Introduction
Asthma is becoming a more prevalent disease since the early 1990s. From 1982 to 1992, the rate of asthma jumped from 34.7 to 49.4 per thousand.[1] The prevalence of asthma in the USA is around 8%.[2] There also has been some mixed trends around the world where different countries have either had increasing cases or have been stagnant.[3] In children, asthma is presented predominantly in males until the age of 20, where the disease equally prevalent. Differences in childhood can be due to atopy, or because boys have a reduced airway size compared to girls.[4] There is a family history component of asthma, as well. However, the genes responsible for inheriting asthma remain unidentified. There are mechanisms of the phenotype of asthma that has a strong correlation of being inherited, but the mechanism is more complex, as asthma does not follow a Mendelian pattern. Asthma is most likely transmitted by multiple genes, with some variation of locus heterogeneity and polygenic inheritance leading to asthma expression being multifaceted. Atopy or IgE antibodies attack specific antigens or pollutants, which can contribute to the disease. Research has shown that asthma was closely related to the total IgE serum level.[5] Enhanced IgE response to environmental factors such as house dust mites, animal allergens, mold, farm animals, have contributed to sensitize asthma exacerbating its symptoms and attributing to increased airway reactivity. The reason being is that there is increased exposure to these allergens, but less data is available on the causality. Air pollution and the causation of asthma are also less clear; however, there is a relationship with smoking and the increased risk of asthma.[6] Interestingly enough, obesity showed a positive linear relationship between asthma and increased BMI.[7] More research needs to be done to have a clearer picture of the multifactorial disease.
Organ Systems Involved
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Organ Systems Involved
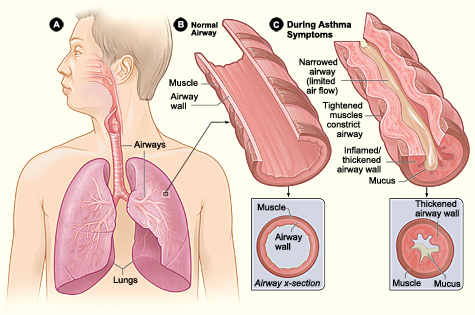
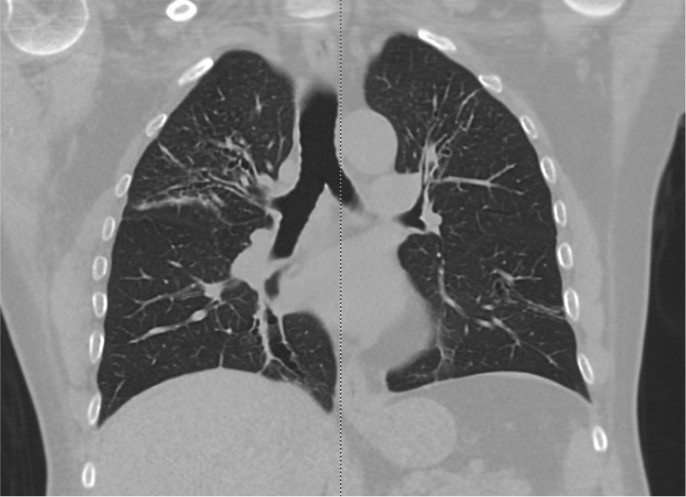
The organ system affected by asthma is the lungs. The lungs consist of lobes and segments, with the right lung having ten segments and the left lung having eight or nine, depending on the division of the lobe.[8] Anatomically, the respiratory system falls into two zones, characterized by the conducting zone and the respiratory zone. The conducting zone extends from the nose to the bronchioles, and the respiratory zone where gas exchange takes place is from the alveolar duct to the alveoli.[9] Asthma is primarily involved in the bronchial tree, with its primary job to distribute air throughout the lungs until reaching the alveolar sacs. The bronchi stem from the end of the trachea, which divides into left and right bronchi. The right bronchus has a wider diameter and lies more vertically, while the left bronchus is smaller and more horizontal. The bronchi then divide into secondary and tertiary bronchi. The bronchi contain smooth muscle and elastic fibers to maintain their wall integrity, which change based on the contraction and relaxation of smooth muscle by inflammatory mediators, bronchoconstrictor, or bronchodilators.[10] As one progresses further from the bronchi to the alveoli, there are much more smooth muscle fibers involved.[9] In normal respiratory physiology, lung compliance is the willingness for the lungs to distend, while elastance is the ability of the lungs to return to their resting position. In patients with asthma, the physiologic mechanism changes due to inflammation, decreasing the radius of the airway.[11] All of these mechanisms together change the compliance of the lungs slightly to increase the work of breathing.
Mechanism
There are two phases of an asthma exacerbation, which include the early phase and the late phase. The early phase is initiated by IgE antibodies that are sensitized and released by plasma cells. These antibodies respond to certain triggers in the environment, such as the risk factors listed above. IgE antibodies then bind to high-affinity mast cells and basophils. When a pollutant or risk factor gets inhaled, the mast cells release cytokines and eventually de-granulate. Released from mast cells are histamine, prostaglandins, and leukotrienes. These cells, in turn, contract the smooth muscle and cause airway tightening.[12] Th2 lymphocytes play an integral role where they produce a series of interleukins (IL-4, IL-5, IL-13) and GM-CSF, which aid in communication with other cells and sustain inflammation. IL-3 and IL-5 help eosinophils and basophils survive. IL-13 is involved in remodeling, fibrosis, and hyperplasia.[13] Within the next several hours, the late phase occurs, in which eosinophils, basophils, neutrophils, and helper and memory T-cells all localize to the lungs as well, which perform bronchoconstriction and cause inflammation. Mast cells also play an essential role in bringing the late-phase reactants to the inflamed sites.[14] It is critical to recognize both of these two mechanisms to target therapy and relieve both bronchoconstriction and inflammation, depending on the severity of the disease. Interestingly, those with a thicker airway over time have a longer disease duration due to a narrower airway.[15] As a result of inflammation and bronchoconstriction, there is an intermittent airflow obstruction, resulting in increased work of breathing.
Airway hyperresponsiveness is a crucial feature of asthma; this is an exaggerated bronchoconstrictor response, usually to different stimuli. There are a variety of mechanisms leading to airway hyperresponsiveness. Some explanations are due to increased histamine from mast cells or increase airway smooth muscle mass. Also, there is an increased vagal tone and increased intracellular free calcium that further enhances airway smooth muscle cell contractility.[15] To assess airway hyperresponsiveness, bronchial provocation tests are used to determine the severity.[16] This aspect is clinically significant because the presence of airway hyperresponsiveness is associated with a greater decline in lung function and increased risk for the development and exacerbation of asthma from childhood to adulthood.[17] Therefore, targeted treatment can be employed early to combat asthma and hyperresponsiveness. All of these mechanisms together change the compliance of the lungs slightly to increase the work of breathing. In combination with inflammation, granular white blood cells, exudate, and mucous occupying the bronchiolar trees, it can be increasingly difficult for a person to breathe normally. The number of myofibroblasts, which give rise to collagen, will cause an increase in the epithelium, which narrows the smooth muscle layer and lamina reticularis.[18] As a result, there is an increased thickening of the basement membrane. A person can have irreversible obstruction of airflow, which is believed to be due to airway remodeling.[19]
Remodeling occurs by epithelial cells transitioning to mesenchymal, increasing the smooth muscle content. Epithelial cells lose their cell adhesion and functional polarity with tight junctions, reformatting their cells to develop into mesenchymal cells.[18] Additionally, eosinophils can further exacerbate airway remodeling due to their release of TGF-B and cytokines by interactions with mast cells. These mechanisms of airway remodeling may worsen inflammation and aggravate asthma over time if not treated and managed correctly.[15]
Related Testing
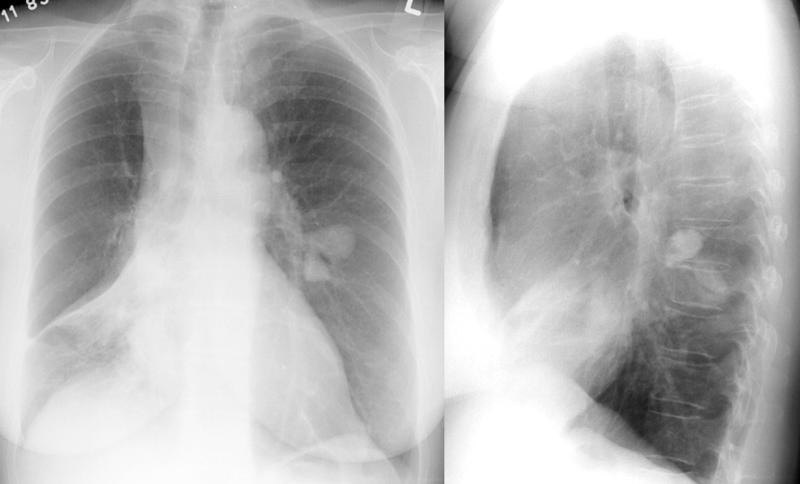
To diagnose asthma, clinicians can do a variety of tests. Tests must determine: expiratory airflow limitation, documentation of reversible obstruction, and rule out any exclusion of an alternative diagnosis. Assessing the patient’s obstruction via spirometry and checking for a reversible change after a bronchodilator is suggestive of the diagnosis of asthma. By using spirometry, physicians can diagnose asthma as well as the severity of obstruction.[20] The definition of the obstruction of air is spirometry of FEV1 less than 0.8, and the FEV1/FVC ratio is less than 0.70. The worse the asthma is, the lower the number is for FEV1 and the FEV1/FVC ratio. Another method of testing, if spirometry is normal, is bronchoprovocation testing with methacholine. Methacholine is a muscarinic agonist, which in the lungs constricts smooth muscle via M1, M2, and M3 receptors.[21] Methacholine can determine the severity of bronchoconstriction. Allergy testing is not necessarily useful in diagnosing asthma, but it can help identify certain triggers that worsen it.
Clinical Significance
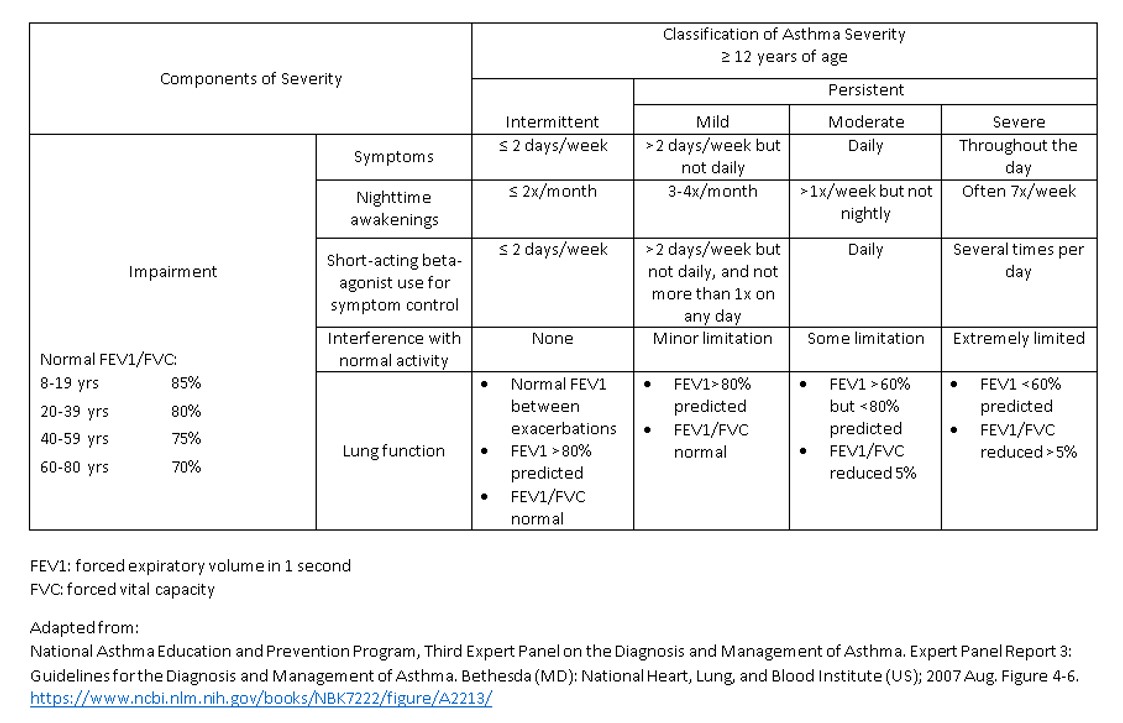
Asthma can paint a slightly different clinical picture, and clinicians must identify them. Asthmatic patients can usually have but are not limited to, wheezing, shortness of breath, and a cough, which is often worse at night. There are various triggers that intensify asthma. Such triggers are cold air, exercise, and the pollutants listed above. Other non-specific symptoms that could suggest a severe obstruction can be tachypnea, tachycardia, or a patient seated in a tripod position. Asthma can be a severe disease if not treated and managed correctly. Since there are two phases of asthma, it is essential to try to target and decrease bronchoconstriction, inflammation, and airway remodeling. Asthma is defined in different stages depending on spirometry and/or clinical indications. There are four stages regarding the severity of asthma, intermittent, mild, moderate, and severe. Depending on the specific stage of asthma, treatment and management change. Intermittent asthma occurs when one has symptoms less than two days a week and nighttime awakenings less than two times a month. Mild asthma consists of having episodes more than two days a week (but not daily), while there are nighttime awakenings of 3 to 4 times a month. Moderate asthma is where the patient is symptomatic daily and has nighttime awakenings greater than once a week but not nightly. Severe asthma is when a patient is symptomatic throughout the day and often has nighttime awakenings more than seven times within a week. Based on these criteria, correct treatment can be administered to decrease the symptoms of the patient. The most common medications used are short-acting beta-agonists, long-acting beta-agonists, muscarinic antagonists, and inhaled and systemic glucocorticoids. The idea behind a beta-agonist is to try to bronchodilate the patient’s lungs when they become constricted during an asthma attack. The mechanism behind beta-agonists is that they are G protein receptors that activate cAMP. cAMP then activates smooth muscle relaxation by a mechanism not fully understood. Also, a glucocorticoid may be used to decrease the inflammation and remodeling of the lungs. The primary mechanism of a glucocorticoid is to increase the production of IL-10. IL-10 inhibits inflammatory cytokines, T-cell activation, and different white cells such as mast cells and eosinophils.[22] These effects decrease inflammation and help the patient breathe better in the short and long term. Muscarinic antagonists block the inflammatory effect by diminishing the attraction and life of inflammatory cells, diminishing cytokine release.[23] Muscarinic antagonists can be paired with a beta-agonist or glucocorticoid for a synergistic effect.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC. Surveillance for asthma--United States, 1980-1999. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C. : 2002). 2002 Mar 29:51(1):1-13 [PubMed PMID: 12420904]
Centers for Disease Control and Prevention (CDC). Vital signs: asthma prevalence, disease characteristics, and self-management education: United States, 2001--2009. MMWR. Morbidity and mortality weekly report. 2011 May 6:60(17):547-52 [PubMed PMID: 21544044]
Maio S, Baldacci S, Carrozzi L, Pistelli F, Angino A, Simoni M, Sarno G, Cerrai S, Martini F, Fresta M, Silvi P, Di Pede F, Guerriero M, Viegi G. Respiratory symptoms/diseases prevalence is still increasing: a 25-yr population study. Respiratory medicine. 2016 Jan:110():58-65. doi: 10.1016/j.rmed.2015.11.006. Epub 2015 Nov 14 [PubMed PMID: 26614595]
Weiss ST, Gold DR. Gender differences in asthma. Pediatric pulmonology. 1995 Mar:19(3):153-5 [PubMed PMID: 7792116]
Burrows B, Martinez FD, Halonen M, Barbee RA, Cline MG. Association of asthma with serum IgE levels and skin-test reactivity to allergens. The New England journal of medicine. 1989 Feb 2:320(5):271-7 [PubMed PMID: 2911321]
Gilliland FD, Islam T, Berhane K, Gauderman WJ, McConnell R, Avol E, Peters JM. Regular smoking and asthma incidence in adolescents. American journal of respiratory and critical care medicine. 2006 Nov 15:174(10):1094-100 [PubMed PMID: 16973983]
Camargo CA Jr, Weiss ST, Zhang S, Willett WC, Speizer FE. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Archives of internal medicine. 1999 Nov 22:159(21):2582-8 [PubMed PMID: 10573048]
Chaudhry R, Bordoni B. Anatomy, Thorax, Lungs. StatPearls. 2023 Jan:(): [PubMed PMID: 29262068]
Patwa A, Shah A. Anatomy and physiology of respiratory system relevant to anaesthesia. Indian journal of anaesthesia. 2015 Sep:59(9):533-41. doi: 10.4103/0019-5049.165849. Epub [PubMed PMID: 26556911]
Amador C, Weber C, Varacallo MA. Anatomy, Thorax, Bronchial. StatPearls. 2025 Jan:(): [PubMed PMID: 30726038]
Grinnan DC, Truwit JD. Clinical review: respiratory mechanics in spontaneous and assisted ventilation. Critical care (London, England). 2005 Oct 5:9(5):472-84 [PubMed PMID: 16277736]
Liu MC, Hubbard WC, Proud D, Stealey BA, Galli SJ, Kagey-Sobotka A, Bleecker ER, Lichtenstein LM. Immediate and late inflammatory responses to ragweed antigen challenge of the peripheral airways in allergic asthmatics. Cellular, mediator, and permeability changes. The American review of respiratory disease. 1991 Jul:144(1):51-8 [PubMed PMID: 2064141]
Zhu Z, Homer RJ, Wang Z, Chen Q, Geba GP, Wang J, Zhang Y, Elias JA. Pulmonary expression of interleukin-13 causes inflammation, mucus hypersecretion, subepithelial fibrosis, physiologic abnormalities, and eotaxin production. The Journal of clinical investigation. 1999 Mar:103(6):779-88 [PubMed PMID: 10079098]
Level 3 (low-level) evidenceStewart AG, Tomlinson PR, Fernandes DJ, Wilson JW, Harris T. Tumor necrosis factor alpha modulates mitogenic responses of human cultured airway smooth muscle. American journal of respiratory cell and molecular biology. 1995 Jan:12(1):110-9 [PubMed PMID: 7529028]
Doeing DC, Solway J. Airway smooth muscle in the pathophysiology and treatment of asthma. Journal of applied physiology (Bethesda, Md. : 1985). 2013 Apr:114(7):834-43. doi: 10.1152/japplphysiol.00950.2012. Epub 2013 Jan 10 [PubMed PMID: 23305987]
Brannan JD, Lougheed MD. Airway hyperresponsiveness in asthma: mechanisms, clinical significance, and treatment. Frontiers in physiology. 2012:3():460. doi: 10.3389/fphys.2012.00460. Epub 2012 Dec 10 [PubMed PMID: 23233839]
Chapman DG, Irvin CG. Mechanisms of airway hyper-responsiveness in asthma: the past, present and yet to come. Clinical and experimental allergy : journal of the British Society for Allergy and Clinical Immunology. 2015 Apr:45(4):706-19. doi: 10.1111/cea.12506. Epub [PubMed PMID: 25651937]
Kudo M, Ishigatsubo Y, Aoki I. Pathology of asthma. Frontiers in microbiology. 2013 Sep 10:4():263. doi: 10.3389/fmicb.2013.00263. Epub 2013 Sep 10 [PubMed PMID: 24032029]
Limb SL, Brown KC, Wood RA, Wise RA, Eggleston PA, Tonascia J, Adkinson NF Jr. Irreversible lung function deficits in young adults with a history of childhood asthma. The Journal of allergy and clinical immunology. 2005 Dec:116(6):1213-9 [PubMed PMID: 16337448]
National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. The Journal of allergy and clinical immunology. 2007 Nov:120(5 Suppl):S94-138 [PubMed PMID: 17983880]
Buels KS, Fryer AD. Muscarinic receptor antagonists: effects on pulmonary function. Handbook of experimental pharmacology. 2012:(208):317-41. doi: 10.1007/978-3-642-23274-9_14. Epub [PubMed PMID: 22222705]
Level 3 (low-level) evidenceMoore KW, de Waal Malefyt R, Coffman RL, O'Garra A. Interleukin-10 and the interleukin-10 receptor. Annual review of immunology. 2001:19():683-765 [PubMed PMID: 11244051]
Level 3 (low-level) evidenceD'Amato M, Vitale C, Molino A, Lanza M, D'Amato G. Anticholinergic drugs in asthma therapy. Current opinion in pulmonary medicine. 2017 Jan:23(1):103-108 [PubMed PMID: 27820743]
Level 3 (low-level) evidence