Introduction
Acute mesenteric ischemia (AMI) is a condition due to a sudden decline in blood flow through the mesenteric vessels. Without appropriate and timely treatment, necrosis of the small and large intestine results, leading to sepsis and potentially death. Due to the difficulty of diagnosis and the rapid progression, the condition is life-threatening if not identified and treated early. Diagnosis is difficult because symptoms are not specific, and the index of suspicion has to be high. Mortality rates for AMI range between 60% and 80%. AMI is classified as either occlusive or nonocclusive mesenteric ischemia (NOMI). Occlusive mesenteric arterial ischemia (OMI) is subdivided into acute thromboembolism and acute thrombosis. A mesenteric venous thrombosis is a form of AMI that is covered in a different chapter.[1][2][3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Embolic patients commonly have a positive medical history of cardiovascular diseases including recent myocardial infarction, congestive heart failure, and atrial fibrillation. Causes include peripheral arterial emboli, cardiac emboli, and an atheromatous plaque that ruptured or dislodged after surgery. [4][5][6]
The typical thrombotic patient experiences a history of postprandial abdominal pain, leading to food avoidance and weight loss. Causes include atheromatous vascular disease (e.g., atherosclerosis, aortic aneurysm, aortic dissection) and decreased cardiac output due to a secondary cause (e.g., dehydration, myocardial infarction, congestive heart failure).
The NOMI patient is typically critically ill, presents with several severe comorbidities, and is hemodynamically unstable. Causes include drugs that reduce blood flow (e.g., vasopressors and ergotamines), hypotension from severe medical conditions (e.g., myocardial infarction, sepsis, CHF, and renal disease), and patients that recently received major surgery (e.g., cardiac and abdominal surgery). [7][8][9]
Epidemiology
AMI is a rare syndrome with a prevalence of 1 out of 1000 hospital admissions. For all cases of AMI, arterial embolism accounts for 40% to 50%, arterial thrombosis 25% to 30%, and NOMI represents 20% of cases. AMI is typically seen in women, older patients, and patients presenting with numerous severe comorbidities.
Pathophysiology
An acute mesenteric arterial embolism is often cardiogenic in origin and primarily affects the superior mesenteric artery (SMA). Preceding events include atrial tachyarrhythmia, congestive heart failure, myocardial ischemia or infarction, cardiomyopathy, and ventricular aneurysm, which results in thrombus formation that later embolizes to cause ischemia. Patients with acute mesenteric arterial thrombosis commonly have a pre-existing atherosclerotic disease. Vasospasm in the SMA often accompanies NOMI secondary to cardiac failure, peripheral hypoxemia, or reperfusion injury.
Toxicokinetics
In rare instances, vasopressors (e.g., cocaine and norepinephrine) and ergotamines may cause NOMI. These agents cause vasoconstriction and reduced blood flow in the mesentery, which may result in ischemia of the bowel.
History and Physical
AMI patients typically present with abdominal pain that does not correlate with physical exam findings. Tenderness to palpation occurs when the entire bowel wall is involved, which is a later presentation when necrosis begins to occur. Patients with an embolic disease typically have a history of the bowel emptying violently, followed by severe pain. The syndrome rapidly advances to ischemia and necrosis because collateral blood flow is limited. Thrombosis may take days or weeks to progress, with abdominal pain gradually worsening. Patients also may have a combination of diarrhea, distention, bloody stool, and most importantly, a history of postprandial pain, suggesting chronic mesenteric ischemia. NOMI progresses slowly, and the associated abdominal pain is not localized and varies in severity and consistency. These patients are critically ill (e.g., septic shock, cardiac disease, and respiratory failure), hypotensive, and usually on vasopressor agents.
Evaluation
Laboratory values and biomarkers for AMI are nonspecific and do not have diagnostic power. Elevated D(-)-lactate and lactate dehydrogenase are seen in late-stage AMI. CT angiography is the preferred method for imaging all types of AMI. Sensitivities for CT range from 96% to 100% and 89% to 94% for specificities. Catheter-directed angiography has fallen out of favor during the initial stages of AMI diagnosis because the added surgical stress is a burden on an already critically ill patient when used in conjunction with endovascular interventions to treat AMI. Plain abdominal radiography, duplex ultrasonography, and magnetic resonance angiography have narrow indications in diagnosing AMI.
Treatment / Management
Initial medical treatment focuses on fluid resuscitation and correcting electrolyte imbalances. Avoid vasopressors and alpha-adrenergic agents, which may cause vasospasm. Broad-spectrum antibiotics should be given before surgery to avoid abdominal sepsis if the necrotic bowel is resected.[10][11][12](B3)
Early surgical exploration is required to assess the level of ischemia and spread of necrosis. Revascularization of the bowel is the primary goal of surgery and excision of necrotic bowel is necessary. After revascularization, the bowel should be assessed for viability, which includes checking for pulses with a continuous wave Doppler, peristalsis, and normal color. Depending on the vessel occlusion type and location, open or endovascular surgical interventions are indicated in treating occlusive mesenteric arterial ischemia. Bowel resection occurs in 53% of second-look surgeries and 31% during exploratory surgery at the first attempt to revascularization. The difficulty of assessing the extent of necrosis of the bowel warrants a second-look surgery 12 to 48 hours after revascularization.
As NOMI is secondary to vasospasm rather than occlusion, treatment is medically focused and relies upon reversing the underlying cause of the low-flow state. Catheter-directed papaverine (phosphodiesterase inhibitor) delivered by a side-hole catheter or thrombolysis catheter is an interventional option.[13][14]
Differential Diagnosis
The early identification of AMI is paramount to reduce the likelihood of debilitating morbidity and high mortality. AMI has a vague presentation, and a high index of suspicion is necessary to diagnose suspected patients because of the life-threatening potential of the disease. Findings of abdominal pain out of proportion to a physical exam and cardiovascular risk factors that predispose a patient to embolism and peripheral thrombosis should alert the clinician to consider AMI. Diseases to consider in the differential diagnosis are those that cause acute abdominal pain and are therefore variable. These include acute colitis, ruptured abdominal aortic aneurysm, bowel obstruction, diabetic ketoacidosis, gastrointestinal perforation, and malignancy.
Prognosis
The prognosis of AMI is poor, with patients experiencing high morbidity and mortality rates. While there is a downward trend in mortality rates since the 1960s, the AMI mortality range remains high, occurring at rates between 60% and 80%. The specific AMI classification affects the likelihood of mortality, with acute embolism having a better prognosis, followed by NOMI and acute thrombosis. Factors associated with mortality include advanced age, bowel resection during second-look surgery, metabolic acidosis, renal insufficiency, and symptom duration.
A study by Gupta et al. found a 30-day morbidity rate of 56%. Major postoperative 30-day complications included ventilator use over 48 hours, septic shock, pneumonia, and sepsis. Follow-up surgical interventions were common, with 30% of patients revisiting the surgical department in 30-days, and 14% of patients having a hospital stay longer than 30 days.
Enhancing Healthcare Team Outcomes
AMI is a life-threatening disorder and is very difficult to diagnose. The disorder is best managed by an interprofessional team that includes a radiologist, general surgeon, internist, emergency department physician, and a gastroenterologist. If time allows, the patient should be seen by a stoma nurse, because if the bowel is found to be necrotic, most patients end up with the colostomy/ileostomy.[1][15][16]
The outcomes for patients with this disorder are guarded. Many patients are elderly with other comorbidities. Every effort should be made to adequately resuscitate the patient prior to surgery.
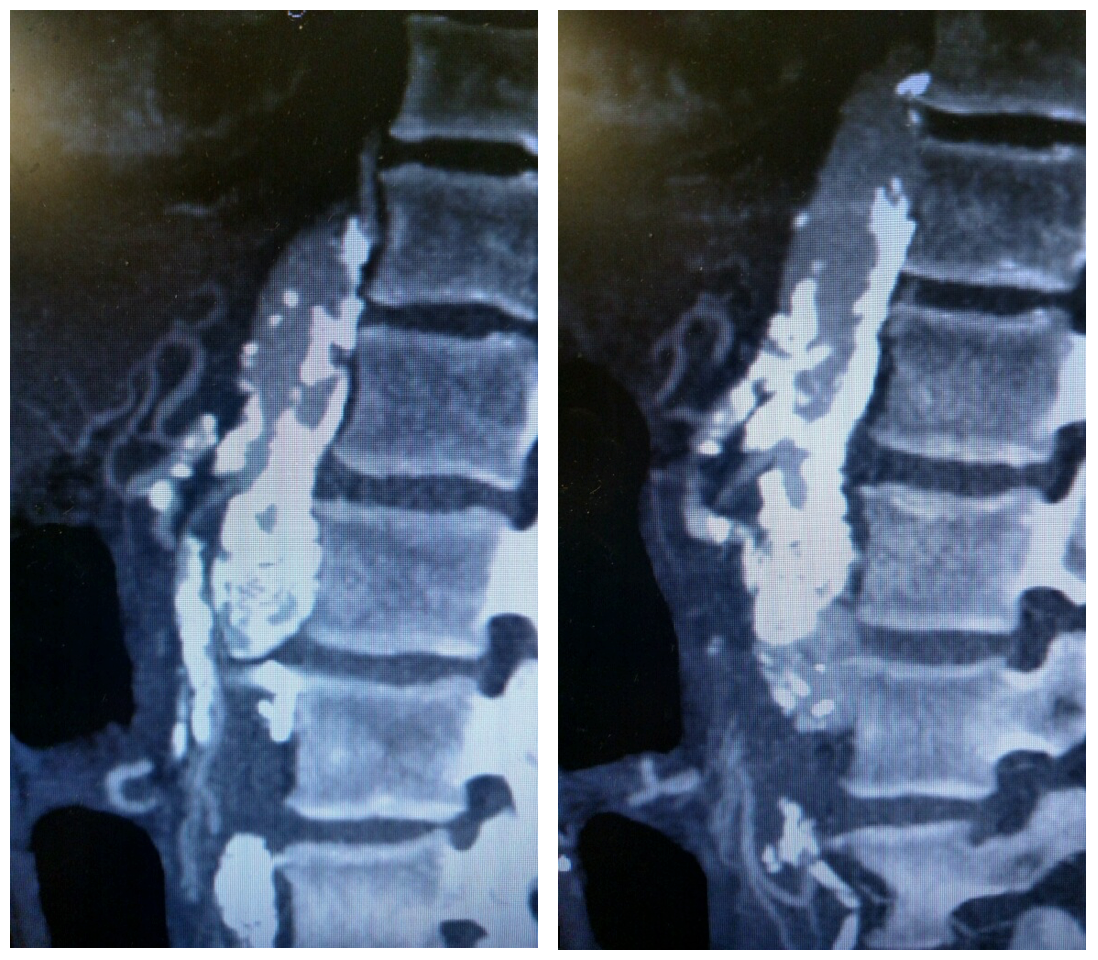
Media
(Click Image to Enlarge)
References
Bath J, Hartwig J, Dombrovskiy VY, Vogel TR. Trends in management and outcomes of vascular emergencies in the nationwide inpatient sample. VASA. Zeitschrift fur Gefasskrankheiten. 2020 Mar:49(2):99-105. doi: 10.1024/0301-1526/a000791. Epub 2019 Apr 25 [PubMed PMID: 31021300]
Khan SM, Emile SH, Wang Z, Agha MA. Diagnostic accuracy of hematological parameters in Acute mesenteric ischemia-A systematic review. International journal of surgery (London, England). 2019 Jun:66():18-27. doi: 10.1016/j.ijsu.2019.04.005. Epub 2019 Apr 16 [PubMed PMID: 30999055]
Level 1 (high-level) evidenceRobles-Martín ML, Reyes-Ortega JP, Rodríguez-Morata A. A Rare Case of Ischemia-Reperfusion Injury After Mesenteric Revascularization. Vascular and endovascular surgery. 2019 Jul:53(5):424-428. doi: 10.1177/1538574419839547. Epub 2019 Apr 14 [PubMed PMID: 30982410]
Level 3 (low-level) evidenceFranca E, Shaydakov ME, Kosove J. Mesenteric Artery Thrombosis. StatPearls. 2023 Jan:(): [PubMed PMID: 30969585]
Mizumoto M, Ochi F, Jogamoto T, Okamoto K, Fukuda M, Yamauchi T, Miyata T, Tashiro R, Eguchi M, Kitazawa R, Ishii E. Nonocclusive Mesenteric Ischemia Rescued by Immediate Surgical Exploration in a Boy with Severe Neurodevelopmental Disability. Case reports in pediatrics. 2019:2019():5354074. doi: 10.1155/2019/5354074. Epub 2019 Feb 19 [PubMed PMID: 30915251]
Level 3 (low-level) evidenceStahl K, Busch M, Maschke SK, Schneider A, Manns MP, Fuge J, Wiesner O, Meyer BC, Hoeper MM, Hinrichs JB, David S. A Retrospective Analysis of Nonocclusive Mesenteric Ischemia in Medical and Surgical ICU Patients: Clinical Data on Demography, Clinical Signs, and Survival. Journal of intensive care medicine. 2020 Nov:35(11):1162-1172. doi: 10.1177/0885066619837911. Epub 2019 Mar 25 [PubMed PMID: 30909787]
Level 2 (mid-level) evidenceKaradeniz E, Bayramoğlu A, Atamanalp SS. Sensitivity and Specificity of the Platelet-Lymphocyte Ratio and the Neutrophil-Lymphocyte Ratio in Diagnosing Acute Mesenteric Ischemia in Patients Operated on for the Diagnosis of Mesenteric Ischemia: A Retrospective Case-Control Study. Journal of investigative surgery : the official journal of the Academy of Surgical Research. 2020 Sep:33(8):774-781. doi: 10.1080/08941939.2019.1566418. Epub 2019 Mar 19 [PubMed PMID: 30885018]
Level 2 (mid-level) evidenceKurita D, Fujita T, Horikiri Y, Sato T, Fujiwara H, Daiko H. Non-occlusive mesenteric ischemia associated with enteral feeding after esophagectomy for esophageal cancer: report of two cases and review of the literature. Surgical case reports. 2019 Feb 20:5(1):36. doi: 10.1186/s40792-019-0580-2. Epub 2019 Feb 20 [PubMed PMID: 30788678]
Level 3 (low-level) evidenceSomarajan S, Muszynski ND, Olson JD, Bradshaw LA, Richards WO. Magnetoenterography for the Detection of Partial Mesenteric Ischemia. The Journal of surgical research. 2019 Jul:239():31-37. doi: 10.1016/j.jss.2019.01.034. Epub 2019 Feb 20 [PubMed PMID: 30782544]
Expert Panels on Vascular Imaging and Gastrointestinal Imaging:, Ginsburg M, Obara P, Lambert DL, Hanley M, Steigner ML, Camacho MA, Chandra A, Chang KJ, Gage KL, Peterson CM, Ptak T, Verma N, Kim DH, Carucci LR, Dill KE. ACR Appropriateness Criteria(®) Imaging of Mesenteric Ischemia. Journal of the American College of Radiology : JACR. 2018 Nov:15(11S):S332-S340. doi: 10.1016/j.jacr.2018.09.018. Epub [PubMed PMID: 30392602]
Daoud H, Abugroun A, Subahi A, Khalaf H. Isolated Superior Mesenteric Artery Dissection: A Case Report and Literature Review. Gastroenterology research. 2018 Oct:11(5):374-378. doi: 10.14740/gr1056w. Epub 2018 Oct 1 [PubMed PMID: 30344810]
Level 3 (low-level) evidenceLuther B, Mamopoulos A, Lehmann C, Klar E. The Ongoing Challenge of Acute Mesenteric Ischemia. Visceral medicine. 2018 Jul:34(3):217-223. doi: 10.1159/000490318. Epub 2018 Jun 18 [PubMed PMID: 30140688]
Bala M, Kashuk J, Moore EE, Kluger Y, Biffl W, Gomes CA, Ben-Ishay O, Rubinstein C, Balogh ZJ, Civil I, Coccolini F, Leppaniemi A, Peitzman A, Ansaloni L, Sugrue M, Sartelli M, Di Saverio S, Fraga GP, Catena F. Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery. World journal of emergency surgery : WJES. 2017:12():38. doi: 10.1186/s13017-017-0150-5. Epub 2017 Aug 7 [PubMed PMID: 28794797]
Salsano A, Salsano G, Spinella G, Palombo D, Santini F. Acute Mesenteric Ischemia: Have the Guidelines of the World Society of Emergency Surgery Analyzed All the Available Evidence? Cardiovascular and interventional radiology. 2018 Feb:41(2):358-359. doi: 10.1007/s00270-017-1817-8. Epub 2017 Oct 30 [PubMed PMID: 29086055]
Scali ST, Ayo D, Giles KA, Gray S, Kubilis P, Back M, Fatima J, Arnaoutakis D, Berceli SA, Beck AW, Upchurch GJ, Feezor RJ, Huber TS. Outcomes of antegrade and retrograde open mesenteric bypass for acute mesenteric ischemia. Journal of vascular surgery. 2019 Jan:69(1):129-140. doi: 10.1016/j.jvs.2018.04.063. Epub 2018 Jun 29 [PubMed PMID: 30580778]
Yang S, Zhao Y, Chen J, Ni Q, Guo X, Huang X, Xue G, Zhang L. Clinical Features and Outcomes of Patients With Acute Mesenteric Ischemia and Concomitant Colon Ischemia: A Retrospective Cohort Study. The Journal of surgical research. 2019 Jan:233():231-239. doi: 10.1016/j.jss.2018.08.010. Epub 2018 Aug 31 [PubMed PMID: 30502253]
Level 2 (mid-level) evidence