Introduction
As an optical system, the eyes function in line with the basic principles of refraction.[1] Visual clarity depends on the ability to bring incident light rays to a point focus at the fovea centralis.[2] Schematically, the cornea and crystalline lens provide the requisite total dioptric power (about +60 diopters; the cornea makes up about + 40 to + 48 diopters).[3]
Accommodation is the adaptative faculty that enables clear vision with subjective variation in the linear distance of visual targets.[4] This is accomplished by the autonomic adjustment of crystalline lens dioptric powers to provide focus on the presented stimuli. The main stimulus is 'blur.'[5]
The focusing powers of the crystalline lens are directly proportional to the increase or decrease in lens convexity. At the near point of accommodation, the ciliary muscles contract and relax zonular tension, thus enabling increased convexity and focusing power. For the far point of accommodation, the ciliary muscles relax and exert greater tension on the zonules (of Zinn), thus reducing lenticular convexity.
Under typical conditions, the healthy eye responds to near-point (linear) stimuli by activating the near triad, which includes accommodation, convergence, and miosis. These mechanisms are synergistically engaged to enable single, clear binocular vision.[6]
Inhibition in one of these reflexes can most likely lead to dysfunction of accommodative response. Concerning the near reflexes, accommodation and convergence are most closely intertwined. This interrelationship can be reported as the 'accommodative convergence to accommodation (AC/A) ratio.[7] Depending on the underlying accommodative dysfunction, the ac/a ratio may be either low, normal, or high.[8]
The accommodative mechanisms can be subject to functional anomalies in maintaining visual clarity. Based on the Duke-Elder classification, these include:
- Accommodative insufficiency (AI)[9][10]
- Accommodative spasm[11]
- Accommodative inertia[12]
- Ill-sustained accommodation[13]
- Accommodative infacility[14]
AI is a functional vision anomaly characterized by the inability to sustain focus at near.[15] With this condition, the accommodative response is often suboptimal compared to expected normal ranges.[16]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Depending upon the severity and type, errors of refraction are often characterized by intermittent or sustained periods of 'blur' resulting from a defocus of visual targets.[17] When significant (moderate to high) refractive errors are uncorrected or markedly under-corrected, an extra accommodative effort is involuntarily exerted in an attempt to clear the optical defocus.[18]
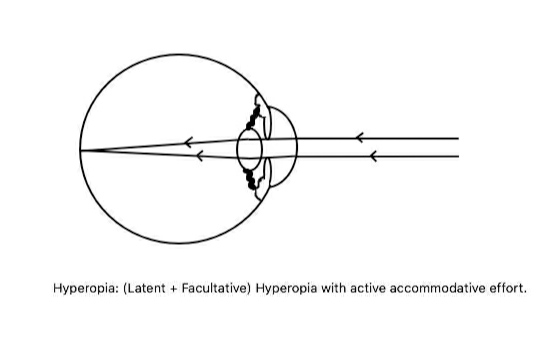
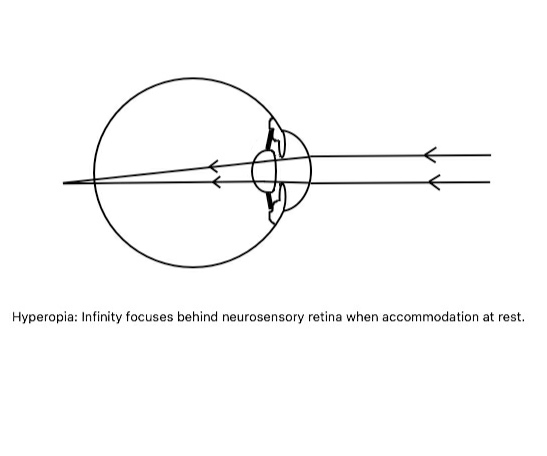
With repetitive exertion, fatigue of the ciliary muscles usually develops.[19] This, in turn, can cause an insufficient response from the accommodative faculty. Amongst the errors of refraction, hyperopic errors make up the most likely cause of AI, usually when the dioptric value of facultative hyperopia is significant (See hyperopia images).[20] At the far point of accommodation, the dioptric equivalent of accommodation is at its minimum. Individuals predisposed to near-functional visual limitations (of which hyperopes comprise a major group) are likely to present with symptoms of AI.[21]
This group of individuals at risk excludes presbyopes and those with organic causes, like autonomic degenerative diseases. These are related to other comorbid factors (such as age-related crystalline nuclear sclerosis and neurological involvement).[22]
Individuals with visual tasks that require prolonged and repetitive stimulation at the near point of accommodation can often develop symptoms of chronic fatigue consistent with AI.[11] These may include school-age children, office desk workers, high-precision artisans, etc.[23]
AI may also occur as a side effect of exposure to therapeutic doses of pharmacological agents, which include parasympatholytics (such as hyoscine and atropine) and sympathomimetic agents.[24]
Epidemiology
Accommodative dysfunction occurs in the majority of patients with binocular vision problems. Limited data are reported in the literature regarding the actual prevalence of accommodative dysfunction in the general population.[25] Several studies reviewing the prevalence of symptomatic accommodative dysfunction amongst non-presbyopic patients suggest AI is the most common finding.[26]
Most data account for the prevalence of accommodative dysfunction amongst school children ranging from 8 to 15 years of age.[27] Studies have shown that most children with CI also tend to have accommodative dysfunction.[28] Husainideen and Murali performed a meta-analysis of related literature and determined that accommodative dysfunction and asthenopia are the most commonly encountered signs in AI. Symptoms included floating words while reading, difficulty sustaining prolonged reading, and eyestrain, among others.[29][30]
Children with cerebral palsy are also reported to have lower accommodative amplitudes as compared to age-matched peers.[31] Reports of accommodative and vergence dysfunction amongst younger adults ranging from 18 to 35 years show that these are commonplace.[32] This may be due to the increasing amounts of tasks carried out with digital screens, computers, and cellular phones.[33]
History and Physical
An individual with AI tends to complain of blurry vision during near visual tasks, headaches, visual fatigue, and other asthenopic symptoms (such as eyestrain, diplopia, etc.).[15][34] Patients with this disorder can also experience a psychological ripple effect, manifesting as irritability, loss of concentration during near work, and even disinterest in academic activities (especially amongst school-age children).[35] Secondary convergence insufficiency (CI) in AI is possible, in which the symptoms tend predominantly to be due to AI.[36]
Young children may become symptomatic after an illness or fever.[37] For adults who experience vertigo, the presence of ataxia, facial asymmetry, palpebral ptosis, anisocoria, exophthalmos, excess fatigability, and strabismus should raise concerns about possible underlying severe diseases. A history of systemic vascular disease, especially diabetes mellitus, can be significant amongst adults, considering that these patients can develop autonomic denervation at the ciliary ganglion.
The clinician should consider other essential factors in the history of the patient, which include: substance abuse, trauma, infectious disease, anemia, demyelinating disease, myasthenia gravis (MG being the more localized finding), and Grave's orbitopathy.
Evaluation
For proper diagnosis of accommodative and vergence dysfunction, numerous tests and examinations should be performed to provide a proper diagnosis. Optimal correction of any existing refractive error is obligatory.[38] Measurements of accommodative function should be taken with the individual's optimal (near and distance) correction in place. Assessment of the accommodative parameters is essential to empirically determine if relevant parameters are within the expected spread of values from age and sex-matched individuals. Several tests are useful in the diagnosis of AI, including negative relative accommodation (NRA), near the point of convergence (NPC), and positive relative accommodation (PRA). Tests for accommodative facility, accommodative lead, and lag (using monocular estimation method retinoscopy) are also important in making a proper diagnosis.[39]
The NPC, for example, is useful in detecting the presence of convergence insufficiency together with AI.[40] The presence of a manifest or latent deviation can be ascertained using a unilateral or alternate cover test (see strabismic image).[41] Deviations can then be measured using prism bars or loose prisms (See prism images).[42]
Parameters representing the ability to stimulate accommodative responses optimally to presented stimuli are often reduced for individuals with AI. These patients tend to show reduced amplitudes of accommodation (AoA) beyond the minimum expected finding based on Hofstetter's formulae (15-0.25×age) or Donders table of age-expected diopters of accommodation.[13] The A of A can be determined by applying either the push-up technique or minus lens-to-blur method.[43] The latter method usually produces lower values by about 2 diopters.
Individuals who under-accommodate at near usually manifest a lag of accommodation, while patients who over-accommodate manifest an accommodative lead. Accommodative lag/lead can be determined either by the monocular estimated method (MEM) retinoscopy or by the fused cross-cylinder (FCC) test.[44]
The FCC test is the more subjective option and tends to be tedious and less accurate, especially for young children. MEM retinoscopy is performed with fixation directed to a near target. An attempt is then made to swiftly neutralize the movement of the reflex with spherical lenses of appropriate power. The expected finding is a lag between +0.25 DS and +0.75 DS. A lag greater than +1.00 DS indicates the presence of AI.
Accommodative facility testing is another method to assess the subject's ability to stimulate and relax accommodative responses at a normal rate. It also tests the accuracy of repetitive alterations in demand on the accommodative system. This is often determined using +/-2.00diopter flipper lenses.[45] This test can be conducted monocularly or binocularly. Normally, these lenses should be cleared monocularly to a minimum of 11 cycles per minute. Individuals with AI will fail the +/-2.00 diopter flipper test.
NRA/PRA values are indirect measurements of the fusional vergence abilities of the eye. The procedure for testing NRA involves adding plus lenses over the distance correction until the letters blur out. This same procedure is repeated for the PRA, with the only difference being that minus lenses are used in place of the plus lenses.[46]
Horizontal fusional vergence amplitudes (both near and far) are measured using base-in (BI) and base-out prisms (BO). BI prisms are used for negative fusional vergence (NFV), and BO prisms for positive fusional vergence (PFV) amplitudes. Blur, break, and recovery findings are then compared to Morgan's expected ranges. Individuals with symptomatic AI will demonstrate suboptimal fusional vergence in reserve to meet certain accommodative demands.
The AC/A ratio is a key factor to consider in the proper diagnosis and management of accommodative and vergence dysfunction. The normal value is 4:1. Horizontal phoria findings at near can be used to determine the AC/A ratio gradient. In determining the AC/A ratio gradient, +1.00D lenses are used to induce a prismatic effect (with the optimal near prescription in place) for esophoric findings, while -1.00D lenses are placed in the near prescription for exophoric findings. The difference between phorias with and without the gradient lens is then taken as a fractional value of the lens power used.
Treatment / Management
Treatment of AI should begin with proper refraction and correcting any underlying refractive error. It should be noted that low levels of ametropia may have an exacerbating effect on individuals with AI. Correction of these small refractive errors may substantially alleviate the symptoms of AI for the sufferer.[16] Plus, lenses are known to reduce the accommodative demand at near. Examination signs commonly found in AI patients point to the usefulness of added plus lenses in managing this condition.
Examples of these signs include low PRA and amplitude of accommodation values. Others are high retinoscopic values as measured with the MEM method and difficulty clearing the minus lenses during accommodative facility testing. This may be a problem for myopes as prescribing plus lenses can negate the refractive endpoint. Myopes, however, may benefit from bifocals or progressive lenses, especially if they are found to suffer AI or accommodative esophoria. Studies have shown that this may slow myopic progression.[47] (A1)
In cases where the cause of AI is organic or due to a paralysis of the accommodative system, plus lenses can be recommended either permanently or temporarily as needed.[48] Because such causes are organic, they may present with different levels of accommodative dysfunction between the two eyes. It is, therefore, common to see such patients with varying amounts of "adds" between the two eyes.
Vision therapy offers some promise in managing AI and is generally aimed at improving accommodative amplitude and positive fusional vergence in reserve.[16] Training regimens depend on the patient's age, personal motivation, and compliance.
Differential Diagnosis
The differential diagnosis of AI is key to the clinical decision-making processes regarding management and evaluation.[49] A key difference is that only AI presents with a reduced AoA. AI sufferers tend only to show difficulty in stimulating accommodation, while accommodative excess sufferers show difficulty in relaxing accommodation.[50] Patients with accommodative dysfunctions will find it difficult to stimulate and relax accommodation.[51] Local and/or systemic diseases may cause a phenomenon known as accommodative paralysis, marked by a sharp reduction in AoA. Drugs have also been shown to induce accommodative paralysis.
Pseudo-CI is a key differential diagnosis to actual CI. This is often considered an AI with a secondary CI finding. In true CI, the NPC is receded. However, measures of accommodation, such as the AoA, are within normal limits. In cases of CI, when an accommodative anomaly exists, there tends to be an accommodative excess. From a clinical perspective, repetition of the NPC with +0.75 or +1.00 lenses may improve performance in pseudo-CI cases. In contrast to just AI, high plus lenses tend to increase exophoria, thus making it more difficult for the patients to converge (while worsening symptoms). In such cases, tailored vision therapy can be of great value.
Certain ocular diseases like Adie's tonic pupil can present symptoms mimicking AI. Infective conditions that produce neuropathological sequelae like syphilis and meningitis may also affect accommodative ability by disrupting the parasympathetic pathway.[52] Several drugs can also affect the accommodative triad and cause an accommodative dysfunction.[53][54] A good case history is of great importance in the treatment of AI.
Prognosis
The prognosis of AI is directly related to the degree to which accompanying symptoms can be alleviated through oculovisual therapeutic management.
Complications
As with other vergence anomalies, AI can degenerate and become strabismic without proper management. AI can also present with poor academic performance in affected children.[25]
Deterrence and Patient Education
Successful outcomes of vision therapy are only achievable if the patient is compliant. Subjects with AI, particularly latent hyperopes, may become discouraged from wearing their spectacle routinely. Parents can show dissatisfaction and disagree with the recommendation of bifocal lenses for their children. Thorough approaches that encourage patient adherence and family support are crucial.[25]
Enhancing Healthcare Team Outcomes
Accommodative and vergence dysfunction can sometimes be indicative of a potentially debilitating disease.[55] Individuals with signs and symptoms of AI, especially those with a prior history of systemic vascular and autoimmune disease or patients with acute neurologic deficits, must be thoroughly assessed by clinicians.[56]
The patient may require interprofessional management, which includes neurological, hematological, pathological, and infectious disease evaluation and testing. Important signs and symptoms to consider, especially during triage, include persistent or intermittent diplopia. Cover testing and extraocular muscle (EOM) function assessment can provide better insight into underlying causes. Acute onsets of abnormalities of accommodation and vergence should seek urgent neuro-ophthalmic evaluation. [Level 1]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Shoji T, Kato N, Ishikawa S, Ibuki H, Yamada N, Kimura I, Shinoda K. Association between axial length and in vivo human crystalline lens biometry during accommodation: a swept-source optical coherence tomography study. Japanese journal of ophthalmology. 2020 Jan:64(1):93-101. doi: 10.1007/s10384-019-00700-8. Epub 2019 Nov 23 [PubMed PMID: 31760515]
Rehman I, Mahabadi N, Motlagh M, Ali T. Anatomy, Head and Neck, Eye Fovea. StatPearls. 2023 Jan:(): [PubMed PMID: 29493926]
Ayres BD, Rapuano CJ. Refractive power of the cornea. Comprehensive ophthalmology update. 2006 Sep-Oct:7(5):243-51; discussion 253-5 [PubMed PMID: 17132433]
Grzybowski A, Schachar RA, Pierscionek BK, Levy NS, Schachar IH. Importance of Accommodation and Eye Dominance for Measuring Objective Refractions. American journal of ophthalmology. 2017 Jun:178():187-188. doi: 10.1016/j.ajo.2017.03.024. Epub 2017 Apr 12 [PubMed PMID: 28411860]
Atchison DA, Varnas SR. Accommodation stimulus and response determinations with autorefractors. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2017 Jan:37(1):96-104. doi: 10.1111/opo.12340. Epub [PubMed PMID: 28030883]
Ghoushchi VP, Mompeán J, Prieto PM, Artal P. Binocular dynamics of accommodation, convergence, and pupil size in myopes. Biomedical optics express. 2021 Jun 1:12(6):3282-3295. doi: 10.1364/BOE.420334. Epub 2021 May 11 [PubMed PMID: 34221660]
Schor CM. A dynamic model of cross-coupling between accommodation and convergence: simulations of step and frequency responses. Optometry and vision science : official publication of the American Academy of Optometry. 1992 Apr:69(4):258-69 [PubMed PMID: 1565425]
Reynolds MM, Diehl NN, Mohney BG. Outcomes in accommodative esotropia with a high AC/A ratio. European journal of ophthalmology. 2021 Nov:31(6):3342-3348. doi: 10.1177/1120672120977831. Epub 2020 Dec 24 [PubMed PMID: 33356527]
Atiya A, Hussaindeen JR, Kasturirangan S, Ramasubramanian S, Swathi K, Swaminathan M. Frequency of undetected binocular vision anomalies among ophthalmology trainees. Journal of optometry. 2020 Jul-Sep:13(3):185-190. doi: 10.1016/j.optom.2020.01.003. Epub 2020 May 31 [PubMed PMID: 32493674]
Hussaindeen JR, Rakshit A, Singh NK, George R, Swaminathan M, Kapur S, Scheiman M, Ramani KK. Prevalence of non-strabismic anomalies of binocular vision in Tamil Nadu: report 2 of BAND study. Clinical & experimental optometry. 2017 Nov:100(6):642-648. doi: 10.1111/cxo.12496. Epub 2016 Nov 18 [PubMed PMID: 27859646]
Shukla Y. Accommodative anomalies in children. Indian journal of ophthalmology. 2020 Aug:68(8):1520-1525. doi: 10.4103/ijo.IJO_1973_18. Epub [PubMed PMID: 32709767]
Balke M, Skjöld G, Lundmark PO. Comparison of Short-Term Effects of Treatment of Accommodative Infacility with Low Plus Addition in Single Vision Rx or Vision Therapy: A Pilot Study. Clinical optometry. 2022:14():83-92. doi: 10.2147/OPTO.S355508. Epub 2022 Jun 2 [PubMed PMID: 35677714]
Level 3 (low-level) evidenceReindel W, Zhang L, Chinn J, Rah M. Evaluation of binocular function among pre- and early-presbyopes with asthenopia. Clinical optometry. 2018:10():1-8. doi: 10.2147/OPTO.S151294. Epub 2018 Jan 4 [PubMed PMID: 30214336]
Guo DY, Shen YY, Zhu MM, Zhan YY, Wang XW, Xia JH, Jiang B, Gu YS, Long Y. Virtual reality training improves accommodative facility and accommodative range. International journal of ophthalmology. 2022:15(7):1116-1121. doi: 10.18240/ijo.2022.07.11. Epub 2022 Jul 18 [PubMed PMID: 35919330]
Nunes AF, Monteiro PML, Ferreira FBP, Nunes AS. Convergence insufficiency and accommodative insufficiency in children. BMC ophthalmology. 2019 Feb 21:19(1):58. doi: 10.1186/s12886-019-1061-x. Epub 2019 Feb 21 [PubMed PMID: 30791877]
Hussaindeen JR, Murali A. Accommodative Insufficiency: Prevalence, Impact and Treatment Options. Clinical optometry. 2020:12():135-149. doi: 10.2147/OPTO.S224216. Epub 2020 Sep 11 [PubMed PMID: 32982529]
Wood JM, Chiu CN, Kim GH, Le J, Lee HJ, Nguyen T, Black AA. Refractive blur affects judgement of pedestrian walking direction at night. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2021 May:41(3):582-590. doi: 10.1111/opo.12811. Epub 2021 Mar 27 [PubMed PMID: 33772849]
Cufflin MP, Mallen EA. Blur adaptation: clinical and refractive considerations. Clinical & experimental optometry. 2020 Jan:103(1):104-111. doi: 10.1111/cxo.13033. Epub 2019 Dec 4 [PubMed PMID: 31801179]
Carapancea M. [Ciliospastic myopia and cilio-relaxing asthenopia as manifestations of visual fatigue caused by hypermetropic accomodative overstrain]. Fiziologia normala si patologica. 1970 Mar-Apr:16(2):129-35 [PubMed PMID: 5419018]
Ntodie M, Saunders KJ, Little JA. Correction of Low-Moderate Hyperopia Improves Accommodative Function for Some Hyperopic Children During Sustained Near Work. Investigative ophthalmology & visual science. 2021 Apr 1:62(4):6. doi: 10.1167/iovs.62.4.6. Epub [PubMed PMID: 33821881]
Arnold RW. Pseudo-false positive eye/vision photoscreening due to accommodative insufficiency. A serendipitous benefit for poor readers? Binocular vision & strabismus quarterly. 2004:19(2):75-80 [PubMed PMID: 15180592]
Level 3 (low-level) evidenceBalgos MJTD, Vargas V, Alió JL. Correction of presbyopia: An integrated update for the practical surgeon. Taiwan journal of ophthalmology. 2018 Jul-Sep:8(3):121-140. doi: 10.4103/tjo.tjo_53_18. Epub [PubMed PMID: 30294526]
Randolph SA. Computer Vision Syndrome. Workplace health & safety. 2017 Jul:65(7):328. doi: 10.1177/2165079917712727. Epub [PubMed PMID: 28628753]
Makowski AL, Lindgren K, Locke JP. Visual side effects of scopolamine/ dextroamphetamine among parabolic fliers. Aviation, space, and environmental medicine. 2011 Jul:82(7):683-8 [PubMed PMID: 21748905]
Chen AM, Roberts TL, Cotter SA, Kulp MT, Sinnott LT, Borsting EJ, Tea YC, Jones-Jordan LA, Hertle R, Mitchell GL, Eugene Arnold L, Chase C, Scheiman MM, Convergence Insufficiency Treatment Trial - Attention and Reading Trial (CITT-ART) Investigator Group. Effectiveness of vergence/accommodative therapy for accommodative dysfunction in children with convergence insufficiency. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2021 Jan:41(1):21-32. doi: 10.1111/opo.12747. Epub 2020 Oct 29 [PubMed PMID: 33119180]
Hashemi H, Khabazkhoob M, Nabovati P, Shahraki FA, Ostadimoghaddam H, Faghihi M, Aghamirsalim M, Doostdar A, Yekta A. Accommodative insufficiency in a student population in Iran. Journal of optometry. 2019 Jul-Sep:12(3):161-167. doi: 10.1016/j.optom.2018.03.006. Epub 2018 May 22 [PubMed PMID: 29802027]
Chang MY, Morrison DG, Binenbaum G, Heidary G, Trivedi RH, Galvin JA, Pineles SL. Home- and Office-Based Vergence and Accommodative Therapies for Treatment of Convergence Insufficiency in Children and Young Adults: A Report by the American Academy of Ophthalmology. Ophthalmology. 2021 Dec:128(12):1756-1765. doi: 10.1016/j.ophtha.2021.05.017. Epub 2021 Jun 23 [PubMed PMID: 34172337]
DuPrey KM, Webner D, Lyons A, Kucuk CH, Ellis JT, Cronholm PF. Convergence Insufficiency Identifies Athletes at Risk of Prolonged Recovery From Sport-Related Concussion. The American journal of sports medicine. 2017 Aug:45(10):2388-2393. doi: 10.1177/0363546517705640. Epub 2017 May 16 [PubMed PMID: 28511593]
Watt T, Robertson K, Jacobs RJ. Refractive error, binocular vision and accommodation of children with Down syndrome. Clinical & experimental optometry. 2015 Jan:98(1):3-11. doi: 10.1111/cxo.12232. Epub 2014 Nov 13 [PubMed PMID: 25395109]
Satgunam P, Datta S, Sumalini R. Near vision in individuals with Down syndrome: a vision screening study. Eye (London, England). 2019 Aug:33(8):1254-1260. doi: 10.1038/s41433-019-0402-6. Epub 2019 Mar 26 [PubMed PMID: 30914784]
Leat SJ. Reduced accommodation in children with cerebral palsy. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 1996 Sep:16(5):385-90 [PubMed PMID: 8944183]
Level 2 (mid-level) evidenceFranco S, Moreira A, Fernandes A, Baptista A. Accommodative and binocular vision dysfunctions in a Portuguese clinical population. Journal of optometry. 2022 Oct-Dec:15(4):271-277. doi: 10.1016/j.optom.2021.10.002. Epub 2021 Nov 28 [PubMed PMID: 34852966]
Jaiswal S, Asper L, Long J, Lee A, Harrison K, Golebiowski B. Ocular and visual discomfort associated with smartphones, tablets and computers: what we do and do not know. Clinical & experimental optometry. 2019 Sep:102(5):463-477. doi: 10.1111/cxo.12851. Epub 2019 Jan 21 [PubMed PMID: 30663136]
Sterner B, Gellerstedt M, Sjöström A. Accommodation and the relationship to subjective symptoms with near work for young school children. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2006 Mar:26(2):148-55 [PubMed PMID: 16460315]
Abdi S, Brautaset R, Rydberg A, Pansell T. The influence of accommodative insufficiency on reading. Clinical & experimental optometry. 2007 Jan:90(1):36-43 [PubMed PMID: 17177664]
Level 3 (low-level) evidenceMikolich JR, Alloush N. Percutaneous transluminal coronary angioplasty in dextrocardia: case report. Cardiovascular and interventional radiology. 1988 Jun:11(3):140-2 [PubMed PMID: 2971444]
Level 3 (low-level) evidenceCacho P, García A, Lara F, Seguí MM. Diagnostic signs of accommodative insufficiency. Optometry and vision science : official publication of the American Academy of Optometry. 2002 Sep:79(9):614-20 [PubMed PMID: 12322932]
Hashemi H, Nabovati P, Yekta A, Aghamirsalim M, Rafati S, Ostadimoghaddam H, Razmjoo H, Khabazkhoob M. Convergence Insufficiency in the Geriatric Population. Optometry and vision science : official publication of the American Academy of Optometry. 2021 Jun 1:98(6):613-619. doi: 10.1097/OPX.0000000000001709. Epub [PubMed PMID: 34081652]
López-Artero E, Garzón N, Rodríguez-Vallejo M, García-Montero M. Feasibility of optical quality analysis system for the objective assessment of accommodation insufficiency: a phase 1 study. Journal of optometry. 2021 Jul-Sep:14(3):287-294. doi: 10.1016/j.optom.2020.06.004. Epub 2020 Aug 12 [PubMed PMID: 32800453]
Level 2 (mid-level) evidenceScheiman M, Kulp MT, Cotter SA, Lawrenson JG, Wang L, Li T. Interventions for convergence insufficiency: a network meta-analysis. The Cochrane database of systematic reviews. 2020 Dec 2:12(12):CD006768. doi: 10.1002/14651858.CD006768.pub3. Epub 2020 Dec 2 [PubMed PMID: 33263359]
Level 1 (high-level) evidenceMorimoto T, Kanda H, Hirota M, Nishida K, Fujikado T. Insufficient accommodation during binocular near viewing in eyes with intermittent exotropia. Japanese journal of ophthalmology. 2020 Jan:64(1):77-85. doi: 10.1007/s10384-019-00695-2. Epub 2019 Nov 9 [PubMed PMID: 31707606]
Pang Y, Gnanaraj L, Gayleard J, Han G, Hatt SR. Interventions for intermittent exotropia. The Cochrane database of systematic reviews. 2021 Sep 13:9(9):CD003737. doi: 10.1002/14651858.CD003737.pub4. Epub 2021 Sep 13 [PubMed PMID: 34516656]
Level 1 (high-level) evidenceChen Y, Zhang C, Ding C, Tao C, Bao J, Zheng J, Chen H. Repeatability of two subjective accommodative amplitude measurements and agreement with an objective method. Clinical & experimental optometry. 2019 Jul:102(4):412-417. doi: 10.1111/cxo.12884. Epub 2019 Mar 13 [PubMed PMID: 30866109]
Ren Q, Yue H, Zhou Q. [Effects of orthokeratology lenses on the magnitude of accommodative lag and accommodativeconvergence/accommodation]. Zhong nan da xue xue bao. Yi xue ban = Journal of Central South University. Medical sciences. 2016 Feb:41(2):169-73. doi: 10.11817/j.issn.1672-7347.2016.02.009. Epub [PubMed PMID: 26932215]
Adler P, Scally AJ, Barrett BT. Test-retest reproducibility of accommodative facility measures in primary school children. Clinical & experimental optometry. 2018 Nov:101(6):764-770. doi: 10.1111/cxo.12691. Epub 2018 May 8 [PubMed PMID: 29740867]
Chen M, Long Q, Gu H, Hong J. Accommodation changes after visian implantable collamer lens with central hole for high myopia: A STROBE-compliant article. Medicine. 2019 Jul:98(28):e16434. doi: 10.1097/MD.0000000000016434. Epub [PubMed PMID: 31305467]
Fulk GW, Cyert LA, Parker DE. A randomized trial of the effect of single-vision vs. bifocal lenses on myopia progression in children with esophoria. Optometry and vision science : official publication of the American Academy of Optometry. 2000 Aug:77(8):395-401 [PubMed PMID: 10966065]
Level 1 (high-level) evidenceGarcía-Montero M, Antona B, Barrio AR, Nieto-Zayas C, Martínez-Alberquilla I, Hernández-Verdejo JL. The role of clinical diagnosis criteria on the frequency of accommodative insufficiency. International journal of ophthalmology. 2019:12(4):647-653. doi: 10.18240/ijo.2019.04.20. Epub 2019 Apr 18 [PubMed PMID: 31024821]
Houston CA, Jone D, Weir CR. An unusual cause of asthenopia: "pseudo-accommodative insufficiency" associated with a high AC:A ratio. The British journal of ophthalmology. 2000 Dec:84(12):1438 [PubMed PMID: 11186867]
Level 3 (low-level) evidencePorcar E, Montalt JC, Pons ÁM, España-Gregori E. Symptomatic accommodative and binocular dysfunctions from the use of flat-panel displays. International journal of ophthalmology. 2018:11(3):501-505. doi: 10.18240/ijo.2018.03.22. Epub 2018 Mar 18 [PubMed PMID: 29600186]
Wick B, Yothers TL, Jiang BC, Morse SE. Clinical testing of accommodative facility: Part 1. A critical appraisal of the literature. Optometry (St. Louis, Mo.). 2002 Jan:73(1):11-23 [PubMed PMID: 12363234]
Sakai T, Shikishima K, Mizobuchi T, Yoshida M, Kitahara K. Bilateral tonic pupils associated with neurosyphilis. Japanese journal of ophthalmology. 2003 Jul-Aug:47(4):368-71 [PubMed PMID: 12842205]
Level 3 (low-level) evidenceOstrin LA, Glasser A. Autonomic drugs and the accommodative system in rhesus monkeys. Experimental eye research. 2010 Jan:90(1):104-12. doi: 10.1016/j.exer.2009.09.015. Epub 2009 Sep 24 [PubMed PMID: 19782072]
Level 3 (low-level) evidenceGhobadi M, Nabovati P, Hashemi H, Talaei A, Fathi HR, Yekta Y, Ostadimoghaddam H, Yekta A, Khabazkhoob M. Accommodative and convergence anomalies in patients with opioid use disorder. Clinical & experimental optometry. 2022 May:105(4):392-397. doi: 10.1080/08164622.2021.1932431. Epub 2021 Jun 24 [PubMed PMID: 34167446]
Musa MJ, Zeppieri M. Foster Kennedy Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 35881754]
Musa M, Aluyi-Osa G, Zeppieri M. Foster Kennedy Syndrome (FKS): A Case Report. Clinics and practice. 2022 Jul 12:12(4):527-532. doi: 10.3390/clinpract12040056. Epub 2022 Jul 12 [PubMed PMID: 35892442]
Level 3 (low-level) evidence