula or tibia is pathognomonic for a syndesmotic injury and is termed a Maisonneuve fracture. This, by definition, cannot be an isolated fibula shaft fracture due to ligamentous involvement and will require different treatment. Likewise, a fracture of the fibula within 15 cm of the ankle joint is likely to have either bony involvement of the tibia, ligamentous injury, or both.[5]
Treatment / Management
In most instances, the treatment for isolated fibular shaft fractures is nonoperative. Since the shaft of the fibula is not a weight-bearing portion of the bone, patients can be treated with a weight-bearing as tolerated restriction, and some practitioners may utilize a walking boot for comfort.[6]
Differential Diagnosis
- Osteoid osteoma
- Ewing sarcoma
- Osteosarcoma
- Osteomyelitis
- Muscle spasm
- Ankle sprain
- Tendon rupture
- Compartment syndrome
- Nerve entrapment
Prognosis
Patients with an isolated fibula shaft fracture typically have promising outcomes. These are often treated conservatively and symptomatically. There are seldom long term limitations, and patients often go on to union between 6-8 weeks if they have minimal comorbidities.
Complications
Complications that are related to fractures of the fibula shaft are rare but do exist. Case reports exist of damage to the superficial peroneal nerve. There have also been reports of arterial damage and compartment syndrome in patients with isolated fibula fractures.[7][8][9]
Nonunions may also present and may be symptomatic, in which case a compression plate and autogenous bone grafting is the gold standard treatment. These plates can be left in place for life unless they become irritable. Removal is usually delayed until at least 12 months.[10][11]
Enhancing Healthcare Team Outcomes
Isolated fibula shaft fractures are often treated nonoperatively and symptomatically with acceptable results. However, it is important to establish appropriate interprofessional communication to ensure proper diagnosis and rule out other injuries that could influence a different, maybe surgical treatment. This communication amongst physicians, those in orthopedics and elsewhere, as well as other health care professionals, can enhance patient-centered care and ultimately lead to improved outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Gupton M, Munjal A, Kang M. Anatomy, Bony Pelvis and Lower Limb: Fibula. StatPearls. 2025 Jan:(): [PubMed PMID: 29261984]
Carto C, Lezak B, Varacallo MA. Anatomy, Bony Pelvis and Lower Limb: Distal Tibiofibular Joint (Tibiofibular Syndesmosis). StatPearls. 2025 Jan:(): [PubMed PMID: 31613435]
Manganaro D, Alsayouri K. Anatomy, Bony Pelvis and Lower Limb: Ankle Joint. StatPearls. 2025 Jan:(): [PubMed PMID: 31424742]
Sarpong NO, Levitsky M, Held M, Coury J, Greisberg J, Vosseller JT. Isolated fibular stress fractures: Radiographic parameters. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2020 Dec:26(8):935-938. doi: 10.1016/j.fas.2019.12.004. Epub 2020 Jan 9 [PubMed PMID: 31937428]
Fang C, Platz A, Müller L, Chandy T, Luo CF, Vives JMM, Leung F, Babst R. Evaluation of an expectation and outcome measurement questionnaire in ankle fracture patients: The Trauma Expectation Factor Trauma Outcomes Measure (TEFTOM) Eurasia study. Journal of orthopaedic surgery (Hong Kong). 2020 Jan-Apr:28(1):2309499019890140. doi: 10.1177/2309499019890140. Epub [PubMed PMID: 31916492]
van Leeuwen CAT, Hoffman RPC, Hoogendoorn JM. Long-term outcome in operatively and non-operatively treated isolated type B fibula fractures. Injury. 2019 Dec:50(12):2318-2323. doi: 10.1016/j.injury.2019.10.006. Epub 2019 Oct 4 [PubMed PMID: 31607441]
al-Awami SM, Sadat-Ali M, Sankaran-Kutty M. Arterial injury complicating fracture of the fibula: a case report. Injury. 1987 May:18(3):214-5 [PubMed PMID: 3508855]
Level 3 (low-level) evidenceCorey RM, Salazar DH. Entrapment of the Superficial Peroneal Nerve Following a Distal Fibula Fracture. Foot & ankle specialist. 2017 Feb:10(1):69-71. doi: 10.1177/1938640016640887. Epub 2016 Jul 7 [PubMed PMID: 27044598]
Pichler W, Clement H, Boldin C, Grechenig W, Tesch NP. Primary transection of the superficial peroneal nerve resulting from a distal fibula fracture. Journal of orthopaedic trauma. 2007 Mar:21(3):212-4 [PubMed PMID: 17473759]
Level 3 (low-level) evidenceRandall RM, Nagle T, Steckler A, Billow D, Berkowitz MJ. Dual Nonlocked Plating as an Alternative to Locked Plating for Comminuted Distal Fibula Fractures: A Biomechanical Comparison Study. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2019 Sep:58(5):916-919. doi: 10.1053/j.jfas.2019.01.017. Epub 2019 Jul 23 [PubMed PMID: 31345755]
Ye MY, Vaughn J, Briceno J, Kwon JY. Screw distraction technique for gaining fibular length. Injury. 2018 Dec:49(12):2322-2325. doi: 10.1016/j.injury.2018.09.010. Epub 2018 Sep 10 [PubMed PMID: 30262207]