Introduction
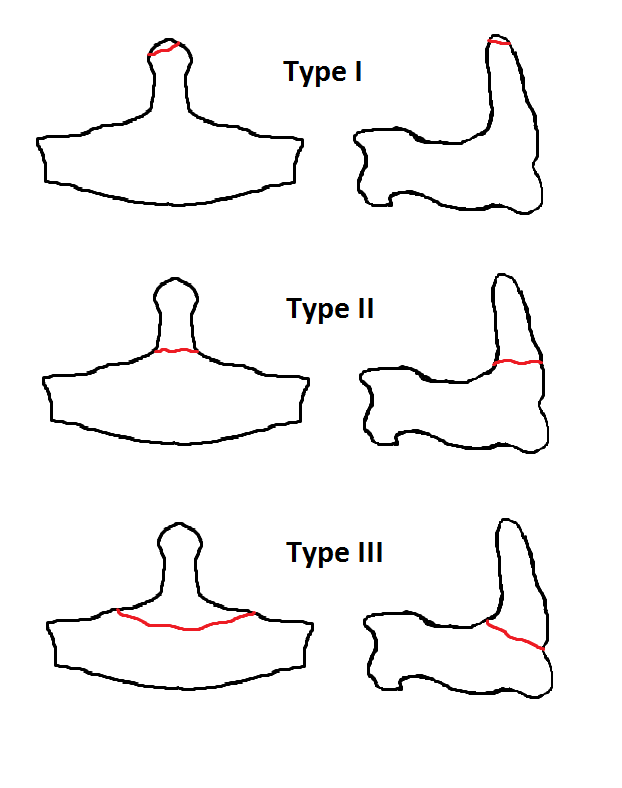
The odontoid process, known as the dens, is a bony element extending superiorly from the second cervical vertebra (C2, or the axis). The odontoid process is a pivotal point for rotation, with the first cervical vertebra (C1, or the atlas) rotating around it to provide the most significant single component of lateral rotation in the cervical spine. Fractures of the odontoid process are categorized into 3 types: type I, type II, and type III, depending on the location and morphology of the fracture.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Odontoid fractures occur as a result of trauma to the cervical spine. In younger patients, they are typically the result of high-energy trauma, which can occur as the result of a motor vehicle, diving, or skiing accident. In older people, the trauma can occur due to lower energy impacts such as falls from a standing position. The most common mechanism of injury is hyperflexion of the cervical spine, pushing the head and C1 vertebra backward. If the energy, mechanism, and resulting force are severe enough, the odontoid will fracture with varying displacement and degrees of comminution. The risk is elevated further if the patient's bone density is compromised secondary to osteopenia/osteoporosis.
The transverse ligament runs posterior to the odontoid process and attaches to the lateral masses of C1 bilaterally. If the cervical spine is excessively flexed, the transverse ligament can transmit the excessive anterior forces to the odontoid process, resulting in an odontoid fracture.[1]
Epidemiology
Odontoid fractures constitute 10% to 20% of cervical spine fractures in adults and emerge as the predominant fracture subtype among individuals aged 65 and older.[2] The axis is the most common vertebra to be involved in cervical spine injuries, and odontoid fractures account for 50% of all C2 fractures.[3] These fractures exhibit a bimodal distribution, with peaks observed among young adults and older individuals.[2]
Odontoid fractures result from an interaction between the load magnitude and bone quality.[4] This results from high-impact forces in young cohorts in contrast to more trivial injuries among older people. Hyperflexion injury causes the skull and C1 arch to produce traction at the odontoid process. The transverse ligament functions to limit the posterior movement of the dens.[5] Type II is the most common of the types of odontoid fractures and accounts for over 50% of all odontoid fractures. Type III odontoid fractures make up most of the remaining odontoid fractures. Type I odontoid fractures are rare.[1] Road traffic accidents cause most cases.[3] In a study of over 30,000 patients, the average age of the cohorts was 77, with 54% female patients.[6]
Pathophysiology
Advanced age and large occiput-C2 angles are predictive of the odontoid fracture angle.[7] In cases of odontoid fractures, the atlantoaxial joint and the fractured segment move together, leading to severe pain during neck movements.[5] The nonunion rate following conservative management can be as high as 90% due to thin bony trabeculae and watershed zones at the base of the dens.[5]
Nonoperative management of odontoid fractures can lead to solid fusion, unstable nonunion, and fibrous nonunion.[8] The fusion is governed by the pattern of injury, fracture subtype, slope of the fracture line, angulation (more or less than 11°), displacement (more or less than 5 mm), blood supply, bone quality, and age of the fracture and that of the patient.[2] Patients aged 50 or older experience a 21-fold increase in nonunion rate.[9]
History and Physical
Younger patients with an odontoid fracture often have identifiable recent trauma such as a motor vehicle accident, sports-related impact, diving accident, or fall from a height or downstairs. In contrast, older patients, who tend to have less resilient bones, can sustain an odontoid fracture after minor trauma, including falling from ground level or running into a door or cabinet, in addition to the mechanisms observed in the younger cohort.
During physical examination, patients may report high posterior cervical pain exacerbated by motion and tenderness to palpation. Additionally, patients may present with dysphagia attributed to a retropharyngeal hematoma or associated parapharyngeal swelling. Patients may also exhibit myelopathic spinal cord injuries, manifesting as paresthesias in the arms or legs, weakness of the limbs, or other neurological dysfunctions. Odontoid fractures typically result in fewer spinal cord injuries due to the relatively spacious dimensions of the spinal canal at the level of the odontoid process compared to the diameter of the spinal cord.
Evaluation
Evaluation of Odontoid Fractures
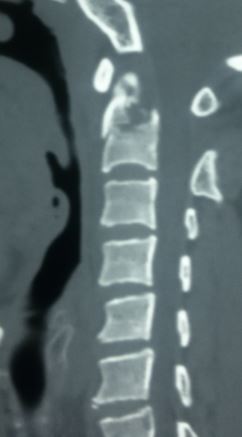
X-rays of the cervical spine include lateral, anterior-posterior, and open-mouth views of the fracture (see Images. Odontoid Fracture (Lateral) and Odontoid Fracture (AP)). Although computed tomography (CT) scans offer higher sensitivity and specificity rates, experienced clinicians can still discern suspected injuries using radiographs. Moreover, flexion-extension radiographs are recommended for suspected occipitocervical instability, particularly useful in type I odontoid fractures or cases involving os odontoideum. Initial stability observed on upright radiographs often indicates stability during follow-up assessments.[10]
CT spine imaging offers superior resolution of the bony elements, facilitating precise identification and characterization of odontoid fractures. This also allows the recognition of anatomical anomalies, such as defects in the posterior arch of C1, which can inform management strategies.[11] In addition, CT angiography is justified in cases where the fracture extends near vascular zones, allowing assessment of the vertebral artery's course during posterior fixation.[12]
Magnetic resonance imaging (MRI) is utilized to evaluate the integrity of the transverse ligament and the spinal cord in patients with neurological deficits.[13]
Classification of Odontoid Fractures
Anderson and D'Alonzo classification of odontoid fractures, which is the most commonly used classification of fractures of the odontoid process of C2, categorizes odontoid fractures into 3 types based on their anatomic location (see Image. Odontoid Fracture Classification).
- Type I odontoid fractures involve the apex of the dens and are generally stable. However, if instability is suspected, particularly due to the avulsion of the alar ligament, dynamic radiographic imaging is recommended.
- Type II odontoid fractures involve the neck of the odontoid process and are categorized based on the pattern of the fracture line into anterior oblique, posterior oblique, and horizontal variants.[5] They represent the most common subtype and are generally considered unstable. The type IIA variant specifically features unstable comminuted fractures at the base of the dens.[5]
- Type III fractures extend into the body of C2.[14] Non-surgical treatment with external immobilization remains the preferable option for most patients with this type of fracture.[15]
Grauer classification of odontoid fractures divides odontoid fractures into 3 groups, particularly subdividing type II fractures into 3 subclasses (A, B, and C).
Treatment / Management
The primary goal of management is to achieve fracture stability.[2] A fibrous union can often provide sufficient stability.[10][17] In cases without instability observed on flexion/extension views or ligamentous injury detected on an MRI scan, external immobilization using a rigid brace or halo vest can facilitate fracture healing, typically occurring within 12 weeks.[10](B3)
Conservative Approach
For patients exhibiting the following criteria, a conservative approach may be justified:
For types I, II, and III fractures, halo fixation or cervical traction along with a rigid cervical collar results in fusion rates of:
- Type I fractures: 100% in most cases
- Type II fractures: Approximately 90%
- Type II fractures: 60% [13]
A cervical collar offers biomechanical superiority over halo orthoses with minimal risk of concurrent device-related complications.[2] Soft collars deliver comparable benefits in aged patients compared to rigid collars.[18] The use of a halo vest was not associated with increased mortality.[19] Both conservative treatment and surgery exhibited similarly low in-hospital mortality rates.(B2)
Indications for Surgery in Type II Fractures
Criteria of Instability
- Fracture age equal to or more than 6 months
- Comminuted fracture
- Rupture of the transverse ligament
- Nonreducible or malaligned fracture pattern
- Dens displacement more or equal to 6 mm
- Angulation greater more or equal to 10°
- Fracture gap more than or equal to 2 mm
- Lateral mass gap >2 mm [20][21]
Both anterior and posterior fixation techniques have equivalent clinical results.[5] Anterior odontoid screw fixation preserves neck movements while providing fusion rates of 80% to 100%.[5](B2)
The posterior inferior fracture type and concurrent tear of the transverse ligament are selected for the posterior fixation.[5] Historically, Brooks and Gallie undertook posterior cervical fusion, and later Dickman and Sonntag's methods incorporated the use of sublaminar wires and bone grafts, providing a fusion rate of 86%. This was followed by a transarticular screw, as described by Jeanneret and Magerl, which provided almost 100% fusion.[13] The Goel-Harms technique (C1 lateral mass and C2 pedicle screws) is now an excellent alternative to anterior fixation.[22][23](B2)
After the advent of the Goel posterior joint manipulation technique, most of the once irreducible atlantoaxial dislocations could be reduced, and the need for transoral odontoidectomy became almost nil.[24] Bone grafting provides long-term stability.[13] Sublaminar wiring can impinge upon the spinal canal, and C1-C2 joint fusion restricts neck ranges of movements.[13]
Anterior Fixation
Nakanishi described the technique of anterior odontoid screw fixation, which is advocated for:
- Fractures less than 6 months old
- Fractures with an anterior-inferior sloping fracture line
- Transverse fractures without any comminuted segments at the base [2][5] (B2)
There is no need for bone grafting and minimal risk of injury to the vertebral artery. There are also mild limitations in functional abilities following the procedure.[25](B2)
Prerequisites for the Anterior Odontoid Screw Fixation
The bicortical purchase and superior and posterior breach of the odontoid tip significantly govern postoperative alignment.[26] Lag, Herbert, and Acutrak screws are used for anterior odontoid fixation.[27][28] Both single or 2-screw anterior odontoid screws have shown similar clinical results.[13] There are anatomical limitations and variability in the placement of two odontoid screws.[29][30](B2)
Subsets not Appropriate for Anterior Odontoid Screw Fixation
- Type IIA fractures
- Rupture of the transverse ligament
- Associated atlantoaxial dislocation
- Osteopenia
- Injury older than 6 months
- Anterior oblique fracture slope
- Short neck
- Barrel-shaped chest
- Severe kyphosis [5][20] (B2)
Recent Advances in Assisting Instrumentation
- O-arm navigation [31]
- A 3D print model [32][33]
- Endoscopic approach [34]
- Robotics [35]
- CT-guided navigation [36] (B2)
The odontoid screw fixation technique is not recommended for children aged 6 and younger.[37] However, this technique is feasible for children aged 6 to 18, with careful consideration of appropriate screw diameter, length, and angle based on actual CT measurements.[37] An anterior approach is more suitable for younger cohorts.[2](B2)
There is a level II recommendation for surgical stabilization in geriatric patients due to the high risk of high nonunion.[5] Meta-analysis has revealed superior fusion with posterior fixations.[5] There is a high risk of reoperation rates owing to osteopenia following anterior odontoid fixation.[23] There is also an increased risk of postoperative pneumonia, swallowing dysfunction, and increased technical problems.[2][20](B2)
A marked variation exists in the treatment strategies and follow-up and imaging algorithms.[38] Major comorbidities and older age are significant factors in refraining from surgical fixation.[39] The proportion of crossover from primary external immobilization to surgery was 14.4%, whereas the proportion of revision surgery in the primary surgical group was 9.5%.[40] Operative treatment has shown an average increase of 3.7% per year; operative management for managing geriatric odontoid fractures nearly doubled between 2003 and 2017.[6] Increased sagittal balance and bone fusion within the atlantodental interspace are associated with a high risk of nonunion.[41] In older patients, a duration from injury to surgery exceeding 7 days appears to carry a 48 times higher risk for nonunion, even with anterior odontoid screw fixation.[42] (B2)
Differential Diagnosis
To prevent unnecessary interventions, it is crucial to recognize the entities mentioned below that can be mistaken for an odontoid fracture.
Os Odontoideum
Os odontoideum is a recognized anatomical variant of the normal odontoid process. During development, the spine features multiple ossification centers, including one in the odontoid process, one in the odontoid tip, and one in the vertebral body. If the ossification centers in the odontoid process and the vertebral body do not fuse properly, the odontoid process can appear detached from the vertebral body, resembling a type II odontoid fracture. In younger children, where complete ossification of the spine has not yet occurred, the expected growth pattern and ossification can also simulate a type II odontoid fracture.[43]
Persistent Ossiculum Terminale
The rostral tip of the odontoid process has a separate ossification center during development from the remaining odontoid process. When the 2 ossification centers fail to fuse, there can be a persistent gap between the odontoid process and the tip of the odontoid process, which can mimic a type I odontoid fracture.
Prognosis
Children typically achieve stable fusion with halo immobilization. However, patients aged 50 and older have a 21 times higher risk of nonunion with halo immobilization.[13]
The fusion rate is 88% when surgery is performed within 6 months of injury, dropping to 25% when surgery is delayed beyond 18 months after injury.[13] If a patient fails external immobilization and is within 6 months of the injury, anterior odontoid screw placement is an option.
For cases with a displaced distal fracture segment or facet malalignment causing cervicomedullary compression that is irreducible despite traction, transoral ventral decompression may be necessary before posterior fusion. Alternatively, anterior extrapharyngeal open reduction and internal fixation have been introduced to manage this problem.[44]
Complications
Mortality at the time of injury is observed in 25% to 40% of patients.[45] Among survivors, most are typically neurologically intact. However, this can introduce the risk of instability at the atlantoaxial region and spinal cord injury, leading to conditions such as Brown-Sequard syndrome, spinal cord transection, cruciate paralysis, myelopathy, and persistent disabling neck pain in approximately 25% of patients.[13][46][47]
Concurrent injuries associated with and complicating odontoid fractures may include anterior cervical wedge fracture, atlantooccipital dissociation, cervical burst fracture, cervical facet dislocation, cervical spinous process fracture, extension cervical teardrop fracture, flexion cervical teardrop fracture, Hangman's fracture, isolated transverse process fractures, and Jefferson fracture.
Deterrence and Patient Education
Postoperatively, patients should be monitored for retropharyngeal hematoma, dysphagia, aspiration, vocal cord paralysis, and surgical site infections. Patients must recognize these signs and symptoms and immediately contact their surgeon's office.
Enhancing Healthcare Team Outcomes
Odontoid fractures typically result from trauma to the cervical spine, often affecting younger patients. Effective patient care requires a coordinated interprofessional team approach to provide care that minimizes the risk of further injury. Trauma nurses are responsible for cervical spine immobilization; radiologists are critical in reviewing radiographic imaging. Neurosurgeons and orthopedic spine surgeons collaborate to provide definitive care and minimize the risk of further injury.
Physiatrists and rehabilitation nurses are critical in coordinating care and providing feedback to the interprofessional healthcare team. Pharmacists often assist the team in maintaining pain control for acutely injured patients. Nurses liaise between various disciplines, assisting in patient assessment, monitoring patients intraoperatively, and addressing questions from patients and their families. The entire team of interprofessional healthcare members should maintain accurate and updated patient records to ensure everyone operates with the same information. This collaborative approach among the care team leads to improved patient outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Robinson AL, Möller A, Robinson Y, Olerud C. C2 Fracture Subtypes, Incidence, and Treatment Allocation Change with Age: A Retrospective Cohort Study of 233 Consecutive Cases. BioMed research international. 2017:2017():8321680. doi: 10.1155/2017/8321680. Epub 2017 Jan 15 [PubMed PMID: 28182084]
Level 2 (mid-level) evidenceDeluca A, Wichlas F, Deininger C, Traweger A, Mueller EJ. Reevaluation of a classification system: stable and unstable odontoid fractures in geriatric patients-a radiological outcome measurement. European journal of trauma and emergency surgery : official publication of the European Trauma Society. 2022 Aug:48(4):2967-2976. doi: 10.1007/s00068-022-01985-0. Epub 2022 May 21 [PubMed PMID: 35597894]
Bakhsh A, Alzahrani A, Aljuzair AH, Ahmed U, Eldawoody H. Fractures of C2 (Axis) Vertebra: Clinical Presentation and Management. International journal of spine surgery. 2020 Dec:14(6):908-915. doi: 10.14444/7139. Epub 2020 Dec 29 [PubMed PMID: 33560250]
Benca E, Zderic I, van Knegsel KP, Caspar J, Hirtler L, Fuchssteiner C, Strassl A, Gueorguiev B, Widhalm H, Windhager R, Varga P. Biomechanical Assessment of Fracture Loads and Patterns of the Odontoid Process. Spine. 2022 Sep 1:47(17):1212-1220. doi: 10.1097/BRS.0000000000004369. Epub 2022 Jul 14 [PubMed PMID: 35853162]
Sommer F, Kirnaz S, Goldberg J, McGrath L Jr, Navarro-Ramirez R, Gadjradj P, Medary B, Härtl R. Treatment of Odontoid Fractures in Elderly Patients Using C1/C2 Instrumented Fusion Supplemented With Bilateral Atlantoaxial Joint Spacers: A Case Series. International journal of spine surgery. 2022 Jun:16(3):442-449. doi: 10.14444/8250. Epub [PubMed PMID: 35772974]
Level 2 (mid-level) evidenceAlluri R, Bouz G, Solaru S, Kang H, Wang J, Hah RJ. A Nationwide Analysis of Geriatric Odontoid Fracture Incidence, Complications, Mortality, and Cost. Spine. 2021 Jan 15:46(2):131-137. doi: 10.1097/BRS.0000000000003734. Epub [PubMed PMID: 33038203]
Gold C, Seaman S, Yamaguchi S. Relationship between odontoid fracture angle and cervical sagittal balance. Surgical neurology international. 2021:12():157. doi: 10.25259/SNI_829_2020. Epub 2021 Apr 14 [PubMed PMID: 33948327]
Florman JE, Gerstl JVE, Kilgallon JL, Riesenburger RI. Fibrous Nonunion of Odontoid Fractures: Is It Safe To Accept Nonoperative Management? A Systematic Review. World neurosurgery. 2022 Aug:164():298-304. doi: 10.1016/j.wneu.2022.05.116. Epub 2022 Jun 2 [PubMed PMID: 35659587]
Level 1 (high-level) evidenceLennarson PJ, Mostafavi H, Traynelis VC, Walters BC. Management of type II dens fractures: a case-control study. Spine. 2000 May 15:25(10):1234-7 [PubMed PMID: 10806499]
Level 2 (mid-level) evidenceWilson C, Hoyos M, Huh A, Priddy B, Avila S, Mendenhall S, Anokwute MC, Eckert GJ, Stockwell DW. Institutional review of the management of type II odontoid fractures: associations and outcomes with fibrous union. Journal of neurosurgery. Spine. 2021 Jan 22:34(4):623-631. doi: 10.3171/2020.8.SPINE20860. Epub 2021 Jan 22 [PubMed PMID: 33482645]
Butt BB, Gagnet P, Patel R, Aleem I. Congenital defect of the posterior arch of C1: a case report. Journal of spine surgery (Hong Kong). 2021 Jun:7(2):214-217. doi: 10.21037/jss-20-628. Epub [PubMed PMID: 34296035]
Level 3 (low-level) evidenceWindsor TA, Tewelde SZ, Blosser KM, Richardson AC. An odontoid fracture and vertebral artery injury in fast-track. Clinical case reports. 2020 Sep:8(9):1847-1849. doi: 10.1002/ccr3.2952. Epub 2020 May 25 [PubMed PMID: 32983515]
Level 3 (low-level) evidenceRao G, Apfelbaum RI. Odontoid screw fixation for fresh and remote fractures. Neurology India. 2005 Dec:53(4):416-23 [PubMed PMID: 16565532]
Fazzolari B, Jannelli G, Conti E, Delitala A, Tessitore E, Brunori A. Clinical and radiological outcome after minimally invasive surgical approach for type II unstable odontoid fractures. Neuro-Chirurgie. 2021 Jul:67(4):350-357. doi: 10.1016/j.neuchi.2020.11.014. Epub 2020 Dec 15 [PubMed PMID: 33338497]
Rizvi SAM, Helseth E, Aarhus M, Harr ME, Mirzamohammadi J, Rønning P, Mejlænder-Evjensvold M, Linnerud H. Favorable prognosis with nonsurgical management of type III acute odontoid fractures: a consecutive series of 212 patients. The spine journal : official journal of the North American Spine Society. 2021 Jul:21(7):1149-1158. doi: 10.1016/j.spinee.2021.02.003. Epub 2021 Feb 10 [PubMed PMID: 33577924]
Moscolo F, Meneghelli P, Boaro A, Impusino A, Locatelli F, Chioffi F, Sala F. The use of Grauer classification in the management of type II odontoid fracture in elderly: Prognostic factors and outcome analysis in a single centre patient series. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2021 Jul:89():26-32. doi: 10.1016/j.jocn.2021.04.015. Epub 2021 Apr 29 [PubMed PMID: 34119278]
Sucu HK. A True Percutaneous Anterior Odontoid Screw Fixation: The Results of 42 Cases by a Single Surgeon. World neurosurgery. 2022 Oct:166():e892-e904. doi: 10.1016/j.wneu.2022.07.125. Epub 2022 Aug 7 [PubMed PMID: 35948230]
Level 3 (low-level) evidenceColeman N, Chan HH, Gibbons V, Baker JF. Comparison of Hard and Soft Cervical Collars for the Management of Odontoid Peg Fractures in the Elderly. Geriatric orthopaedic surgery & rehabilitation. 2022:13():21514593211070263. doi: 10.1177/21514593211070263. Epub 2022 Mar 18 [PubMed PMID: 35320993]
Honda A, Michihata N, Iizuka Y, Mieda T, Takasawa E, Ishiwata S, Matsui H, Fushimi K, Yasunaga H, Chikuda H. Clinical features and early post-operative complications of isolated C2 odontoid fractures: a retrospective analysis using a national inpatient database in Japan. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2021 Dec:30(12):3631-3638. doi: 10.1007/s00586-021-06862-9. Epub 2021 May 6 [PubMed PMID: 33959795]
Level 2 (mid-level) evidenceFiani B, Doan T, Covarrubias C, Shields J, Sekhon M, Rose A. Determination and optimization of ideal patient candidacy for anterior odontoid screw fixation. Surgical neurology international. 2021:12():170. doi: 10.25259/SNI_165_2021. Epub 2021 Apr 19 [PubMed PMID: 34084598]
Koshimizu H, Nakashima H, Ito K, Ando K, Kobayashi K, Kato F, Sato K, Deguchi M, Matsubara Y, Inoue H, Kanemura T, Urasaki T, Yoshihara H, Wakao N, Shinjo R, Imagama S. Risk factors of non-union in Anderson-D'Alonzo type III odontoid fractures with conservative treatment. Journal of orthopaedics. 2021 Mar-Apr:24():280-283. doi: 10.1016/j.jor.2021.03.012. Epub 2021 Mar 29 [PubMed PMID: 33897130]
Yee TJ, Strong MJ, Willsey MS, Oppenlander ME. Cervical 1-2 Posterior Instrumented Fusion Utilizing Computer-Assisted Navigation With Harvest of Rib Strut Autograft: 2-Dimensional Operative Video. Operative neurosurgery (Hagerstown, Md.). 2021 May 13:20(6):E433. doi: 10.1093/ons/opab029. Epub [PubMed PMID: 33571358]
Jain AK, Tawari M, Rathore L, Sahana D, Mishra H, Kumar S, Sahu RK. An experience with Goel-Harms C1-C2 fixation for type II odontoid fractures. Journal of craniovertebral junction & spine. 2022 Apr-Jun:13(2):175-181. doi: 10.4103/jcvjs.jcvjs_22_22. Epub 2022 Jun 13 [PubMed PMID: 35837432]
Govindasamy R, Preethish-Kumar V, Gopal S, Rudrappa S. Is Transoral Surgery Still a Relevant Procedure in Atlantoaxial Instability? International journal of spine surgery. 2020 Oct:14(5):657-664. doi: 10.14444/7096. Epub 2020 Oct 19 [PubMed PMID: 33077434]
Wolan-Nieroda A, Maciejczak A, Drużbicki M, Guzik A. Determinants of health-related quality of life in patients with fracture of the axis vertebrae. Scientific reports. 2021 Sep 24:11(1):19075. doi: 10.1038/s41598-021-98476-w. Epub 2021 Sep 24 [PubMed PMID: 34561492]
Level 2 (mid-level) evidenceTyagi G, Patel KR, Singh GJ, Uppar AM, Beniwal M, Rao KVLN, Pruthi N, Bhat D, Somanna S, Chandramouli B, Dwarakanath S. Anterior Odontoid Screw Fixation for C2 Fractures: Surgical Nuances, Complications, and Factors Affecting Fracture Union. World neurosurgery. 2021 Aug:152():e279-e288. doi: 10.1016/j.wneu.2021.05.077. Epub 2021 May 28 [PubMed PMID: 34058365]
Duransoy YK, Mete M, Ünlü Ünsal Ü, Aydın M, Zileli M. Anterior odontoid screw fixation using Acutrak screw: Report of 19 patients. Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery : TJTES. 2021 Jul:27(4):472-477. doi: 10.14744/tjtes.2020.86345. Epub [PubMed PMID: 34213004]
Pongmanee S, Kaensuk S, Sarasombath P, Rojdumrongrattana B, Kritworakarn N, Liawrungrueang W. Anterior screw fixation for type II odontoid process fractures: A single-center experience with the double Herbert screw fixation technique (Retrospective cohort study). Annals of medicine and surgery (2012). 2022 Feb:74():103337. doi: 10.1016/j.amsu.2022.103337. Epub 2022 Feb 5 [PubMed PMID: 35198171]
Level 2 (mid-level) evidenceAcharya S, Kumar M, Ghosh JD, Adsul N, Chahal RS, Kalra KL. Morphometric parameters of the odontoid process of C2 vertebrae, in Indian population, a CT evaluation. Surgical neurology international. 2021:12():494. doi: 10.25259/SNI_417_2021. Epub 2021 Sep 30 [PubMed PMID: 34754544]
Choudhary KS, Doddamani RS, Devarajan LJ, Agrawal M, Sawarkar D, Meena RK, Varma S, Kumar A, Singh P, Chandra PS, Kale SS. Feasibility of Double Anterior Odontoid Screw: A CT-Based Morphometric Analysis of the Axis in Adult Indian Population. Neurology India. 2020 Nov-Dec:68(6):1361-1366. doi: 10.4103/0028-3886.304125. Epub [PubMed PMID: 33342869]
Level 2 (mid-level) evidenceZhao R, Ding W, Li X, Han FY, Yang D, Yang S. Application of the O-arm Intraoperative Imaging System to Assist Anterior Cervical Screw Fixation for Odontoid Fractures. Journal of visualized experiments : JoVE. 2022 Aug 30:(186):. doi: 10.3791/64471. Epub 2022 Aug 30 [PubMed PMID: 36121255]
Abreu PG, Romero C, Lourenço JAB, Pappamikail L, Brito M, Teles P, Correia J. Case report: Challenging post-traumatic pseudoarthrosis of C2 odontoid fracture and extreme C1-C2 subluxation. Surgical neurology international. 2022:13():137. doi: 10.25259/SNI_10_2022. Epub 2022 Apr 8 [PubMed PMID: 35509539]
Level 3 (low-level) evidenceLi Y, Lin J, Wang Y, Luo H, Wang J, Lu S, Xu Y. Comparative study of 3D printed navigation template-assisted atlantoaxial pedicle screws versus free-hand screws for type II odontoid fractures. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2021 Feb:30(2):498-506. doi: 10.1007/s00586-020-06644-9. Epub 2020 Oct 23 [PubMed PMID: 33098009]
Level 2 (mid-level) evidenceKedia S, Sawarkar D, Sharma R, Mansoori N, Lalwani S, Gupta D, Kumar R, Kale SS. Endoscopic Anterior Odontoid Screw Fixation for the Odontoid Fracture: A Cadaveric Pilot Study. Asian journal of neurosurgery. 2021 Jan-Mar:16(1):67-71. doi: 10.4103/ajns.AJNS_312_20. Epub 2021 Mar 20 [PubMed PMID: 34211869]
Level 3 (low-level) evidenceLebl DR, Avrumova F, Abjornson C, Cammisa FP. Cervical Spine Navigation and Enabled Robotics: A New Frontier in Minimally Invasive Surgery. HSS journal : the musculoskeletal journal of Hospital for Special Surgery. 2021 Oct:17(3):333-343. doi: 10.1177/15563316211026652. Epub 2021 Jul 1 [PubMed PMID: 34539275]
Issa M, Kiening KL, Unterberg AW, Scherer M, Younsi A, Fedorko S, Oskouian RJ, Chapman JR, Ishak B. Morbidity and Mortality in Patients over 90 Years of Age Following Posterior Stabilization for Acute Traumatic Odontoid Type II Fractures: A Retrospective Study with a Mean Follow-Up of Three Years. Journal of clinical medicine. 2021 Aug 24:10(17):. doi: 10.3390/jcm10173780. Epub 2021 Aug 24 [PubMed PMID: 34501228]
Level 2 (mid-level) evidenceDou H, Xie C, Zhu S, Wang X, Huang Q, Zhou F. Feasibility analysis of the use of anterior screw fixation in the treatment of pediatric odontoid fracture. Translational pediatrics. 2021 Apr:10(4):967-972. doi: 10.21037/tp-21-101. Epub [PubMed PMID: 34012844]
Level 2 (mid-level) evidenceWatts A, Athanassacopoulos M, Breakwell L, Chiverton N, Cole A, Ivanov M, Tomlinson J. Management of C2 odontoid peg fragility fractures - A UK survey of spinal surgeons. Injury. 2022 Mar:53(3):1057-1061. doi: 10.1016/j.injury.2021.09.057. Epub 2021 Oct 1 [PubMed PMID: 34635337]
Level 3 (low-level) evidenceRizvi SAM, Helseth E, Rønning P, Mirzamohammadi J, Harr ME, Brommeland T, Aarhus M, Høstmælingen CT, Ølstørn H, Rydning PNF, Mejlænder-Evjensvold M, Utheim NC, Linnerud H. Odontoid fractures: impact of age and comorbidities on surgical decision making. BMC surgery. 2020 Oct 14:20(1):236. doi: 10.1186/s12893-020-00893-7. Epub 2020 Oct 14 [PubMed PMID: 33054819]
Rizvi SAM, Helseth E, Harr ME, Mirzamohammadi J, Rønning P, Mejlænder-Evjensvold M, Linnerud H. Management and long-term outcome of type II acute odontoid fractures: a population-based consecutive series of 282 patients. The spine journal : official journal of the North American Spine Society. 2021 Apr:21(4):627-637. doi: 10.1016/j.spinee.2020.11.012. Epub 2020 Dec 17 [PubMed PMID: 33346157]
Yamaguchi S, Park BJ, Takeda M, Mitsuhara T, Shimizu K, Chen PF, Woodroffe RW. Healing process of Type II odontoid fractures after C1-C2 posterior screw fixation: Predictive factors for pseudoarthrosis. Surgical neurology international. 2022:13():116. doi: 10.25259/SNI_198_2022. Epub 2022 Mar 31 [PubMed PMID: 35509583]
Ricciardi L, Trungu S, Scerrati A, De Bonis P, Rustemi O, Mazzetto M, Lofrese G, Cultrera F, Barrey CY, Di Bartolomeo A, Piazza A, Miscusi M, Raco A. Odontoid screw placement for Anderson type II odontoid fractures: how do duration from injury to surgery and clinical and radiological factors influence the union rate? A multicenter retrospective study. Journal of neurosurgery. Spine. 2021 Jan 1:34(1):27-31. doi: 10.3171/2020.6.SPINE20318. Epub 2020 Oct 2 [PubMed PMID: 33007754]
Level 2 (mid-level) evidencePereira Duarte M, M Das J, Camino Willhuber GO. Os Odontoideum. StatPearls. 2024 Jan:(): [PubMed PMID: 31194437]
Patkar S. Unstable odontoid fractures: technical appraisal of anterior extrapharyangeal open reduction internal fixation for irreducible unstable odontoid fractures. Patient series. Journal of neurosurgery. Case lessons. 2021 Nov 15:2(20):CASE21501. doi: 10.3171/CASE21501. Epub 2021 Nov 15 [PubMed PMID: 36061093]
Level 3 (low-level) evidenceMaeda K, Ichiba T. Unusual Clinical Course of Odontoid Fracture: Transient Prehospital Cardiopulmonary Arrest. Cureus. 2020 Dec 18:12(12):e12157. doi: 10.7759/cureus.12157. Epub 2020 Dec 18 [PubMed PMID: 33489569]
Zygogiannis K, Georgoulis JD, Antonopoulos SI, Gourtzelidis G, Chatzikomninos I. Cruciate Paralysis Following a Displaced Type II Odontoid Fracture: A Case Report. Cureus. 2022 May:14(5):e25181. doi: 10.7759/cureus.25181. Epub 2022 May 21 [PubMed PMID: 35747018]
Level 3 (low-level) evidenceAgunbiade S, Belton PJ, Mesfin FB. Spinal Cord Transection in a Type II Odontoid Fracture From a Ground-Level Fall. Cureus. 2020 Dec 28:12(12):e12342. doi: 10.7759/cureus.12342. Epub 2020 Dec 28 [PubMed PMID: 33520537]