Introduction
Chondrosarcomas are malignant cartilaginous neoplasms with diverse morphological features and clinical behavior. They account for about 20% of all primary malignant tumors of the bone [1]. They usually arise in the pelvis or long bones [2]. Primary or conventional chondrosarcoma arises in preexisting normal bone and is distinguished from the rarer secondary tumors, which occur in a preexisting enchondroma or osteochondroma [1]. Conventional chondrosarcoma, which accounts for 85%–90% of chondrosarcomas is subdivided into the central, periosteal, and peripheral subgroups [3]. Non-conventional chondrosarcoma variants include clear cell chondrosarcoma, mesenchymal chondrosarcoma, and dedifferentiated chondrosarcoma [3]. The radiographic features of chondrosarcoma are often very characteristic, and a definitive diagnosis can usually be made by imaging examination alone.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The majority of chondrosarcomas are sporadic, but they may develop from the malignant transformation of osteochondromas and enchondromas [3]. Malignant transformation occurs in 5% of osteochondromas either multiple or solitary forms [3].
Epidemiology
Primary central chondrosarcoma is the third most common primary malignancy of bone after myeloma and osteosarcoma. Chondrosarcoma is a tumor of adulthood and older age. The majority of patients are older than 50 years of age at diagnosis, with a slight male predominance [4]. The most common locations of involvement of chondrosarcoma include the bones of the axial skeleton (pelvis, scapula, sternum, and ribs) followed by the proximal femur and proximal humerus [1]. Involvement of the hands and feet is rare.
Pathophysiology
Chromosomal anomalies detected in some types of chondrosarcomas include 9p21, 10, 13q14, and 17p13. Chromosomal structural abnormalities and genetic instability are reported in well-differentiated chondrosarcomas analyzed by cytogenetics. Moreover, the amplification of MYC and AP-1transcription factors plays a vital role in the pathogenesis of chondrosarcoma [3].
Histopathology
Macroscopic findings:
Chondrosarcomas are large tumors, usually greater than 4 cm in size [5]. They have a translucent lobular, blue-grey, or white cut surface corresponding to the presence of hyaline cartilage. There may be areas containing myxoid or mucoid material and cystic changes. Yellow-white chalky areas of calcium deposit are commonly present (mineralization). Erosion and destruction into soft tissue may be seen.
Microscopic findings:
Chondrosarcomas show abundant blue-grey cartilage matrix-production. Irregularly shaped lobules of cartilage varying in size and shape are present. Fibrous bands separate these lobules or permeate bony trabeculae. Calcified areas suggesting the presence of a pre-existing enchondroma can often be found. The chondrocytes are atypical, with variable size and shape and contain enlarged hyperchromatic nuclei. Binucleation is frequently seen. Chondroid matrix liquefaction or myxoid changes are a common feature of chondrosarcomas. Necrosis and mitoses can be seen. There is often permeation into the cortical bone and the marrow space with entrapment of bony trabeculae [5].
Grading of chondrosarcomas is essential and is useful in predicting histological behavior. Chondrosarcomas are divided into three grades based upon their histopathology:
- Grade I: considered to be low-grade (locally aggressive), also called atypical cartilaginous tumor [4]. Grade I lesions will often closely resemble normal cartilage or the benign enchondroma. In this instance, the distinction between benign and malignant often depends on the demonstration of a “chondrosarcoma permeation pattern” where the tumor infiltrates through the marrow cavity instead of being confined by the native architecture. Grade I chondrosarcoma is moderately cellular and contain hyperchromatic, plump nuclei of uniform size.
- Grade II tumors contain a greater degree of nuclear atypia hyperchromasia, and nuclear size and are more cellular. Mitoses can be found.
- Grade III tumors are more pleomorphic and atypical than grade II chondrosarcomas. Mitoses are more easily detected. The cells at the periphery of the lobules are less differentiated and become spindled.
- The fourth group of chondrosarcomas, considered as grade IV; is called dedifferentiated chondrosarcoma and makes up 10% of all chondrosarcomas [4]. Dedifferentiation occurs in a small subset of patients and is defined histologically by the presence of a high-grade, often spindled or pleomorphic tumor without significant cartilaginous matrix. Dedifferentiated chondrosarcoma is, by definition, a high-grade neoplasm with an inferior prognosis.
Other less common types of chondrosarcomas are mesenchymal and clear cell chondrosarcomas [4].
Immunophenotype:
Only a small percentage of the IDH1 mutations (20%) can be identified using a specific IDH1 R132H antibody.
History and Physical
Local swelling and pain are the most common presenting symptoms. The symptoms are usually of long duration (months to years). Tumors located in the skull base can cause neurological symptoms.
Evaluation
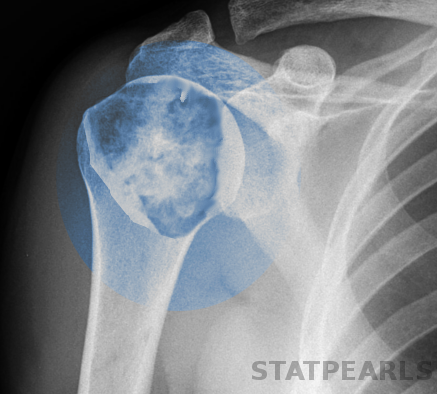
Plain radiography:
Plain radiography is used for initial evaluation. Plain x-rays allow the identification of the cartilaginous nature and the aggressiveness of the lesion [6]. Plain x-rays may reveal the following findings:
- Lytic lesions in 50% of the cases
- Intralesional calcifications: in about 70% of the cases (popcorn calcification or rings and arcs calcification)
- Endosteal scalloping
- Permeative appearance or moth-eaten appearance in high-grade chondrosarcomas
- Cortical remodeling, thickening, and periosteal reaction
Computed tomography scan:
Computed tomography scan can reveal the following findings [6]:
- Matrix calcification in 94% of the cases
- Endosteal scalloping
- A cortical breach in about 90% of long bone chondrosarcoma
- Heterogenous contrast enhancement
Magnetic resonance imaging:
In typical forms, MRI demonstrates a lobulated lesion with a high-signal intensity on T2 and a low or intermediate signal on T1-weighted images [7] [6].
Tissue biopsy:
Tissue biopsy is essential to diagnose chondrosarcoma and differentiate it from other malignant or benign bone tumors. Biopsy should be taken from the most aggressive portion of cancer as determined by imaging.
Treatment / Management
Surgery:
Location and histologic grade determine the treatment approaches of chondrosarcoma. The primary treatment modality of chondrosarcoma is surgical excision. Low-grade central chondrosarcoma can be treated with intralesional curettage, burring and surgical adjuvant application such as hydrogen peroxide [8]. (B2)
Tumors with intraarticular or soft tissue involvement, larger tumors, axial or pelvic tumors must be treated with wide excision. For the intermediate or high-grade chondrosarcoma, wide en bloc excision is the surgical approach of choice [9].
Chemotherapy:
Chemotherapy is generally not efficient in conventional chondrosarcoma. However, it may have a role in dedifferentiated chondrosarcomas containing a high-grade spindle cell component [10].(B2)
Radiation therapy:
After incomplete resection of high-risk chondrosarcomas, radiation therapy is indicated to improve the high local failure rates. These indications include locally recurrent tumors intermediate to high-grade tumors, and tumors in locations where surgical resection is challenging or limited. Definitive radiation can also be indicated for unresectable tumors [11].
Differential Diagnosis
- Chondromyxoid fibroma
- Enchondroma
- Chondroblastic osteosarcoma
- Fracture callus
Prognosis
Histological grade is the single most important predictor of local recurrence and metastasis. Low-grade chondrosarcomas, which grow insidiously and rarely metastasize, have a good prognosis. The 5-year survival of grade I chondrosarcomas is 83%. High-grade chondrosarcoma and dedifferentiated chondrosarcoma, by comparison, have an inferior prognosis due to the rapid growth of the tumor and the propensity for early metastasis [12]. The 5-year survival of grade II and III chondrosarcomas is of 53% [9].
Complications
Recurrence of the tumor
Distant metastases: the primary site of metastasis is the lung. The rate of metastasis varies according to the grade of chondrosarcoma [3].
- Low-grade: less than 10%
- Intermediate-grade: 10%–50%
- High-grade : 50%–70% [3].
Consultations
Orthopedics
Oncology
Deterrence and Patient Education
Patients and their families need to be educated on how to recognize the early signs and symptom of bone tumors. Patients with signs of bone pain, swelling of bones or joints, any palpable mass found on the bones, should seek early intervention. Treatment of chondrosarcoma is mainly surgical. Local recurrence can occur after surgery, so long term follow-up is recommended to monitor these patients closely.
Enhancing Healthcare Team Outcomes
Chondrosarcoma is ideally managed by an interprofessional team that consists of orthopedists, radiologists, surgical oncologists, oncologists, pathologists, and specialty care nurses. Correlation between gross, radiographic, and microscopic features of the lesion is crucial to establish the definitive diagnosis of chondrosarcoma. Postoperatively, patients require long term follow-up due to the possibility of tumor recurrence and distant metastases. The prognosis for patients with low-grade disease is excellent. Pharmacists review medications, check for drug-drug interactions, and provide patient education. Specialty care nurses in perianesthesia, operating room, orthopedics, and oncology are involved in monitoring patients, educating patients and their families, and providing updates to the team about the patient's condition. Thereby the team can improve outcomes for this condition. [Level 5]
Media
References
Thorkildsen J, Taksdal I, Bjerkehagen B, Haugland HK, Børge Johannesen T, Viset T, Norum OJ, Bruland Ø, Zaikova O. Chondrosarcoma in Norway 1990-2013; an epidemiological and prognostic observational study of a complete national cohort. Acta oncologica (Stockholm, Sweden). 2019 Mar:58(3):273-282. doi: 10.1080/0284186X.2018.1554260. Epub 2019 Jan 11 [PubMed PMID: 30632866]
Level 2 (mid-level) evidenceSangma MM, Dasiah S. Chondrosarcoma of a rib. International journal of surgery case reports. 2015:10():126-8. doi: 10.1016/j.ijscr.2015.03.052. Epub 2015 Mar 28 [PubMed PMID: 25841154]
Level 3 (low-level) evidenceNazeri E, Gouran Savadkoohi M, Majidzadeh-A K, Esmaeili R. Chondrosarcoma: An overview of clinical behavior, molecular mechanisms mediated drug resistance and potential therapeutic targets. Critical reviews in oncology/hematology. 2018 Nov:131():102-109. doi: 10.1016/j.critrevonc.2018.09.001. Epub 2018 Sep 12 [PubMed PMID: 30293700]
Level 3 (low-level) evidencevan Praag Veroniek VM, Rueten-Budde AJ, Ho V, Dijkstra PDS, Study group Bone and Soft tissue tumours (WeBot), Fiocco M, van de Sande MAJ. Incidence, outcomes and prognostic factors during 25 years of treatment of chondrosarcomas. Surgical oncology. 2018 Sep:27(3):402-408. doi: 10.1016/j.suronc.2018.05.009. Epub 2018 May 6 [PubMed PMID: 30217294]
Murphey MD, Walker EA, Wilson AJ, Kransdorf MJ, Temple HT, Gannon FH. From the archives of the AFIP: imaging of primary chondrosarcoma: radiologic-pathologic correlation. Radiographics : a review publication of the Radiological Society of North America, Inc. 2003 Sep-Oct:23(5):1245-78 [PubMed PMID: 12975513]
Ollivier L, Vanel D, Leclère J. Imaging of chondrosarcomas. Cancer imaging : the official publication of the International Cancer Imaging Society. 2003 Oct 22:4(1):36-8. doi: 10.1102/1470-7330.2003.0022. Epub 2003 Oct 22 [PubMed PMID: 18211859]
Varma DG, Ayala AG, Carrasco CH, Guo SQ, Kumar R, Edeiken J. Chondrosarcoma: MR imaging with pathologic correlation. Radiographics : a review publication of the Radiological Society of North America, Inc. 1992 Jul:12(4):687-704 [PubMed PMID: 1636034]
Level 2 (mid-level) evidenceLeerapun T, Hugate RR, Inwards CY, Scully SP, Sim FH. Surgical management of conventional grade I chondrosarcoma of long bones. Clinical orthopaedics and related research. 2007 Oct:463():166-72 [PubMed PMID: 17632422]
Level 2 (mid-level) evidenceGelderblom H, Hogendoorn PC, Dijkstra SD, van Rijswijk CS, Krol AD, Taminiau AH, Bovée JV. The clinical approach towards chondrosarcoma. The oncologist. 2008 Mar:13(3):320-9. doi: 10.1634/theoncologist.2007-0237. Epub [PubMed PMID: 18378543]
Cesari M, Bertoni F, Bacchini P, Mercuri M, Palmerini E, Ferrari S. Mesenchymal chondrosarcoma. An analysis of patients treated at a single institution. Tumori. 2007 Sep-Oct:93(5):423-7 [PubMed PMID: 18038872]
Level 2 (mid-level) evidenceSuit HD, Goitein M, Munzenrider J, Verhey L, Davis KR, Koehler A, Linggood R, Ojemann RG. Definitive radiation therapy for chordoma and chondrosarcoma of base of skull and cervical spine. Journal of neurosurgery. 1982 Mar:56(3):377-85 [PubMed PMID: 7057235]
Stevenson JD, Laitinen MK, Parry MC, Sumathi V, Grimer RJ, Jeys LM. The role of surgical margins in chondrosarcoma. European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2018 Sep:44(9):1412-1418. doi: 10.1016/j.ejso.2018.05.033. Epub 2018 Jun 8 [PubMed PMID: 29929901]