Introduction
Smooth muscle is found throughout the body where it serves a variety of functions. It is in the stomach and intestines where it helps with digestion and nutrient collection. It is found throughout the urinary system where it functions to help rid the body of toxins and works in electrolyte balance. It is found throughout arteries and veins where it plays a vital role in the regulation of blood pressure and tissue oxygenation. Without these vital functions, the body would not be able to maintain the most basic functions.
Smooth muscle differs from skeletal muscle in a variety of ways, perhaps the most important being its ability to be contracted and controlled involuntarily. The nervous system can use smooth muscle to tightly regulate many of the body's subsystems for life with no thought from the user. A person does not need to think about their blood pressure for it to adapt to increasing oxygen demands from exercise. The nervous system instead uses hormones, neurotransmitters, and other receptors to control smooth muscle spontaneously.
Smooth muscle also plays an important role in the disease process throughout the body. The use of bronchodilators to relax airway smooth muscle is an important and life-saving treatment in asthmatics.[1] Likewise, medications like metoclopramide can stimulate and promote gastric emptying by increasing smooth muscle signaling. Perhaps one of the most well-known uses of medical therapy and smooth muscle is the use of nitrates in the treatment of ischemic heart disease[2] where nitrates, in combination with ACEI, can improve patient mortality.[3] The singularly large impact that smooth muscle has throughout the body makes it an important topic for medical professionals to understand. As many treatments at their core rely on modifying the signaling pathways that affect smooth muscle.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
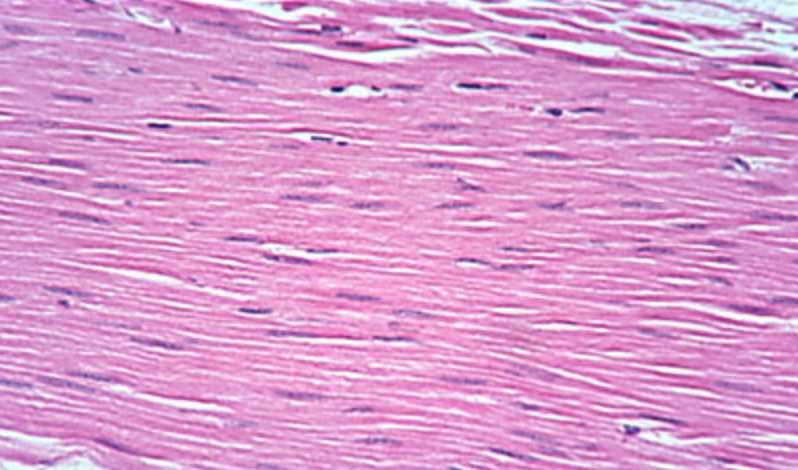
Smooth muscle differs from skeletal muscle in function. Unlike skeletal muscle, smooth muscle is capable of maintaining tone for extended periods and often contracts involuntarily. At a cellular level, smooth muscle can be described as an involuntary, non-striated muscle. Smooth muscle consists of thick and thin filaments that are not arranged into sarcomeres giving it a non-striated pattern. On microscopic examination, it will appear homogenous. Smooth muscle cytoplasm contains a large amount of actin and myosin. Actin and myosin act as the main proteins involved in muscle contraction. Actin filaments attach to dense bodies that are spread throughout the cell. Dense bodies can be observed under an electron microscope and appear dark. Another important structure is the calcium-containing sarcoplasmic reticulum which aids in sustaining contraction. The shape of the smooth muscle is described as fusiform, which is described as being round in the center and tapering at each end. Smooth muscle can tense and relax but has greater elastic properties than striated muscle. This is important in organ systems like the urinary bladder where contractile tone must be preserved.
Actin and myosin form continuous chains within the smooth muscle cell which are anchored at the dense bodies. The intermediate and thin filaments formed by the actin and myosin chains can then stretch to dense bodies located on adjacent smooth muscle cells forming a mesh-like network encircling a large number of smooth muscle cells. By implementing adherens junctions or connexins, the smooth muscle cells contract uniformly in what has been described as a spiral corkscrew fashion.
The function of smooth muscle can be expanded on a much larger scale to the organ systems it helps regulate. The functions of smooth muscle in each organ system is an incredibly broad topic and beyond the overall scope of this article. For simplicity, the basic functions of smooth muscle in the organ systems are listed below.
- Gastrointestinal tract: Propulsion of the food bolus
- Cardiovascular: Regulation of blood flow and pressure via vascular resistance
- Renal: Regulation of urine flow
- Genital: Contractions during pregnancy, propulsion of sperm
- Respiratory tract: Regulation of bronchiole diameter
- Integument: Raises hair with erector pili muscle
- Sensory: Dilation and constriction of the pupil as well as changing lens shape
Embryology
Smooth muscle is derived from both mesoderm and neural crest cells. This is because smooth muscle contributes to many different tissues throughout the body. One unique feature of neural crest cells is their migration that occurs during embryological development. For this reason, numerous tissues throughout the body are derived from neural crest cells. Neural crest cells play an important role in the development of smooth muscle throughout the body, specifically in the regulation of blood vessels.
Vascular smooth muscle cells arise from multiple origins; this becomes medically significant because it may contribute to the site-specific localization of vascular diseases. For example, atherosclerosis and aortic aneurysms often present at specific vascular locations. In the past, this was thought to be related to hemodynamics and underlying vessel structure. However, there is increasing evidence that smooth muscle cell embryonic lineage may play a role in determining the location and presentation of the disease.[4] Smooth muscle cell development is also an important factor in the development of the endothelial network. Vascular smooth muscle cells sometimes referred to as mural cells, are important for vascular development and stability. Mural cells wrap around larger vessels and are heavily relied upon in the regulation of blood flow, endothelial network growth, and vessel stability. However, little is know about the effect of their developmental origins or the signaling process that leads to vessel development. The development of vascular smooth muscle cells is an important target for vascular tissue engineering and therapeutic revascularization.[5]
Blood Supply and Lymphatics
Due to smooth muscles' widespread presence throughout the body, blood supply and lymphatic contributions vary by region. Almost every artery in the body supplies blood to smooth muscle whether that is in the form of endothelial smooth muscle located directly in the artery or smooth muscle within an organ system such as arteries of the gastrointestinal tract. It becomes more important to recognize how smooth muscles impact blood supply themselves. For example, within the cardiovascular system, smooth muscle helps to regulate blood flow by controlling the diameter of the vessel. As previously discussed vascular pathologies of smooth muscle can have devasting effects on the body and lead to significant pathology. Atherosclerosis once thought to be only a function of hemodynamics and vessel structure has more recently been shown to be linked as well to smooth muscle development.[4] Research has even shown that continuous vascular smooth muscle activation can lead to the formation of pulmonary hypertension.[6] Within the lungs, pathologic activation of smooth muscle can lead to the development of asthma. Asthma occurs when smooth muscle constriction leads to obstruction of the airway. Recent studies have shown that the smooth muscle layer may be increased in thickness before the onset of asthma even occurs, from which a genetic link may be derived.[7]
Nerves
Similar to the blood supply, the innervation of smooth muscle varies widely by location and function. Vascular smooth muscle is primarily innervated by the sympathetic nervous system. Alpha-1 and alpha-2 receptors function to cause vasoconstriction by contracting vascular smooth muscle cells leading to systemic hypertension. Beta-2 receptors also respond to sympathetic stimulation but produce a vasodilatory effect and which will lead to systemic hypotension. However, parasympathetic stimulation also plays an important role in the contraction of smooth muscle cells. Studies performed as early as 1925 demonstrated the effect of parasympathetic innervation on the gastrointestinal tract.[8] More recently researchers have been able to show how the sympathetic, parasympathetic, and enteric nervous systems all work uniformly to effect and contract smooth muscle.[9] Sympathetic stimulation of smooth muscle is received by contributions from spinal levels T1 to L2 of the spine. Each of these contributions finds its way into the sympathetic trunk which functions to route autonomic nervous supply to organs and tissue throughout the body. The parasympathetic nervous system functions in three parts, the cranial nerves, vagus nerve, and pelvic splanchnic nerves. Each nerve in the parasympathetic system regulates a specific portion of the body, the vagus, for instance, innervates the gastrointestinal tract from the esophagus to the proximal portion of the large intestines, while also sending out branches to the heart, larynx, trachea, bronchi, liver, and pancreas. The sympathetic and parasympathetic nervous systems are collectively referred to as the autonomic nervous system. The complex nature of the autonomic nervous system allows for tight unconscious control of digestions, respiratory rate, urination, heart rate, blood pressure, and many other critical body functions.
Ultimately innervation from the autonomic nervous system leads to a calcium release in smooth muscle tissue. Smooth muscle contraction is dependent on calcium influx. Calcium is increased within the smooth muscle cell through two different processes. First depolarization, hormones, or neurotransmitters cause calcium to enter the cell through L-type channels located in the caveolae of the membrane. Intracellular calcium then stimulates the release of calcium from the sarcoplasmic reticulum (SR) by way of ryanodine receptors and IP3, this process is referred to as calcium-induced calcium release.[10] Unlike skeletal muscle, smooth muscle calcium release from the sarcoplasmic reticulum is not physically coupled to the ryanodine receptor. Once calcium has entered the cell it is free to bind calmodulin, which transforms into activated calmodulin. Calmodulin then activates the enzyme myosin light chain kinase (MLCK), MLCK then phosphorylates a regulatory light chain on myosin. Once phosphorylation has occurred a conformational change takes place in the myosin head, this increases myosin ATPase activity which promotes interaction between the myosin head and actin. Cross-bridge cycling then occurs, and tension is generated. The tension generated is relative to the amount of calcium concentration within the cell. ATPase activity is much lower in smooth muscle than it is in skeletal muscle. This factor leads to the much slower cycling speed of smooth muscle. However, the longer period of contraction leads to a potentially greater force of contraction in smooth muscle. Smooth muscle contraction is enhanced even further through the use of connexins. Connexins allow for intercellular communication by allowing calcium and other molecules to flow to neighboring smooth muscle cells. This action allows for rapid communication between cells and a smooth contraction pattern.
Steps involved in smooth muscle cell contraction:
- Depolarization of membrane or hormone/neurotransmitter activation
- L-type voltage-gated calcium channels open
- Calcium-induced calcium release from the SR
- Increased intracellular calcium
- Calmodulin binds calcium
- Myosin light chain kinase activation
- Phosphorylation of myosin light chain
- Increase Myosin ATPase activity
- Myosin-P binds Actin
- Cross-bridge cycling leads to muscle tone
Dephosphorylation of myosin light chains terminates smooth muscle contraction. Unlike skeletal muscle smooth muscle is phosphorylated during its activation. This creates a potential difficulty in that simply reducing calcium levels won't produce muscle relaxation. Myosin light chain phosphatase (MLCP) is, instead is responsible for dephosphorylation of the myosin light chains ultimately leading to smooth muscle relaxation.
Muscles
Smooth muscle can be found in all the organ systems below:
- Gastrointestinal tract
- Cardiovascular: Blood vessel and lymphatic vessels
- Renal: Urinary bladder
- Genital: Male and female reproductive tracts
- Respiratory tract
- Integument: erector pili of the skin
- Sensory: Ciliary muscle and iris of the eye
Physiologic Variants
Smooth muscle consists of two types single-unit and multi-unit. Single-unit smooth muscle consists of multiple cells connected through connexins that can be stimulated in a synchronous pattern from only one synaptic input. Connexins allow for cell-to-cell communication between groups of single-unit smooth muscle cells. This inter-cellular communication allows ions and molecules to diffuse between cells giving rise to calcium waves. This unique property of single-unit smooth muscle allows for synchronous contraction to occur.[11] Multi-unit smooth muscle differs from single-unit in that each smooth-muscle cell receives its synaptic input. This allows for multi-unit smooth muscle to have much finer control. Multi-unit smooth muscle is found in the airways of the lungs, large arteries, and ciliary muscles of the eye.
Surgical Considerations
Due to autonomic control regulatory effects of smooth muscle, every surgery will be impacted by its overall function. Monitoring a patient's vital signs during surgery is paramount to a successful procedure and the stressors of surgery can have a vast impact on the autonomic nervous system which is responsible for regulating smooth muscle contraction. Surgery can even be targeted at modifying the function of smooth muscle as in the case of a vagotomy. Overstimulation of the vagus nerve has been speculated to be a possible cause for peptic ulcer disease, vagotomy is a classical surgical procedure that aims at treating this disorder by removing the vagus nerve at the level of the stomach and thus removing stimulation. However, this procedure has fallen out of favor recently due to advancements in medical therapy for peptic ulcer disease but may still show some benefit in certain patients.[12] Another example is the treatment of certain neuroendocrine tumors like an adrenal pheochromocytoma which has the potential to cause cardiovascular complications during surgery by releasing excess catecholamines. Proper management requires an in-depth knowledge of how alpha and beta blockades will affect smooth muscle and the downstream effects of those changes on bodily functions.[13] Due to its regulatory control effects, sufficient knowledge of the function and impact of smooth muscle contraction on the body systems becomes paramount when preparing for and performing any surgery.
Clinical Significance
It is estimated that in the year 2013 health care costs associated with asthma reached $81.9 billion in the United States.[14] With such a large health care burden it is astonishing to realize that asthma results from something as simple as smooth muscle contraction. Smooth muscle is an integral part of the human body, its function is required for life and can be found in almost every organ system. In the cardiovascular system, smooth muscle is used in vessels to maintain blood pressure and flow, in the lungs it opens and closes airways, in the gastrointestinal system it plays a role in motility and nutrition collection, and yet it still serves a purpose in almost every other organ system as well. The wide distribution of smooth muscle throughout the body and its many unique properties make it imperative for medical professionals to have an in-depth understanding of its anatomy, physiology, function, and disease applications.
From a functional aspect, smooth muscle physiology is responsible for maintaining and preserving every vital sign. Regardless of whether a patient presents with acute emergent disease or a chronic disease, it is likely that smooth muscle has played some role in its development. In an acute setting, many life-saving therapies directly target smooth muscle. In these settings, a firm foundation and understanding of smooth muscle will help health professionals save lives. An even broader understanding of smooth muscle will help clinicians to increase the quality of life of their patients. As part of the biopsychosocial model, it is also important to take into consideration the psycho-social factors that may be overlooked with the diseases of smooth muscle, for example, a patient diagnosed with neurogenic bladder disease may become socially isolated to avoid the embarrassment associated with their disease state. When approaching smooth muscle dysfunction, it is important for healthcare providers to appreciate the many facets of how the disease will impact their patients.
As with all aspects of medicine, a continuing amount of research will likely change our future understanding of smooth muscle and its overall effects on disease. Current research into smooth muscle has shown promise in future implications such as restoring endothelial tissue which in the future could lead to new ways to encourage revascularization. Even small changes in understanding like this could have an astronomical impact on the treatment and mortality of cardiovascular disease in the future.[4] While smooth muscle remains an exceptionally deep topic, a solid understanding of its impact on healthcare even at the most basic level will give healthcare professionals tools to provide better healthcare outcomes now and into the future.
Other Issues
Smooth muscle anatomy, physiology, and function remain a broad and relatively elusive topic despite the amount of funding and research efforts put into understanding it. As more time and effort is put into understanding smooth muscle our ability to treat the pathophysiology that comes with its dysfunction will broaden. It is important the clinicians continue to learn and study the impact that smooth muscle can have. As discussed, future methods may involve stimulating the regrowth of tissue with smooth muscle modulating factors. It is not inappropriate to think that many advances in the future of medical management will focus on impacting smooth muscle in some way or another.
Media
(Click Image to Enlarge)
References
Williams DM, Rubin BK. Clinical Pharmacology of Bronchodilator Medications. Respiratory care. 2018 Jun:63(6):641-654. doi: 10.4187/respcare.06051. Epub [PubMed PMID: 29794201]
Giuseppe C, Paul J, Hans-Ulrich I. Use of nitrates in ischemic heart disease. Expert opinion on pharmacotherapy. 2015:16(11):1567-72. doi: 10.1517/14656566.2015.1052742. Epub 2015 Jun 1 [PubMed PMID: 26027641]
Level 3 (low-level) evidence. GISSI-3: effects of lisinopril and transdermal glyceryl trinitrate singly and together on 6-week mortality and ventricular function after acute myocardial infarction. Gruppo Italiano per lo Studio della Sopravvivenza nell'infarto Miocardico. Lancet (London, England). 1994 May 7:343(8906):1115-22 [PubMed PMID: 7910229]
Level 1 (high-level) evidenceSinha S, Iyer D, Granata A. Embryonic origins of human vascular smooth muscle cells: implications for in vitro modeling and clinical application. Cellular and molecular life sciences : CMLS. 2014 Jun:71(12):2271-88. doi: 10.1007/s00018-013-1554-3. Epub 2014 Jan 18 [PubMed PMID: 24442477]
Level 3 (low-level) evidenceBargehr J, Low L, Cheung C, Bernard WG, Iyer D, Bennett MR, Gambardella L, Sinha S. Embryological Origin of Human Smooth Muscle Cells Influences Their Ability to Support Endothelial Network Formation. Stem cells translational medicine. 2016 Jul:5(7):946-59. doi: 10.5966/sctm.2015-0282. Epub 2016 May 18 [PubMed PMID: 27194743]
Khalil RA. Regulation of Vascular Smooth Muscle Function. 2010:(): [PubMed PMID: 21634065]
James AL, Noble PB, Drew SA, Mauad T, Bai TR, Abramson MJ, McKay KO, Green FHY, Elliot JG. Airway smooth muscle proliferation and inflammation in asthma. Journal of applied physiology (Bethesda, Md. : 1985). 2018 Oct 1:125(4):1090-1096. doi: 10.1152/japplphysiol.00342.2018. Epub 2018 Jul 19 [PubMed PMID: 30024335]
Veach HO. Studies on the innervation of smooth muscle: III. Splanchnic Effects on the Lower End of the Oesophagus and Stomach of the Cat. The Journal of physiology. 1925 Oct 31:60(5-6):457-78 [PubMed PMID: 16993768]
Lazebnik LB, Lychkova AE. Interaction between different parts of the autonomic nervous system in the regulation of smooth muscles in the femoral artery and trachea. Bulletin of experimental biology and medicine. 2006 Jan:141(1):5-8 [PubMed PMID: 16929950]
Level 3 (low-level) evidenceJackson WF, Boerman EM. Voltage-gated Ca(2+) channel activity modulates smooth muscle cell calcium waves in hamster cremaster arterioles. American journal of physiology. Heart and circulatory physiology. 2018 Oct 1:315(4):H871-H878. doi: 10.1152/ajpheart.00292.2018. Epub 2018 Jun 29 [PubMed PMID: 29957015]
Pogoda K, Kameritsch P, Mannell H, Pohl U. Connexins in the control of vasomotor function. Acta physiologica (Oxford, England). 2019 Jan:225(1):e13108. doi: 10.1111/apha.13108. Epub 2018 Jul 22 [PubMed PMID: 29858558]
Lagoo J, Pappas TN, Perez A. A relic or still relevant: the narrowing role for vagotomy in the treatment of peptic ulcer disease. American journal of surgery. 2014 Jan:207(1):120-6. doi: 10.1016/j.amjsurg.2013.02.012. Epub 2013 Oct 16 [PubMed PMID: 24139666]
Ramachandran R, Rewari V. Current perioperative management of pheochromocytomas. Indian journal of urology : IJU : journal of the Urological Society of India. 2017 Jan-Mar:33(1):19-25. doi: 10.4103/0970-1591.194781. Epub [PubMed PMID: 28197025]
Nurmagambetov T, Kuwahara R, Garbe P. The Economic Burden of Asthma in the United States, 2008-2013. Annals of the American Thoracic Society. 2018 Mar:15(3):348-356. doi: 10.1513/AnnalsATS.201703-259OC. Epub [PubMed PMID: 29323930]