Introduction
Spinal stenosis is a condition in which the nerve roots are compressed by a number of pathologic factors, leading to symptoms such as pain, numbness, and weakness. The upper neck (cervical) and lower back (lumbar) areas most frequently are affected, although the thoracic spine also can be compressed most frequently by a disk herniation. Three different anatomic sites within the vertebral canal can be affected by spinal stenosis. First, the central canal, which houses the spinal cord, can be narrowed in an anterior-posterior dimension, leading to compression of neural elements and reduction of blood supply to the spinal cord in the cervical area and the cauda equina in the lumbar area. Secondly, the neural foramen, which are openings through which the nerve roots exit the spinal cord, can be compressed as a result of disk herniation, hypertrophy of the facet joints and ligaments, or unstable slippage of one vertebral body relative to the level below. Lastly, the lateral recess, which is seen in the lumbar spine only and is defined as the area long the pedicle that a nerve root enters just before its exit through the neural foramen, can be compressed from a facet joint hypertrophy. [1][2][3] Depending on the level of the spine affected, each type of compression can lead to different symptoms that warrant a particular treatment modality.
Most patients will experience some type of pain associated with the spine but luckily, even without surgery, the majority will have an uneventful recovery. Only 1-3% will have a herniated disc and less than 2% will have compression of a nerve root.
Spinal stenosis is common with aging but predicting which individual will develop symptoms is not possible. In most cases, the degenerative process can be controlled by changes in lifestyle.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Spinal stenosis can be caused by congenital or acquired etiologies. Only 9% of the cases result from congenital etiologies. Some common congenital causes include achondroplasia, shortened pedicles, osteopetrosis, apical vertebral wedging, spinal dysraphism, segmentation failure early vertebral arch ossification, thoracolumbar kyphosis, morquio syndrome, and osseous exostosis.
Acquired stenosis occurs primarily from trauma, degenerative changes, iatrogenic causes, and systemic processes. Trauma usually affects the vertebral canal acutely with a mechanical force. Degenerative changes occur when there is a narrowing of the central canal and lateral recess from posterior disk herniation, ligamentum flavum hypertrophy, and spondylolisthesis. Laminectomy, fusion, and discectomy surgeries can cause iatrogenic spinal stenosis.[4][5][6][7]
Epidemiology
In the United States, spinal stenosis if widely seen in outpatient clinics among the geriatric population. LSS in earlier ages is usually due to congenital malformations, while patients over the age of 50 years are likely due to degenerative causes. Studies have shown that 1/1000 persons over the age of 65 years and about 5/1000 persons over the age of 50 years are likely to get spinal stenosis.[7] The prevalence of the disease is predicted to increase to about 18 million in the next decade. For adults above the age of 65 years undergoing spine surgery, lumbar spinal stenosis (LSS) is the leading diagnosis. As you go down the lumbar spine the nerve root area ratio decreases and this increases the incidence of foraminal stenosis hence spinal stenosis.
Pathophysiology
Spinal stenosis is a disease process that results from the narrowing of the vertebral spinal canal and the lateral recesses. This often leads to the compression of the structures located within the spinal canal, including the spinal cord, nearby nerve tissue, and cerebrospinal fluid. There are multiple factors that can lead to the narrowing. This includes bulging or protrusion of the intervertebral disc, herniation of the nucleus pulposus posteriorly, epidural fat deposition, hypertrophy of posterior longitudinal ligament, or the ligamentum flavum, and hypertrophy of the facet joints. [7][8] Spinal cord injury can result in cord lead major complications such as myelopathic syndrome or cauda equina syndrome.
History and Physical
Initial evaluation of a patient with spinal stenosis often begins with a detailed history of symptoms and physical exam, with a focus on sensation, motor strength, reflexes, special tests, and gait. Stenosis in the cervical spine can lead to radicular symptoms due to nerve root compression and myelopathy due to spinal cord compression. Patients initially present with neck or arm pain. If a patient has a nerve root impingement, radicular symptoms occur and depend on the level affected. For example, a C5-6 disk herniation leads to C6 radiculopathy. C6-7 disk herniation is the most common, leading to a wrist drop and paresthesia in the 2 and three fingers. C5-6 disk herniation is the next common, resulting in weakness in forearm flexion and paresthesia in the thumb and radial forearm. C7-T1 disk herniation can lead to weakness in the hand intrinsic muscles and numbness in the 4 and five digits. Lastly, a C4-5 disk herniation can lead to deltoid weakness and shoulder paresthesia. Patients also can experience pain and paresthesia in the head, neck, and shoulder. Cervical spondylotic myelopathy can be seen in patients with greater than 30% spinal narrowing, leading to clumsiness in the upper extremities, gait disturbance, lower extremity weakness, and ataxia.
Stenosis in the lumbar spine can lead to neurogenic claudication, myeloradiculopathy symptoms, sensory disturbances, motor weakness, and pathologic reflexes. Patients will present with complaints of cramping pain in the leg, calf, and or buttocks. They might report an increase in pain with walking or standing for prolonged periods and relief when sitting or leaning forward while using a shopping cart. [9] Disk herniation is most common at the L4-5 and L5-S1 levels. A herniated disk at L5-S1 can lead to plantarflexion weakness, decrease sensation in the lateral foot, and cause pain in the posterior leg. A disk herniation at L4-5 can lead to a foot drop and numbness in the large toe web and dorsal aspect of the foot. Lastly, an L3-4 disk herniation can lead to knee extension weakness, numbness in the medial foot, and pain in the anterior thigh.
Evaluation
Diagnosis can be made through imaging with an extended-release x-ray, CT, and MRI. With the availability of MRI, a plain radiograph is of limited value although dynamic views in flexion and extension modes can demonstrate dynamic instability or spondylolisthesis. CT can help differentiate calcified disks or bone osteophytes from “soft disks,” differentiate ossification of the posterior longitudinal ligament from a thickened posterior longitudinal ligament and detect bone fractures or lytic lesions. MRI is the gold standard; it is able to show intrinsic cord abnormalities, the degree of spinal stenosis, and differentiate other conditions such as tumors, hematoma, or infection. If a patient has a pacemaker and cannot obtain an MRI, a CT myelogram can be performed to identify the level and degree of stenosis.[10][11][12]
Electrodiagnostic studies are often performed to help rule out and rule in the differential diagnosis. Nerve conduction studies along with needle electromyography and somatosensory evoked potentials.
Treatment / Management
In patients who suffer from cervical stenosis without myelopathy, conservative management with bracing, rest, or anti-inflammatory medications initially can be employed. For those with myelopathy, surgical decompression can provide some relief from pain and sensory loss and can prevent the exacerbation of myelopathy. Depending on the levels involved and the pathology, anterior or posterior decompression and fusion can be employed to relieve the compression and stabilize the spine. In the lumbar spine, initial management of back pain can be done with NSAIDs and physical therapy followed by interventional pain management strategies for persistent pain. When conservative management is inadequate, or the patient develops progressive myelopathy, neurologic deficits, or spinal instability, surgical decompression, and fusion are recommended. Depending on the nature of the pathology, a variety of approaches, including anterior, lateral, or posterior can be employed to restore lumbar lordosis, decompress the stenosis, and promote fusion.[13][14][15](A1)
Differential Diagnosis
- Lumbar Compression Fracture
- Lumbar Degenerative Disk Disease
- Lumbar Facet Arthropathy
- Lumbar Spondylosis
- Mechanical Low Backpain
- Rehabilitation for Osteoarthritis
- Rheumatoid Arthritis
- Spondylodiskitis
- Spondylolisthesis Imaging
Enhancing Healthcare Team Outcomes
Patients with spinal stenosis are often first encountered by the nurse practitioner, primary care physician, emergency department physician, and internist. If the patients are asymptomatic, there is usually no treatment necessary. Patients with pain should be encouraged to participate in an exercise program, discontinue smoking, and maintain a healthy weight. The few patients with nerve compression should be referred to an orthopedic or neurosurgeon. However, the primary care providers should educate the patient on potential complications of the surgery, which can be disabling. It is essential to take an interprofessional team including a team of physicians (physical medicine and rehabilitation, pain management, orthopedist, and/or neurosurgeons), physical therapists, occupational therapist, social workers, and case managers who can work together to coordinate mobilization with outpatient therapy and aggressive multifaceted rehabilitation so we can improve a patient's functional status. [16] Typically there is a long and difficult recovery ahead for patients with spinal stenosis, but with a coordinated effort between the various medical disciplines and departments, the best outcomes for patients can be achieved. [17](Level V)
Media
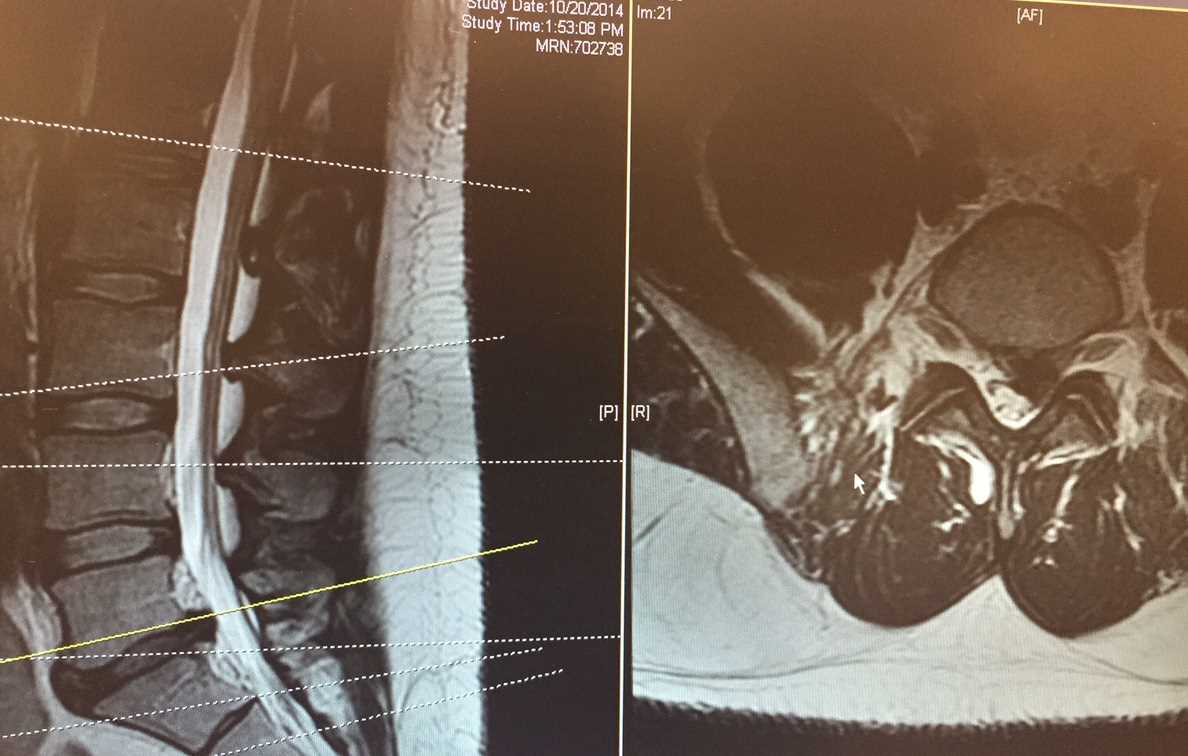
(Click Image to Enlarge)
References
Tang C, Moser FG, Reveille J, Bruckel J, Weisman MH. Cauda Equina Syndrome in Ankylosing Spondylitis: Challenges in Diagnosis, Management, and Pathogenesis. The Journal of rheumatology. 2019 Dec:46(12):1582-1588. doi: 10.3899/jrheum.181259. Epub 2019 Apr 1 [PubMed PMID: 30936280]
Glassman DM, Magnusson E, Agel J, Bellabarba C, Bransford RJ. The impact of stenosis and translation on spinal cord injuries in traumatic cervical facet dislocations. The spine journal : official journal of the North American Spine Society. 2019 Apr:19(4):687-694. doi: 10.1016/j.spinee.2018.10.015. Epub 2018 Oct 25 [PubMed PMID: 30914130]
Bindal S, Bindal SK, Bindal M, Bindal AK. Noninstrumented Lumbar Fusion with Bone Morphogenetic Proteins for Spinal Stenosis with Spondylolisthesis in the Elderly. World neurosurgery. 2019 Jun:126():e1427-e1435. doi: 10.1016/j.wneu.2019.02.251. Epub 2019 Mar 21 [PubMed PMID: 30904805]
Messiah S, Tharian AR, Candido KD, Knezevic NN. Neurogenic Claudication: a Review of Current Understanding and Treatment Options. Current pain and headache reports. 2019 Mar 19:23(5):32. doi: 10.1007/s11916-019-0769-x. Epub 2019 Mar 19 [PubMed PMID: 30888546]
Level 3 (low-level) evidenceUrits I, Burshtein A, Sharma M, Testa L, Gold PA, Orhurhu V, Viswanath O, Jones MR, Sidransky MA, Spektor B, Kaye AD. Low Back Pain, a Comprehensive Review: Pathophysiology, Diagnosis, and Treatment. Current pain and headache reports. 2019 Mar 11:23(3):23. doi: 10.1007/s11916-019-0757-1. Epub 2019 Mar 11 [PubMed PMID: 30854609]
Bagley C, MacAllister M, Dosselman L, Moreno J, Aoun SG, El Ahmadieh TY. Current concepts and recent advances in understanding and managing lumbar spine stenosis. F1000Research. 2019:8():. pii: F1000 Faculty Rev-137. doi: 10.12688/f1000research.16082.1. Epub 2019 Jan 31 [PubMed PMID: 30774933]
Level 3 (low-level) evidenceMelancia JL, Francisco AF, Antunes JL. Spinal stenosis. Handbook of clinical neurology. 2014:119():541-9. doi: 10.1016/B978-0-7020-4086-3.00035-7. Epub [PubMed PMID: 24365318]
Akar E, Somay H. Comparative morphometric analysis of congenital and acquired lumbar spinal stenosis. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2019 Oct:68():256-261. doi: 10.1016/j.jocn.2019.07.015. Epub 2019 Jul 19 [PubMed PMID: 31331753]
Level 2 (mid-level) evidenceSchroeder GD, Kurd MF, Vaccaro AR. Lumbar Spinal Stenosis: How Is It Classified? The Journal of the American Academy of Orthopaedic Surgeons. 2016 Dec:24(12):843-852 [PubMed PMID: 27849674]
Shim DM, Kim TG, Koo JS, Kwon YH, Kim CS. Is It Radiculopathy or Referred Pain? Buttock Pain in Spinal Stenosis Patients. Clinics in orthopedic surgery. 2019 Mar:11(1):89-94. doi: 10.4055/cios.2019.11.1.89. Epub 2019 Feb 18 [PubMed PMID: 30838112]
Stienen MN, Ho AL, Staartjes VE, Maldaner N, Veeravagu A, Desai A, Gautschi OP, Bellut D, Regli L, Ratliff JK, Park J. Objective measures of functional impairment for degenerative diseases of the lumbar spine: a systematic review of the literature. The spine journal : official journal of the North American Spine Society. 2019 Jul:19(7):1276-1293. doi: 10.1016/j.spinee.2019.02.014. Epub 2019 Mar 2 [PubMed PMID: 30831316]
Level 1 (high-level) evidenceKaye AD, Manchikanti L, Novitch MB, Mungrue IN, Anwar M, Jones MR, Helander EM, Cornett EM, Eng MR, Grider JS, Harned ME, Benyamin RM, Swicegood JR, Simopoulos TT, Abdi S, Urman RD, Deer TR, Bakhit C, Sanapati M, Atluri S, Pasupuleti R, Soin A, Diwan S, Vallejo R, Candido KD, Knezevic NN, Beall D, Albers SL, Latchaw RE, Prabhakar H, Hirsch JA. Responsible, Safe, and Effective Use of Antithrombotics and Anticoagulants in Patients Undergoing Interventional Techniques: American Society of Interventional Pain Physicians (ASIPP) Guidelines. Pain physician. 2019 Jan:22(1S):S75-S128 [PubMed PMID: 30717501]
Lavi ES, Pal A, Bleicher D, Kang K, Sidani C. MR Imaging of the Spine: Urgent and Emergent Indications. Seminars in ultrasound, CT, and MR. 2018 Dec:39(6):551-569. doi: 10.1053/j.sult.2018.10.006. Epub 2018 Oct 19 [PubMed PMID: 30527521]
Deer TR, Grider JS, Pope JE, Falowski S, Lamer TJ, Calodney A, Provenzano DA, Sayed D, Lee E, Wahezi SE, Kim C, Hunter C, Gupta M, Benyamin R, Chopko B, Demesmin D, Diwan S, Gharibo C, Kapural L, Kloth D, Klagges BD, Harned M, Simopoulos T, McJunkin T, Carlson JD, Rosenquist RW, Lubenow TR, Mekhail N. The MIST Guidelines: The Lumbar Spinal Stenosis Consensus Group Guidelines for Minimally Invasive Spine Treatment. Pain practice : the official journal of World Institute of Pain. 2019 Mar:19(3):250-274. doi: 10.1111/papr.12744. Epub 2018 Dec 2 [PubMed PMID: 30369003]
Level 3 (low-level) evidenceWilliamson E, Ward L, Vadher K, Dutton SJ, Parker B, Petrou S, Hutchinson CE, Gagen R, Arden NK, Barker K, Boniface G, Bruce J, Collins G, Fairbank J, Fitch J, French DP, Garrett A, Gandhi V, Griffiths F, Hansen Z, Mallen C, Morris A, Lamb SE. Better Outcomes for Older people with Spinal Trouble (BOOST) Trial: a randomised controlled trial of a combined physical and psychological intervention for older adults with neurogenic claudication, a protocol. BMJ open. 2018 Oct 18:8(10):e022205. doi: 10.1136/bmjopen-2018-022205. Epub 2018 Oct 18 [PubMed PMID: 30341124]
Level 1 (high-level) evidenceZaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical Versus Nonsurgical Treatment for Lumbar Spinal Stenosis. Spine. 2016 Jul 15:41(14):E857-E868. doi: 10.1097/BRS.0000000000001635. Epub [PubMed PMID: 27128388]
Level 3 (low-level) evidenceKoenders N, Rushton A, Verra ML, Willems PC, Hoogeboom TJ, Staal JB. Pain and disability after first-time spinal fusion for lumbar degenerative disorders: a systematic review and meta-analysis. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2019 Apr:28(4):696-709. doi: 10.1007/s00586-018-5680-3. Epub 2018 Jul 11 [PubMed PMID: 29995169]
Level 1 (high-level) evidence