Introduction
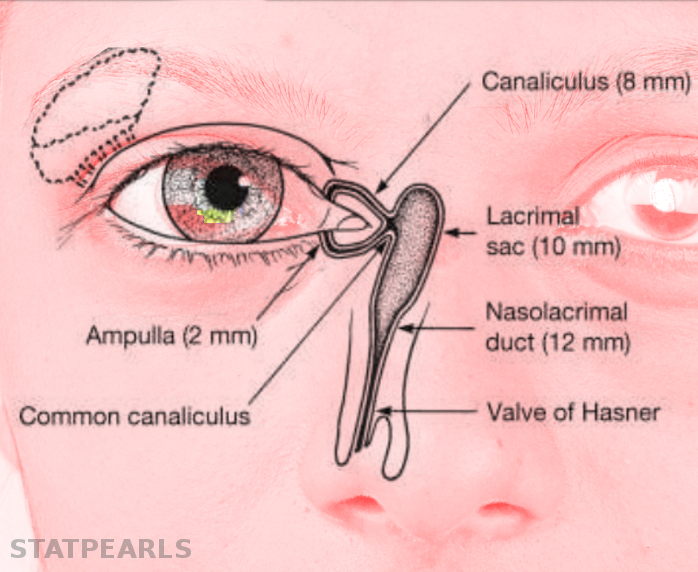
The lacrimal duct system transmits tears from the surface of the eye to the nasal cavity. Tears enter the duct system at the lacrimal punctae and conduct through canaliculi within the eyelids. The canaliculi drain into the lacrimal sac. Tears continue down the intra-osseous lacrimal duct where they exit into the nasal cavity at the inferior meatus. Obstruction of the lacrimal duct system results in epiphora or excessive tearing. This condition is particularly common in children but is also common in adults.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The lacrimal duct system comprises upper and lower sections. Tears first enter the upper system at the lacrimal punctum. This visible structure contains a 0.2 to 0.3 mm opening at the mucocutaneous border on each of the upper and lower eyelids. The upper and lower lid punctae sit 5 mm and 6 mm, respectively, lateral to the medial canthal edge. The punctae typically oppose each other when the eyelids are closed. After entering the punctae, tears conduct through the canicular system. The 2 mm long vertical canaliculus extends perpendicular from the eyelid margin before widening to form the ampulla. At the ampulla, the canaliculus makes a 90-degree turn medially.[1] The canaliculi then continue 8 mm horizontally, following the arc of the eyelid. In 90% of individuals, the lower and upper canaliculi join proximal to the lacrimal sac, forming a single 3 to 5 mm long common canaliculus. For the remaining 10% of people, the canaliculi enter the lacrimal sac directly and independently. Just proximal to the lacrimal sac, the common canaliculus dilates to form the sinus of Maier. Tissue in-foldings form the valve of Rosenmuller, separating the common canaliculus from the lacrimal sac.[2] This separation prevents reflux through the lacrimal system.
The lower system comprises the lacrimal sac and the lacrimal duct. The lacrimal sac is anterior to the orbital septum, nestled in its own fascia in the lacrimal fossa. The lacrimal crest of the maxillary bone forms the anterior border of the lacrimal fossa. The lacrimal crest of the small lacrimal bone forms the posterior border of the lacrimal fossa. The suture line joining the lacrimal and maxillary bones marks the medial border of the lacrimal fossa.[3]
The site of insertion of the common canaliculus into the lacrimal sac serves as a marker of the division. The lacrimal sac fundus lies above the insertion, and the body lies below. The lacrimal sac is 12 to 15 mm long, 2 to 3 mm wide, 4 to 6 mm deep, and is predominantly in a collapsed position.[4]
The tendinous insertions of the orbicularis muscle bind the lacrimal sac anteriorly and posteriorly, aiding in the movement of tears. Posterior to the sac, the deep heads of the pre-tarsal and preseptal orbicular muscles insert. Anterior to the sac, the superficial heads of the pre-tarsal and preseptal orbicularis muscles insert onto the anterior crest of the lacrimal fossa. Together, these insertions help squeeze the lacrimal sac to move tears forward through the system.[5]
In the coronal plane, the lacrimal duct extends infero-posteriorly from the sac at an angle between 15 and 30 degrees. From the midsagittal plane, it extends infero-laterally at an angle of about 5 degrees. The intraosseous duct transits through the maxillary bone. Its medial border is formed by the ethmoid bone superiorly and the inferior turbinate inferiorly. It is about 12 mm long and 3 to 5 mm wide. It opens into the inferior meatus at the valve of Hasner. The ostium’s location is variable, but it is generally 25 to 35 mm posterior to the external nares and 4 to 18 mm above the nasal floor.
Embryology
The nasolacrimal duct forms from a cord of ectodermal cells beginning at the seventh week of development. The surface ectodermal cord joins with a growing cord of epithelial cells extending from the nasal cavity. The cord bifurcates in the canthal area, forming early canaliculi. These projections reach the lid margins at 12 weeks.[6] By seven months' gestation, the papilla and punctual portions of the nasolacrimal duct system are fully formed and patent. The nasal lacrimal duct system canalizes along its extent simultaneously. The last portion to canalize, and the most frequent site of obstruction, is the opening to the inferior meatus of the nasal cavity. After birth, the size of the nasolacrimal duct system continues to increase relative to the surrounding facial structures. The most growth occurs in the first six months after birth.[7]
Blood Supply and Lymphatics
The superior and inferior palpebral arteries supply the canaliculi with blood. These are terminal branches of the ophthalmic artery. The angular vessels branching off of the facial artery run superficially and supply the lacrimal sac.
Nerves
Cranial nerve VII provides motor innervation to the orbicularis muscle. This muscle helps pump tears through the nasolacrimal duct system. The fifth cranial nerve provides sensation superficial to the region of the nasolacrimal duct system.
Muscles
The superficial and deep heads of the pre-tarsal tendons of the orbicularis muscle control the pumping action of the lacrimal system. The tendon heads juxtaposed with the cananiculi and the lacrimal sac. Therefore, when the orbicularis muscle contracts, so do the tendon heads, and in concert so does the lacrimal system. This contraction facilitates the capillary action of the lacrimal puncta and lacrimal system that directs the flow of tears to the nasal cavity.
Physiologic Variants
For people of East Asian descent, the medial wall of the lacrimal sac is formed predominantly by the thicker maxillary bone rather than the lacrimal bone.[8] It is crucial to keep this in mind when forming the ostium during a dacryocystorhinostomy because the maxillary bone is thicker than the lacrimal bone.
In 10% to 15% of individuals, the ethmoid air cells may extend anteriorly beyond the posterior lacrimal crest. During a dacryocystorhinostomy, take care to avoid aberrant entrance into the air cells.
Clinical Significance
Nasolacrimal duct obstruction is a common problem, especially in children. Up to 1 in 9 newborns have a congenital nasolacrimal duct obstruction.[9] It most often leads to excessive tearing and epiphora. Probing of the system and sometimes stenting are interventions that open the system and permit tears to flow normally.
It is also a potential site of infection termed dacryocystitis. This condition is more common in children, and in the most severe sequelae can lead to orbital cellulitis. Dacryocystitis can be acute or chronic; it can also be congenital or acquired. When present, there is medial canthal swelling of dacryocystitis, usually below the medial canthal tendon.
Media
References
Takahashi Y, Kakizaki H, Nakano T, Asamoto K, Ichinose A, Iwaki M. Anatomy of the vertical lacrimal canaliculus and lacrimal punctum: a macroscopic study. Ophthalmic plastic and reconstructive surgery. 2011 Sep-Oct:27(5):384-6. doi: 10.1097/IOP.0b013e318219a54b. Epub [PubMed PMID: 21562437]
Tucker NA, Tucker SM, Linberg JV. The anatomy of the common canaliculus. Archives of ophthalmology (Chicago, Ill. : 1960). 1996 Oct:114(10):1231-4 [PubMed PMID: 8859082]
Ali MJ, Schicht M, Paulsen F. Morphology and morphometry of lacrimal drainage system in relation to bony landmarks in Caucasian adults: a cadaveric study. International ophthalmology. 2018 Dec:38(6):2463-2469. doi: 10.1007/s10792-017-0753-6. Epub 2017 Dec 8 [PubMed PMID: 29222730]
Alherabi A, Marglani O, Herzallah I, Shaibah H, Alaidarous T, Alkaff H, Farooq M, Bamahfouz A, Al-Khatib T, Marzouki H. Endoscopic anatomy of the lacrimal sac for dacryocystorhinostomy. A cadaveric study. Saudi medical journal. 2017 Mar:38(3):245-250. doi: 10.15537/smj.2017.3.15937. Epub [PubMed PMID: 28251218]
Tong J, Lopez MJ, Patel BC. Anatomy, Head and Neck: Eye Orbicularis Oculi Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 28722936]
Sevel D. Development and congenital abnormalities of the nasolacrimal apparatus. Journal of pediatric ophthalmology and strabismus. 1981 Sep-Oct:18(5):13-9 [PubMed PMID: 7299606]
Moscato EE, Kelly JP, Weiss A. Developmental anatomy of the nasolacrimal duct: implications for congenital obstruction. Ophthalmology. 2010 Dec:117(12):2430-4. doi: 10.1016/j.ophtha.2010.03.030. Epub 2010 Jul 24 [PubMed PMID: 20656354]
Level 2 (mid-level) evidenceYe H, Feng Y, Yin S. [Anatomy study of the lacrimal bone in dacryocystorhinostomy]. Lin chuang er bi yan hou tou jing wai ke za zhi = Journal of clinical otorhinolaryngology, head, and neck surgery. 2007 Sep:21(17):774-6 [PubMed PMID: 17993012]
Sathiamoorthi S, Frank RD, Mohney BG. Incidence and clinical characteristics of congenital nasolacrimal duct obstruction. The British journal of ophthalmology. 2019 Apr:103(4):527-529. doi: 10.1136/bjophthalmol-2018-312074. Epub 2018 Jun 6 [PubMed PMID: 29875230]