Introduction
Anterior chest wall pain after median sternotomy for open cardiothoracic surgery is common and can be debilitating for months afterward. As the field of anesthesiology adopts more opioid-sparing techniques, regional anesthesia has gained favor. Traditional neuraxial anesthesia is often avoided for cardiac surgical procedures as they require full heparinization. Other techniques like paravertebral or erector spinae blocks are cumbersome to perform post-operatively as the patient is intubated and in the supine position. For these reasons, parasternal blocks such as the pecto-intercostal fascial plane (PIFP) block are becoming increasingly popular.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
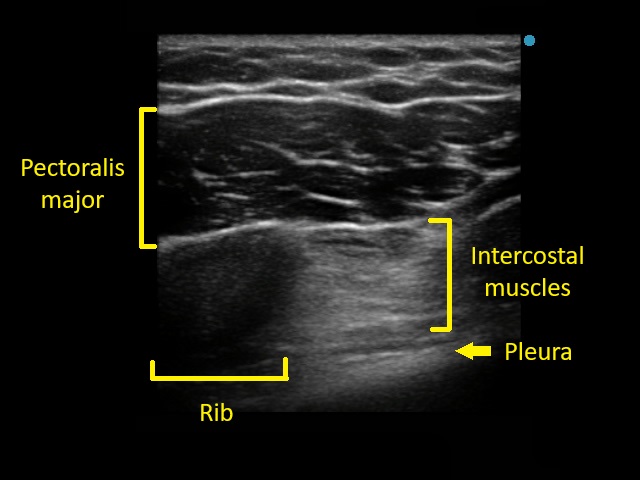
The thoracic intercostal nerves are responsible for the sensory innervation of the chest wall.[1] From superficial to deep, the parasternal chest wall consists of skin, subcutaneous tissue, the pectoralis major muscle, the intercostal muscles (external, internal, and innermost), the transversus thoracis muscle, and the pleura.[2] The innermost intercostal muscle and transversus thoracis muscle lie in the same plane, just above the pleura, with the transversus thoracis covering the anterior-medial chest wall and the innermost intercostal muscle covering the lateral and posterior chest wall. The internal mammary artery and the intercostal nerve run in the plane above this innermost intercostal/transversus thoracis muscle layer. After supplying the lateral cutaneous branches responsible for sensory innervation of the lateral chest wall, the rest of the intercostal nerve travels to the parasternal region, where it courses through the internal intercostal muscle, external intercostal membrane, then the pectoralis major muscle to provide sensation to the anterior chest wall via the anterior cutaneous branches.[1] The PIFP block deposits local anesthetic at the fascial layer between the pectoralis major and the external intercostal muscle/membrane. Therefore, it blocks the anterior cutaneous branches before the intercostal nerve pierces the pectoralis major.
The advantage of fascial plane blocks over intercostal nerve blocks is that fascial spread can cover multiple dermatomal distributions unilaterally. De la Torre and colleagues, who first described the PIFP block, instructed the insertion of the block needle at the sixth intercostal space.[3] Other groups have described injection anywhere between the third and fifth intercostal spaces.[4][5][6] The goal of the PIFP block is to target T2 to T6.[4][7] For practical application, performing the block at the midpoint of the sternotomy incision is recommended. If multilevel spread is not visualized on ultrasound, consider performing multilevel injections.[7][8]
The correct application of ultrasound for the PIFP block keeps the intercostal muscle layers between the nerve block needle and the internal mammary artery (see Image. Parasternal Doppler). This provides a layer of safety from potentially damaging the artery most utilized in coronary artery bypass graft surgery.
Indications
The PIFP block targets the anterior cutaneous branches of the second through sixth intercostal nerves and is indicated for analgesia of the sternum and parasternal regions of the chest wall. It was first described by de la Torre et al. in 2014 for adjuvant analgesia after breast surgery.[3] The PIFP block has since been adopted more frequently for median sternotomy and anterior minimally invasive thoracotomy.[9][10][11][12] Interestingly, the PIFP block may be indicated over a transversus thoracis muscle plane (TTMP) when the internal mammary artery is to be harvested. This point is discussed below in the “Clinical Significance” section.
Additional reported indications for the PIFP block include sternal and anterior rib fractures.[13][14] The PIFP block has also been shown to benefit pediatric patients undergoing open cardiac surgery as well as more minor procedures such as subcutaneous implantable cardioverter-defibrillator devices.[15][16][17] Finally, a case report by Sahoo and colleagues describes the successful use of the PIFP block to treat a patient with severe chronic post-sternotomy pain syndrome 9 months after coronary artery bypass graft surgery.[18] After a single iteration of the procedure, the patient described significant pain relief even at the 6-month follow-up.
Contraindications
Contraindications for the PIFP block parallel those of other regional nerve blocks. These include allergy to local anesthetics, infection or malignancy at the injection site, and patient refusal. No contraindications specific to performing the PIFP block have been described.[7]
Caution should be taken when patients have comorbidities that increase the risk of local anesthetic systemic toxicity (LAST). These include hepatic dysfunction (as the liver metabolizes amide anesthetics), metabolic syndromes, and extremes of age.[19]
Due to the proximity of the pleura, pneumothorax is a serious potential complication of the PIFP block. Compromised pulmonary function or previous lung resection is a relative contraindication to consider. In open cardiac surgery, however, bilateral chest tubes are often planned and can mitigate this complication.
Equipment
Performing the PIFP block under ultrasound guidance minimizes the risk of complications. The basic equipment needed includes:
- Ultrasound machine with high-frequency linear transducer
- Sterile ultrasound sleeve and gel
- Sterile gloves
- Chlorhexidine 2% or other antiseptic preparations
- Two (if bilateral) 20 to 30 mL syringes containing local anesthetic with or without adjuncts. Typically, 0.25% to 0.5% bupivacaine (to a maximum of 2.5 mg/kg) is used.
- Short bevel nerve block needle, typically 18 G to 22 G, 50 to 100 mm in length, with extension tubing
- Standard American Society of Anesthesiology physiologic monitors should be applied: pulse oximetry, noninvasive blood pressure, and electrocardiography. Temperature and end-tidal CO2 are not necessary if the patient is awake.
Personnel
The PIFP block should be performed by a provider who regularly performs ultrasound-guided regional anesthesia and is familiar with the relevant anatomy.
A second provider should be present to perform a safety timeout or local institutional equivalent. At that time, providers confirm the correct procedure, patient, and side (usually bilateral) and review the patient’s allergies. The second provider will also assist with the procedure by controlling the syringe with the local anesthetic solution, aspirating and injecting it as directed by the provider performing the block.
Finally, a clinical provider must actively monitor the patient after the block for signs of LAST, administer rescue medications, and call for help if necessary.
Preparation
The patient’s medical and surgical history should be reviewed, focusing on the patient’s allergies, prior exposure to anesthesia, any respiratory conditions, and coagulation status. The provider should describe the procedure and its risks, benefits, and alternatives. The patient should discuss these with the provider until they express understanding and make an informed decision about whether to proceed with the block.
The patient should be monitored physiologically, including pulse oximetry, noninvasive blood pressure, and electrocardiography. The patient should also have intravenous access. If performed when the patient is awake, intravenous anxiolytic medication may be advisable.
Prior to the procedure, a safety timeout or equivalent should be performed to confirm the correct procedure, correct patient, and correct side (usually bilateral), as well as to review the patient’s allergies. Finally, one must ensure that a qualified provider is available to actively monitor the patient after the block for signs of LAST and to respond appropriately.
Technique or Treatment
With the patient in the supine position, the patient is prepped and draped in a sterile fashion. A high-frequency linear ultrasound transducer with a sterile cover is placed 2 to 3 cm lateral to the border of the sternum in a cranial-caudal orientation. The third and fourth ribs with underlying acoustic shadows are identified. Then, from superficial to deep, the following structures are identified: the subcutaneous tissue, pectoralis major muscle, intercostal muscles (external, internal, and innermost), and the pleura (see Image. Ultrasound View). Due to anatomic variability, the transversus thoracis muscle may not be visible, especially if the probe is too far lateral from the sternum.
An echogenic nerve block needle is inserted in-plane relative to the probe — just superior and superficial to the third rib (as a safeguard from inadvertently going through pleura) — and guided toward the T3 to T4 intercostal space to the fascial plane between the pectoralis major and intercostal muscles. After a negative aspiration to avoid intravascular administration, a 1 to 2 mL test dose of sterile saline is injected to confirm the needle tip position and fascial plane spread. Once confirmed, 10 to 15 mL of the local anesthetic solution is injected in small aliquots, being mindful to aspirate before each injection to avoid intravascular administration. This procedure should then be repeated on the contralateral side.
Complications
The PIFP block shares the potential complications of all regional anesthetic blocks: excessive bleeding or hematoma formation at the puncture site, infection, damage to nearby neurovascular structures, intravascular injection, and LAST.
Reports describing complications specific to the PIFP block are scarce due to its recent emergence.[1][7] The incidence of pneumothorax, a potentially serious complication, is very low with real-time ultrasound guidance. The sequelae of pneumothorax are also mitigated during open cardiac surgery, as bilateral chest tubes are often planned. Damage to the internal mammary artery could be catastrophic for patients whose surgical plan includes its harvest. As the PIFP block is more superficial, it is considered safer than the TTMP block with respect to this potential complication.
Clinical Significance
Poorly controlled acute surgical pain after sternotomy has been associated with chronic post-sternotomy pain syndromes in 11% to 56% of patients and severe incapacitating chronic pain in 3% to 5% of patients.[20][21][22] Analgesia for cardiac surgery had traditionally relied on large doses of intravenous opioids.[7] Opioid administration can lead to delayed extubation, hypoventilation, bowel dysfunction, longer hospital stays, prolonged opioid use after discharge, and potentially opioid dependence or opioid-induced hyperalgesia. Thoracic epidural analgesia and even paravertebral nerve blocks remain controversial due to the risk of neuraxial hematoma formation in these patients who are fully heparinized intraoperatively. Although bilateral erector spinae plane blocks could provide adequate analgesia to the entire thoracic wall from approximately T2 to T9, this block cannot be performed in the supine patient and is consequently not easily performed postoperatively. Intercostal nerve blocks are easy to perform, even without ultrasound guidance, but require numerous bilateral blocks. As a result, fascial plane chest wall blocks are becoming increasingly popular.
A parasternal block (PSB) provides significant analgesia after sternotomy by targeting the anterior cutaneous branches of the intercostal nerves, most importantly T2 to T6.[1] A PSB can be done blindly or under ultrasound guidance. A systematic review by King et al. observed a statistically significant reduction in both postoperative visual analog pain scale scores and opioid use by patients who received a PSB for cardiac surgery.[23] As ultrasound guidance has become widely available, allowing for reproducible deposition of local anesthetic at specific planes, two specific fascial plane blocks have emerged as the most common PSBs: the TTMP and the PIFP.[24]
As mentioned previously, the PIFP block was first described by de la Torre et al. in 2014 for analgesia after breast surgery.[3] This group highlighted the advantages of this technique: covering numerous dermatomes with a single puncture, minimizing pleural or vessel injury, and decreasing systemic absorption compared to intercostal nerve blockade. Recently, most studies of the PIFP block have been in cardiac surgical patients. Kumar et al. performed a single-blinded prospective randomized control trial of 40 patients given a PIFP block or a placebo. This study found significantly less rescue fentanyl was needed in the blocked group.[5] Hamed et al. randomized 70 patients to PIFP block or placebo and found mean morphine consumption in the first 24 hours was lower and mean time to first analgesic request was higher in the PIFP group.[25] In a single-center, prospective, randomized, and placebo-controlled quadruple-blinded study of 80 patients, Khera and colleagues found patients who received the PIFP block tended to require less opioid analgesia and tended to experience a lower incidence of in-hospital delirium; however, these differences did not reach statistical significance.[11] Most convincingly, Zhang et al. reported the use of bilateral continuous PIFP block catheters resulted in significantly shorter lengths of hospital stay (8.9 ± 0.9 days vs 6.5 ± 1.1 days, P < 0.01), significantly lower resting pain scores over three days, less sufentanil consumption both intraoperatively and postoperatively, shorter time to first flatus (43 ± 6 hours vs 30 ± 7 hours, P < 0.01), and less incidence of postoperative nausea or vomiting (9.1% vs 27.3%, P < 0.01).[12]
The most important distinction between the PIFP and TTMP is that a PIFP block deposits local anesthetic between the pectoralis major muscle and the internal intercostal muscle, while the TTMP block deposits local anesthetic between the internal intercostal muscle and the transversus thoracis muscle. The PIFP is located further from the heart and lungs, theoretically decreasing the risk of hematoma and pneumothorax.[7] The decrease in hematoma and pneumothorax is supported anecdotally in a small study directly comparing PIFP with TTMP: two patients' TTMP blocks (out of 32 patients) were complicated by pneumothorax compared to 0 of 32 patients receiving PIFP blocks.[8]
In addition, the PIFP block avoids the plane of the Internal Mammary Artery (IMA), enhancing safety. A randomized, double-blind study revealed no significant differences in pain scores and morphine consumption at 24 hours between the PIFP and TTMP groups. However, the TTMP group exhibited a notably shorter time to first opioid request—240 minutes compared to the PIFP group's 600 minutes.[4] The authors noted that left IMA harvest in 85% of TTMP patients may have affected the spread of local anesthetic along its intended plane. Without Doppler imaging, distinguishing the shared plane of the transversus thoracis muscle and the IMA is challenging, presenting a significant risk of catastrophic injury (see Images. Parasternal Doppler and Ultrasound View). Consequently, the choice of surgical IMA harvest emerges as a pivotal factor in deciding the appropriate fascial plane block technique.
On a separate note, Toscano et al. remarked that the PIFP often required injections at multiple intercostal levels as the local anesthetic failed to spread across the fascial plane under ultrasound visualization.[8] A small cadaveric study by Douglas et al. supports this claim.[26] Again, multilevel injections should be considered when multilevel spread is not visualized on ultrasound.
Enhancing Healthcare Team Outcomes
The PIFP block is a useful tool for providing analgesia to the anterior chest wall and is applicable to a variety of procedures, from subcutaneous defibrillator placement to median sternotomy. Detailed knowledge of relevant anatomy is crucial for proper execution of the PIFP and decreasing the risk of pneumothorax, hematoma, and injury to the internal mammary artery. While fascial plane blocks usually cross dermatomes unilaterally, multi-level injections should be considered if local anesthetic spread is not well visualized.
The field of anesthesiology is embracing opioid-sparing techniques such as regional nerve and fascial plane blocks. Other members of the patient care team such as nurse anesthetists, nurses, physician assistants, or anesthesiologist assistants are frequently asked to assist with the procedure. Assistance with the procedure may entail maintenance of the sterile field, administration of medications, monitoring vital signs, preparation of equipment, and verification of the timeout process.
Those who assist with the procedure and monitor the patient afterward should be familiar with the potential complications. Significant complications to be aware of and monitored for include pneumothorax, LAST, bleeding, and infection. Nursing staff should be cognizant of LAST symptoms such as periorbital paresthesia, metallic taste, or tinnitus and skilled in monitoring for signs such as tachycardia, electrocardiography changes, hypotension, and rapid-onset seizure. If a patient requires treatment for LAST, pharmacists offer expertise in medication logistics to help the team administer the correct dosage of intralipid as quickly as possible. Monitoring is usually carried out immediately in the operating theater and is then extended to the postoperative areas (intensive care unit or postanesthesia care unit). Patient safety requires coordinated efforts across many disciplines across many locations in the hospital. Rapid and effective communication among surgeons, anesthesiologists, advanced practitioners, nursing staff, pharmacists, and other healthcare professionals is necessary to limit adverse outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
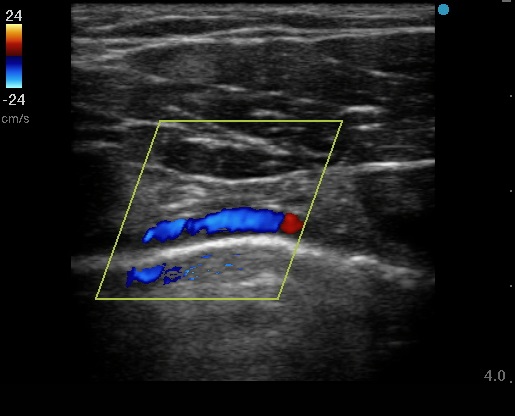
Parasternal Doppler. Ultrasound visualization of the internal mammary artery (IMA) during a PIFP block helps keep the intercostal muscle layers between the nerve block needle and the IMA providing a layer of safety from potentially damaging the artery that is most utilized in coronary artery bypass graft surgery.
Contributed by Alexander Zhu MD
References
Kelava M, Alfirevic A, Bustamante S, Hargrave J, Marciniak D. Regional Anesthesia in Cardiac Surgery: An Overview of Fascial Plane Chest Wall Blocks. Anesthesia and analgesia. 2020 Jul:131(1):127-135. doi: 10.1213/ANE.0000000000004682. Epub [PubMed PMID: 32032103]
Level 3 (low-level) evidenceTang A, Bordoni B. Anatomy, Thorax, Muscles. StatPearls. 2024 Jan:(): [PubMed PMID: 30855905]
de la Torre PA, García PD, Alvarez SL, Miguel FJ, Pérez MF. A novel ultrasound-guided block: a promising alternative for breast analgesia. Aesthetic surgery journal. 2014 Jan 1:34(1):198-200. doi: 10.1177/1090820X13515902. Epub [PubMed PMID: 24396082]
Kaya C, Dost B, Dokmeci O, Yucel SM, Karakaya D. Comparison of Ultrasound-Guided Pecto-intercostal Fascial Block and Transversus Thoracic Muscle Plane Block for Acute Poststernotomy Pain Management After Cardiac Surgery: A Prospective, Randomized, Double-Blind Pilot Study. Journal of cardiothoracic and vascular anesthesia. 2022 Aug:36(8 Pt A):2313-2321. doi: 10.1053/j.jvca.2021.09.041. Epub 2021 Oct 1 [PubMed PMID: 34696966]
Level 1 (high-level) evidenceKumar AK, Chauhan S, Bhoi D, Kaushal B. Pectointercostal Fascial Block (PIFB) as a Novel Technique for Postoperative Pain Management in Patients Undergoing Cardiac Surgery. Journal of cardiothoracic and vascular anesthesia. 2021 Jan:35(1):116-122. doi: 10.1053/j.jvca.2020.07.074. Epub 2020 Jul 30 [PubMed PMID: 32859487]
Ellouze O, Missaoui A, Berthoud V, Bouhemad B, Guinot PG. Parasternal Pectoral Block for Right Anterior Minimally Invasive Thoracotomy in Cardiac Surgery. Journal of cardiothoracic and vascular anesthesia. 2020 Feb:34(2):450-453. doi: 10.1053/j.jvca.2019.08.007. Epub 2019 Aug 12 [PubMed PMID: 31500983]
Ritter MJ, Christensen JM, Yalamuri SM. Regional Anesthesia for Cardiac Surgery: A Review of Fascial Plane Blocks and Their Uses. Advances in anesthesia. 2021 Dec:39():215-240. doi: 10.1016/j.aan.2021.08.001. Epub 2021 Oct 1 [PubMed PMID: 34715976]
Level 3 (low-level) evidenceToscano A, Capuano P, Perrucci C, Giunta M, Orsello A, Pierani T, Costamagna A, Tedesco M, Arcadipane A, Sepolvere G, Buono G, Brazzi L. Which ultrasound-guided parasternal intercostal nerve block for post-sternotomy pain? Results from a prospective observational study. Journal of anesthesia, analgesia and critical care. 2023 Nov 16:3(1):48. doi: 10.1186/s44158-023-00134-2. Epub 2023 Nov 16 [PubMed PMID: 37974241]
Level 2 (mid-level) evidenceLiu V, Mariano ER, Prabhakar C. Pecto-intercostal Fascial Block for Acute Poststernotomy Pain: A Case Report. A&A practice. 2018 Jun 15:10(12):319-322. doi: 10.1213/XAA.0000000000000697. Epub [PubMed PMID: 29293481]
Level 3 (low-level) evidenceBloc S, Perot BP, Gibert H, Law Koune JD, Burg Y, Leclerc D, Vuitton AS, De La Jonquière C, Luka M, Waldmann T, Vistarini N, Aubert S, Ménager MM, Merzoug M, Naudin C, Squara P. Efficacy of parasternal block to decrease intraoperative opioid use in coronary artery bypass surgery via sternotomy: a randomized controlled trial. Regional anesthesia and pain medicine. 2021 Aug:46(8):671-678. doi: 10.1136/rapm-2020-102207. Epub 2021 May 14 [PubMed PMID: 33990437]
Level 1 (high-level) evidenceKhera T, Murugappan KR, Leibowitz A, Bareli N, Shankar P, Gilleland S, Wilson K, Oren-Grinberg A, Novack V, Venkatachalam S, Rangasamy V, Subramaniam B. Ultrasound-Guided Pecto-Intercostal Fascial Block for Postoperative Pain Management in Cardiac Surgery: A Prospective, Randomized, Placebo-Controlled Trial. Journal of cardiothoracic and vascular anesthesia. 2021 Mar:35(3):896-903. doi: 10.1053/j.jvca.2020.07.058. Epub 2020 Jul 24 [PubMed PMID: 32798172]
Level 1 (high-level) evidenceZhang Y, Gong H, Zhan B, Chen S. Effects of bilateral Pecto-intercostal Fascial Block for perioperative pain management in patients undergoing open cardiac surgery: a prospective randomized study. BMC anesthesiology. 2021 Jun 22:21(1):175. doi: 10.1186/s12871-021-01391-w. Epub 2021 Jun 22 [PubMed PMID: 34157970]
Level 1 (high-level) evidenceRaza I, Narayanan M, Venkataraju A, Ciocarlan A. Bilateral Subpectoral Interfascial Plane Catheters for Analgesia for Sternal Fractures: A Case Report. Regional anesthesia and pain medicine. 2016 Sep-Oct:41(5):607-9. doi: 10.1097/AAP.0000000000000388. Epub [PubMed PMID: 27145074]
Level 3 (low-level) evidenceBurns LT, Beasley DA, Stevens MA, Crabtree DE, Mehaffey GR. Pectointercostal Fascial Block Catheters for Thoracic Injuries: A Case Series. A&A practice. 2018 Dec 15:11(12):340-343. doi: 10.1213/XAA.0000000000000821. Epub [PubMed PMID: 30085936]
Level 2 (mid-level) evidenceZhang Y, Min J, Chen S. Perioperative Pain Management With Bilateral Pecto-intercostal Fascial Block in Pediatric Patients Undergoing Open Cardiac Surgery. Frontiers in cardiovascular medicine. 2022:9():825945. doi: 10.3389/fcvm.2022.825945. Epub 2022 Jun 22 [PubMed PMID: 35811718]
Elbardan IM, Shehab AS, Mabrouk IM. Comparison of Transversus Thoracis Muscle Plane Block and Pecto-Intercostal Fascial Plane Block for enhanced recovery after pediatric open-heart surgery. Anaesthesia, critical care & pain medicine. 2023 Aug:42(4):101230. doi: 10.1016/j.accpm.2023.101230. Epub 2023 Apr 7 [PubMed PMID: 37031816]
Koller MP, Cortez D, Kim TW. Nerve Blocks for Postoperative Pain Management in Children Receiving a Subcutaneous Implantable Cardioverter-Defibrillator: A Case Series. A&A practice. 2020 Nov:14(13):e01351. doi: 10.1213/XAA.0000000000001351. Epub [PubMed PMID: 33236870]
Level 2 (mid-level) evidenceSahoo RK, Kar R, Patel R, Kumar M, Giri D, Biswas M, Nair AS. Pectoral-intercostal fascial plane block in chronic post-sternotomy pain. Annals of cardiac anaesthesia. 2022 Jan-Mar:25(1):97-99. doi: 10.4103/aca.ACA_62_20. Epub [PubMed PMID: 35075030]
Mahajan A, Derian A. Local Anesthetic Toxicity. StatPearls. 2024 Jan:(): [PubMed PMID: 29763139]
Meyerson J, Thelin S, Gordh T, Karlsten R. The incidence of chronic post-sternotomy pain after cardiac surgery--a prospective study. Acta anaesthesiologica Scandinavica. 2001 Sep:45(8):940-4 [PubMed PMID: 11576043]
Kalso E, Mennander S, Tasmuth T, Nilsson E. Chronic post-sternotomy pain. Acta anaesthesiologica Scandinavica. 2001 Sep:45(8):935-9 [PubMed PMID: 11576042]
Kleiman AM, Sanders DT, Nemergut EC, Huffmyer JL. Chronic Poststernotomy Pain: Incidence, Risk Factors, Treatment, Prevention, and the Anesthesiologist's Role. Regional anesthesia and pain medicine. 2017 Nov/Dec:42(6):698-708. doi: 10.1097/AAP.0000000000000663. Epub [PubMed PMID: 28937533]
King M, Stambulic T, Hassan SMA, Norman PA, Derry K, Payne DM, El Diasty M. Median sternotomy pain after cardiac surgery: To block, or not? A systematic review and meta-analysis. Journal of cardiac surgery. 2022 Nov:37(11):3729-3742. doi: 10.1111/jocs.16882. Epub 2022 Sep 13 [PubMed PMID: 36098374]
Level 1 (high-level) evidenceDesire SM, Hayward G. Transversus Thoracic Muscle Plane Block (TTMPB). StatPearls. 2024 Jan:(): [PubMed PMID: 36508536]
Hamed MA, Abdelhady MA, Hassan AASM, Boules ML. The Analgesic Effect of Ultrasound-guided Bilateral Pectointercostal Fascial Plane Block on Sternal Wound Pain After Open Heart Surgeries: A Randomized Controlled Study. The Clinical journal of pain. 2022 Feb 7:38(4):279-284. doi: 10.1097/AJP.0000000000001022. Epub 2022 Feb 7 [PubMed PMID: 35132025]
Level 1 (high-level) evidenceDouglas RN, Kattil P, Lachman N, Johnson RL, Niesen AD, Martin DP, Ritter MJ. Superficial versus deep parasternal intercostal plane blocks: cadaveric evaluation of injectate spread. British journal of anaesthesia. 2024 May:132(5):1153-1159. doi: 10.1016/j.bja.2023.08.014. Epub 2023 Sep 21 [PubMed PMID: 37741722]