Introduction
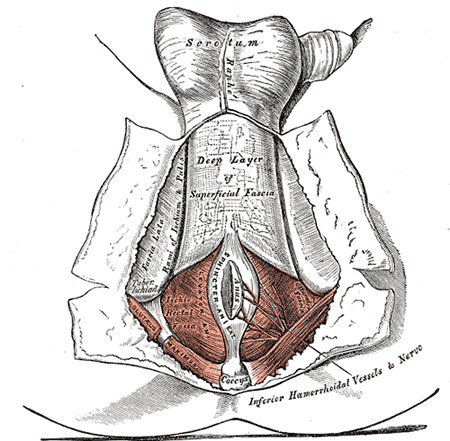
In some anatomy textbooks, the ischioanal fossa is also referred to as the ischiorectal fossa. The ischioanal fossa is a space filled with fat lateral to the anal canal and just below the pelvic diaphragm. The ischioanal fossa has a shape of a triangular pyramid, with the apex at the boundary of the anal canal and the obturator fascia and the base directed towards the perineal surface.[1] See Image. Ischioanal Fossa. The ischioanal fossa is divided into the perianal space and the ischiorectal space by the perianal fascia. The perianal fascia is an extension of the insertion of the longitudinal muscles of the anal canal outwards between the subcutaneous external sphincter and the external sphincter muscle. This fascia extends across the ischiorectal fossa to the tuberosity of the ischium. The fat of the perianal space is closely packed and finely granular, while large lobules of avascular fat fill the ischiorectal space.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Boundaries of the ischioanal fossa are:
- The apex is the intersecting fibers of the obturator internus and the levator ani muscles: these are the condensed fibers of the medial aspect of the parietal pelvic fascia covering the obturator internus muscle, named arcus tendineus of the endopelvic fascia, on which the iliococcygeus portion of the levator ani muscle inserts. The sacrospinous ligament delimits the lateral-posterior aspect.
- The base is oriented inferiorly and posteriorly; it is delimitated by the gluteus maximus muscle and the sacrotuberous ligament, the coccyx, the anococcygeal raphe, the external anal sphincter, the posterior margin of the superficial perineal fascia, and the posterior border of the transversus superficialis muscle of the perineum.
- The floor is the skin of the posterior quadrants of the perineum, limited by the ischial tuberosities and the coccyx and separated by the anococcygeal raphe.
- The roof comprises the inferior fascia covering the levator ani muscle.
- The pyramid wall comprises the puborectalis muscle and the pubococcygeal muscle covering the anal canal, and the external anal sphincter.
- The medial aspect of the obturator fascia, the ischial tuberosity, and the obturator internus muscle form the lateral wall. The fascia covering the lateral wall duplicates to form the canal where the pudendal vessels run. The sacrotuberous ligament is inserted into the ischial tuberosity; it blends the fibers with the tendon of the biceps femoris muscle and continues to the inferior pubic angle as the falciform ligament.[2] See Image. Hip Bone Anatomy.
The ischioanal fossa anteriorly continues to the pubic bones between the muscular layers and the fascia of the levator ani muscle above and the deep, transverse perineal muscle and the compressor urethra muscle below, running laterally to the urogenital organs. As a result, the fatty space assumes a wedge shape around the portion of the pelvic viscera under the levator ani muscle, from the pubis to the coccyx.[3] The contents of the ischioanal fossa include the following structures, all prone to lesions or compression:
- Internal pudendal artery, vein, and nerve.[4][3]
- Inferior rectal artery and vein
- Inferior rectal nerve
- Posterior scrotal vessels and nerves
- Perineal branch of S4 and perforating cutaneous nerve
- Lymphatics
- Subcutaneous fat is abundant on both sides of the anal canal, which permits distension of the anal canal during defecation. The different adipose tissue around the anal canal and into the ischioanal fossa could help the tone of the plate of the levator ani muscle to balance the gradient pressures of the different intra-and extra-peritoneal spaces of the abdomen, pelvis, and perineum.[1]
Embryology
A distinct fascial septum connecting the parietal and visceral sides of the ischiorectal fossa is present in fetal specimens. The dense fibrous connective tissue attaches inferiorly to the posterior side of the anterior perineal membrane (urogenital diaphragm).[5] In adult cadavers, the connective fibers spread around the lobules of the fatty tissue and hang firmly with dense fibrous tissue of the obturator internus muscle, the gluteus maximus muscle, and the inferior surface of the fascia of the levator ani muscle.[6]
Blood Supply and Lymphatics
The blood supply is chiefly from the internal pudendal artery, which may have different branching variables. The paraaortic lymph nodes are placed around the abdominal aorta and present the lymph node chain to which all the lymph nodes that drain the abdominal and pelvic viscera refer. The 2 lumbar lymphatic trunks are born from the paraaortic lymph nodes. The internal iliac lymph nodes form the internal iliac plexus along with the afferent collectors, draining the lymph from the urinary tract, the genital organs, the perineum, the rectum, the pelvic cord, and the muscles of the posterior thigh and buttock.
Nerves
The pudendal nerve provides sensory and motor innervation. The pudendal nerve derives from the ventral rami of sacral nerves (second, third, fourth). The pudendal nerve then divides into the dorsal, perineal, and inferior rectal.
Surgical Considerations
Anal abscesses are the most common pathology and represent the acute phase of an infection that originates from the glands secreting mucus present between the sphincters or between the muscles surrounding and close to the anus. Anal fistulas represent the chronic phase of this infection. Abscesses and fistulas are, therefore, 2 stages of the same disease. When the glands between the sphincters become inflamed, it forms a collection of pus (anal abscess), making its way to the skin that lines the anus and can escape spontaneously or require a surgical incision for evacuation. The channel through which the pus has passed may persist, and the orifice outside and near the anus remains open (anal fistula). There are different anorectal spaces in which the abscess fluid can flow through from 1 to another:[7]
- The perianal space is located at the level of the anal orifice. Continuous with the ischioanal space laterally and superiorly, it continues between the external and internal sphincter.
- The ischiorectal space (or ischioanal space) extends from the levator ani muscle to the perineum lateral to the anal canal.
- The intersphincteric space is located between the internal and external sphincters; it continues inferiorly into the perianal space and superiorly into the rectum wall.
- The supra levator space (or pelvic-rectal space) is limited superiorly by the peritoneum, laterally by the pelvic wall, medially by the rectal wall, and inferiorly by the levator ani muscle.
- The deep post-anal space is found at the front of the apex of the coccyx. It is limited superiorly by the plate of the levator ani muscle and inferiorly by the anococcygeal raphe. It is the posterior part of the ischioanal fossa where the 2 spaces meet.
The clinical examination usually starts by observing and palpating the skin of the perineal region posterior to the apex of the ischial tuberosities; color, swelling, and tenderness are evaluated. A rectal exam can more directly give access to the ischiorectal space. It may reveal a cord-like thickening under the mucosa, or there may be granulation tissue or a frank abscess. Anoscopy or proctoscopy is usually required to find the location of the primary opening. Fistulography may be needed to delineate the fistulous tract. MRI and CT scans are done in complex cases or for recurrent lesions. Surgery is required to drain the abscess and close the fistula.
Clinical Significance
The ischioanal fossa is susceptible to the formation of abscesses. If not recognized and left untreated, they can cause fistulous connections within the anal canal, usually just above the dentate line. Often, several fistulous tracks end blindly in the fatty tissue. The most common etiologies for an anal fistula are Crohn disease, foreign bodies, infections (tuberculosis), actinomycosis, and lymphogranuloma venereum. Trauma, hemorrhoidectomy, and episiotomy are also possible causes of an abscess. In rare cases, an anal adenocarcinoma may present with features of a chronic anal fistula. Anal fistulas and ischioanal abscesses tend to be more common in males between the ages of 30 and 48. Primary pathologic conditions originating in the ischioanal fossa proper are rare. Lesions include lipomatous tumors, aggressive angiomyxoma, vascular lesions, and neurogenic tumors. The medial border lesions of the ischioanal fossa include urogenital and anorectal diseases. Urogenital space lesions include the female: Bartholin gland cysts, Skene gland cysts, urethral diverticulum, trauma, and cervical and vaginal cancer. Endometriosis is a rare but possible occurrence. In males, the differential diagnosis for a mass in the ischiorectal fossa is limited to trauma or malignancy (prostate and penile cancer). Both sexes may have urethral or bladder carcinoma. Congenital and developmental disorders that involve the ischiorectal fossa include Gartner duct cyst, Klippel-Trenaunay syndrome, tail-gut cyst, labial cyst, and rectal duplication. Posterior perineal hernias are usually acquired and occur through a defect in the levator ani muscle; congenital defects are rare in this location.[8]
Other Issues
The ischiorectal fossa can be examined by intra-rectal touch, but it can also be evaluated by external examination. The skin of the posterior perineum is located lateral to the anal complex of muscles and delimited by the ischial tuberosities, the sacrotuberous ligament. The coccyx forms the external doorway for the ischioanal fossa space used for manual evaluation and pelvic floor therapy. Soft-tissue mobilization techniques are also useful in nerve entrapment syndromes.[9] Placement of the tips of the fingers on the area and gently wait for tissue release (as a proprioceptive perception) in front of the palpating hand, assisted by the weight of the therapist's body leaning forward. See Image. Anatomy of the Hip. The ischiorectal fossa is the space that exists between the internal surface of the perineal skin and the plane of the plate of the levator ani muscle. It is perceived as descending during inhalation and rising during exhalation. Testing and treating the density of the fatty tissue is essential to rehabilitate the perineal space after surgery or inflammation (scar treatment).[10][11] Improving the quality of the tissue is important to re-establish the function of the pelvic floor and to avoid after-surgery complications (sexual dysfunction, urological, and proctological dysfunction).[12] The ischiorectal space changes with the contraction of the levator ani muscle and the gluteus maximus muscle.[13] Other factors that alter the space include the connective fibers enveloping the adipose lobules that attach to the fascia of the muscles surrounding the ischiorectal space; these functionally link the pelvic floor diaphragm to the thoracic diaphragm[14] through the thoracolumbar fascia[15] and to the hip and the lower limb by the external rotator muscles of the femur.[14][15]
Media
(Click Image to Enlarge)
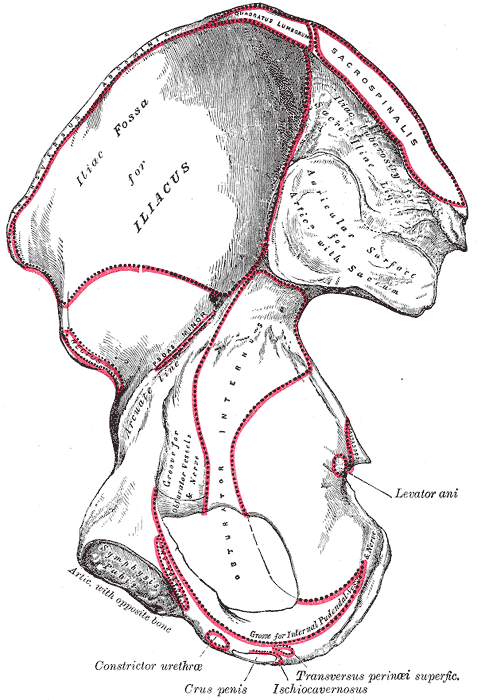
Hip Bone Anatomy. Anatomy includes transverse abdominis, quadratus lumborum, sacrospinalis, iliac tuberosity, sacroiliac ligament, iliac fossa, iliacus, rectus, symphysis pubis, constrictor urethra, crus penis, transversus perinei superficial ischiocavernosus, ischiocavernosus, levator ani, obturator internus, sacrum, and auricular surface.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
MORGAN CN. The surgical anatomy of the ischiorectal space. Proceedings of the Royal Society of Medicine. 1949 Mar:42(3):189-200 [PubMed PMID: 18126986]
Loukas M, Louis RG Jr, Hallner B, Gupta AA, White D. Anatomical and surgical considerations of the sacrotuberous ligament and its relevance in pudendal nerve entrapment syndrome. Surgical and radiologic anatomy : SRA. 2006 May:28(2):163-9 [PubMed PMID: 16463079]
Montoya TI, Calver L, Carrick KS, Prats J, Corton MM. Anatomic relationships of the pudendal nerve branches. American journal of obstetrics and gynecology. 2011 Nov:205(5):504.e1-5. doi: 10.1016/j.ajog.2011.07.014. Epub 2011 Jul 20 [PubMed PMID: 21889763]
Maldonado PA, Chin K, Garcia AA, Corton MM. Anatomic variations of pudendal nerve within pelvis and pudendal canal: clinical applications. American journal of obstetrics and gynecology. 2015 Nov:213(5):727.e1-6. doi: 10.1016/j.ajog.2015.06.009. Epub 2015 Jun 10 [PubMed PMID: 26070708]
Hammer RP Jr, Shrewsbury MM. A reconsideration of the ischiorectal fossa. Diseases of the colon and rectum. 1977 Nov-Dec:20(8):681-9 [PubMed PMID: 923399]
Zhang JF, Du ML, Sui HJ, Yang Y, Zhou HY, Meng C, Qu MJ, Zhang Q, Du B, Fu YS. Investigation of the ischioanal fossa: Application to abscess spread. Clinical anatomy (New York, N.Y.). 2017 Nov:30(8):1029-1033. doi: 10.1002/ca.22901. Epub 2017 Jun 6 [PubMed PMID: 28509338]
Hogan AM, Mannion M, Ryan RS, Khan W, Waldron R, Barry K. Beware the ischiorectal abscess. International journal of surgery case reports. 2013:4(3):299-301. doi: 10.1016/j.ijscr.2012.08.005. Epub 2012 Sep 1 [PubMed PMID: 23396392]
Level 3 (low-level) evidenceLlauger J, Palmer J, Pérez C, Monill J, Ribé J, Moreno A. The normal and pathologic ischiorectal fossa at CT and MR imaging. Radiographics : a review publication of the Radiological Society of North America, Inc. 1998 Jan-Feb:18(1):61-82; quiz 146 [PubMed PMID: 9460109]
Martin R, Martin HD, Kivlan BR. NERVE ENTRAPMENT IN THE HIP REGION: CURRENT CONCEPTS REVIEW. International journal of sports physical therapy. 2017 Dec:12(7):1163-1173 [PubMed PMID: 29234567]
Zanier E, Bordoni B. A multidisciplinary approach to scars: a narrative review. Journal of multidisciplinary healthcare. 2015:8():359-63. doi: 10.2147/JMDH.S87845. Epub 2015 Aug 12 [PubMed PMID: 26316774]
Level 3 (low-level) evidenceBordoni B, Zanier E. Skin, fascias, and scars: symptoms and systemic connections. Journal of multidisciplinary healthcare. 2013:7():11-24. doi: 10.2147/JMDH.S52870. Epub 2013 Dec 28 [PubMed PMID: 24403836]
Faubion SS, Shuster LT, Bharucha AE. Recognition and management of nonrelaxing pelvic floor dysfunction. Mayo Clinic proceedings. 2012 Feb:87(2):187-93. doi: 10.1016/j.mayocp.2011.09.004. Epub [PubMed PMID: 22305030]
Soljanik I, Janssen U, May F, Fritsch H, Stief CG, Weissenbacher ER, Friese K, Lienemann A. Functional interactions between the fossa ischioanalis, levator ani and gluteus maximus muscles of the female pelvic floor: a prospective study in nulliparous women. Archives of gynecology and obstetrics. 2012 Oct:286(4):931-8. doi: 10.1007/s00404-012-2377-4. Epub 2012 Jun 13 [PubMed PMID: 22692630]
Bordoni B, Zanier E. Anatomic connections of the diaphragm: influence of respiration on the body system. Journal of multidisciplinary healthcare. 2013:6():281-91. doi: 10.2147/JMDH.S45443. Epub 2013 Jul 25 [PubMed PMID: 23940419]
Willard FH, Vleeming A, Schuenke MD, Danneels L, Schleip R. The thoracolumbar fascia: anatomy, function and clinical considerations. Journal of anatomy. 2012 Dec:221(6):507-36. doi: 10.1111/j.1469-7580.2012.01511.x. Epub 2012 May 27 [PubMed PMID: 22630613]