Anatomy, Shoulder and Upper Limb, Wrist Joint
Anatomy, Shoulder and Upper Limb, Wrist Joint
Introduction
The wrist joint also referred to as the radiocarpal joint is a condyloid synovial joint of the distal upper limb that connects and serves as a transition point between the forearm and hand. A condyloid joint is a modified ball and socket joint that allows for flexion, extension, abduction, and adduction movements.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The function of the wrist joint is to provide range of motion necessary to adequately perform daily functions while maintaining a physiologic level of inherent stability. This is accomplished, in part, by the osseous articular components creating a condyloid joint that permits simultaneous movement in two perpendicular planes, in this case, dorsopalmar and radioulnar.[1] This movement allows for a wide range of motion necessary to facilitate functional use of the hand.
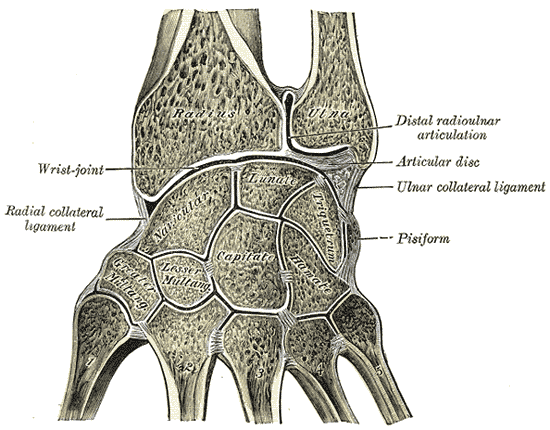
The joint itself is formed through the articulations between the distal radius and the scaphoid, lunate, and triquetrum. The proximal articulation forms a concave shape composed of a combination between the distal end of the radius and articular disk. The distal articulation is convex and composed of the scaphoid, lunate, and triquetrum bones of the proximal hand. Note that the ulna is not part of the wrist joint itself, as it articulates with the distal via the distal radioulnar joint (DRUJ).[2]
The four ligaments responsible for maintaining the stability of the joint are the palmar and dorsal radiocarpal ligaments and the ulnar and radial collateral ligaments.[2] The palmar radiocarpal ligaments are the strongest supporting structures, and these ligaments connect the radius to both the proximal and distal rows of carpal bones. Besides stability, the ligaments also ensure that the hand and forearm move together during supination.
The dorsal radiocarpal ligament is similar to the palmar ligament except that it is located on the dorsal side of the wrist joint and its alternative function is to ensure that the hand moves with the forearm during pronation. The ulnar collateral ligament runs from the ulnar styloid process to the triquetrum and pisiform bones, and the radial collateral ligament runs from the radial styloid process to the scaphoid and trapezium bones. Both collateral ligaments provide stability by reducing lateral motion.
Surrounding the wrist joint is a dual-layered joint capsule, which is common amongst all synovial joints. The outer layer is fibrous and attaches to the radius, ulna, and carpal bones. The inner layer forms a synovial membrane which secretes synovial fluid and lubricates the joint.[3]
Embryology
The wrist joint forms at weeks 5 and 6 from mesenchyme in each limb bud. Synovial joint formation is induced by Hox transcription factors at specific points along the developing limb bones.[4] Those segments will form a joint interzone composed of compacted chondrogenic precursors.[5] The interzone then cavitates to form the joint space.[6] For cavitation to occur, the interzone must reduce cellularity through organized cell death, split apart, and accumulate hyaluronan. After cavitation, morphogenesis occurs under the influence of many patterning signals to produce the proper shape of the synovial joint. The 2 opposing ends of the interzone differentiate into articular cartilage, and the surrounding mesoderm condenses to form the joint capsule.[5]
For the wrist, a slightly more complicated process occurs to develop the final joint. Initially, the lunate bone is located between the developing radius and ulnar bones. The ulna itself forms an articulating surface within the joint. Through differential growth patterns, the lunate eventually migrates into its physiologic and anatomic location, and the distal ulna eventually resorbs proximally until it no longer articulates with the wrist joint itself. In effect, the articular disk takes its place.
Blood Supply and Lymphatics
Blood supply to the forearm and hand arises from the ulnar and radial arteries. Both arteries provide vasculature to the wrist joint through penetrating branches from the dorsal and palmar carpal arches.[7]
Lymphatic drainage occurs via lymphatic vessels that connect to the epitrochlear nodes and eventually the axillary nodes.[8]
Nerves
The wrist joint receives innervation from the three major nerves of the forearm.[9]
- Median nerve: Via the anterior interosseous branch
- Radial nerve: Via the posterior interosseous branch
- Ulnar nerve: Directly through its deep motor branches
Muscles
Muscles in the forearm control wrist movement. The body of each muscle is located proximally in the forearm, and their tendons extend distally across the wrist joint. Their actions can group muscles associated with the wrist joint.[10]
- Flexion: Flexor carpi radialis, flexor carpi ulnaris, flexor digitorum superficialis, flexor digitorum profundus, and to a lesser extent flexor pollicis longus and palmaris longus
- Extension: Extensor carpi radialis longus, extensor carpi radialis brevis, extensor carpi ulnaris, extensor digitorum and to a lesser extent extensor indicis
- Abduction: Abductor pollicis longus, flexor carpi radialis, extensor carpi radialis longus, and extensor carpi radialis brevis
- Adduction: Flexor carpi ulnaris, extensor carpi ulnaris
Surgical Considerations
Carpal Tunnel Syndrome and Carpal Tunnel Release
Carpal tunnel syndrome (CTS) is a clinical condition that occurs secondary to a compression neuropathy affecting the median nerve as it transitions from the forearm to the hand via the carpal tunnel. In refractory cases that have failed nonoperative treatment/management, a carpal tunnel release is performed. The majority of carpal tunnel releases are performed with an open surgical approach, although the endoscopic procedure has been somewhat increasing in popularity but remains controversial.[11]
Technique
Landmarks are identified and marked with a skin marker. A longitudinal incision is made with the distal extent marked by the intersection of Kaplan’s cardinal line and the radial border of the fourth digit. The incision extends proximally and just distal to the wrist crease.
The dissection is carried down through the subcutaneous tissue and palmar fascia to expose the transverse carpal ligament (TCL). The palmaris brevis muscle typically lies directly on top of the TCL. Incise and feather the palmaris brevis muscle. Utilizing a combination of self-retaining and manual blunt retractors/elevators, expose the TCL for meticulous incision.
The ulnar aspect of the TCL, just radial to the hook of the hamate, is sharply incised both proximally and distally. Care is taken to protect the median nerve. Release the distal forearm fascia proximally as this can be a secondary site of compression. Assess the median nerve before closure.
Use 3-0 nylon to close the skin and dress the wound in a soft dressing. After the procedure, the patient is encouraged to elevate the wrist to reduce swelling. Pain, swelling, and stiffness is a common post-procedure, and wrist soreness may last from weeks to months. Complications are rare but include the standard complications of bleeding, infection, and nerve injury.[12]
Other Wrist Reconstruction Procedures
Other reconstructive procedures are considered in the setting of various clinical conditions and complex deformities. These conditions include but are not limited to:
- Scaphoid lunate advanced collapse (SLAC)
- Scaphoid nonunion advanced collapse (SNAC)
- Other degenerative wrist conditions
- Rheumatoid arthritis
- Pisotriquetral arthritis
- DRUJ abutment/arthrosis
Procedures utilized in the appropriate clinical setting include:
- Proximal row carpectomy (PRC)
- Scaphoid excision and 4 corner fusion
- Total wrist fusion
- Total wrist replacement
Clinical Significance
Carpal Tunnel Syndrome
The carpal tunnel is a space-bound by carpal bones and a transverse ligament. Within the tunnel run the tendons of the flexor digitorum superficialis, flexor digitorum profundus, and flexor pollicis longus in addition to the median nerve. Carpal tunnel syndrome occurs with overuse of the wrist and entrapment of the median nerve within the canal. Nerve compression leads to nocturnal paresthesia and pain.[13] Risk factors include female gender, pregnancy, diabetes, and obesity. Dorsal dislocation of the lunate can also cause acute carpal tunnel. A physical exam will show the weakness of grip, positive Tinel’s sign, positive Phalen’s test, and if severe, thenar atrophy. Numbness will be over the index and middle fingers with sparing of the thenar eminence since the palmar cutaneous branch of the median nerve enters the hand external to the carpal tunnel. Treatment includes night splinting, over the counter anti-inflammatory medications, corticosteroid injections, and as a last result, surgery which is discussed above.[13]
Arthritis
Both osteoarthritis and rheumatoid arthritis can affect the wrist joint. Osteoarthritis is general wear-and-tear arthritis that arises due to the mechanical destruction of articular cartilage. It is more common in weight-bearing joints, therefore, we will focus on rheumatoid arthritis in this review. The pathogenesis of rheumatoid arthritis is autoimmune destruction of articular cartilage.[14] Inflammatory cells and cytokines produce granulation tissue known as a pannus which erodes articular cartilage and bone. A typical presentation includes pain and morning stiffness lasting greater than 1 hour that improves with use. Joint involvement is typically symmetric and systemic symptoms such as fever, fatigue, and weight loss may be associated with severe disease. Imaging findings include joint space narrowing, bone erosion, soft tissue swelling and subchondral cysts.[15] Deformities of the fingers may also be seen in advanced disease with subluxation and ulnar deviation. The gold standard for treatment is the disease modifying agent methotrexate.
Scaphoid Fracture
More common in the younger population, a scaphoid fracture results from a blow to the wrist often by falling on an outstretched hand. The scaphoid bone is unique because of its retrograde blood supply from distal to proximal.[16] A fracture to the scaphoid can disrupt blood supply to the proximal portion of the bone. Failure to revascularize can lead to avascular necrosis. The clinical sign of a scaphoid fracture is tenderness to palpation in the anatomical snuffbox.[16] The anatomical snuffbox is a triangular depression at the base of the thumb where the scaphoid bone articulates with the radius. Its borders are the extensor pollicis longus tendon (medial), extensor pollicis longus (lateral), and radial styloid process proximally. Because the fracture is not always seen initially on x-ray, if the history and physical exam point to scaphoid fracture, the patient should either undergo additional imaging or have their wrist placed in a splint for two weeks until repeat imaging.[16] Fractures of the distal scaphoid can be treated with a splint or cast while fractures that occur in the middle or more proximally may require surgery due to a poor blood supply.
Distal Radius Fracture
The most common wrist fracture sustained secondary to a fall on an outstretched hand is a (dorsally displaced) distal radius fracture. [17] This may be referred to by some physicians as a Colles' fracture, although it is important to note that this implies that the fracture remains extra-articular in addition to dorsal displacement. Other patterns of distal radius fractures depend on the direction of the traumatic force in addition to the relative position of the wrist joint:
- Die-punch: depressed lunate facet fracture fragment at the articular surface of the distal radius
- Barton's: volar lip fracture pattern with radiocarpal joint subluxation/dislocation
- Chauffer's: radial styloid fracture
- Smith's: volar displaced fracture pattern, extra-articular
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Kauer JM. Functional anatomy of the wrist. Clinical orthopaedics and related research. 1980 Jun:(149):9-20 [PubMed PMID: 7408322]
Lewis OJ, Hamshere RJ, Bucknill TM. The anatomy of the wrist joint. Journal of anatomy. 1970 May:106(Pt 3):539-52 [PubMed PMID: 4987391]
Ralphs JR, Benjamin M. The joint capsule: structure, composition, ageing and disease. Journal of anatomy. 1994 Jun:184 ( Pt 3)(Pt 3):503-9 [PubMed PMID: 7928639]
Level 3 (low-level) evidenceSeifert A, Werheid DF, Knapp SM, Tobiasch E. Role of Hox genes in stem cell differentiation. World journal of stem cells. 2015 Apr 26:7(3):583-95. doi: 10.4252/wjsc.v7.i3.583. Epub [PubMed PMID: 25914765]
Hita-Contreras F, Martínez-Amat A, Ortiz R, Caba O, Alvarez P, Prados JC, Lomas-Vega R, Aránega A, Sánchez-Montesinos I, Mérida-Velasco JA. Development and morphogenesis of human wrist joint during embryonic and early fetal period. Journal of anatomy. 2012 Jun:220(6):580-90. doi: 10.1111/j.1469-7580.2012.01496.x. Epub 2012 Mar 19 [PubMed PMID: 22428933]
Archer CW, Dowthwaite GP, Francis-West P. Development of synovial joints. Birth defects research. Part C, Embryo today : reviews. 2003 May:69(2):144-55 [PubMed PMID: 12955858]
Level 3 (low-level) evidenceMikić Z. The blood supply of the human distal radioulnar joint and the microvasculature of its articular disk. Clinical orthopaedics and related research. 1992 Feb:(275):19-28 [PubMed PMID: 1735212]
Gaisne E, Chaise F, Bellemère P, Friol JP. [Anatomy of the lymphatic system of the arm]. Annales de chirurgie de la main et du membre superieur : organe officiel des societes de chirurgie de la main = Annals of hand and upper limb surgery. 1994:13(3):172-8 [PubMed PMID: 7524584]
Fukumoto K, Kojima T, Kinoshita Y, Koda M. An anatomic study of the innervation of the wrist joint and Wilhelm's technique for denervation. The Journal of hand surgery. 1993 May:18(3):484-9 [PubMed PMID: 8515020]
Boles CA, Kannam S, Cardwell AB. The forearm: anatomy of muscle compartments and nerves. AJR. American journal of roentgenology. 2000 Jan:174(1):151-9 [PubMed PMID: 10628472]
Kim PT, Lee HJ, Kim TG, Jeon IH. Current approaches for carpal tunnel syndrome. Clinics in orthopedic surgery. 2014 Sep:6(3):253-7. doi: 10.4055/cios.2014.6.3.253. Epub 2014 Aug 5 [PubMed PMID: 25177448]
Steinberg DR. Surgical release of the carpal tunnel. Hand clinics. 2002 May:18(2):291-8 [PubMed PMID: 12371031]
Aroori S, Spence RA. Carpal tunnel syndrome. The Ulster medical journal. 2008 Jan:77(1):6-17 [PubMed PMID: 18269111]
Angelotti F, Parma A, Cafaro G, Capecchi R, Alunno A, Puxeddu I. One year in review 2017: pathogenesis of rheumatoid arthritis. Clinical and experimental rheumatology. 2017 May-Jun:35(3):368-378 [PubMed PMID: 28631608]
Heidari B. Rheumatoid Arthritis: Early diagnosis and treatment outcomes. Caspian journal of internal medicine. 2011 Winter:2(1):161-70 [PubMed PMID: 24024009]
Rhemrev SJ, Ootes D, Beeres FJ, Meylaerts SA, Schipper IB. Current methods of diagnosis and treatment of scaphoid fractures. International journal of emergency medicine. 2011 Feb 4:4():4. doi: 10.1186/1865-1380-4-4. Epub 2011 Feb 4 [PubMed PMID: 21408000]
Wadsworth TG. Colles' fracture. BMJ (Clinical research ed.). 1990 Jul 28:301(6745):192-4 [PubMed PMID: 2203485]