Anatomy, Bony Pelvis and Lower Limb: Femoral Artery
Anatomy, Bony Pelvis and Lower Limb: Femoral Artery
Introduction
The femoral artery is a large blood vessel that provides oxygenated blood to lower extremity structures and in part to the lower anterior abdominal wall. The common femoral artery arises as a continuation of the external iliac artery after it passes under the inguinal ligament. The femoral artery, vein, and nerve all exist in the anterior region of the thigh known as the femoral triangle, just inferior to the inguinal ligament. Within the femoral triangle, the anatomical relationship from medial to lateral is femoral vein, common femoral artery, and femoral nerve. The artery and vein are both contained within the femoral sheath while the nerve is not.[1] The common femoral artery bifurcates and gives off the deep femoral artery and continues distally in the medial thigh as the superficial femoral artery. The superficial femoral artery becomes the popliteal artery at the level of the adductor hiatus which is located in the distal thigh just above the knee. The deep femoral artery terminates as perforating arteries in the thigh which provide oxygenated blood to the thigh musculature and hip.[2]
Besides providing oxygen-rich blood to the lower extremity tissues, the common femoral artery is clinically significant because it is a common site of peripheral arterial disease complications such as claudication and critical limb ischemia. Additionally, the common femoral artery serves as a preferred site for percutaneous catheterization for a wide variety of endovascular procedures. A thorough understanding of the anatomy and potential variations of the femoral artery is crucial for surgeons and interventionalists in order to avoid complications.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The common femoral artery forms as a continuation of the external iliac artery inferior to the level of the inguinal ligament. The common femoral artery is located just medial to the midpoint of the inguinal ligament in the inguinal crease region. The two bony landmarks useful for identifying the inguinal ligament are the anterior superior iliac spine and pubic symphysis. The average common femoral artery measures approximately 4 cm in length and lies just anterior to the femoral head [3]. The average length and diameter of the common femoral artery can be quite variable depending on individual characteristics such as height, weight, sex and body surface area[3]. According to one study, the average common femoral artery diameter is 6.19 mm +/- 1.2 mm [3]. Vascular branches arising from the common femoral artery may include the superficial inferior epigastric artery, superficial circumflex artery, superficial external pudendal artery and the medial and/or lateral circumflex arteries.[4][5][7]
Distal to the origin of these smaller branches, the common femoral artery bifurcates into the deep femoral (or profunda femoris) and superficial femoral artery.
The superficial femoral artery plays a crucial role in delivering oxygenated blood to the entire lower leg. Before entering the adductor canal, it gives off the descending genicular artery that supplies part of the knee.[5] As the superficial femoral artery traverses the adductor canal within the thigh, it gives off minor branches to the muscles of the thigh. Once it emerges from the adductor hiatus more posteriorly, it becomes the popliteal artery which provides oxygen-rich blood to the rest of the knee compartment and distal lower extremity and foot via the anterior tibial artery and tibioperoneal trunk.
The femoral vein courses posterior to the femoral artery through the adductor canal.
The deep femoral artery gives rise to medial and lateral circumflex arteries that supply the femur and hip region before it dives deep into the thigh compartment and terminates as perforating deep tissue branches.[6]
Embryology
At the 6-mm embryologic stage, the umbilical artery gives rise to the sciatic artery which becomes the dominant blood supply to the developing lower limb. Subsequently, the iliofemoral system begins to form as the sciatic artery regresses during the 6-33 mm stage.[12] If the sciatic artery fails to regress, it can lead to complications later in life such as early atherosclerotic disease, thromboembolic events or aneurysm formation.[11]
The vasculature establishes its adult pattern by the 8th week of embryologic development. Another rare vascular anomaly associated with abnormal embryological development is a duplicated superficial femoral artery.[12]
Blood Supply and Lymphatics
The deep veins of the leg are typically named in accordance with the artery and drain the lower extremity musculature. The superficial veins are responsible for draining the lower extremity cutaneous circulation. All of the superficial veins eventually drain into the saphenous system which empties into the common femoral vein in the proximal thigh. The femoral vein courses posterior to the femoral artery as it courses through the adductor canal.[8]
The primary lymphatic chain that drains the lower extremities and groin is the most medially located structure within the femoral triangle.
Nerves
The L2, L3, and L4 nerve roots give rise to the femoral nerve which then descends inferiorly and passes posterior to the inguinal ligament. In the femoral triangle, the femoral nerve is located lateral to the femoral artery and exterior to the femoral sheath.[7] The femoral nerve delivers motor innervation to the anterior muscles of the thigh (quadriceps, sartorius, iliacus, and pectineus). It also supplies cutaneous sensation to the anterior thigh and anteromedial aspect of the leg.[5] The surgeon must exercise care to avoid injuring the femoral nerve while performing femoral artery percutaneous catheterization.[8]
Muscles
After branching off of the deep femoral artery, the medial circumflex artery courses along the posterior aspect of the femur and supplies blood to the thigh adductors (longus, magnus, and brevis), gracilis, pectineus as well as the primary blood supply to the hip joint.[7][9] The lateral circumflex courses laterally and supplies oxygenated blood to the major knee extensor group including vastus lateralis, vastus intermedius, and rectus femoris. Vastus medialis is supplied in part by both the superficial femoral artery and deep femoral artery. The perforating arteries of the deep femoral artery supply the four hamstring muscles (semitendinosus, semimembranosus, short and long head of biceps.[7] After exiting the adductor canal, the superficial femoral artery continues distally as the popliteal artery which serves the entire calf and foot with oxygen-rich blood.
Physiologic Variants
Although many benign variants of the femoral artery exist, there are some that are considered to be rare and potentially dangerous to the patient. The origins of smaller arteries off of the femoral artery can be highly variable. Less common abnormalities include a duplicated or absent deep femoral artery, lateral and medial circumflex arteries originating from the common or superficial femoral artery instead of the deep femoral artery.[12][7] The clinical significance of this variant is that the common femoral artery may appear to trifurcate instead of bifurcate.[9] The precise level of the common femoral artery bifurcation may vary from person to person and often does not align with the inguinal crease. Ultrasound examination is routinely used for safe and effective vascular access. Another potential abnormality of the femoral artery is the presence of a persistent sciatic artery. It occurs when the embryonic vessel fails to regress and thus remains the dominant feeding vessel to the lower extremity. Serious limb ischemia complications may arise due to higher rates of an aneurysm and thromboembolic complications in this unusual variant.[10] Finally, an even more unusual variant is the presence of duplicate superficial femoral arteries and knowledge of this plays a vital role in preprocedural planning.[11]
Surgical Considerations
The region of the anterior thigh that lies just inferior to the inguinal ligament is termed the femoral triangle. Within the femoral triangle, there is discrete organization of key structures, and a thorough understanding of these anatomical relationships is necessary to avoid inadvertent injury to the femoral artery, vein, and nerve during procedures such as percutaneous catheterization, hernia repairs and nerve blocks.
During percutaneous vascular access procedures, the common femoral artery is often desirable as an access point because it is suitable for large-diameter catheters and sheaths to be placed which allows for a wide variety of endovascular procedures. It is essential to access the common femoral artery just superior to the bifurcation of the superficial and deep femoral branches to reduce complications. Although the inguinal crease is frequently used as an initial landmark, ultrasound guidance is more precise when determining the relevant anatomy, specifically the common femoral artery bifurcation and inferior epigastric artery. Arteriotomy site should be between the common femoral artery bifurcation and the inferior epigastric artery. Fluoroscopy is also useful to identify the femoral head which is often a useful anatomical landmark for accessing the common femoral artery.[2]
Endovascular intervention is common in patients with clinically significant peripheral arterial disease. The atherosclerotic burden most afflicts the superficial femoral artery, common femoral artery and/or the popliteal artery. Patients with heavily calcified arteries exhibiting clinical signs and symptoms such as claudication or critical limb ischemia may require endovascular angioplasty (ballooning) with or without stenting to improve distal blood flow. If an artery is unable to be repaired endovascularly, vascular surgical consult may be necessary for an arterial bypass procedure.[11]
Clinical Significance
In individuals with peripheral arterial disease (PAD) the most common sites of involvement are the superficial femoral artery and the common femoral artery. Symptoms that indicate femoral artery disease may include claudication (pain or cramping sensation) in the thighs and calves, cold, discolored extremities, poor wound healing below the lesion, change in sensation, and in end-stage disease, gangrene or necrosis of the digits. Chronic health conditions that increase a patient’s risk of PAD include age, obesity, diabetes, hypertension, hyperlipidemia, coronary atherosclerotic disease, vasculitis, sedentary lifestyle, and smoking. It is worth noting that the absence of these risk factors does not preclude a patient from having PAD.[7]
In instances where the common and superficial femoral arteries are chronically occluded, extensive collaterals may be present between the deep femoral artery, and thus distal blood flow is more robust than expected.[12] Prior to any percutaneous endovascular intervention, a comprehensive clinical evaluation including palpating pulses, visual evaluation of the extremity, Doppler ultrasound, ankle-brachial indices, and patient symptoms should take place. If warranted, a CT-angiogram (CTA) of the lower extremities may be performed to better evaluate the extent of atherosclerotic disease and assist in further management.[7]
Other Issues
The course of the common femoral artery over the femoral head is important because it acts as a hard surface to which manual pressure can be effectively applied after percutaneous catheterization. Accessing more superiorly or inferiorly can make hemostasis difficult to achieve and lead to greater complications. Complications of femoral artery access include hematomas, pseudoaneurysms, injury to the femoral nerve, retroperitoneal hemorrhage, arteriovenous fistulas, and distal embolization of atherosclerotic plaque. Hematomas and hemorrhage may occur with inadequate thrombosis of the arteriotomy and present in the groin or flank.[3] The level of the inferior epigastric artery is generally accepted as the superior boundary of potential arteriotomy sites. More superior than this places the patient at increased risk of bleeding into the retroperitoneal space. Alternatively, arteriotomies of the superficial femoral artery are at increased risk of avoidable complications.[13][14] Checking for complications post-procedurally and educating the patient about concerning signs for which they should seek immediate medical attention is of utmost importance.
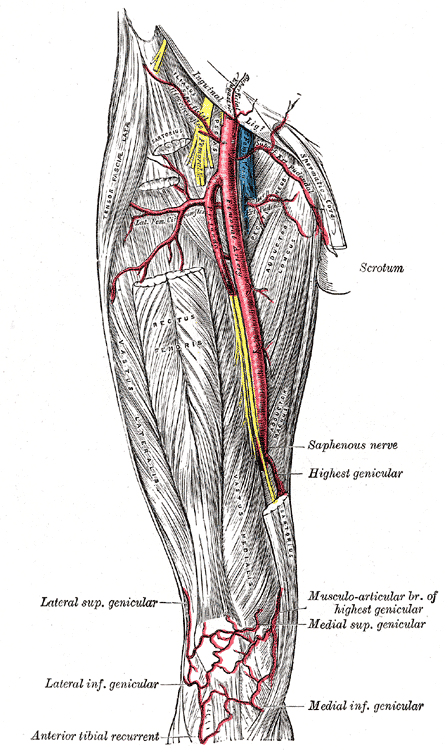
Media
(Click Image to Enlarge)
References
Weledji EP, Elong FA. Lipoma in the femoral triangle. JRSM open. 2017 Apr:8(4):2054270417692730. doi: 10.1177/2054270417692730. Epub 2017 Apr 3 [PubMed PMID: 28491332]
Hwang JY. Doppler ultrasonography of the lower extremity arteries: anatomy and scanning guidelines. Ultrasonography (Seoul, Korea). 2017 Apr:36(2):111-119. doi: 10.14366/usg.16054. Epub 2017 Jan 18 [PubMed PMID: 28219004]
Ahn HY, Lee HJ, Lee HJ, Yang JH, Yi JS, Lee IW. Assessment of the optimal site of femoral artery puncture and angiographic anatomical study of the common femoral artery. Journal of Korean Neurosurgical Society. 2014 Aug:56(2):91-7. doi: 10.3340/jkns.2014.56.2.91. Epub 2014 Aug 31 [PubMed PMID: 25328644]
Ogami K, Murata H, Sakai A, Sato S, Saiki K, Okamoto K, Manabe Y, Hara T, Tsurumoto T. Deep and superficial circumflex iliac arteries and their relationship to the ultrasound-guided femoral nerve block procedure: A cadaver study. Clinical anatomy (New York, N.Y.). 2017 Apr:30(3):413-420. doi: 10.1002/ca.22852. Epub 2017 Mar 9 [PubMed PMID: 28192858]
Gocmen-Mas N, Aksu F, Edizer M, Magden O, Tayfur V, Seyhan T. The arterial anatomy of the saphenous flap: a cadaveric study. Folia morphologica. 2012 Feb:71(1):10-4 [PubMed PMID: 22532178]
Zlotorowicz M, Czubak-Wrzosek M, Wrzosek P, Czubak J. The origin of the medial femoral circumflex artery, lateral femoral circumflex artery and obturator artery. Surgical and radiologic anatomy : SRA. 2018 May:40(5):515-520. doi: 10.1007/s00276-018-2012-6. Epub 2018 Apr 12 [PubMed PMID: 29651567]
Kasapis C, Gurm HS. Current approach to the diagnosis and treatment of femoral-popliteal arterial disease. A systematic review. Current cardiology reviews. 2009 Nov:5(4):296-311. doi: 10.2174/157340309789317823. Epub [PubMed PMID: 21037847]
Level 1 (high-level) evidenceEl-Ghanem M, Malik AA, Azzam A, Yacoub HA, Qureshi AI, Souayah N. Occurrence of Femoral Nerve Injury among Patients Undergoing Transfemoral Percutaneous Catheterization Procedures in the United States. Journal of vascular and interventional neurology. 2017 Jun:9(4):54-58 [PubMed PMID: 28702121]
Reardon CM, O'Ceallaigh S, O'Sullivan ST. An anatomical study of the superficial inferior epigastric vessels in humans. British journal of plastic surgery. 2004 Sep:57(6):515-9 [PubMed PMID: 15308397]
Wang B, Liu Z, Shen L. Bilateral persistent sciatic arteries complicated with chronic lower limb ischemia. International journal of surgery case reports. 2011:2(8):309-12. doi: 10.1016/j.ijscr.2011.07.010. Epub 2011 Oct 12 [PubMed PMID: 22096762]
Level 3 (low-level) evidenceHapugoda S, Hsu CC, Kwan GN, Watkins TW, Rophael JA. Duplication of the superficial femoral artery: comprehensive review of imaging literature and insight into embryology. Acta radiologica open. 2016 Jul:5(7):2058460116659098. doi: 10.1177/2058460116659098. Epub 2016 Jul 26 [PubMed PMID: 27504194]
Kruse RR, Doomernik DE, Maltha KV, Kooloos JGM, Kozicz TL, Reijnen MMPJ. Collateral artery pathways of the femoral and popliteal artery. The Journal of surgical research. 2017 May 1:211():45-52. doi: 10.1016/j.jss.2016.11.068. Epub 2016 Dec 14 [PubMed PMID: 28501130]
Sherev DA, Shaw RE, Brent BN. Angiographic predictors of femoral access site complications: implication for planned percutaneous coronary intervention. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2005 Jun:65(2):196-202 [PubMed PMID: 15895402]
Level 2 (mid-level) evidenceEllis SG, Bhatt D, Kapadia S, Lee D, Yen M, Whitlow PL. Correlates and outcomes of retroperitoneal hemorrhage complicating percutaneous coronary intervention. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2006 Apr:67(4):541-5 [PubMed PMID: 16547938]
Level 2 (mid-level) evidence