Introduction
According to the American Society of Plastic Surgeons, nearly 45,000 rhinoplasties were performed in the United States (US) in 2022, making it the third most popular facial plastic surgical procedure after blepharoplasty and rhytidectomy (2022 ASPS Statistics). Since its first description by John Roe in 1887, both the technical and philosophical approaches to rhinoplasty have evolved substantially. Current indications for rhinoplasty vary widely, including aesthetic enhancement, improvement of nasal airflow, gender affirmation, and oncologic or traumatic reconstruction, each requiring different techniques.[1] Early rhinoplasty was exclusively cosmetic and relied predominantly on reduction maneuvers. As understanding of nasal anatomy advanced, a more proportional approach to the operation developed, incorporating cartilage grafting and suture refinement.
Among the pioneers of rhinoplasty are Jacques Joseph, Maurice Cottle, Samuel Fomon, and Jack Sheen, whose techniques remain in use today to varying degrees. Joseph, a German surgeon at the turn of the twentieth century, emphasized the importance of correcting the nasal septum while reducing the dorsal hump and strongly advocated for the positive psychological effects of aesthetic surgery.[2] Cottle, the founder of the American Rhinological Society in 1954, invented the dorsal preservation technique for hump reduction and recognized the critical role of the nasal septum in shaping the external nose, famously stating, "As the septum goes, so goes the nose."[3] Additionally, Cottle co-founded the American Academy of Facial Plastic and Reconstructive Surgery in 1964 with Goldman and Fomon. Fomon, who served as a US Army Medical Corps officer during World War I, began his career as an anatomist and brought his expertise and passion for teaching to facial surgery. He made education in rhinoplasty theory and technique widely available in the United States during the mid-twentieth century.[4] Sheen is perhaps best known for his seminal textbook Aesthetic Rhinoplasty (1978 1st ed), but his insights opened doors to considering nonCaucasian/ethnic rhinoplasty and revision rhinoplasty. The latter has greatly benefited from the spreader graft technique he described in 1984.[5][6]
As rhinoplasty techniques have evolved, so has the understanding of the complex interplay among aesthetics, breathing, smell, and psychology, all of which are intricately connected within the small confines of the nose. An adverse outcome in these areas can mar the patient's perception of the result, while a good outcome can provide multifactorial benefits. The nose is the central landmark of the face; its proportions and symmetry are directly linked to the overall perception of facial beauty, making the stakes very high when attempting significant modifications.[7] The broad range of nasal appearances among genders, ethnicities, and ages, coupled with anatomical variations from trauma and prior surgery, along with the myriad described operative techniques and the preferences of each patient, makes achieving consistent results challenging even for very experienced surgeons. The nose continues to change shape over time, especially after surgery, and predicting its appearance 20 years in the future is more art than science. For this reason, it has been said that rhinoplasty surgeons can only truly appreciate the extent of their surgical skills as they prepare to retire.
Assessing outcomes in rhinoplasty is complex and challenging, requiring subjective and objective input from patients and surgeons. Surgeons typically rely on physical examinations and comparisons of preoperative and postoperative photographs within the context of normative nasofacial proportions to evaluate a surgery's success. They may also review their revision and complication rates, which are typically reported to be up to 15% and 3%, respectively, and track patient satisfaction.[8][9][10]
Patient-reported outcomes include validated instruments such as the Standardized Cosmesis and Health Nasal Outcomes Survey, Rhinoplasty Outcomes Evaluation, and Nasal Obstruction Symptom Evaluation questionnaires. These tools seek to quantify postoperative quality of life changes and are arguably the most important measures of a surgery's effectiveness.[11][12][13] Consequently, patient selection is considered the most critical predictor of operative success and the most effective means of avoiding litigation or the need for secondary surgery, which is notoriously complex.
Planning revision surgery, whether for cosmetic or functional reasons, must account for the difficulty of meticulous dissection through a previously operated and scarred field, the potential lack of available cartilage for grafting and structural support, injury to the vascularity of the nose and its impact on healing in the septum and skin-soft tissue envelope (SSTE), and the psychological impact on the patient, which may affect rapport and reasonable expectations. These factors, among others, must be considered when performing what is widely regarded as the most complicated of facial plastic surgical procedures.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
A deep understanding of anatomical and physiological relationships within the nose is the cornerstone of good decision-making during rhinoplasty. Modifying 1 nasal structure will frequently impact others and affect the overall appearance of the nose and face. Common examples of these unintended consequences, or the "Newton third law of rhinoplasty" (every action has an equal and opposite reaction), include tip rotation after cephalic trimming, increased alar flare after tip deprojection, tip deprojection after opening the nose, tip rotation and columellar retraction after septocolumellar suturing, and many others.
External Nose
The external nose consists of a bony and cartilaginous framework enveloped by muscle, soft tissue, and skin.
Nasal bones and cartilage
The upper third of the nose, or "bony vault," is composed of the paired nasal bones medially and the frontal processes of the maxillae laterally (see Image. External Nasal Skeleton), which constitute the bony pyramid. Medially, the nasal bones join with the ethmoid bone's perpendicular plate—the bony septum's upper component—which extends inferiorly and posteriorly to the bony vault. The middle third, or "midvault," is formed by the upper lateral cartilages, which attach to the nasal bones cranially.
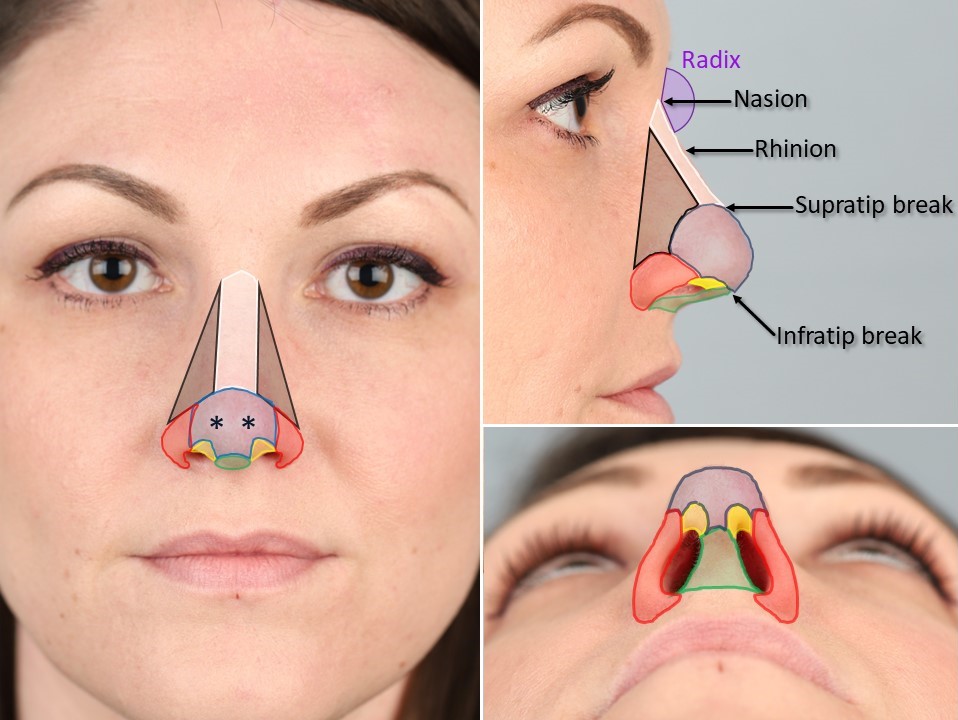
The nasal bones overlap the upper lateral cartilages for 4 to 5 mm on either side of the rhinion, providing additional support for the midvault. The rhinion, the point at which the nasal bones end in the midline and give way to the cartilaginous septum, is an important anatomical landmark concerning the aesthetics of the dorsal contour (see Image. External Nasal Anatomy). The upper lateral cartilages fuse with the cartilaginous septum along the dorsal midline of the nose, forming an angle classically described as 10 to 15 degrees.[14] This narrow portion of the nasal passage is called the internal nasal valve. During surgical maneuvers, it is important to maintain or widen this angle to optimize postoperative airflow.
The 2 lower lateral, or alar, cartilages each consist of a lateral and a medial crus, which support the columella and the lateral aspect of the nasal tip, respectively. Between the medial and lateral crura is a bend known as the middle or intermediate crus. The intermediate crura constitute the domes underlying the tip-defining points of the nose, which are the small, paired reflections seen in direct lighting (see Image. External Nasal Anatomy).
The nasal tip has 3 major support mechanisms: the size/shape/resiliency of the lower lateral cartilages, the attachment of the lower lateral cartilages to the upper lateral cartilages at the "scroll" region, and the attachment of the medial crura of the lower lateral cartilages to the caudal septum, and 6 minor tip support mechanisms: the interdomal ligaments, the SSTE, the anterior septal angle, the anterior nasal spine, the membranous septum, and the sesamoid cartilages).[15] They also provide the framework for the external nasal valves, the regions bounded by the caudal margins of the lower lateral cartilages, the septum and columella, and the nasal sill. Of note is that the nasal alae do not contain cartilage but rather fibrofatty tissue, as the lateral crura of the lower lateral cartilages pass just superior to the alar grooves.
Muscles
The main mimetic muscles of the nose are the nasalis, dilator naris, levator labii alaeque nasi, and depressor septi. These muscles are enclosed and interconnected by a fibrous fascia that constitutes part of the superficial musculoaponeurotic system of the face. The clinical significance of the nasal muscles is easily underestimated. Still, they are important for maintaining patency of the external nasal valve, as evidenced by the unilateral nasal airway obstruction commonly experienced by patients with Bell palsy and other types of facial paralysis.[16] For this reason, some surgeons prefer to raise local flaps in a subdermal plane rather than the deeper and better-perfused submuscular plane when performing nasal reconstruction to avoid malposition of the muscles and potential nasal valve dysfunction.
Septum and skin-soft tissue envelope
While the SSTE of the nose varies greatly in thickness and texture by sex, age, ethnicity, and history of prior surgery or trauma, the tissue covering the rhinion is the thinnest, followed by the upper third, and then lower third, which is the thickest and most sebaceous. The latter's texture resembles that of the forehead and glabella, which are important considerations for reconstruction, particularly with paramedian forehead flaps.[17]
Internal Nose
The internal nose comprises the septum, the turbinates, the olfactory cleft, the lateral nasal wall, and the nasal floor, all covered by mucosa. The septum and the inferior turbinates are the most critical structures with respect to aesthetic and airway concerns.
Septum
The nasal septum, a rigid structure covered by mucosa, is located in the midline of the nasal cavity, where it separates the left and right nasal passages and constitutes the principal support of the external nose. The anterior aspect of the septum is occupied by the quadrangular cartilage, while the posterior portion is bony.
The bony components are the perpendicular plate of the ethmoid superiorly, the vomer posteriorly, and the maxillary crest inferiorly (see Image. Internal Nasal Anatomy). The junction of the quadrangular cartilage and the perpendicular plate of the ethmoid bone at the dorsal aspect of the septum is known as the "keystone" area, and its preservation during surgery is critical for the maintenance of support for the external nose and avoidance of a saddle deformity (see Image. Saddle Nose).
The septum is the primary determinant of the dorsal projection of the nose in the midvault, and the caudal portion of the septum influences how low the columella hangs below the alar margins; septal deviations in these areas are liable to result in visible distortion of the external nasal contour. At the junction between the dorsal and caudal margins of the septum lies the anterior septal angle, which supports the nasal tip and contributes to nasal projection. When performing a septoplasty or septal cartilage harvest, it is important to leave an L-shaped strut of 10 to 15 mm in width along the dorsal and caudal margins of the quadrangular cartilage to provide adequate structural support for the nose. Similarly, the keystone and the junction of the caudal septum and the anterior nasal spine should ideally be left intact or carefully reconstructed if violated.
The superior aspect of the septum also constitutes 1 of the boundaries of the internal nasal valve, along with the caudal margin of the upper lateral cartilage and the head of the inferior turbinate. The internal valve is the narrowest portion of the nasal passage, with an angle ranging from 52 degrees if completely patent to 0 degrees if obstructed by the septal swell body, a collection of glandular tissue within the submucosa of the superior aspect of the nasal septum encountered in about half of patients.[14]
Turbinates
Turbinates are bony outgrowths along the lateral nasal wall covered by mucosa and containing vascular erectile tissue. These structures form pathways wherein the air flows and is warmed and humidified. They also help remove particles from the inspired air and assist in regulating the airflow by contracting and expanding.
Within each nasal passage are superior, middle, and inferior turbinates, with the superior and middle being processes of the ethmoid bone and the inferior turbinate, or concha, being a separate bone altogether (see Image. Internal Nasal Anatomy). Most of the airflow passes below the middle and inferior turbinates. Conditions like rhinitis and septal deviation can induce turbinate hypertrophy, obstructing airflow. Turbinate reduction is commonly performed concurrently with septoplasty and septorhinoplasty.
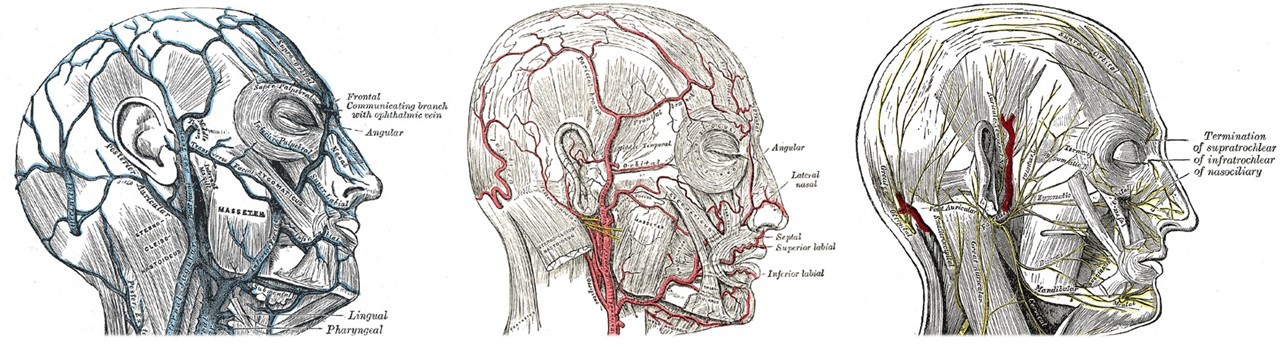
Nasal Blood Supply
The nose has a rich vascular network (see Image. Veins, Arteries, and Nerves of the Face and Scalp), allowing for the broad undermining of the SSTE without compromising tissue perfusion. The main nasal arteries are the supratrochlear and the facial artery, branches of the internal and external carotid, respectively. Both these arteries, together with branches of the ascending columellar arteries, widely anastomose, forming a robust network. Blood is supplied to the nasal septum by the anterior and posterior ethmoid arteries, originating from the ophthalmic artery (a branch of the internal carotid artery), the sphenopalatine artery (a branch of the external carotid artery), and the septal branch of the superior labial artery (a branch of the facial artery). All these branches come together in a network known as the Kiesselbach plexus, the most common site from which epistaxis originates (see Image. Blood Supply of the Nasal Septum). Venous drainage primarily flows through tributaries of the facial vein.
Nasal Innervation
The motor supply to the nose muscles comes via the facial nerve's buccal branch. Sensory innervation is more complicated, with multiple branches of the ophthalmic nerve (cranial nerve [CN] V1), the infratrochlear and external nasal nerves, the maxillary nerve CN V2, and the infraorbital and nasopalatine nerves—contributing to a mosaic of sensory distributions (see Image. Veins, Arteries, and Nerves of the Face and Scalp). The nose also provides special sensation via olfactory nerve filaments that traverse the cribriform plate to innervate the olfactory epithelium, which lines the olfactory cleft at the roof of the nasal cavity and covers portions of the superior septum and the superior turbinates.[18]
Indications
Rhinoplasty is performed for functional problems, aesthetic issues, or, more often, a combination of both. Patients who present with either nasal obstruction or cosmetic concerns often overlook the impact that correcting one issue may have on the other. Without appropriate preoperative counseling and a surgical plan that balances form and function, these patients may not be satisfied postoperatively.[19] This underscores the importance of establishing a strong surgeon-patient rapport.
While much has been written about the difficulty of identifying the ideal candidate for rhinoplasty, there is no proven way to consistently recognize high-risk patients who may be unhappy with the outcome. Therefore, surgeons must physically and psychologically evaluate patients to predict whether an operation will be beneficial. During the initial visit, the priority is to ascertain the patient’s goals and determine if their expectations are achievable, as postoperative patient satisfaction is the primary determinant of surgical success.[20] By asking open-ended questions about the patient's life and context, such as family composition and social relationships, the surgeon can gather verbal and nonverbal cues to understand the patient. As a guide, the acronym SYLVIA (secure, young, listens, verbal, intelligent, attractive) has been used to describe a good rhinoplasty candidate, while SIMON (single, immature, male, overexpectant, narcissistic) represents patients who may be unsuitable for surgery.
Regarding the nose itself, it is important to discuss the specific features patients dislike, such as dorsal humps, nasal deviation, or tip asymmetry, and explain systematically what can be improved and how. Many surgeons use 2- or 3-dimensional computer simulation software to illustrate an approximation of the surgical result.[21] This tool has gained popularity, and in a 2017 survey, 63% of rhinoplasty surgeons reported using it during consultations.[22] While computer simulation can help establish reasonable expectations for some patients, others may fixate on the simulated outcome and find it difficult to be satisfied with anything less. Consequently, a significant number of surgeons have chosen not to adopt computer simulation.
While establishing which patients are good candidates for primary rhinoplasty can be challenging, determining who would benefit from revision rhinoplasty can be even more complex. These patients' expectations are shaped by their previous experiences, which may lead them to have a better understanding of what to anticipate. Conversely, this may cause them to be less reasonable, expecting the new surgeon to fix what they perceive as a "botched" operation by the previous surgeon. The surgical techniques employed in revision surgery may differ significantly from those used in primary rhinoplasty. The second or third operation might be more aggressive than the first, or it could be minimally invasive and aimed at addressing 1 or 2 small deficiencies. These preoperative decisions will inform the surgeon's operative approach: whether to open the nose, operate endonasally, or deliver the nasal tip.
The open approach exposes the entire cartilaginous nasal skeleton and provides excellent access to the bony vault as well (see Image. Open Rhinoplasty Approach). This method can be used for primary and revision rhinoplasty. However, opening the nose a second or third time is far more challenging due to scar tissue and previous manipulation of the cartilage. Tip modification surgery is most easily performed via the open approach because of the enhanced exposure, making it the preferred method in many teaching institutions.[23] The tip is also exposed when a delivery approach is selected, though it requires separating the tip into the left and right domes, which are then distorted as they are delivered into their respective nares (see Image. Tip Delivery Rhinoplasty). Many experienced surgeons employ the tip delivery approach, but it requires substantial skill and is challenging to master.
The endonasal approach allows modification of the upper third of the nose, particularly osteotomies and dorsal hump reduction. Spreader grafts can also be placed endonasally, though many surgeons prefer the open approach to ensure precise placement. Some maneuvers within the lower third are possible endonasally, such as alar batten graft placement, rim graft placement, and cephalic trimming. However, more delicate interdomal and transdomal suturing or nuanced grafting is often performed via an open approach. For some patients, the primary indication for the surgical approach is the anticipated recovery. The endonasal and tip delivery approaches result in decreased severity and duration of postoperative edema compared to the open approach and avoid creating a columellar scar.
Contraindications
Common contraindications for rhinoplasty include:
Psychiatric Disorders
Body dysmorphic disorder is characterized by an excessive preoccupation with an imagined or barely noticeable defect in appearance.[24] As a result, patients with this condition have difficulty socializing, poor quality of life, and higher rates of depression and suicide.[25] Surgeons need to recognize this diagnosis early in the preoperative process because symptoms may worsen postoperatively, and it is doubtful that a patient with body dysmorphic disorder will be satisfied with the results of a rhinoplasty. Unfortunately, no validated instrument can consistently diagnose body dysmorphic disorder. Similarly, patients with poorly controlled depression are at risk for decompensation postoperatively; surgery should be deferred until mood symptoms stabilize.[26] If clinical suspicion of psychiatric disorders arises, referral for preoperative behavioral health evaluation is imperative.
Obstructive Sleep Apnea
This common condition is characterized by repeated airway obstruction episodes and sleep arousal. Patients with obstructive sleep apnea are known to have a higher risk of perioperative complications.[27] The diagnosis is often suspected based on the patient’s symptoms and body habitus, although it can be asymptomatic. Screening questionnaires are available but have limited specificity. Polysomnography is the gold standard for diagnosing obstructive sleep apnea.
Although it is not an absolute contraindication, patients with this condition should be advised of the risks, and preoperative measures like using a continuous positive airway pressure device should be implemented to reduce complication rates. A plan should be in place to admit patients with obstructive sleep apnea for overnight observation after surgery if they are having difficulty maintaining oxygen saturation in the recovery room.
Cocaine Use
Inhaled cocaine induces intense vasoconstriction as well as chronic mucosal inflammation due to contaminating additives.[28] Rhinoscopy findings can vary from mild erythema to large septal perforations. Patients who are actively using cocaine are also more likely to have postoperative complications like septal collapse or impaired mucosal healing, and they should be advised to avoid elective nasal surgery. Patients who have previously used cocaine may be considered for nasal surgery on an individual basis, bearing in mind that healing impairment may persist in the long term.
Tobacco Smoking
Although it appears that tobacco smoking does not significantly affect nasoseptal surgery outcomes, patients should be encouraged to quit before the procedure because of the myriad harmful systemic effects of tobacco.[10][29]
Bleeding Disorders
Impaired coagulation may cause postoperative complications and make the surgery itself more challenging. Patients should be asked about a history of excessive bruising or bleeding, consumption of drugs, supplements, or vitamins that alter the coagulation cascade, or history of thrombotic events in the past. If possible, any drugs, vitamins, or supplements that impair coagulation should be suspended preoperatively.Examples of over-the-counter supplements that may exacerbate bleeding include aloe, chamomile, chondroitin, cranberry, dong quai, echinacea, ephedra, evening primrose, fenugreek, feverfew, flaxseed, garlic, ginger, gingko, ginseng, goldenseal, glucosamine, grapefruit, green tea, kava, meadowsweet, milk thistle, oregano, red clover, saw palmetto, turmeric, and white willow.[30]
Age
Surgery is usually performed when the nasal skeleton has developed completely, and the nasal shape is not expected to change significantly for the foreseeable future. This age is approximately 15 for females and 17 for males.
Recent Prior Rhinoplasty
Generally, patients who underwent previous rhinoplasty and are unhappy with the results should wait at least 1 year before assessing the final result and considering a revision procedure.
Equipment
Equipment required off the surgical field includes:
- Preoperative photographs posted for reference
- Tape or adhesive film dressings to protect the eyes
- Cottonoid pledgets for nasal packing, soaked in decongestant (0.05% oxymetazoline or 4% cocaine)
- Local anesthetic (1% lidocaine with 1:100,000 epinephrine) in 3 cc syringes with 27 gauge, 1.5-inch needles
- Nasal speculum (Vienna)
- Bayonet forceps
- Headlight
Equipment required on the surgical field includes:
- Skin marker
- Sutures (7-0 polyglactin, 6-0 polypropylene, 6-0 plain gut, 5-0 polydioxanone, 5-0 chromic gut, 4-0 chromic gut, 3-0 nylon)
- Double-prong skin hooks (Joseph 2 mm, 7 mm, and 10 mm; Guthrie scleral hooks)
- Scalpels (Bard-Parker #15, #15c, #11; #6700 Beaver; dermatome blade for carving costal cartilage)
- Nasal specula (Vienna, Cottle, Killian)
- Scissors (Converse, Wilmer, Joseph, Giunta, Cottle, Fomon upper and lower lateral, Gorney shears, Mayo, iris)
- Elevators (Cottle, Freer, Pierce, Woodson, Joseph, Sayre, Boies)
- Osteotomes and mallets (Anderson-Neivert, Rubin)
- Cartilage crusher (Cottle)
- Cutting grid (Sheen)
- Caliper (Tebbetts)
- Rasps (coarse and fine diamond, push and pull steel)
- Forceps (Adson-Brown, Cushing-Brown bayonet, dressing bayonet, Castroviejo 0.5 mm, Takahashi, Blakeseley)
- Needle holders (Halsey, Castroviejo)
- Rongeurs (Jansen-Middleton open and closed biting)
- Suction (Frazier tip, 10 Fr)
- Retractors (Aufricht, Bernstein, Gruber)
- Bipolar cautery forceps
- Thrombin-gelfoam hemostatic matrix
- Fibrin glue
- Gauze
- Cotton-tipped applicators
- Piezotome
- Tape dressings
- Splints or packing (Doyle splints or iodine and petrolatum-impregnated gauze)
- Nasal cast (thermoplastic or malleable)
- Saline irrigation and bulb syringe
- Antibiotic ointment (mupirocin or similar; petroleum-based ointments, such as bacitracin, are avoided because of the risk of myospherulosis)
- Long-acting local anesthetic (liposomal bupivacaine)
- Microdebrider for turbinoplasty (2 mm)
Personnel
Rhinoplasty is typically performed by an otolaryngologist, facial plastic surgeon, or a plastic surgeon. Some oral-maxillofacial surgeons are also trained to perform rhinoplasty. While a surgical assistant is not necessary, one may be helpful for retraction, suctioning, and suture cutting. A surgical technician or scrub nurse is, however, essential. A rhinoplasty will also need a circulating nurse and an anesthesia provider if performed under general anesthesia. These procedures are typically performed in an ambulatory setting unless social circumstances preclude this option, so an escort to drive the patient home is mandatory.
Preparation
Preoperative
The initial preparation for rhinoplasty consists of appropriate counseling and an examination. Eliciting a history of prior nasal surgery and the patient's experience with both it and the previous surgeon can be informative for the sake of operative planning and for establishing reasonable expectations for the patient and the new surgeon alike. Any psychiatric comorbidities, such as a tendency towards depression or body dysmorphic disorder, should be recognized at this time so that either appropriate treatment planning (to include behavioral health referral) can be initiated or surgery can be deferred. Other medical problems, including obstructive sleep apnea, recurrent or chronic sinusitis, hypertension, and bleeding diatheses should be discussed, as they may necessitate additional surgical interventions or medical management. Recreational drug use may have an impact on the selection of anesthetic agents and analgesic medications, but cocaine use in particular may require cancellation or delay of surgery due to the adverse effects it has on the vascularity of the nasal mucosa.
As part of the examination, high-quality preoperative photographs should be taken with the patient's face aligned in the Frankfort horizontal plane (a line running between the inferior orbital rim and the top of the external auditory canal should be parallel to the floor), including the following views: frontal, bilateral profiles, bilateral three-quarter view, basal view, and dorsal view (see Image. Standard Photographs for Rhinoplasty). These will provide points of reference for counseling and intraoperative decision-making and may be used for medicolegal purposes as well. Counseling will depend largely on the goals of the patient, balancing aesthetic and functional expectations, particularly in the case of reduction rhinoplasty in women. The greatest risk of any facial surgery is dissatisfaction with the cosmetic outcome either immediately or in the future, but other risks include pain, bleeding, bruising, swelling, infection, scarring, damage to the SSTE, nasal obstruction, change or decrease in sense of smell, septal perforation, numbness or sensitivity in the distribution of the nasopalatine nerve, cerebrospinal fluid leak, postoperative depression, and need for further surgery.[9] Patients undergoing revision surgery, and those who require post-traumatic or oncologic reconstruction, should also consent to the harvest of tissue at extranasal sites, including conchal cartilage, costal cartilage, and temporoparietal or temporalis fascia; the risks of these graft harvests should be discussed as well.
Nasal analysis and Exeamination
The external nose is divided into 9 aesthetic subunits (dorsum, 2 sidewalls, tip, 2 alae, columella, 2 soft tissue triangles; see Image. External Nasal Anatomy), which are most relevant to oncologic reconstruction; for the purposes of rhinoplasty, the nose is more often divided into upper, middle and lower thirds, as described above. The upper third begins at the nasofrontal suture superiorly and widens as it approaches the middle third. The middle third also widens inferiorly where it merges with the lower third at the scroll. The lower third is the broadest portion of the nose, with the alar base equal in width to the intercanthal distance in Caucasian individuals or as wide as the intercaruncular distance in individuals of Sub-Saharan African descent.[31]
The most superior extent of the nose is the nasofrontal suture, whose midline point is known as the nasion. The nasion is the deepest portion of the region known as the radix, or root of the nose. The depth of the radix is determined by the position of the nasofrontal suture relative to the prominence of the glabella and of the rhinion and therefore plays an important role in the perception of a nose's dorsal projection, particularly if there is a hump. For example, a nose with a deep radix and prominent dorsum will be seen to have a hump (a "Roman" nose), whereas a nose with an equally prominent dorsum and a shallow radix, in which the nose seems to join directly with the forehead, will not be perceived as having a hump at all (a "Greek" nose; see Image. Roman and Greek Noses). In this way, the nose can be viewed through a Taoist lens; just as there can be no perception of light without darkness to which it can be compared, or heat without cold, the radix defines the hump and vice versa. Ideally, the nasofrontal angle, which is centered at the radix, should measure approximately 115º to 130º in a Caucasian individual, but less in Asian, Latin, and African individuals.
The differences stem from variations in overall proportions by race; Caucasian noses tend to have a leptorrhine configuration (relatively slim and highly projected with a robust osteocartilaginous framework) while Sub-Saharan African noses are typically platyrrhine in appearance (flatter and wider with smaller nasal bones and less septal cartilage) and Asian, Middle Eastern and Latin noses lie somewhere on a spectrum between the 2 extremes (mesorrhine).[32][33] Admittedly, specific ethnic nasal features are far more nuanced than the simple framework the 3 categories suggest; however, this classification scheme does provide a foundation upon which rhinoplasty surgeons can communicate and refine techniques.
As the examination progresses down the nose, the symmetry, particularly with respect to deviations from the midline, should be assessed. A nose whose upper, middle, and lower thirds all point in the same direction away from the midline is known as a "deviated" nose, whereas a nose with a C-shaped curvature, commonly resulting from a blow to the side of the nose, is referred to as "crooked" or "twisted." The symmetry of the face should be evaluated as well because hemifacial microsomia is common and can have a major impact on both the appearance of the nose and the extent to which deviations can be straightened. Contour irregularities at the rhinion, such as small projections or "horns" may be best appreciated in the profile or three-quarter views, or even by palpation. Stigmata of prior surgery should be identified, such as an open roof deformity, in which a dorsal hump with a large bony component was removed and the cut medial edges of the nasal bones are palpable or visible due to a midline gap in the bony vault.
Other common sequelae of rhinoplasty include saddling of the midvault due to inadequate support of the dorsal septum and the "inverted V" deformity, in which the caudal edges of the nasal bones are sharply visible due to descent of the upper lateral cartilages into the nose. The latter typically occurs as a result of an endonasal dorsal hump reduction that disarticulates the upper lateral cartilages from the dorsal septum but does not resuspend them to reconstruct the midvault. Failure to reduce the cartilaginous portion of a dorsal hump adequately relative to the bony portion (or over-resection of the bony portion relative to the cartilaginous portion) may cause a "polly beak" deformity, in which the supratip portion of the middle third appears rounded and over-projected, conveying the appearance of a parrot's bill. Tip ptosis and development of scar tissue in the supratip region can further exacerbate this deformity, which must not be confused with a true dorsal hump, as they are managed differently.
Evaluation of the middle third should also include assessment of the internal nasal valves with a modified Cottle maneuver, in which the patient is asked to inhale through the nose with and without a small instrument (cerumen loop or the back end of a cotton-tipped applicator, for example) supporting, but not lateralizing, the upper lateral cartilage. Substantial subjective airflow improvement with support indicates that opening the internal nasal valve during surgery may be beneficial. A similar maneuver may be performed at the external nasal valve; alternatively, some surgeons prefer to look for the dynamic collapse of the alae with inspiration as an indicator of external nasal valve insufficiency. If the patient demonstrates symptomatic dynamic alar collapse, marking the points of maximum collapse preoperatively will enable the surgeon to reinforce the external nasal valves accordingly.
The lower third is the most complicated aspect of the nose to manage due to the complicated relationships among its aesthetic subunits, its respiratory function, and its ethnic variations (see Image. Nasal Analysis). The ideal projection of the nasal tip out of the facial plane may be measured against the standards described by Simons, Goode, and Crumley (Simons: tip projection should equal the height of the cutaneous upper lip, Goode: tip projection to nasal length ratio should be 0.55-0.6:1, Crumley: tip projection, nasal height, and nasal length should constitute a 3:4:5 Pythagorean triangle), although these proportions really only hold true for leptorrhine noses, while mesorrhine and platyrrhine patients will have somewhat lesser projection.[34]
Similar to the dorsal projection, however, the perceived projection of the nasal tip is influenced by the context of the face as a whole, particularly the projection of the chin. If the anteriormost point of the chin, the pogonion, sits behind the nasion when the face is aligned in the Frankfort horizontal plane, the nasal tip will appear more projected, but if the chin is more prominent, the nasal tip will seem less projected. The nasolabial angle in a leptorrhine nose is classically described as 95º to 110º in women (with greater rotation acceptable for shorter women) and 90º to 95º for men, but somewhat less for those with mesorrhine and platyrrhine noses, particularly for Middle Eastern individuals, who may have rather acute nasolabial angles.
When viewed from the side, the length of the nasal tip lobule should equal the width of the ala. When viewed from beneath, the base of the nose should present a generally triangular shape (vs trapezoidal) and the length of the infratip lobule should measure half the length of the columella. The columella, when viewed from the side, should present 2 to 4 mm of height visible below the alar margin. Less columellar show indicates retraction of the caudal septum, likely due to trauma or prior surgery, and more columellar show signifies either a retracted nasal ala or a hanging columella. The width of the base of the nose should be assessed as well, both the alar base width and the alar flare. The alar base width is the distance from the point at which the ala meets the face at the alar crease on the right side to the same point on the left. This distance should equal the intercanthal distance in a leptorrhine nose.
Alar flare, if present, is the distance beyond the alar base width that the lateral extent of the ala reaches due to its convexity; this is commonly seen in platyrrhine noses. Last, the lower lateral cartilages themselves should be assessed in terms of shape and strength. Gentle palpation of the tip of the nose will provide an idea of how strong the cartilages are and how much support there is for the nasal tip. Broad lateral crura of the lower lateral cartilages will cause excessive supratip fullness, while lateral crura that have been excessively narrowed during prior surgery will often produce alar retraction and/or upward tip rotation. Asymmetries in the lower lateral cartilages, such as lateral crural recurvature that narrows the external nasal valve and bossae that disturb the smooth contour and symmetry of the nasal tip, may also result from prior surgery or trauma, or may be congenital; these asymmetries should all be identified preoperatively.
The final portion of the physical examination involves anterior rhinoscopy, which may be supplemented with fiberoptic or rigid nasendoscopy if findings on anterior rhinoscopy do not identify the anatomic etiologies of the patient's functional complaints. The nasal septum should be assessed for deviations, as they can cause symptomatic nasal obstruction. Even for patients without nasal dyspnea, the septum should be visualized to determine the availability of straight cartilage for grafting. For patients who have had prior nasoseptal surgery, the septum should be examined for any perforations, and palpation of the septum with a cotton-tipped applicator will reveal how much cartilage remains to be harvested for grafting.
The vestibules should be inspected without the use of a speculum, which will distort them and make identification of subtle abnormalities like lateral crural recurvature challenging. The turbinates and swell bodies should be assessed as well, the former before and after application of a topical decongestant, to determine whether the reduction would improve nasal airflow. Patients who have previously undergone turbinate reduction and have patent nasal passages on examination but still report nasal obstruction are likely suffering from empty nose syndrome and should not undergo additional surgery to widen the nasal airway, but may benefit from augmentation of inferior turbinate volume instead.[35]
Day of Surgery
In the operating room, general anesthesia is induced, and orotracheal intubation proceeds, with the tube being taped to the midline of the lower lip to keep it out of the way and prevent it from distorting the lower third of the nose. Many surgeons and anesthesia clinicians prefer to employ a total intravenous anesthetic protocol, using propofol and remifentanil, which provide permissive hypotension to decrease bleeding and reduce coughing, agitation, and nausea on emergence.[36][37] Tranexamic acid (1 to 2 g) may be administered at the beginning, and optionally at the end of the procedure as well, to decrease intraoperative bleeding and postoperative ecchymosis and edema. Dexamethasone or another intravenous corticosteroid will help to decrease edema and postoperative nausea.[38][39][40][41] Whether or not to provide prophylactic antibiosis at the beginning of the case is a matter of some controversy, depending on whether the operation is primary or revision, and if extensive grafting is anticipated; there is a clearer consensus that postoperative antibiotics are not necessary.[42][43]
Placing the patient supine, with arms tucked tightly to the sides and the head of the bed elevated slightly will improve the surgeon's access to the nose and further decrease intraoperative bleeding. An orogastric tube may be placed at the beginning of the case and left off suction so that it can be used at the end of the operation to evacuate the stomach contents without having to be placed immediately before emergence, as the passage of the tube may be quite stimulating and contribute to a rough arousal from anesthesia. Before the injection of local anesthetic, the patient's eyes are closed and protected with tape or adhesive film dressings.
Twelve to 15 mL of local anesthetic are injected into the septum, inferior turbinates, nasal dorsum, sidewalls, tip, columella, and along the caudal margins of the lateral crura of the lower lateral cartilages. The medication is allowed to sit for 15 minutes for the vasoconstrictive effect to develop while the patient's face is prepped. After injection, 2 to 3 cottonoid pledgets soaked in a decongestant are placed into each nasal cavity. Male patients may require trimming of the vibrissae to facilitate the visualization needed for injection, and patients with large inferior turbinates may benefit from a decongestant spray in the holding area before arrival in the operating room.
Surgical skin preparation can be accomplished with povidone-iodine, chlorhexidine, or isopropyl alcohol, the latter of which will not obscure the subtleties of skin color and texture. The entire midface from upper lip to forehead should be exposed in the surgical field, as well as both ears, to provide access to conchal cartilage, if necessary. Revision cases may require access to the chest for costal cartilage harvest or the scalp for split calvarial bone harvest. Last, it is important to post the preoperative photographs in the operating room for reference during the case.
Technique or Treatment
Every surgeon may take a different approach to working through a rhinoplasty, and the description that follows is just 1 method. Herein, an "in-to-out and top-to-bottom" workflow is detailed. At the end of this section, see Table. Location, Deformity, and Maneuvers to Consider in Rhinoplasty, which provides a quick reference for the selection of surgical techniques to correct various nasal deformities that may be encountered.
If indicated, the turbinoplasty and reduction of the septal swell body are performed before the rhinoplasty for 2 reasons: 1) bleeding caused by the turbinoplasty will have a chance to resolve during the remainder of the operation rather than continuing through emergence and alarming both the patient and the recovery nurses, and 2) the force required to outfracture the inferior turbinates will be applied before any delicate work is performed in the rest of the nose, rather than afterward, thereby decreasing the risk of disrupting the surgical result. If the nasal septum is so deviated that it denies access to one or both of the inferior turbinates, the turbinoplasty may be deferred until after the septoplasty is complete, but the turbinoplasty should ideally not be delayed until the end of the case. Some surgeons prefer to perform the septoplasty before the rhinoplasty, electing to use a hemitransfixion incision for the septoplasty and then to approach the rhinoplasty afterward. In the workflow below, the septoplasty will be performed after the nose has been opened (if an open approach is employed) to obviate the need for the hemitransfixion incision and improve the exposure of the septum.
Modification of the septum and the dorsal hump is undertaken in the same stage of the surgery, although the order in which they are addressed will vary depending on the technique selected for reduction of the dorsal hump. Resection or rasping should be performed before the septoplasty so that the surgeon can ensure 10 to 15 mm of dorsal septal height remain after cartilage harvest/resection of deviated septal cartilage, as resecting a dorsal hump after septoplasty can result in an overly thin and weak dorsal septal strut. On the other hand, if a dorsal preservation technique is chosen, septoplasty is performed first, including resection of the septal strip that will allow the dorsum to be lowered by a push-down or a let-down maneuver. As a caveat, during revision surgery, the order of the operation may need to diverge from that described below, depending on how scar tissue affects the path of dissection and where grafting materials may have been placed previously.
Incisions and Exposure
For a discussion of the indications for selecting an approach to rhinoplasty, please see the Indications section above.
Open approach: The transcolumellar incision is marked using a stair-step or chevron shape ("inverted-V") to break up the contour of the scar and direct the contractile forces obliquely across the columella to minimize the chance of notching (see Image. Rhinoplasty Incisions). If a chevron-shaped incision is used, the chevron should be at least 3 mm in width at its base to prevent it from flattening during healing and the base should be level with the narrowest portion of the columella, which is where the skin is thinnest and least likely to produce a prominent scar. The incision itself is made with a fine blade, such as a Bard-Parker #11 or #15c, or a #6700 beaver blade, taking care to avoid damaging the underlying medial crura of the lower lateral cartilages. A columellar flap is then elevated up to the domes of the lower lateral cartilages using fine scissors (Wilmer, Converse, iris, etc.). The columellar vessels and intercrural soft tissues are isolated and divided with bipolar electrocautery, thereby exposing the medial surfaces of the medial crura. With a combination of 1 wide and 2 narrow double-pronged skin hooks, the dome of the lower lateral cartilage is flattened and held under tension while the marginal incision is made, continuing laterally from the transcolumellar incision (see Image. Open Rhinoplasty Approach). Fine scissors or a scalpel can be used for this incision. The contralateral marginal incision is then made identically. Two wide double-pronged skin hooks are then placed, one pulling upward under the SSTE and one retracting downward under the domes, so that the soft tissue can be cleared from the superficial surface of the lower and upper lateral cartilages, taking care to leave the perichondrium intact. Either scissors or cotton-tipped applicators can be used for this elevation. With the lower two-thirds of the nasal skeleton exposed, an elevator (Joseph, Cottle, or similar) is used to dissect the periosteum from the nasal bones and the frontal processes of the maxillae, thus completing the open approach.
Endonasal approach: Access is usually obtained via an intercartilaginous incision, made through the scroll region, between the cephalic border of the lateral crus of the lower lateral cartilage and the caudal border of the upper lateral cartilage (see Image. Rhinoplasty Incisions). A wide double-pronged skin hook is used to evert the nasal ala and apply downward tension to the SSTE to facilitate making the incision with a #15 blade. Scissors (eg, Joseph, Giunta, or similar) are then used to dissect blindly along the superficial surface of the upper lateral cartilages and onto the nasal bones. The perichondrium is left intact, but an elevator (eg, Joseph, Cottle, or similar) is used to dissect the periosteum from the nasal bones, and the frontal processes of the maxillae, thus completing the endonasal approach.
If a septoplasty is required, a hemitransfixion incision may be used, and it may be joined to the ipsilateral intercartilaginous incision for greater exposure. If cephalic trimming is planned, intracartilaginous incisions may be added to permit excision of the cephalic margins of the lateral crura of the lower lateral cartilages as well as their underlying vestibular skin (see Image. Rhinoplasty Incisions). Because the inter- and intracartilaginous incisions are located posterior to the tip of the nose, accessing the domes and medial crura of the lower lateral cartilages is challenging via the endonasal approach. If an open approach is not feasible, the tip is best accessed via a delivery approach, which is essentially a modification of the endonasal approach.
Tip-delivery approach: After the endonasal approach is complete, visualization of the lower lateral cartilages may be achieved by delivering the domes into the nasal vestibules via additional incisions. A full-thickness transfixion incision or bilateral hemitransfixion incisions are made in continuity with the medial ends of the intercartilaginous incisions. Then, marginal incisions, without a transcolumellar incision, are made parallel and anterior to the hemitransfixion and intercartilaginous incisions using a scalpel and wide double-pronged skin hook, thereby creating bipedicled (medial and lateral) chondrocutaneous flaps that contain the lower lateral cartilages. After the division of the interdomal ligaments with fine scissors, the domes can be retracted laterally into the nares (see Image. Tip-Delivery Rhinoplasty).
Septoplasty
This procedure is performed for relieving a nasal obstruction, harvesting cartilage for grafting, or correcting a dorsal or caudal nasal deviation. Septoplasty is typically performed early in the rhinoplasty. If the nose is opened, the anterior septal angle of the quadrangular cartilage is easily identified by palpation after the interdomal ligaments have been divided and the lower lateral cartilages retracted away from the midline. If the nose is not opened, a hemitransfixion incision can be used; it is placed along the side of the caudal margin of the septum, just behind the medial crus of the lower lateral cartilage. Either side can be used, with right-handed surgeons typically preferring a left-sided incision for ergonomic reasons, but bilateral septal flaps can be elevated via a single hemitransfixion incision.
Once the septal cartilage is visualized, fine scissors are used to snip down to the level of the perichondrium, which is then gently cross-hatched with a #15 blade scalpel to expose the bare cartilage. An elevator, such as a Woodson or a Cottle, can then be used to develop a plane between the cartilage and the perichondrium. Elevation in this plane then continues superiorly onto the perpendicular plate of the ethmoid bone, posteriorly onto the vomer, and inferiorly over the maxillary crest and onto the nasal floor (see Image. Internal Nasal Anatomy). Passing from the quadrangular cartilage onto these bony structures necessitates a transition to a subperiosteal plane, which is not typically challenging except for along the maxillary crest. Maintaining the dissection within the correct plane is important for 2 reasons: the plane is avascular and therefore likely to result in less bleeding, and keeping the perichondrium or periosteum attached to the mucosa makes the flap stronger and therefore more resistant to tears and subsequent septal perforation.
If the septoplasty is performed via an open rhinoplasty approach, disarticulating the upper lateral cartilages from the dorsal septum early in the process will substantially improve visualization and make room for later spreader graft placement. Once the septal flaps are elevated bilaterally, the deviated bone and cartilage are resected, or straight cartilage is harvested as necessary. The cartilage is often incised with a Freer septal knife, a #15 blade, or a Ballenger swivel knife, while bony cuts are typically made with Gorney double-action nasal shears, Jansen-Middleton rongeurs, and osteotomes (see Image. Septal Cartilage Harvest). It is critical to leave at least 10 to 15 mm of cartilage intact along the dorsal and caudal aspects of the septum (the "L-strut") to provide enough support to the nose to prevent a postoperative saddle deformity. Critical to this is maintaining the integrity of the bony-cartilaginous junction at the keystone, although the bony-cartilaginous junction at the anterior nasal spine is also important for tip support. If the L-strut itself is deviated, grafting techniques may be required to straighten it, and these are often more easily employed via an open rhinoplasty approach. For a more in-depth discussion of septoplasty, please see the following article: Septoplasty.
Dorsal Hump Reduction
Resection: Reduction of a dorsal hump by resection can be accomplished using a rasp, an osteotome, a piezotome, a scalpel, and/or dorsal scissors, depending on the size of the hump, its location, and the surgeon's instrument preference. Given that most dorsal humps are roughly centered over the rhinion and therefore have both cartilaginous and bony components, some combination of sharp excision of cartilage and rasping or osteotomy of the bone is usually required. The cartilage is most frequently addressed with a scalpel, such as a #11 blade, which is used to cut the anterior septal angle to the rhinion, removing a wedge of cartilage that is thickest superiorly; the thickness at this point corresponds to the desired amount of dorsal hump reduction.
Resecting cartilage to the anterior septal angle leaves a smooth dorsum, whereas a shorter resection may contribute to a polly beak deformity. While it is better to remove too little cartilage and then, if necessary, return to resect more, than it is to take too much at the beginning, it is preferable to remove the correct amount initially so that the cartilage has the greatest potential use as a graft, which is difficult to do if the cartilage is shaved in multiple iterations. Cartilage resection may precede disarticulation of the upper lateral cartilages from the dorsal septum (en bloc resection) or it may come after (dorsal strip resection) if the plan involves autospreader flaps to open the internal nasal valve, which are best employed when there is a relative excess of upper lateral cartilage height compared to the dorsal septum (see Image. Dorsal Hump Reduction).
Reduction of humps with small bony components can then be completed with a rasp or piezotome, while larger humps may require resection of the bony component with an osteotome. If an osteotome is used, or even if aggressive rasping is performed, an open roof is likely to result, and this will need to be closed with lateral osteotomies to prevent an open roof deformity of the upper vault. While the goal of dorsal hump reduction is often to create a flat nasal dorsum, it is important to maintain a subtle dorsal hump of the nasal skeleton itself because the SSTE is thinnest over the rhinion and a truly flat nasal dorsal skeleton may cause a pseudo-saddle deformity once the SSTE is redraped over it.
Dorsal preservation: Cottle is credited with describing hump reduction with a dorsal preservation technique, a technique that permits lowering of the nasal dorsum without disarticulating the upper lateral cartilages from the quadrangular cartilage or causing an open roof deformity; in essence, leaving the upper and middle vaults of the nose intact. There are 2 primary dorsal preservation techniques: "push-down" and "let-down." Both of these involve removing a strip of septal cartilage and bone below the dorsum that corresponds in height to the desired degree of dorsal deprojection. This can be accomplished via a hemitransfixion incision or an open rhinoplasty approach, bearing in mind that the upper lateral cartilage should not be disarticulated from the quadrangular cartilage before beginning the septoplasty.
Lateral and transverse osteotomies are then made, which mobilize the bony vault and allow the dorsum to be "pushed down" into its desired position. For larger humps, bilateral intermediate osteotomies made medial to the lateral osteotomies allow resection of slim wedges of bone that then permit even greater descent of the dorsum (see Image. Dorsal Hump Reduction). The osteotomies used for dorsal preservation techniques must be made very precisely, and many surgeons prefer to use a piezotome for this reason. The piezotome, however, is rather bulky and requires substantially more elevation of the maxillary periosteum for access, which may contribute to more postoperative edema than is seen after the use of osteotomes.
Modification of the Bony Vault
Narrowing the bony vault: For adjusting the width of the upper third of the nose, medial and lateral osteotomies are typically performed bilaterally, with the lateral osteotomies taking a high-low-high configuration (see Image. Nasal Osteotomies for Adjusting the Width of the Bony Vault). Most of the lateral osteotomy (the "low" portion) is placed in the nasofacial junction to avoid a visible or palpable step-off. The superior extent of the lateral osteotomy is the nasofrontal suture, to prevent a rocker deformity. The inferior extent is angled to leave a "Webster's triangle" of bone intact at the piriform rim, which keeps lateral alar ligamentous attachments intact for support of the external nasal valve.[44]
As with dorsal preservation techniques, a piezotome may be substituted for the osteotomes. The medial osteotomies are usually made either through intercartilaginous incisions (via an endonasal approach) or via an open rhinoplasty approach. Curved, guarded Anderson-Neivert osteotomes are used most commonly for medial osteotomies, engaging the nasal bones in a paramedian position, between the upper lateral cartilage and dorsal septum, at the edge of the nasal bone. The osteotomy is made continuously, starting superiorly but then rapidly beginning to fade laterally, where it will come close to, but not meet, the superior aspect of the lateral osteotomy.
The reason the medial and lateral osteotomies are kept separate is that a greenstick fracture can then be produced between the 2 osteotomies, which will allow the intervening bone segment to move but still provide it some stability. The nasal bones are comparatively thin and do not require much force to cut, in contrast to the frontal processes of the maxillae, which do require substantial effort to complete the lateral osteotomies. Lateral osteotomies may be made either percutaneously in a "postage stamp" perforation fashion with a small (2-3 mm) straight osteotome, or they may be made via small incisions across the mucosa at the piriform rim, at the level of the junction of the inferior turbinate and the lateral nasal wall. The latter technique usually employs an Anderson-Neivert osteotome after the periosteum has been elevated.
When using Anderson-Neivert osteotomes, it is important to remember that the side-mounted guard will be palpable under the SSTE several millimeters ahead of the cutting edge of the instrument, and this should be taken into account when assessing the progress of the osteotomy. The use of percutaneous postage-stamp osteotomies tends to leave the bony segments more stable than continuous intranasal osteotomies because of the jagged edge of the osteotomy; however, that may also make moving the osteotomized bone segments more challenging. Bones tend to be easier to mobilize after continuous osteotomies, even with some periosteum preserved for stability.
Percutaneous osteotomies have the further disadvantage that the percutaneous entry points may produce visible, albeit small, scars in some patients, particularly those with darker skin. If there are any rough contours after the osteotomies, rasping may be performed to smooth the bone, but rasping mobile bony segments is challenging. Ideally, all rasping should be complete before beginning the osteotomies. If an overly mobile "flail" segment of bone is encountered after the osteotomies are complete, packing the nasal cavity with iodine-impregnated gauze or placing transnasal k-wires will usually provide enough support to keep the bone in the desired position during the early healing process.
Straightening the bony vault: For noses with a deviation in the upper third area, bilateral lateral osteotomies and a transverse nasal root osteotomy will mobilize the bony vault as a unit and permit it to be reoriented. In these cases, the lateral osteotomies typically take a high-to-low configuration and are connected directly with the root osteotomy at the level of the nasofrontal suture to facilitate movement, rather than making a deliberate greenstick fracture (see Image. Nasal Osteotomies for Shifting a Deviated Bony Vault). The root osteotomy is most easily accomplished percutaneously with a 2 to 3-mm straight osteotome placed through a horizontal stab incision at the nasion because it is made very high on the nose.
For severely deviated bony vaults (≥3 mm deflection of the rhinion lateral to the facial midline), an intermediate osteotomy is often required on the side contralateral to the direction of deviation. The intermediate osteotomy produces a slim wedge of bone that telescopes down into the nose and opens a gap into which the bony vault can shift on its way back to midline, similar to the osteotomies used in the let-down dorsal preservation technique. To avoid unintended fractures of the bony pyramid, the use of a Sayre or Boies elevator to raise and shift the vault gently is more effective than attempting to move it with laterally-directed force applied with the surgeon's thumbs. Occasionally, despite mobilizing the bony vault on the left, right, and top, it remains unable to move freely; in these cases, a dorsal septotomy (typically using a pair of scissors to cut the perpendicular plate of the ethmoid) may be required to complete mobilization.
Special situations: When the bony vault is deviated as well as being excessively wide, 2 options exist for planning the osteotomies: 1) medial osteotomies can be added to the lateral, root, and intermediate osteotomies to narrow the vault while repositioning it, or 2) unilateral medial and lateral osteotomies can be made on the side towards which the upper vault has deviated so that that side of the bony vault can be shifted towards the midline, thus straightening and narrowing the upper third. The first option adds to the complexity of the osteotomies and increases the risk that a flail segment or misdirected osteotomy will occur. The second option is only applicable if the nasal bones are not severely deviated, as unilateral medialization in those cases will result in excessive narrowing of the upper third of the nose.
If there is a dorsal hump and a deviated upper vault, a dorsal preservation technique can be used with unilateral let-down osteotomies on the side opposite the direction of deviation. This requires the finesse and precision necessary to employ dorsal preservation techniques but is very reliable when performed correctly. Alternatively, the hump can be resected as described above and the open roof closed asymmetrically to correct the deviation. For noses with complex contours in the upper vault, frequently due to blunt facial trauma or, rarely, multiple prior rhinoplasties, osteotomies through the prior fractures may be the best option to restore a normal shape to the nose; this is a technically challenging procedure that may be more effectively accomplished using computed tomography guidance.[45]
Management of the Midvault
Supporting the internal nasal valve: Patients with congenitally narrow internal valves or acquired narrowing due to trauma or prior rhinoplasty will benefit from spreader grafting, which will open the internal valve angle and correct contour abnormalities, such as an inverted V deformity. While spreader grafting is frequently performed bilaterally, if the valve dysfunction is unilateral or there is a visible concavity on only 1 side of the midvault, only 1 graft may be needed. On the other hand, for patients with a desire to maintain a narrow dorsum for aesthetic reasons, placement of spreader grafts should be considered very carefully, as they can widen the midvault visibly if the SSTE is not thick. The spreader grafts described by Sheen in 1984, also known as "vertical" spreader grafts, were originally placed endonasally into tight tunnels created between the perichondrium and the quadrangular cartilage, just beneath the junction of the upper lateral cartilages and the dorsal septum.[6]
This maneuver had the effect of eliminating the inverted-V appearance while improving nasal airflow. Using this technique, the tunnels must be placed very precisely to ensure that the grafts do not migrate away from the desired location; mattress sutures across the septum using a 4-0 chromic gut may be passed underneath the grafts to help maintain their positioning. Vertical spreader grafts are also commonly placed via open rhinoplasty, which permits better visualization and verification of correct graft placement. The grafts are ideally made from straight segments of harvested septal cartilage, measuring 1 to 2 mm in width, 3 to 4 mm in height, and having a length just longer than the length of the medial margin of the upper lateral cartilage, so that the graft can run the length of the entire junction between the upper lateral cartilage and the septum and underlap the nasal bones slightly (typically 17-20 mm in total).
Vertical spreader graft placement via an open rhinoplasty approach is typically performed in 1 of 2 ways. After disarticulation of the upper lateral cartilage from the quadrangular cartilage, either 1) the graft itself is placed directly between the medial edge of the upper lateral cartilage and the dorsal septum, or 2) the graft is placed just below the junction to wedge the upper lateral cartilage outwards without widening the dorsum as much as option 1, but potentially providing less width to the internal valve as well (see Image. Spreader Grafting). Either permanent 5-0 or 6-0 polypropylene or resorbable 5-0 polydioxanone suture can be used to fixate the grafts and resuspend the upper lateral cartilages, bearing in mind that if permanent sutures are used, it is best to avoid leaving the knot on the dorsum, where it will be most palpable.
If appropriate septal cartilage is unavailable to fashion the spreader grafts, suitable cartilage may be harvested from the auricle or the rib. Auricular cartilage is brittle and flimsy, however, and costal cartilage is prone to warping unless cut obliquely (see Image. Costal Cartilage Grafting).[46] To reduce the chance of a costal cartilage graft warping after placement in the nose, carving the graft and then letting it rest in normal saline for at least 15 minutes should indicate whether or not it will remain straight. Costal cartilage has a concentric lamellar structure, and the inclusion of as many of these layers as possible in the graft will reduce the chance of warping. Costal cartilage may be harvested from the patient or obtained as an irradiated or fresh frozen cadaveric graft. Proponents of both options are outspoken, with critics of cadaveric cartilage use arguing that it is more likely to resorb, while its supporters disagree and point out the risk of pneumothorax and increased pain associated with autologous costal cartilage harvest.[47][48][49]
Alternatively, autospreader flaps may be used instead of vertical spreader grafts if there is an excess of upper lateral cartilage width relative to septal height, as occurs after the reduction of a dorsal hump using a dorsal strip resection. To use autospreader flaps, the mucoperichondrium is first elevated laterally away from the medial margin of the upper lateral cartilages to prevent mucosa from becoming trapped. The upper lateral cartilage is then scored gently on its superficial surface, 2 to 3 mm lateral and parallel to its medial margin to facilitate folding the medial margin inwards. Once the medial margin of the upper lateral cartilage is folded inwards, the cartilage can be sutured to the dorsal septum as described for spreader grafts, thus flaring the upper lateral cartilage laterally and opening the internal nasal valve (see Image. Autospreader Flaps).
Using a dorsal preservation technique for hump reduction will have a similar effect, as the descent of the dorsum will force the upper lateral cartilages outwards. For severely narrowed middle vaults, the horizontal spreader graft, or "butterfly" graft, is also an option. This graft is made from a slightly curved, or even flat, piece of cartilage that is shaped like an oval or a rounded hourglass and placed across the lower midvault, then sutured to the upper lateral cartilages so that it pulls them outward and aggressively opens the internal valve. This graft is often visible beneath the SSTE, and therefore should only be used after appropriate counseling and only for patients for whom nasal breathing is the uncontested top priority.
On the other hand, for mild internal nasal valve collapse, "flaring" sutures may be used instead of grafting. These are horizontal mattress sutures placed from one upper lateral cartilage across the dorsum and into the other, with the suture passing through the upper lateral cartilages running on the deep surface of the cartilage (but not through the mucosa) and parallel to the nasal septum, 2 to 4 mm lateral to the midline. The farther from the midline the sutures are placed, the more flaring of the upper lateral cartilages will occur, opening the internal nasal valves without substantially widening the dorsum. Permanent sutures, such as 5-0 polypropylene, are usually used for this maneuver.
Addressing lateral deviation and contour asymmetry: In the case of the C-shaped nose, or for patients with unilateral midvault narrowing, a unilateral spreader graft on the concave side may be placed. Alternatively, if there is bilateral internal nasal valve obstruction, bilateral spreader grafts can be used, with the graft on the concave side being thicker. Spreader grafts, when made slightly taller (5-6 mm in height) can also be used as septal batten grafts to help straighten the dorsal septal L-strut, which is particularly useful for straightening C-shaped noses. In these cases, if the dorsal septal deviation extends to the anterior septal angle, beyond the caudal margin of the upper lateral cartilage, the spreader graft can be made longer: an "extended" spreader graft.
The caveat to this is that widening the anterior septal angle will result in widening of the supratip area, which is often aesthetically unappealing. For noses that are deviated to one side, rather than having a C-shaped curvature, "clocking" sutures are an effective option to straighten the midvault, with or without spreader graft placement. Clocking sutures are obliquely oriented horizontal mattress sutures used to resuspend the disarticulated upper lateral cartilages to the dorsal septum (and to secure the spreader grafts, if present). They are angled such that the pass through the upper lateral cartilage on the side towards which the nose is deviated is made more caudally than the contralateral pass.
When the suture is tightened, it will cause the upper lateral cartilages and spreader grafts to slide relative to one another and shift the midvault back towards the midline. Overtightening of these sutures will leave a palpable divot in the upper lateral cartilage; however, it is better to place several looser sutures than a single tight one. Unlike flaring sutures, clocking horizontal mattress sutures are thrown so that the deep passes are through the septum, rather than under the upper lateral cartilages.
Correcting a saddle deformity: Mild saddle deformities with predominantly aesthetic effects and negligible resultant nasal obstruction may be corrected with onlay grafting, which is both easy and effective. Crushed septal cartilage is a popular choice, and this can either be inserted into a tight pocket under the SSTE (in endonasal rhinoplasty), or secured with sutures or fibrin glue (in open rhinoplasty). If septal cartilage is not available, auricular or costal cartilage may be used, although they do not crush well and typically need to be diced. Because dicing does not produce as fine a particle as crushing, placement of a fascial graft (temporalis or temporoparietal) under the SSTE will help prevent palpable or visible diced cartilage contours. More severe saddle deformities will affect the nasal airway by causing collapse of the internal nasal valves; these cases require more aggressive treatment.
One option is to rebuild the septum from the bottom up by performing extracorporeal septal reconstruction. This entails using either the available septal cartilage or costal cartilage to fashion an L-strut using 1 or 2 extended spreader grafts and a caudal strut graft. The upper lateral cartilages can then be attached to the construct, thus reopening the internal valves. Some surgeons prefer a "top-down" approach, in which the dorsum is reconstructed with a rigid graft, and the middle vault is suspended from it. A classic example of this is the placement of a split calvarial bone graft into a tight pocket made via an intercartilaginous incision (see Image. Additional Rhinoplasty Grafting Materials). If the nasal bones are rasped to create a raw surface, the graft will usually heal in place without fixation using hardware, although plate and screw fixation is also an option when the graft is placed via an open approach. Rib is a popular grafting material, as well, because it contains both bony and cartilaginous components, and therefore mimics the natural nasal structure more closely than a bone-only calvarial graft.[50]
Management of the Lower Third
Modifying the supratip: A common presenting complaint is a "bulbous" nasal tip, which is frequently a result of excessive width and/or curvature of the lateral crura of the lower lateral cartilages. The classic maneuver to address this problem is cephalic trimming, in which bilateral strips of cartilage along the superior aspects of the lateral crura of the lower lateral cartilages are excised (see Image. Cephalic Trimming). Removing these strips reduces the prominence of the supratip region and also disarticulates the lower lateral cartilages from the upper lateral cartilages.
While the scroll region is technically one of the major tip support mechanisms, the removal of cartilage in this area and resultant soft tissue contraction during the healing process typically results in some upward rotation of the tip over time. When performing a cephalic trim, leaving 7 to 8 mm of lateral crural height intact to prevent alar retraction is known as a "complete strip" technique, referring to the remaining cartilage of the lateral crura. If a wedge of cartilage is removed from the lateral crura in addition to the cephalic trim, the technique is known as an "incomplete strip," which is used to augment the upward rotation of the nasal tip, albeit at the expense of structural stability.
Cephalic trimming can be performed endonasally, using a combination of inter- and intracartilaginous incisions, which results in the removal of the cephalic cartilage strip and its underlying skin. The maneuver may also be performed via the tip-delivery and open approaches without removing additional soft tissue from the cartilage. Similar to the cephalic trim is the cephalic turn-in maneuver, in which the cephalic aspects of the lateral crura of the lower lateral cartilages are folded medially and sutured behind the lateral crura rather than being excised. Doing this narrows the supratip region, like the cephalic trim, but it also helps to straighten out any irregular curves of the lateral crura and provides additional rigidity to reduce dynamic collapse during inspiration. Performing a cephalic turn-in involves making a cartilage incision in the same location as that used for cephalic trimming with a complete strip, but the incision is only partial thickness to facilitate a precise fold.
The vestibular skin is then elevated off the undersurface of the lateral crus to make a pocket that will fit the folded cartilage. Finally, the cartilage is folded and sutured in place, through the vestibular skin and 2 layers of cartilage, with the knot left in the naris; a 5-0 chromic gut suture works well. For noses with overly narrow supratip regions, often due to prior rhinoplasty, placement of a lateral crural spanning graft across the anterior septal angle will help to lateralize the lateral crura of the lower lateral cartilages, thus providing more supratip width and improving the nasal airway. These grafts are trapezoidal and laid flat, transversely atop the quadrangular cartilage, with the wider side of the trapezoid in the cephalic position and the narrow side just behind the nasal tip.
The oblique sides of the trapezoid then push outwards on the lateral crura. Securing this graft very precisely with permanent sutures is critical, as any tilt will cause visible asymmetry in the nasal tip. Lastly, excessive projection of the supratip may be due to a tall anterior septal angle, whether congenital (a "low" hump) or iatrogenic (a polly beak deformity). Removal of a strip of dorsal quadrangular cartilage is a simple remedy for this problem unless the etiology is a scar under the SSTE, in which case, triamcinolone injections or careful surgical debridement will be more effective. Caution should be used when shaving down the anterior septal angle for the same reason that a dorsal hump should be resected before performing a septoplasty; ensuring that an adequate L-strut remains after cartilage removal is critical.
Supporting the external nasal valve: Dynamic alar collapse with inspiration is a good indicator of external valve insufficiency, particularly when it occurs bilaterally. If the dynamic collapse is unilateral only, the etiology is more likely to be asymmetric airflow as a result of a septal deviation. When one side of the nose is significantly more patent than the other, airflow will tend to be more rapid through that side, leading to a decrease in pressure and a relative vacuum, which in turn causes alar collapse; this is an important manifestation of the Bernoulli principle. For these asymmetric alar collapse cases, fixing the septal deviation and reestablishing symmetric airflow will typically solve the problem. If there is bilateral dynamic collapse with inspiration, however, placement of alar batten grafts may be necessary.
Alar batten grafts are oblong and often beveled to minimize the extent to which they are visible beneath the SSTE. They are placed superficial to the lower lateral cartilages and may be implanted via an open approach and secured with sutures or inserted through limited marginal incisions into tight pockets (see Image. Common Cartilage Grafts Employed in Rhinoplasty). The key to ensuring the grafts' effectiveness is identifying the exact location of collapse and placing the grafts so that they underlie the area in question and cantilever off of the bony piriform rim to derive support. Marking the points of maximum collapse during forced inspiration in the preoperative holding area is ideal, but if this does not occur, placing the end of a suction tube near the naris intraoperatively will cause an alar collapse in an approximation of the actual physiological problem.
Modifying alar contour: Depending upon the desired correction, numerous options are available to adjust the contour of the nasal alae. Cephalic turn-in flaps have been discussed above as an effective means of reducing asymmetry and contour irregularity of the lateral crura of the lower lateral cartilages while also reducing supratip fullness. For patients who need correction of lateral crural irregularities but who do not have excess supratip fullness or have already undergone cephalic trimming, placement of lateral crural strut grafts represents an alternative. These grafts, first described by Gunter and Friedman in 1997, are placed on the deep surface of the lateral crura of the lower lateral cartilages and used to straighten, reinforce, or reposition the crura (see Image. Common Cartilage Grafts Employed in Rhinoplasty).[51]
Repositioning of the lateral crura can be accomplished by dissecting them away from the underlying vestibular skin and shifting them inferiorly, particularly to resolve a parenthesis deformity caused by excessive cephalic rotation of the lateral crura, then suturing them in place without grafts; grafting does provide more stability, however. Reinforcement of the alar margin to prevent retraction, reduce dynamic collapse, or reverse retraction can be accomplished with thin alar rim grafts, which may be placed into tight tunnels made just inside the alar margins, or with articulated rim grafts, which are larger, triangular cartilage grafts placed along the alar margins but sutured just lateral to the domes of the lower lateral cartilages (see Image. Common Cartilage Grafts Employed in Rhinoplasty).[52]
Articulated rim grafts, being more robust, are also more effective for managing a cloverleaf deformity, in which there are prominent bilateral vertical creases just between the domes and the alae, resulting in a 4-lobed appearance to the lower third of the nose: 2 domes and 2 alae. For severe alar retraction, however, cartilage grafting alone may not be sufficient, especially if the retraction results from aggressive cephalic trimming with resection of vestibular epithelium; in these cases, placement of composite free chondrocutaneous grafts from the cymba concha or the crus helicis of the auricle may be required.
Adjusting the alar base: The most common techniques used to adjust the width of the alar base are sill and Weir excisions. Both are comparatively simple techniques that remove nothing more than skin and rely upon careful incision placement and meticulous closure to produce the desired result. For an excessively wide alar base, sill excisions can be used to narrow the nostrils either unilaterally or bilaterally. A scalpel is held with the flat of the blade resting on the inner surface of the ala in question and then gently tracked along the contour of the ala until the cutting edge makes contact with the nasal sill, which it will do at a slight angle. The incision is made 3 to 4 mm in length and 2 to 3 mm in depth, with a symmetric incision medially that will remove a wedge of skin.
The incision is closed carefully with fine, resorbable sutures (such as 6-0 plain gut), taking care to evert the wound edges to prevent notching. Ensuring the effect is symmetric between the left and right sides is critical, and this will not always require symmetric excisions. In some cases, an excision is required on only 1 side. Making a single incision on the non-operated side and closing with an identical suture will result in a symmetric scar, which patients tend to tolerate better than no scar on the unoperated nasal sill. Weir excisions are performed when the alar flare, rather than the alar base width, is excessive.[53] These are crescentic skin excisions placed on the posterior aspects of the alae, just anterior to the alar-facial grooves. After meticulous closure, the lateral curvature of the alae is reduced, thus reducing the width of the lower third of the nose commensurately. As with sill excisions, symmetry of the result is critical. Weir excisions and sill excisions may be combined, if appropriate. On the other hand, patients with very narrow nares and minimal alar curvature do not usually require nearly as much intervention to correct. The loss of tip projection inherent in an open rhinoplasty approach is usually sufficient to release the tension in the alae and permit them to curve outward; convex alar rim grafts may also be employed.
Tip Modification
Producing an attractive, natural-appearing, and functional nasal tip is perhaps the most challenging aspect of rhinoplasty, particularly in a previously operated nose. Myriad approaches have been described, evolving from destructive, resection-based maneuvers to reversible techniques that rely upon grafting and suturing.[54] Many of these techniques have more than 1 effect, such as increasing tip projection and refinement, or rotation and projection, which may be beneficial for some patients but inappropriate for others. Because of the volume of information available on the topic, an overview will be presented below. For a more in-depth discussion of tip-shaping rhinoplasty techniques, please see the following article: Rhinoplasty Tip-Shaping Surgery.
Tip projection and support: Techniques for modifying tip projection usually involve either adding onto the nasal tip or pushing up the nasal tip from below. Placing cartilage grafts onto the tip will increase projection as well as change the shape of the tip, according to the shape of the graft, thus also serving to refine it. A similar effect can be achieved with careful placement of sutures into the domes of the lower lateral cartilages. Building up the tip itself can be accomplished to a limited degree with columellar strut grafting, which involves placement of a flat cartilage graft, either rectangular or with a slight angulation about halfway along it, between the medial crura of the lower lateral cartilages (see Image. Columellar Strut).
This graft is commonly used to prevent the loss of projection and support that necessarily accompanies an open rhinoplasty approach due to division of the interdomal ligaments, elevation of the SSTE, and violation of other tip support mechanisms; it also works well for splinting the medial crura, thus straightening the columella. While it may be tempting to use the columellar strut graft to push the nasal tip upward if a significant increase in projection is desired, the graft is not a good choice for this purpose because it should not reach the nasal spine or it will cause clicking as it slips from side to side over the top of the bone. Greater projection of the tip is best accomplished with a septal extension graft, which is a broad, flat graft secured to one side of the caudal end of the nasal septum.
Fashioning this graft requires a fairly large piece of cartilage because it typically needs to overlap the entire height of the caudal septum by 4 to 5 mm for stability and still have the additional breadth and height required to extend the columella and increase tip projection beyond that. The medial crura of the lower lateral cartilages are typically sutured on either side of the septal extension graft, in the "tongue-in-groove" (eg, septocolumellar) fashion described by Kridel, which allows the tip's projection and rotation to be set as necessary while also providing excellent support.[55][56] The septal extension graft is also very effective for straightening a severely deviated caudal septum when used as a caudal septal replacement graft after resection of the deviated portion. Septal extension grafting can also be combined with sutures between the domes (interdomal sutures) to tighten, and thus straighten, the lateral crura of the lower lateral cartilages, a maneuver known as lateral crural tensioning.
The easiest way to employ a septal extension graft may be to suture it securely between the medial crura with 5-0 polydioxanone or chromic gut suture and then, using a double-prong skin hook under the domes, hold the nasal tip in the desired position and then secure the graft to the caudal septum via mattress stitches through the septum with 4-0 chromic gut suture. Reduction of tip projection is simpler to accomplish than augmentation of projection, as opening the nose or making a full transfixion incision will typically disrupt tip support mechanisms enough to provide 2 to 3 mm of tip retrusion. If more deprojection is required, such as for feminizing rhinoplasty, dome resections may be required, in which vertical strips of cartilage are removed from the domes, 2 to 5 mm in width, and the cut edges are sutured back together with an overlap to provide stability. Shortening the lower lateral cartilages in this manner will provide a reduction of tip projection.[57]
Tip rotation: In addition to the projection of the nasal tip out of the facial plane, its position relative to the upper lip is a defining feature, aesthetically speaking. Up to a point, greater rotation is seen as a "cute," youthful, and feminine characteristic, while rotation closer to 90º is more masculine, and tips with acute nasolabial angles often appear "older" and less attractive. These are important considerations when planning aesthetic rhinoplasty, particularly if rejuvenation or feminization is a goal. Understanding how operative maneuvers will affect tip rotation may be best accomplished using the tripod concept, as described by Anderson in 1969.
Each of the lateral crura of the lower lateral cartilages represents one leg of a tripod and the medial crura together serve as the other. Lengthening or shortening any of these legs will affect the position of the apex of the tripod, and therefore, the nasal tip. Fundamentally then, a medial crural steal (using sutures to shift the position of the bend in the lower lateral cartilage so that the domes move towards the medial crura) will decrease rotation and a lateral crural steal will increase it. In practice, however, other techniques are often employed instead. Septocolumellar (tongue-in-groove) suturing without a septal extension graft permits upward rotation of the tip and can also be used to help straighten a caudal septal deviation or contour irregularities of the medial crura.
When overdone, this technique may cause an unsightly reduction of the columellar show; however, a septal extension graft may be required if either substantial upward rotation or counterrotation (downward) is needed. Counterrotation is not commonly desired unless overrotation has occurred as a result of prior rhinoplasty or septal trauma/perforation. Upward rotation is requested much more often, hence the frequency with which cephalic trimming is performed. Caudal septal trimming, in which a slim wedge with its wider end at the anterior septal angle is removed from the caudal margin of the quadrangular cartilage, is another simple means of increasing tip rotation because it causes the medial crura to rotate superiorly as they retract toward the shortened caudal septum.
Tip refinement: Major changes in tip aesthetics often come from the adjustment of projection and rotation; however, the importance of changes to the width and fullness of the tip as well as the prominence and position of the tip-defining points cannot be overlooked. Tip refinement is a subtle and nuanced art that combines careful suture placement and meticulous grafting to produce the desired effect. Interdomal horizontal mattress sutures (between the 2 domes) serve to adjust the distance separating the tip-defining points, and thus the perceived width of the tip. Transdomal, or "intradomal," horizontal mattress sutures are placed across an individual dome to narrow it, thus increasing the definition of the tip-defining point as well as projecting and narrowing that side of the tip.
The surgeon should be aware of the numerous effects these suture techniques produce to avoid unintended consequences (the Newtonian Third Law of Rhinoplasty). While many surgeons prefer to place these sutures via an open approach or tip-delivery, they can be performed endonasally as well, provided that the sutures (5-0 or 6-0 polydioxanone or polypropylene) are thrown so that the knots are placed in the interdomal space to avoid visibility or palpability.[58] Graft placement onto and around the tip can have a similar effect to dome suturing but with fewer sequelae other than an increase in tip projection and the risk of subsequent graft migration. Commonly employed grafts include cap grafts, which sit atop the tip-defining points, and shield grafts, which are wider superiorly and narrow inferiorly (similar to a coffin) to augment the tip as well as the infratip lobule (see Image. Cartilage Grafting).
Careful beveling of these grafts will help to prevent unnatural visible contours under the SSTE, and fixating them securely with 6-0 polypropylene will minimize the chances of malpositioning. The thickness of the SSTE in the tip varies with ethnicity and sex and must be considered when performing tip-refining maneuvers because a thick SSTE will hide imperfections but require aggressive maneuvers to achieve the desired effect, while a thin SSTE will do the opposite. For this reason, Goldman developed a technique that employs vertical dome division and suturing of the cut ends back together in a side-to-side fashion using a horizontal mattress that produces a sharp ridge at the tip-defining point.[59] While this technique would result in unsightly bossae in a Caucasian woman with a thin SSTE, it achieves well-defined tip-defining points in patients with thicker skin.
Additional Grafting
After the structural work outlined above is complete, additional aesthetic adjustment may be desired before closing, particularly onlay or "camouflage" grafting. This can consist of small fragments of cartilage, often crushed or beveled to break up any visible outlines, or pieces of fascia, usually deep or superficial temporal. These grafts may be placed into concavities or laid over irregularities to smooth out the visible contours of the nose. These materials may also be used as premaxillary "plumping" grafts to augment the base of the columella and make the nasolabial angle appear less acute. Small grafts may be secured in tight pockets or fixated with fibrin glue, while larger grafts may require suturing. Large grafts are frequently used for dorsal augmentation, to correct a mild to moderate saddle deformity, project the bridge of a mesorrhine or platyrrine nose, or to decrease the depth of the radix to minimize the appearance of a dorsal hump (see Image. Cartilage Grafting).
Septal or costal cartilage may be used for onlay grafting, but given that the SSTE is often quite thin in this region, large, solid costal cartilage "canoe" grafts are often palpable, if not visible as well. Costal cartilage, being prone to warping, is likely to produce an irregularity over time, and even large septal cartilage grafts can migrate and distort the dorsal contour. Dorsal augmentation can also be performed with crushed or diced cartilage if the cartilage is molded into the desired shape before implantation. Two of the most common methods of achieving this are with the "Turkish delight" and Tasman techniques, in which the crushed cartilage is wrapped inside a sheet of cellulose mesh or fascia, or placed into a 3 cc syringe and fashioned into a hemicylinder with fibrin glue, respectively.[60][61][62] Synthetic implants are also an option, and they can be made from different materials like silicone and expanded polytetrafluoroethylene. The use of these implants is controversial when autologous tissue is available, as implant extrusion, skin loss, and infection are relatively common complications.[63]
Closure and Dressing
Closure is accomplished with resorbable gut sutures inside the nose (4-0 to 6-0), and either non-absorbable (6-0 or 7-0 polypropylene or nylon) or absorbable (7-0 polyglactin) sutures for the transcolumellar incision. For patients with a wide columellar base due to lateral flaring of the medial crural footplates, a buried columellar narrowing suture may be placed at this time. A 6-0 non-absorbable monofilament (polypropylene or nylon) is passed across the columellar base as a vertical mattress, using stab incisions on either side of the columella to bury the suture. If the suture is pulled very tightly, the tip project may increase slightly.
A silastic splint may then be sutured to each side of the septum to provide septal support and improve mucosal healing; this can be done with or without septal quilting sutures.[64] Several strips of paper tape are distributed over the dorsum and a cast is placed over the tape (see Image. Rhinoplasty Dressing). Unless flail bone segments or large septal rents are present, the cast, tape, and splints are removed 7 days postoperatively. The splints, tape, and cast may be left in place for an additional week if prolonged support is required to enhance healing. Injection of liposomal bupivicaine to block the infraorbital, infratrochlear, and external nasal nerves may be performed to improve pain control for the first few postoperative days and reduce opioid requirements.[65]
Table. Location, Deformity, and Maneuvers to Consider in Rhinoplasty
| Location | Deformity | Maneuvers to Consider |
| Upper Third | Dorsal hump |
Small: shaving and rasping Large: incision and osteotomy ± radix grafting, consider preservation techniques (push-down and let-down) |
| Upper Third | Insufficient dorsal projection | Onlay grafting |
| Upper Third | Deviated upper vault | High-low lateral osteotomies ± intermediate osteotomy on the side contralateral to the direction of deviation, and transverse root osteotomy |
| Upper Third | Wide upper vault | High-low-high lateral osteotomies and medial osteotomies |
| Upper Third | Open roof* | High-low lateral osteotomies ± medial osteotomies ± onlay grafting |
| Upper Third | Rocker* | Percutaneous lateral osteotomies |
| Middle Third | Narrow midvault/internal nasal valve collapse | Spreader grafting (unilateral if correcting midvault asymmetry), autospreader flaps if there is upper lateral cartilage excess due to dorsal hump reduction, flaring sutures, or butterfly grafting if severe and SSTE is thick |
| Middle Third | Deviated midvault | Clocking sutures, unilateral spreader grafting |
| Middle Third | Inverted-V* | Resuspend upper lateral cartilages to dorsal septum and/or spreader grafting |
| Middle Third | Saddle* | Onlay grafting and/or dorsal septal reconstruction with extended spreader grafts and caudal strut |
| Lower Third | Excessive supratip width | Cephalic trimming |
| Lower Third | Excessive tip width | Tip-defining suturing, dome division |
| Lower Third | Insufficient tip definition | Tip-defining suturing, tip grafting (shield grafting if infratip lobule insufficient), Goldman dome division technique if SSTE thick, thinning of SSTE |
| Lower Third | Insufficient tip support | Columellar strut grafting or septal extension grafting and septocolumellar suturing |
| Lower Third | Insufficient tip projection |
Mild: tip grafting Severe: septal extension grafting and septocolumellar suturing ± lateral crural steal |
| Lower Third | Excessive tip projection |
Mild: septocolumellar suturing with medial crural steal Severe: dome division and resection |
| Lower Third | Insufficient tip rotation | Septocolumellar suturing |
| Lower Third | Excessive tip rotation | Septal extension grafting and septocolumellar suturing |
| Lower Third | External nasal valve collapse | Alar batten grafts, articulated rim grafts |
| Lower Third | Lower lateral cartilage asymmetry/insufficiency | Cephalic turn-in flaps, lateral crural strut grafting, lateral crural tensioning |
| Lower Third | Narrow nostrils | Deproject tip via open rhinoplasty approach, rim grafts |
| Lower Third | Widened columella | Medial crural footplate suture |
| Lower Third | Excessive alar base width | Nasal sill excisions |
| Lower Third | Excessive alar flare | Weir excisions |
| Lower Third | Caudal septal deflection |
Mild: swinging door technique Severe: resection and replacement with septal extension graft |
| Lower Third | Hanging columella | Septocolumellar suturing |
| Lower Third | Columellar retraction | Septal extension grafting |
| Lower Third | Alar retraction* |
Mild: rim grafting Severe: composite grafting from auricle |
| Lower Third | Tip ptosis* | Septocolumellar suturing ± septal extension grafting, caudal septal trimming |
| Lower Third | Polly beak* | Resection of cartilaginous dorsum and/or augmentation of bony dorsum ± debridement of scar/steroid injection ± correction of tip ptosis |
| Lower Third | Tip bossae* | Tip suturing, lateral crural tensioning, tip grafting |
| Lower Third | Pinched tip* | Lateral crural spanning graft |
| Lower Third | Parenthesis* | Lateral crural repositioning ± lateral crural strut grafts |
| Lower Third | Cloverleaf* | Articulated rim grafts ± septal extension grafting |
| Lower Third | Tombstone* | Remove tip graft or add fascial graft between tip graft and SSTE |
*Typically results from prior surgery.
This list is meant to be a quick reference resource and is by no means exhaustive.
Complications
The complicated interactions among the bones, cartilage, mucosa, skin, and other soft tissue components of the nose and intrinsic patient physiological factors make achieving predictable and consistent results from rhinoplasty a challenging proposition. An excellent result at the first postoperative visit may not remain so 1 year later (or even 5, 10, or 20 years later). Although the risk of major complications is low, every patient has a different experience during the postoperative period, and the healing process will vary for the same patient between surgeries if a revision is performed.
Rhinoplasty complications are generally categorized as functional, aesthetic, hemorrhagic, infectious, and traumatic.[66] While any deviation from the expected course of recovery can be problematic, in the long term, it is the functional and, especially, aesthetic complications that cause patients the greatest psychosocial distress and are most likely to result in litigation.[67] Patients with preexisting psychiatric comorbidities, such as body dysmorphic disorder, depression, and anxiety, are at higher risk of postoperative depression and dissatisfaction with the surgical result. These patients should only be offered surgery after careful counseling and consideration, and they should have strong social support from friends, family, and the interprofessional healthcare team during recovery.[26]
Functional Complications
Nasal obstruction
While many rhinoplasties and septorhinoplasties are performed to improve the airway, a poor result may exacerbate or even cause de novo nasal obstruction. Patients undergoing reduction rhinoplasty are at particular risk for this complication and should be counseled preoperatively to that effect. Nasal obstruction after rhinoplasty typically results from internal valve collapse or septal deviation, although some grafting techniques may also contribute, such as lateral crural strut grafts that impinge on the external nasal valve. Adhesions, or synechiae, between the nasal septum and the inferior or middle turbinates, may also reduce airflow, although these are more common when septal surgery is combined with sinus surgery.
Last, aggressive or repeated operations to reduce the size of the turbinates to improve airflow can cause a sensation of nasal obstruction. When the turbinate mucosa is injured, it may lose the ability to sense airflow despite widely patent nasal passages, and the resulting "empty nose syndrome" can be extremely distressing for patients.[68] Additionally, when airflow through the nasal passages is increased past a certain point in some patients, the mucosa can become dry and atrophic, leading to crusting, hyposmia, and a sense of nasal obstruction. This condition is known as atrophic rhinitis.[69]
Septal perforation
Iatrogenic perforation is most commonly caused by tearing the mucoperichondrium during septal surgery, with persistent perforations more likely to occur when bilateral, opposing mucoperichondrial defects are created and the intervening cartilage or bone is removed. Revision septal surgery presents a higher risk of persistent perforation due to the challenging nature of developing intact septal mucoperichondrial flaps when tissue planes have been replaced by scar tissue and the cartilage or bone between the flaps is absent. Septal perforations can range from small defects that cause a whistling sound when breathing, to large perforations that cause crusting, nasal obstruction, epistaxis, and saddle deformity. Small perforations may not require any treatment beyond nasal saline sprays, but larger perforations may require surgical intervention, such as septal button placement or reconstruction with local, regional, or free tissue transfer.[70]
Hyposmia
Changes to the sense of smell are common after nasal surgery, particularly if the olfactory epithelium is manipulated. Patients may complain of hyposmia, anosmia, dysosmia, or even an improvement in the sense of smell if there was substantial nasal airway obstruction preoperatively.[71] Most cases of postoperative decreases in olfactory acuity are self-limited or may be alleviated with intranasal steroid sprays; however, some cases are persistent and may require olfactory retraining to improve function.[72]
Rhinitis
Nasal discharge, dryness, and congestion are often temporary complications, especially when an obstructed airway has been improved. Symptoms are usually treated with topical agents, such as saline spray and fluticasone. In some cases, an increase in allergic rhinitis symptoms may coincide with the postoperative period if the surgery is performed in the spring or summer, and this should be considered in the differential diagnosis. Likewise, some patients may notice an increase in allergic symptoms after improvement of nasal airflow. If rhinorrhea persists after a few weeks, a cerebrospinal fluid leak should be suspected.
Aesthetic Complications
Some say "happiness is the degree to which perception exceeds expectations." On the other hand, when the perception of the outcome fails to meet patient expectations, dissatisfaction ensues. That said, not all of these instances represent aesthetic complications. Most true aesthetic complications result from surgical misadventures, such as over-resection of cartilage that leaves inadequate support of the nasal skeleton, failure to secure grafts appropriately, or misdirected osteotomies. In addition to new deformities resulting from surgery, failure to correct preoperative abnormalities (such as dorsal deviation, caudal septal deflection, or tip asymmetry) may also be considered adverse events if not "complications."
Upper third
The most common iatrogenic deformities seen in the bony vault are the "open roof," "rocker," and "step-off" deformities, which all result from osteotomies. The open roof is a gap in the bone of the central upper vault that occurs when a dorsal hump is resected but no osteotomies are performed to bring the remaining lateral walls together in the midline. A rocker deformity is caused by lateral osteotomies that continue too far superiorly past the nasofrontal suture and into the frontal bone as it begins to flare out into the glabella. When force is subsequently applied to the lateral walls of the upper vault, the bone inferior to the nasofrontal suture will medialize appropriately, but the bone superior to the suture will "rock" laterally and create a contour abnormality. Step-off deformities are produced by medially placed lateral osteotomies. The bony cut should occur within the nasofacial junction, but if it is placed medially to the junction, the osteotomy may become palpable as a ridge running along the side of the nose.
Middle third
The middle vault of the nose comprises the dorsal aspect of the quadrangular cartilage and the upper lateral cartilage. If an excessive amount of septal cartilage is removed, either harvested for grafting or excised for functional purposes, the dorsum of the midvault may collapse over time, causing a saddle deformity. To prevent this from happening, 10 to 15 mm of dorsal septum height should be left intact after septoplasty or quadrangular cartilage harvest, and the junction of the dorsal quadrangular cartilage and the perpendicular plate of the ethmoid bone at the keystone area should not be disarticulated. Saddle deformities are not all iatrogenic; septal perforations and posttraumatic septal hematomas can also erode support of the nasal dorsum.
The "inverted-V" deformity, on the other hand, is very much a stigma of prior rhinoplasty. When a dorsal hump with a significant cartilaginous component is resected, the junction of the upper lateral cartilages and the dorsal quadrangular cartilage is often removed as part of the hump. If the rhinoplasty is performed through an open approach, resuspending the upper lateral cartilages to the dorsal septum is very straightforward. If the rhinoplasty is performed endonasally, affixing the upper lateral cartilages to the dorsal septum is very challenging and is often not even attempted. Leaving the upper lateral cartilages disarticulated from the quadrangular cartilage allows them to sink downwards into the nose, leaving the dorsal edge of the quadrangular cartilage visible through the thinnest portion of the SSTE and similarly exposing the caudal edges of the nasal bones.
In addition to causing a visible abnormality, failure to resuspend the upper lateral cartilages to the septum is liable to cause internal nasal valve collapse and consequent nasal obstruction, as can a saddle deformity.[73] Las t, the "polly beak" is another iatrogenic deformity that occurs as a result of rhinoplasty, typically caused by an error during dorsal hump reduction. If the bony portion of a dorsal hump is overresected relative to the cartilaginous portion, or if the cartilaginous portion is underresected relative to the bony portion, the patient can be left with what appears to be a dorsal hump centered over the supratip area.
The apparent severity of the polly beak is exacerbated if it is accompanied by tip ptosis, loss of tip projection, or excessive supratip scarring or edema under the SSTE. Supratip scarring and edema, fortunately, can usually be managed successfully with triamcinolone injections and taping rather than requiring operative revision.[74] Most other aesthetic complications will not resolve without surgery, however, which is generally delayed 6 to 12 months after rhinoplasty to let the postoperative edema subside to the greatest extent possible before reoperating.
Lower third
The lower third of the nose, containing the tip and alae, is the most anatomically, functionally, and aesthetically complex portion of the external nose. For this reason, it is prone to several different deformities that may occur after rhinoplasty. Alar retraction is a common problem that occurs after overly aggressive cephalic trimming when a complete strip of lateral crus measuring at least 7 mm in width is not left intact. Excessive manipulation of the domes, either with suturing or cartilage resection, can lead to a "pinched tip" appearance or bossae of the tip, in which wrinkles or folds in the cartilage are visible through the SSTE.
Similarly, a "tombstone" deformity occurs when a tip graft without appropriately beveled edges or a fascial onlay is placed under thin skin, resulting in a starkly visible outline of the graft. Malrotation of the nasal tip can also result from rhinoplasty, either ptosis from failure to support the tip sufficiently or overrotation due to overly aggressive septocolumellar suturing or cephalic trimming. When tip modification maneuvers (eg, transdomal suturing, grafting, division, and tensioning) are performed imprecisely, visible asymmetry may occur either immediately postoperatively or weeks to months later. Finally, excessive resection of the lateral crura of the lower lateral cartilages can disrupt support of the external valve, causing dynamic alar collapse and nasal obstruction. Ironically, the application of grafts to the lateral crura of the lower lateral cartilages, such as lateral crural strut grafts and articulated rim grafts, can themselves cause external nasal valve stenosis if they are too thick.
Hemorrhagic Complications
Epistaxis
Postoperative bleeding is a common occurrence after rhinoplasty and should not necessarily be considered a complication unless epistaxis occurs that is not self-limited and the patient cannot control it at home. Bleeding tends to be mild and usually resolves with head elevation and nasal decongestant sprays. Compression may be applied as well, but this is usually discouraged after nasal surgery due to the risks of pain and compromise of the operative result. If bleeding continues, packing the nose may be required, although this is extremely rare. Patients with this degree of postoperative hemorrhage should undergo an evaluation for hypertension and coagulopathy. Tranexamic acid may be administered intravenously or applied to the packing to increase its efficacy, if necessary.
Septal hematoma
Blood collecting between the septal mucoperichondrial flaps after trauma or septal surgery presents as an erythematous or purpuric mass that is typically visible on both sides of the septum. This is usually painful, and the patient can also present with fever, anosmia, and airflow obstruction. Septal hematomas should be recognized and drained promptly to prevent infection and subsequent erosion of septal cartilage, which may in turn lead to septal perforation and/or a saddle deformity. After evacuation of the hematoma, a drain or nasal passage packing should be placed to prevent reaccumulation of the blood and the patient should be reassessed in 24 hours. If a septal abscess is suspected, antibiotic therapy must be started immediately.
Infectious Complications
Infections after rhinoplasty can range from mild cellulitis of the SSTE to sepsis from toxic shock syndrome. Cellulitis after rhinoplasty usually presents as an early complication and typically responds well to cephalosporins, but close observation is necessary for preventing progression. Cultures and sensitivities should be obtained, and if Pseudomonas aeruginosa is identified, an aminoglycoside or other antipseudomonal agent may be used to irrigate the wound to prevent loss of cartilage. Fortunately, severe infections are very rare, and even minor ones tend to be the sequelae of intrinsic patient factors, such as immunodeficiency or an inability to stop picking at the nasal crusts during the recovery period, rather than the result of bacterial contamination during surgery.
As a whole, infections occur in less than 1% of rhinoplasties. Early evaluation, appropriate antibiotic treatment, and prompt tissue debridement are critical for preventing complications like tissue necrosis and toxic shock syndrome.[10][75][76] Many studies have investigated the efficacy of administering antibiotics during and after nasal surgery, but practices remain varied. There is evidence that a single dose of preoperative prophylactic antibiotics does decrease the risk of postoperative infections.[77] Regarding the use of antibiotics postoperatively, however, neither the World Health Organization nor the American Academy of Otolaryngology-Head and Neck Surgery recommend their use for more than 24 hours.[78][79]
Traumatic Complications
These include septal deformities or collapse due to injury to the L-strut, intracranial injuries, and injury to the lacrimal system. In the case of an unnoticed septal injury, deformities are usually seen as late complications, as the soft tissue envelope contracts over the nasal skeletal framework. These often require secondary procedures to correct them. If a septal injury is noticed during surgery, it must be repaired before the end of the operation.
Sensory nerve injury
The nasopalatine nerve passes through the septum and exits the nasal cavity via the incisive foramen, posterior to the anterior nasal spine. If septal manipulation is performed during the procedure, nerve injury may result, causing hypesthesia or paresthesia of the premaxilla. Patients will complain of numbness or sensitivity of the upper lip, maxillary incisors, and/or the base of the nose. These complaints are almost always self-limited but may persist for weeks or months postoperatively.
Lacrimal system injury
Excessively lateral osteotomies may produce epiphora and bleeding from the lacrimal puncta if the nasolacrimal duct is disrupted. Treatment may require stenting of the lacrimal system, or potentially dacryocystorhinostomy in severe cases. Epiphora can occur in the first few weeks after rhinoplasty due to edema compressing the lacrimal ducts, however, and this resolves spontaneously.
Intracranial injury
These are, fortunately, extremely rare complications and often cannot be avoided by any means other than meticulous surgical technique and good luck that the patient does not have any previously undiagnosed conditions, such as hyperhomocysteinemia or a skull base dehiscence, which may predispose them to thrombosis or cerebrospinal fluid leak, respectively, the latter presenting as clear rhinorrhea and headaches. Most of these cases will be resolved with conservative measures, such as bed rest and elevating the head of the bed, avoidance of straining, and potentially a lumbar drain or blood patch.[80] Nevertheless, neurosurgical consultation is recommended. As a result of a cerebrospinal fluid leak, or even in its absence, meningitis may also occur after rhinoplasty, as can pneumocephalus or even brain laceration.[67] Last, intracranial venous sinus thrombosis has been reported several times in the literature and may be fatal.[81][82]
Clinical Significance
When successful, rhinoplasty has been shown to provide patients myriad benefits in functional and psychological domains. Social confidence can increase significantly with cosmetic improvements, particularly in women, thereby improving quality of life, although men are more likely to be pleased with the outcome than women, based on a 2020 comparison of preoperative and postoperative Rhinoplasty Outcome Evaluation (ROE) scores.[26][83] Sense of smell also tends to benefit, albeit subtly, and even obstructive sleep apnea and snoring may improve in certain cases.[84][85][86] Patients with allergic rhinitis have similar improvements in nasal airflow after rhinoplasty compared to patients without allergic rhinitis, and rhinoplasty may even be a useful adjunct for patients with allergic rhinitis if maximal medical management does not produce sufficient relief of nasal obstruction.[87]
Depending on which maneuvers are employed during surgery, nasal airflow stands to improve significantly as well. Septoplasty with turbinoplasty lowers the Nasal Obstruction Symptom Score (NOSE) score by an average of 40 points. When spreader grafting is added to septoturbinoplasty, the average decrease is 49 points.[88] Septal swell body reduction has also been shown to increase nasal airflow, lowering the NOSE score by 20 to 45 points on average, depending on patient selection.[89]
Successful surgery, however, cannot be taken for granted. Achieving good outcomes requires skilled hands and, more importantly, skilled decision-making from the preoperative evaluation and counseling through to the recovery period. The importance of identifying appropriate surgical candidates, eliciting their goals, providing them with reasonable expectations, and supporting them through the process cannot be overstated. With a firm foundational knowledge of nasal anatomy and physiology, the expert rhinoplasty surgeon does all of this in addition to determining which operative maneuvers will provide the optimal result for the patient, taking into account the context of the patient's face as a whole.
Enhancing Healthcare Team Outcomes
Achieving the best result and smoothest recovery after rhinoplasty can only be accomplished when the skills and talents of every member of the interprofessional team are leveraged appropriately. While it is the surgeon's responsibility to plan and execute the operation proficiently as well as optimize the recovery, the surgery will not proceed safely and efficiently without a skilled anesthesia clinician who can emerge the patient smoothly and without agitation, coughing, emesis, or hemodynamic instability. Psychiatric evaluation is also essential for certain patients, either to distinguish good surgical candidates from poor ones or to optimize marginal candidates for surgery from a behavioral health perspective.
As opioid pain medications fall out of favor, pharmacists are becoming more and more critical for planning multimodality pain management by adding long-acting local anesthetic injections, cyclooxygenase-2 inhibitors, acetaminophen, gabapentin, and potentially other medications to the regimen. Nursing staff provide a primary point of contact for patients throughout the perioperative period, addressing any concerns and providing reassurance as necessary, as well as education regarding additional interventions to increase patient comfort: head of bed elevation, gentle icing of the midface, avoidance of activities that elevate blood pressure, and use of topical or oral Arnica montana.
Media
(Click Image to Enlarge)

Standard Photographs for Rhinoplasty. These views – including bilateral profile and three-quarter views, should be taken prior to and after rhinoplasty in order to inform preoperative counseling and planning as well as to assess results postoperatively. The frontal view (A) provides a perspective on the width of the nose as well as its relationship to the rest of the face. The profile (B), aligned in the Frankfort horizontal plane (dashed line), reveals the projection, rotation, and any dorsal, alar, or columellar irregularities. The three-quarter view (C), aligned in the Frankfort horizontal plane with the tip of the nose tangent to the cheek, permits assessment of the brow-dorsum-tip aesthetic line. The 'bird’s eye' view (D) emphasizes any lateral deviations of the dorsum or tip. The 'worm’s eye,' or basal, view (E), with the nasal tip centered between the brows, allows evaluation of tip deviation, nostril symmetry and nasal base proportions.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
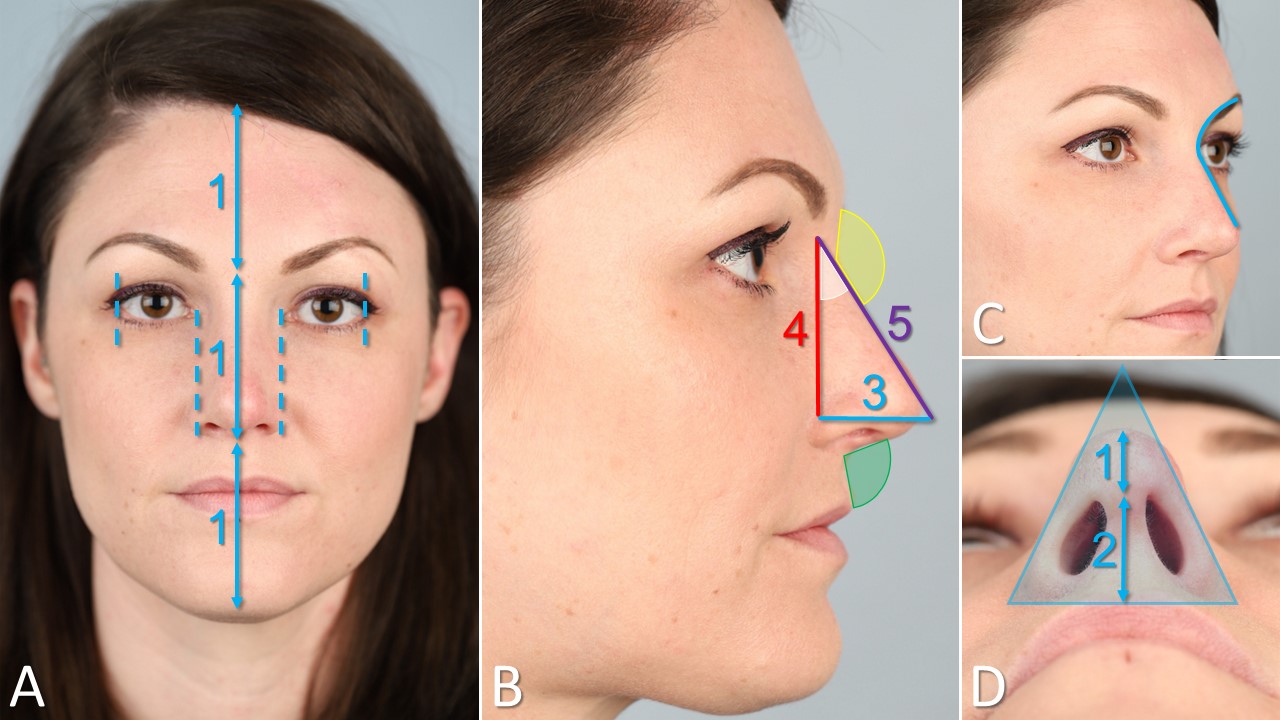
Nasal Analysis. A) The forehead height (trichion to glabella) should equal the midface height (glabella to subnasale) and the lower face height (subnasale to menton). The alar width should equal the intercanthal distance and the palpebral fissure width. B) The tip projection (blue) with the nasal height (red) and length (purple) should make a 3:4:5 Pythagorean triangle. Tip projection should equal cutaneous upper lip height. The nasolabial angle (green) measures the rotation of the nasal tip relative to the upper lip. The nasofacial angle (white) measures the prominence of the nose from the plane of the face, and the nasofrontal angle (yellow) measures the acuity/depth of the nasal radix. C) The three-quarter view assesses the brow-dorsum-tip aesthetic line and emphasizes lateral dorsal contour irregularities, e.g. rhinion horns. D) The basal view evaluates the shape of the nasal base and its proportions; the length of the columella should be twice the infratip lobule length.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
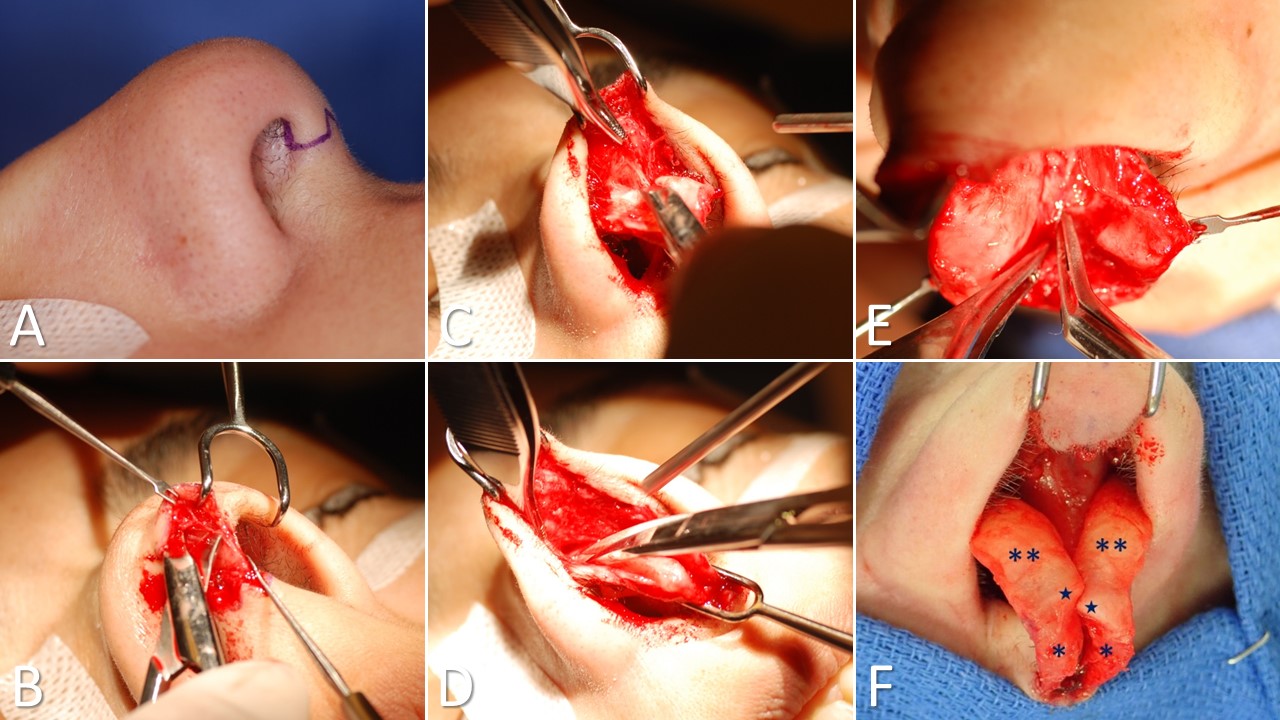
Open Rhinoplasty Approach. The marginal incisions are marked with an “inverted-V” transcolumellar portion (A). The transcolumellar portion is made using a scalpel, followed by the rest of the marginal incisions with scissors (B). The skin-soft tissue envelope is dissected off the lateral crura of the lower lateral cartilages (C). The upper lateral cartilages are exposed (D). The interdomal ligaments are divided to reveal the septal cartilage between the lower lateral cartilages (E). Nasal tip anatomy viewed through an open rhinoplasty approach. The medial crura are indicated by single asterisks, and the lateral crura are indicated by double asterisks. Stars mark the tip-defining points of the domes (F).
Contributed by MH Hohman, MD, FACS, and C Llewellyn, MD
(Click Image to Enlarge)
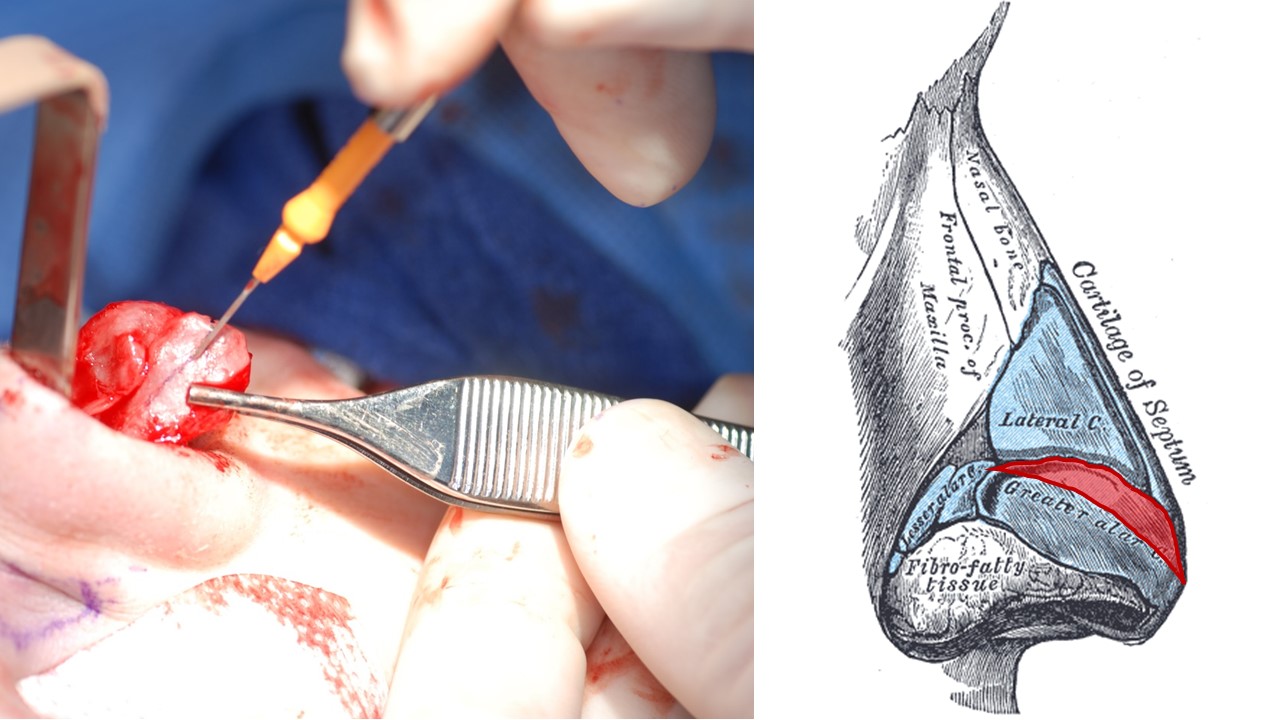
Cephalic Trimming. A cephalic trim of the lateral crus of the lower lateral cartilage reduces supratip width. A 7 mm wide strip of lower lateral cartilage is left intact for tip support (being held in place by forceps). The image on the right shows a schematic of a cephalic trim, with the resected cartilage highlighted in red.
Contributed by Marc H Hohman, MD, FACS and Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
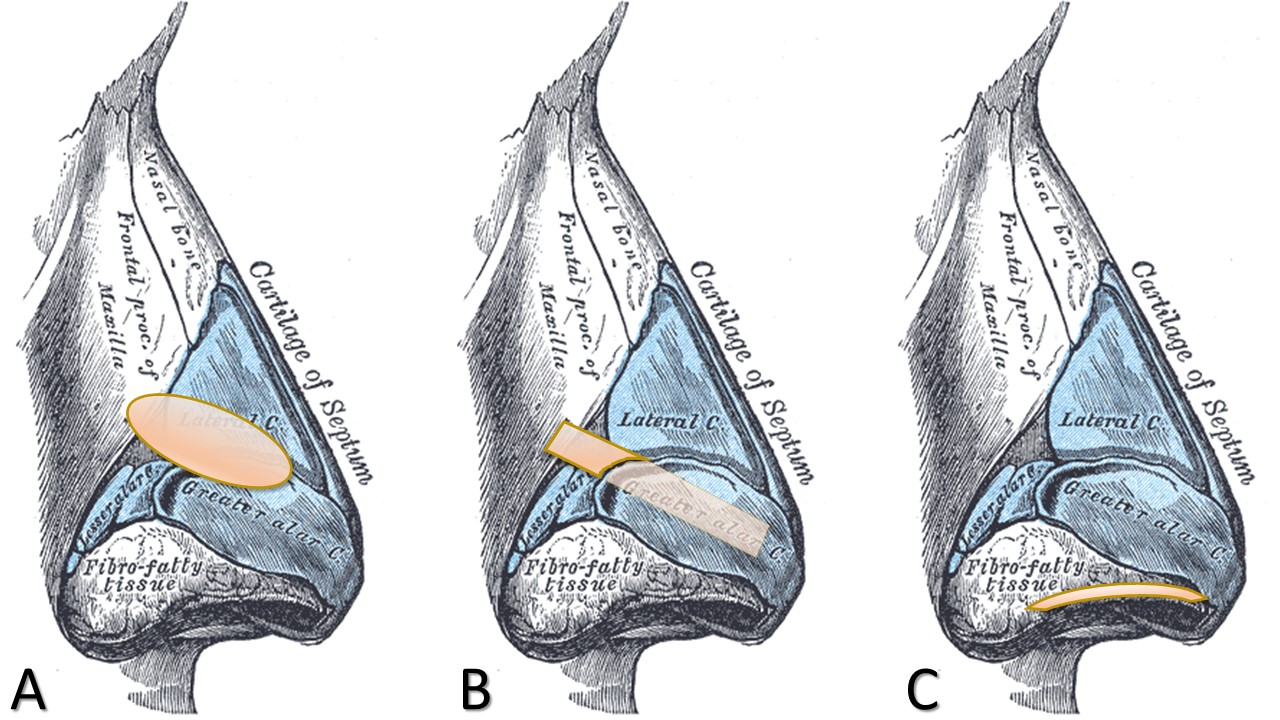
Common Cartilage Grafts Employed in Rhinoplasty. A) Alar batten graft: onlay graft used for supporting the nasal valve and preventing collapse during inspiration. B) Lateral crural strut (Gunter) graft: underlay graft used for straightening and supporting the lateral crus of the lower lateral cartilage – it may or may not extend to the frontal process of the maxilla, depending upon its purpose. C) Alar rim graft: used for supporting the margin of the ala in order to improve symmetry, open the vestibule, and/or prevent alar retraction.
Contributed by Marc H Hohman, MD, FACS and Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
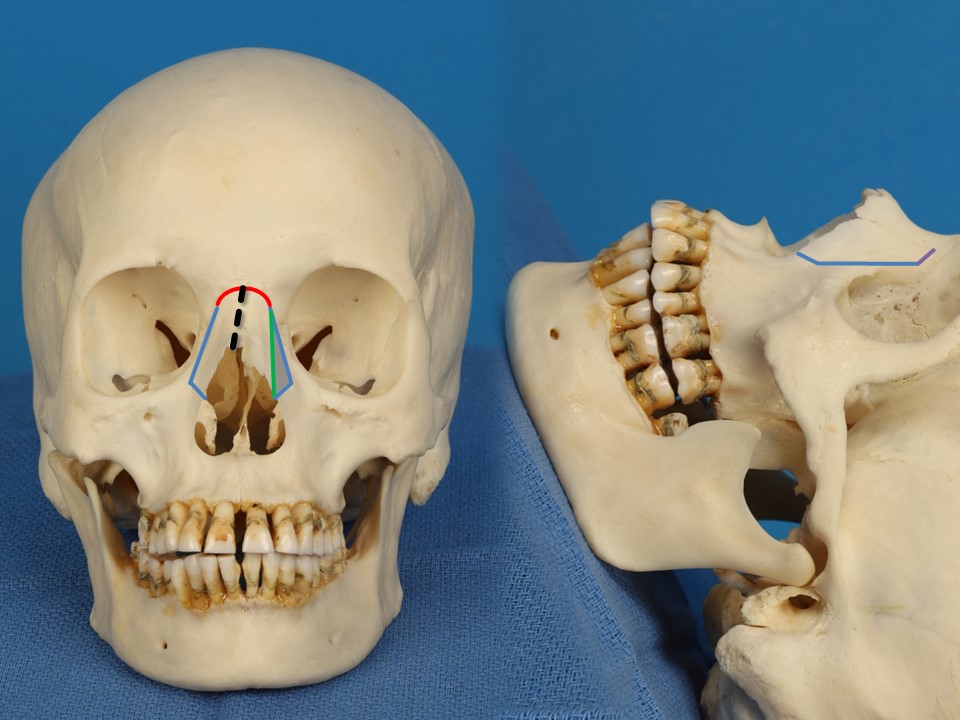
Nasal Osteotomies for Shifting a Deviated Bony Vault. Left: the high-to-low lateral osteotomies (blue) release the lateral attachments of the bony nasal vault at the nasofacial junction. The transverse osteotomy (red) is made percutaneously through the nasofrontal suture. The intermediate osteotomy (green) allows the thin lateral segment (shaded) to collapse inwards and permits the bony vault to shift (to the left in this case). The deviated midline of this patient's bony nasal vault is shown as a dashed black line for illustration purposes. Right: the terms "high-to-low" and "high-low-high" lateral osteotomies refer to the paths the cuts take with the patient in the surgical position, beginning with the origin of the osteotomy near the inferior aspect of the lateral piriform rim. The nasofacial junction corresponds to the "low" portion of the osteotomy. The blue line represents a high-to-low osteotomy. When the purple segment is added, the osteotomy becomes "high-low-high."
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
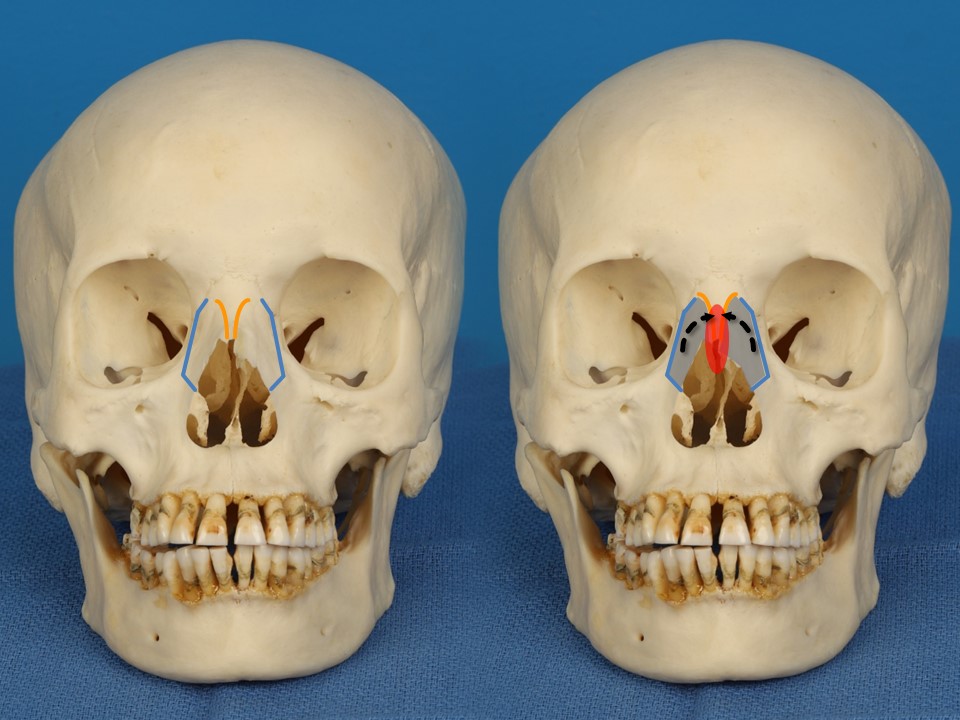
Nasal osteotomies for adjusting the width of the bony vault. The high-low-high lateral osteotomies (blue) release the lateral attachments of the bony nasal vault at the nasofacial junction. The medial osteostomies (orange) flare laterally from a paramedian origin to terminate near the superior extent of the lateral osteotomies. The medial and lateral osteotomies do not meet, but rather allow the superior extent of the bone segments to remain attached via greenstick fractures just superior to the level of the medial canthi. In the right image, the red oval represents a dorsal hump resection and consequent open roof, which is then closed via lateral osteotomies (blue) and completion medial osteotomies (orange) that allow the bone segments (shaded) to be mobilized medially to close the nasal vault.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
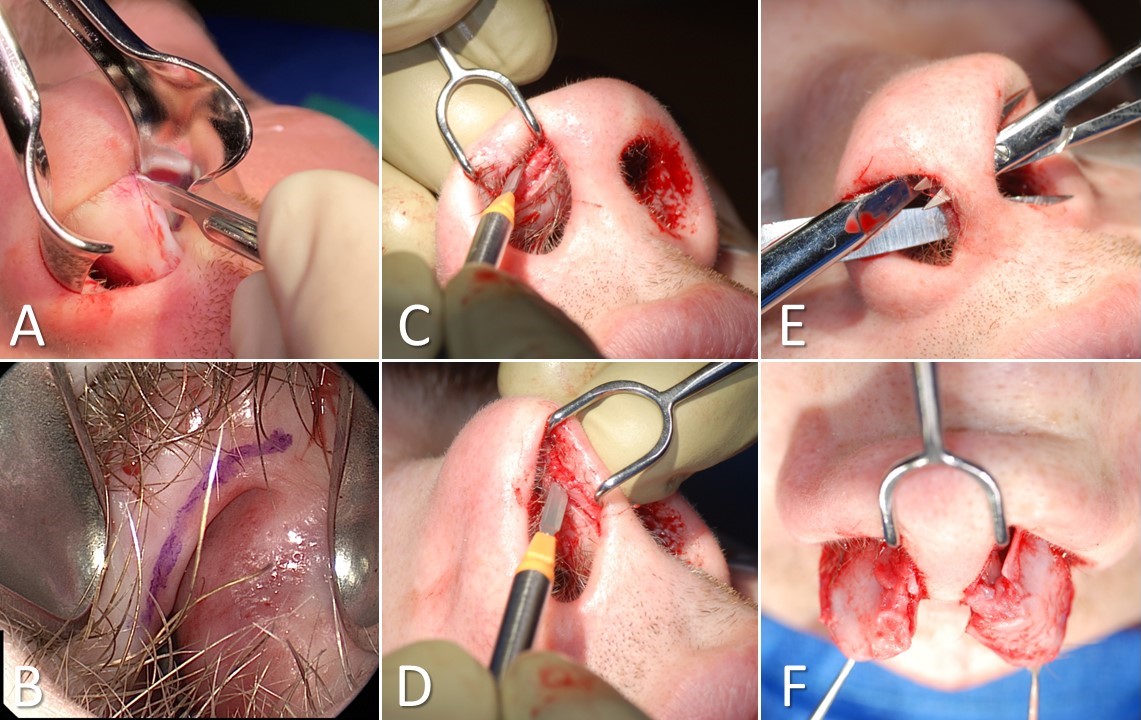
Tip-Delivery Rhinoplasty. A) A hemitransfixion incision on the right side of the caudal septum. The same incision is made on the left. B) An intercartilaginous incision (also used for closed rhinoplasty) is marked between the upper and lower lateral cartilages; it extends to the top of the hemitransfixion. C) The marginal incision follows the inferior edge of the lateral crus of the lower lateral cartilage, parallel and anterior to the intercartilaginous incision. D) The marginal incision continues along the anterior edge of the medial crus of the lower lateral cartilage, parallel and anterior to the hemitransfixion. E) Dissection through the hemitransfixion (large scissors) and marginal incisions (small scissors) releases the lower lateral cartilages anteriorly and posteriorly. F) After separation from the overlying soft tissue, the lower lateral cartilages and their underlying skin are delivered into the nares, remaining attached for perfusion medially and laterally.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
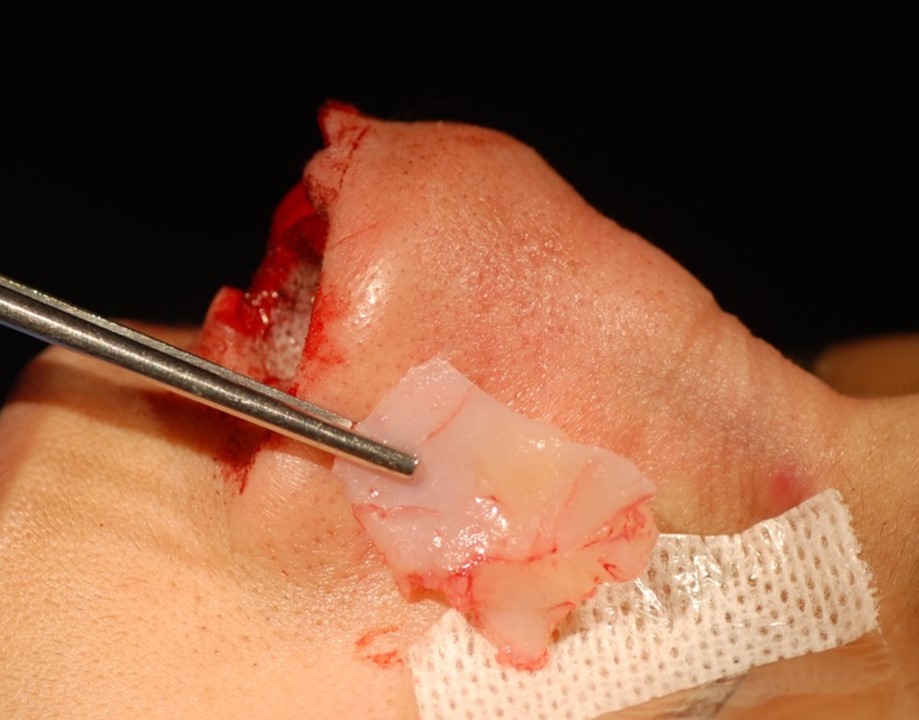
Septal Cartilage Harvest. A comparatively large piece of quadrangular cartilage may be harvested via a septoplasty approach without affecting the appearance or structural support of the nose, provded 10-15 mm of cartilage are left intact dorsally and caudally, and the junctions of the cartilage and bone remain undisturbed at the keystone area and the anterior nasal spine. If the harvested cartilage is sufficiently straight, it can be used for structural grafting. Alternatively, it can still be crushed and used for camouflage grafting.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
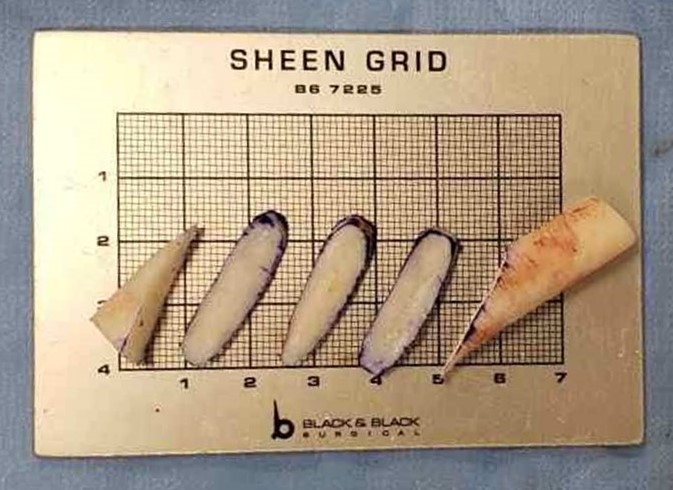
Costal Cartilage Grafting. If sufficient septal cartilage is unavailable for structural grafting, costal cartilage may be employed instead. It is more rigid than auricular cartilage, but prone to warping. Carving the cartilage into flat ellipses, as pictured, generally prevents distortion of the grafts.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
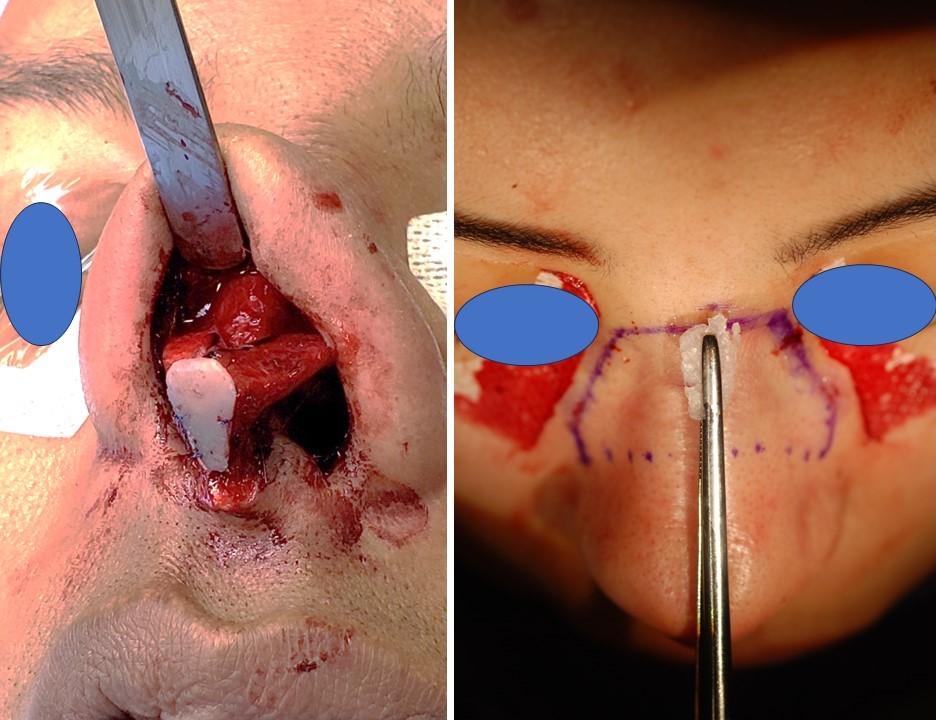
Cartilage grafting. Left: "shield" grafting improves tip definition and projection as well as adding fullness to the infratip lobule. When the inferior component is not included, the technique is termed "cap" grafting, which affects only the nasal tip itself. Right: crushed cartilage grafting is often applied to the radix and may be fixed in place with sutures, fibrin glue, or use of a tight soft tissue pocket. The technique is particularly useful for decreasing the prominence of a dorsal hump when the radix is deep. The cartilage is crushed to prevent its edges from being visible or palpable.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
Rhinoplasty Dressing. One method of dressing the nose involves 1/2 inch sterile tape strips applied in layers over the nasal dorsum and under the tip, followed by a thermoplastic splint to protect the nose and reduce postoperative edema. Silastic splints may be placed internally as well, particularly if a septoplsty is performed.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
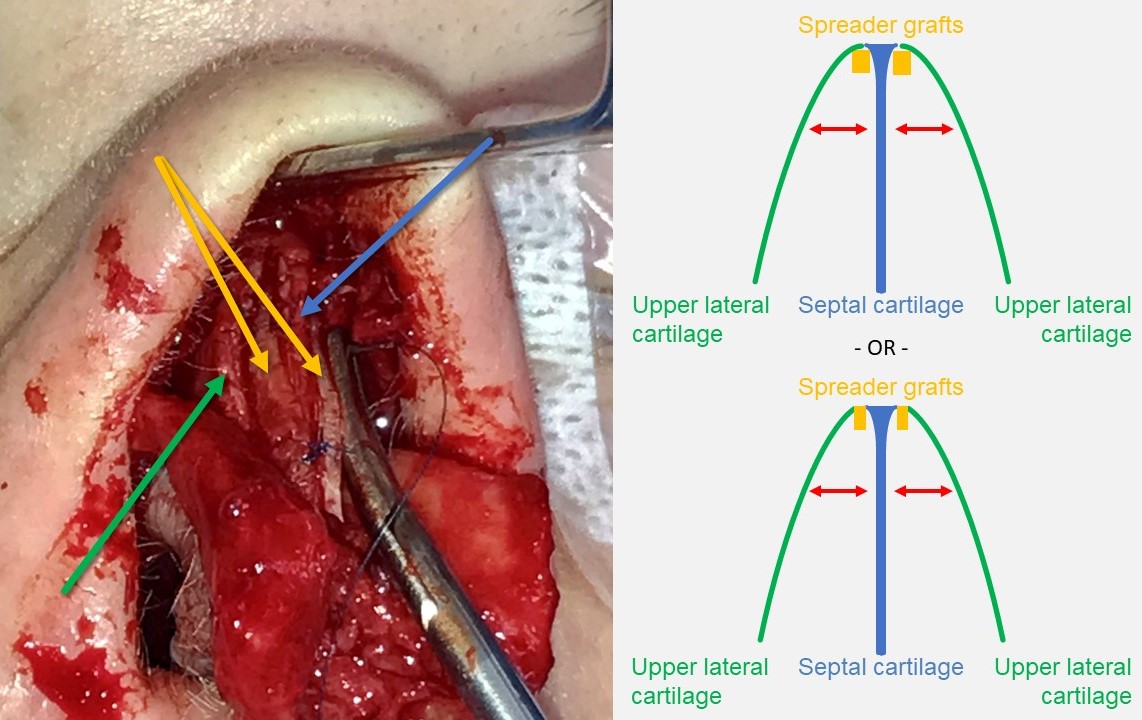
Spreader Grafting. The spreader grafts (yellow arrows), crafted from harvested septal cartilage, are sutured to both sides of the dorsal septal cartilage (blue arrow). The upper lateral cartilages (green arrow) are then either suspended to the spreader grafts or draped over them and sutured directly to the dorsal septum. This technique opens the internal nasal valve and straightens the dorsum, although it may result in a widened dorsal aesthetic.
Contributed by MH Hohman, MD, FACS
(Click Image to Enlarge)

Additional Rhinoplasty Grafting Materials. Left: split calvarial bone. Right: auricular cartilage. For significant saddle nose deformities with cartilaginous septal insufficiency, reconstruction with a split calvarial onlay graft provides support to the nasal dorsum and tip. The graft can be placed into a tight subperiosteal pocket or fixed with screws. A substantial amount of cartilage can be obtained from the auricle without affecting its shape or function. The incision can be made anteriorly or posteriorly, and the entire concha cavum and cymba can be harvested. The cartilage is flexible, but prone to fracture and not structurally strong. As illustrated, there is a resemblance between harvested conchal cartilage and the lower lateral cartilages of the nose; this coincidence is particularly convenient for reconstruction of the nasal tip after major trauma or oncologic resection
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
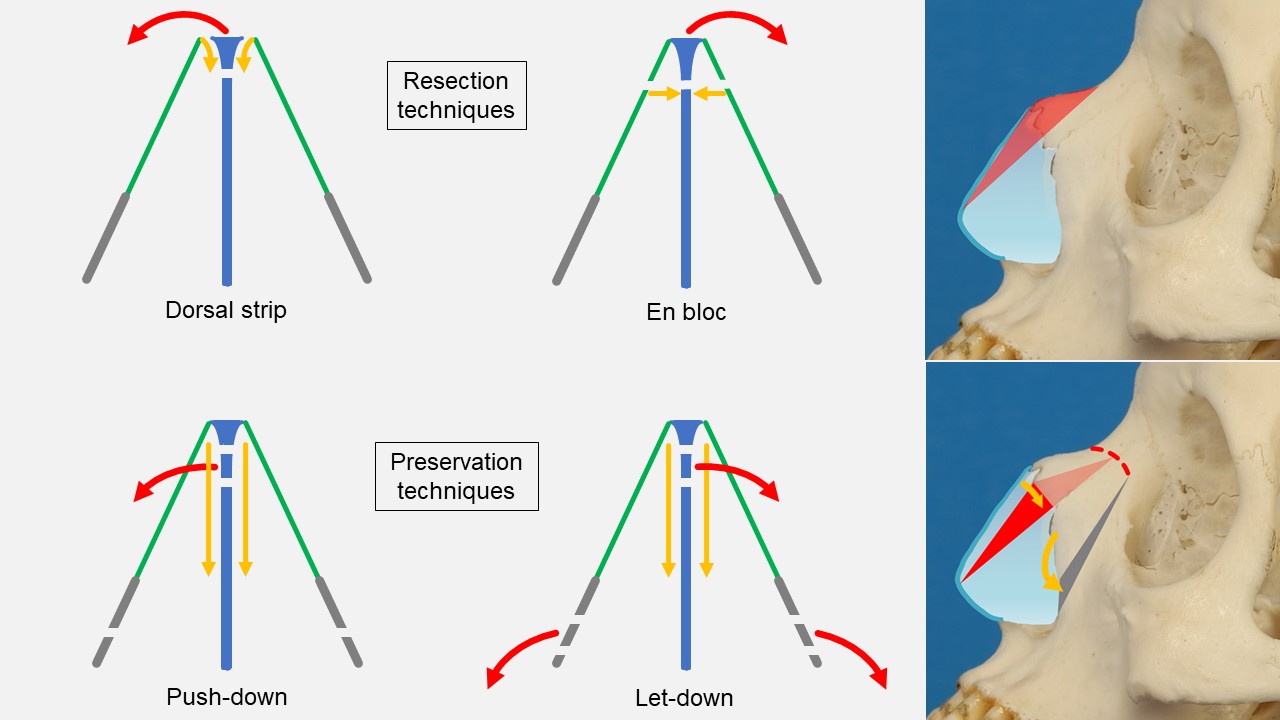
Dorsal Hump Reduction. Blue: septum. Green: upper lateral cartilage (ULC). Grey: frontal process of maxilla. The dorsal strip technique separates the ULCs from the septum, then removes a strip of dorsal septal cartilage. The bony hump is rasped or osteotomized. The ULCs are resuspended to the dorsal septum directly, using autospreader flaps, or with spreader grafts. En bloc resection of the dorsal hump that includes septum, ULCs and nasal bones is performed with a scalpel and osteotome; a resulting open roof deformity requires lateral osteotomies to medialize the lateral wall segments. The push-down technique preserves the intact nasal dorsum unit and impacts the hump downward via removal of a strip of septum just below the keystone area; lateral and transverse osteotomies allow limited descent of the bony vault. For larger humps, the let-down technique permits greater impaction; it is a variant of the push-down in which wedges of bone are removed laterally.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
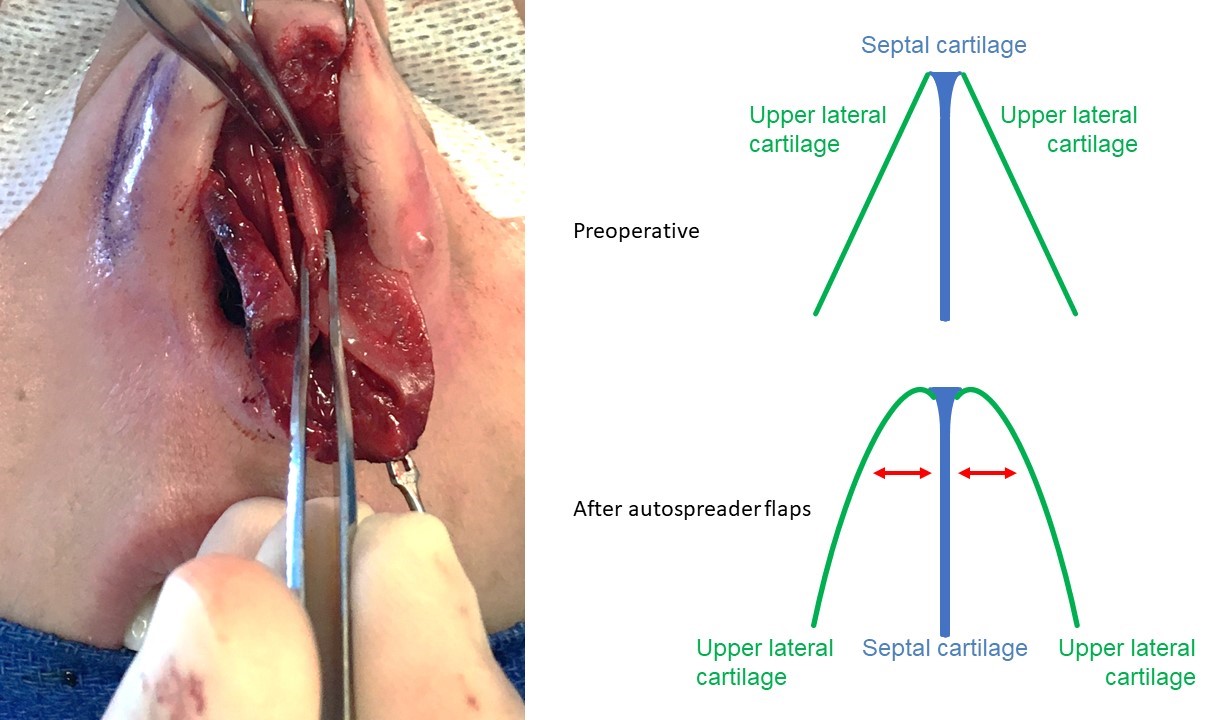
Autospreader Flaps. The photograph shows the dorsal edge of the left upper lateral cartilage being folded medially on itself prior to suspension to the dorsal septal cartilage. As shown in the schematic diagram, folding in the dorsal edge of the upper lateral cartilage causes the rest of the cartilage to bow outward, opening the internal nasal valve.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
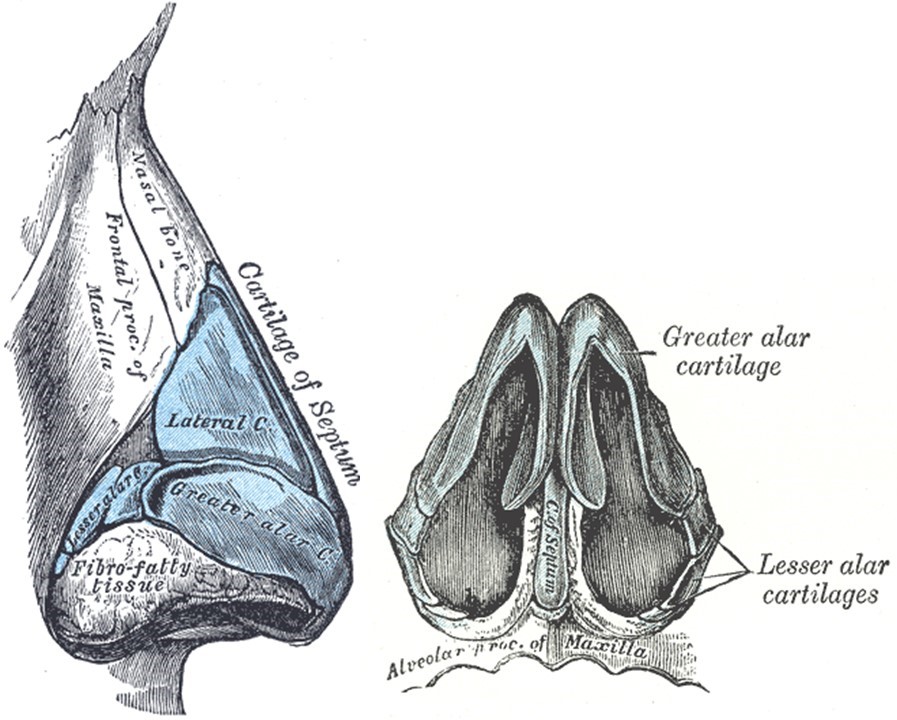
External Nasal Skeleton. The left image represents the lateral view, and the right image represents the basal view. The “greater alar cartilages” labeled in the illustration are more commonly referred to as “lower lateral cartilages,” and the “lateral cartilages” are more commonly called the “upper lateral cartilages.” Additionally, the "lesser alar cartilages" are also known as "sesamoid cartilages."
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
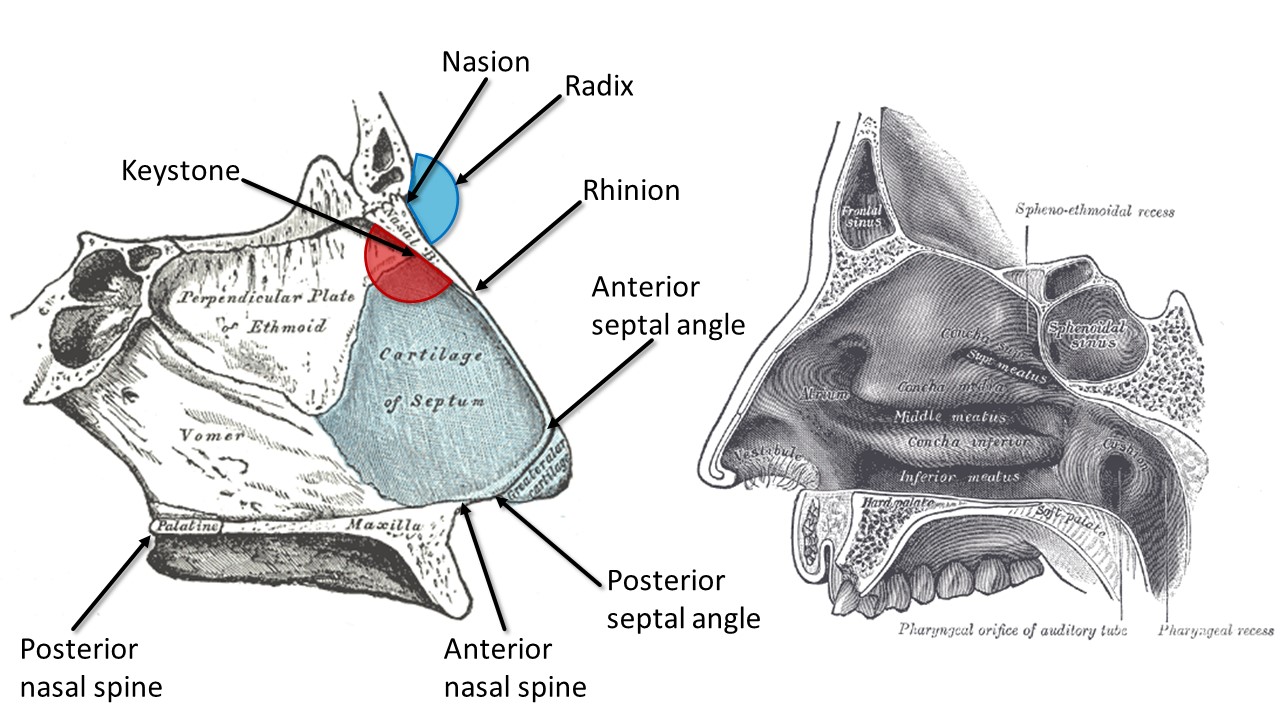
Internal Nasal Anatomy. The right image shows the lateral nasal wall and turbinates, and the left image shows the nasal septum. The blue region represents the radix, or root of the nose, while the red region highlights the keystone area, which is crucial to preserve during surgery for maintaining nasal structural support.
Contributed by MH Hohman, MD, FACS, and Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)

Roman and Greek Noses. Left: a Roman nose (Julius Caesar by Andrea di Pietro di Marco Ferrucci ca. 1512–14, Metropolitan Museum of Art, New York, USA). Right: a Greek nose (Venus de Milo by Alexandros of Antioch? ca. 2nd Century BC, Musée du Louvre, Paris, France)
Bradley Weber, Public Domain, via Wikimedia Commons and Creative Commons CC0 1.0 Universal Public Domain Dedication ("CCO 1.0 Dedication")
(Click Image to Enlarge)
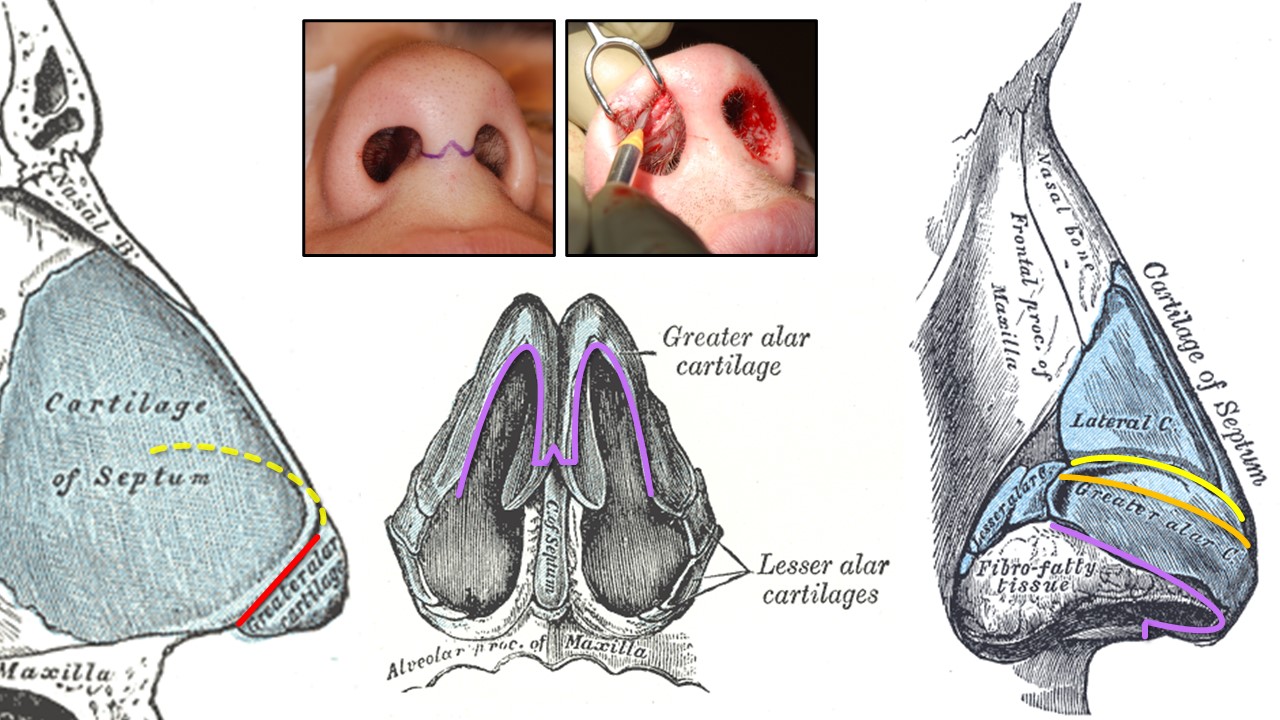
Rhinoplasty Incisions. The red line denotes a transfixion incision used for endonasal septoplasty (unilateral hemitransfixion) or tip-delivery rhinoplasty (full transfixion—through the membranous septum). Yellow indicates an intercartilaginous incision between the upper and lower lateral cartilages at the scroll, used for closed or tip-delivery rhinoplasty when made in continuity with a transfixion incision (dashed yellow line). Orange represents an intracartilaginous incision used for cephalic trimming with an intercartilaginous incision during closed rhinoplasty. Purple denotes marginal incisions along the inferior edges of the lower lateral cartilages for open rhinoplasty. This is also used for tip delivery when the transcolumellar portion is omitted. Photos illustrate the "inverted-V" transcolumellar incision used for open rhinoplasty (left) and the marginal incision for tip delivery without the transcolumellar portion (right).
Contributed by MH Hohman, MD, FACS, and Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
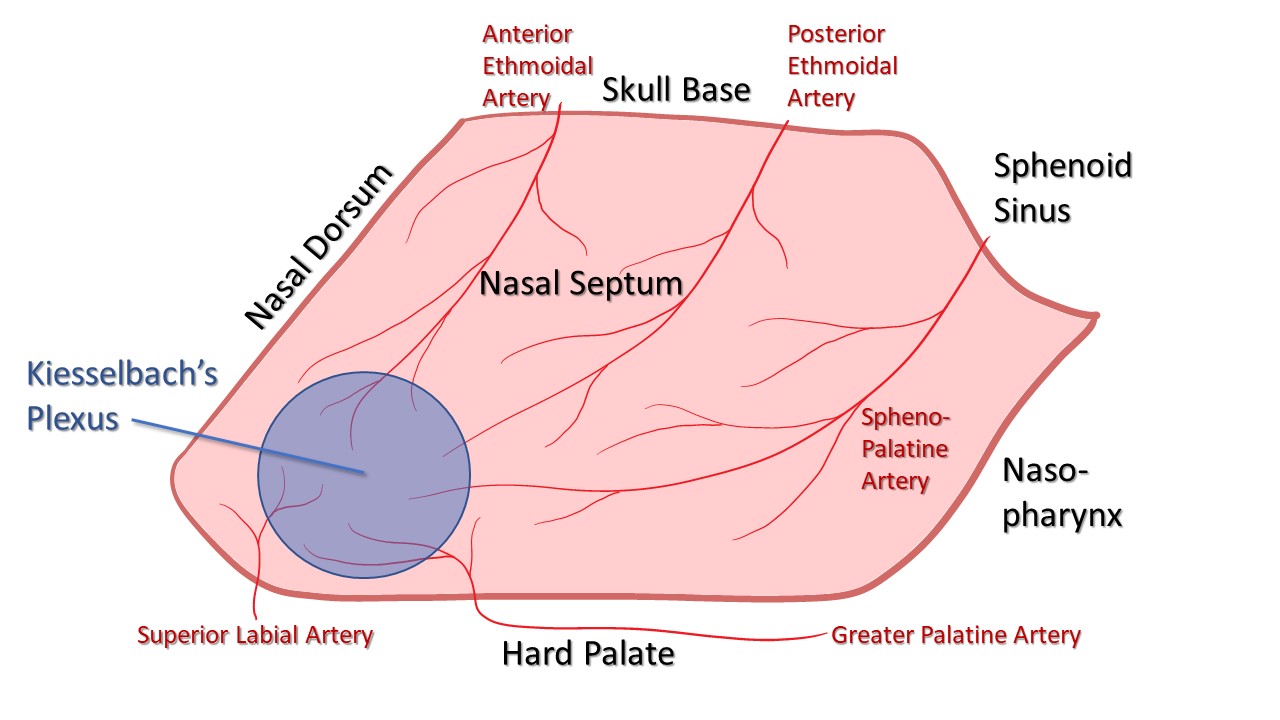
Blood Supply of the Nasal Septum. The anterior and posterior ethmoidal arteries arise from the internal carotid artery. The sphenopalatine and greater palatine arteries branch off the external carotid artery via the internal maxillary artery. The superior labial artery is a terminal branch of the facial artery. These vessels converge at the Kiesselbach plexus, which is located in the Little area on the anteroinferior aspect of the nasal septum.
Contributed by MH Hohman, MD, FACS
References
Rogers BO. John Orlando Roe--not Jacques Joseph--the father of aesthetic rhinoplasty. Aesthetic plastic surgery. 1986:10(2):63-88 [PubMed PMID: 3526833]
Bhattacharya S. Jacques Joseph: Father of modern aesthetic surgery. Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India. 2008 Oct:41(Suppl):S3-8 [PubMed PMID: 20174541]
Friedman O, Ulloa FL, Kern EB. Preservation Rhinoplasty: The Endonasal Cottle Push-Down/Let-Down Approach. Facial plastic surgery clinics of North America. 2021 Feb:29(1):67-75. doi: 10.1016/j.fsc.2020.08.006. Epub [PubMed PMID: 33220845]
Bell JW. Pioneering physician: Samuel Fomon. Archives of otolaryngology (Chicago, Ill. : 1960). 1971 Nov:94(5):387-8 [PubMed PMID: 4940045]
Constantian MB. Jack H. Sheen, M.D., 1925 to 2021. Plastic and reconstructive surgery. 2022 Sep 1:150(3):721-723. doi: 10.1097/PRS.0000000000009393. Epub 2022 Aug 30 [PubMed PMID: 36041002]
Sheen JH. Spreader graft: a method of reconstructing the roof of the middle nasal vault following rhinoplasty. Plastic and reconstructive surgery. 1984 Feb:73(2):230-9 [PubMed PMID: 6695022]
Carvalho B, Ballin AC, Becker RV, Berger CA, Hurtado JG, Mocellin M. Rhinoplasty and facial asymmetry: Analysis of subjective and anthropometric factors in the Caucasian nose. International archives of otorhinolaryngology. 2012 Oct:16(4):445-51. doi: 10.7162/S1809-97772012000400004. Epub [PubMed PMID: 25991972]
Crosara PF, Nunes FB, Rodrigues DS, Figueiredo AR, Becker HM, Becker CG, Guimarães RE. Rhinoplasty Complications and Reoperations: Systematic Review. International archives of otorhinolaryngology. 2017 Jan:21(1):97-101. doi: 10.1055/s-0036-1586489. Epub 2016 Sep 22 [PubMed PMID: 28050215]
Level 1 (high-level) evidenceRettinger G. Risks and complications in rhinoplasty. GMS current topics in otorhinolaryngology, head and neck surgery. 2007:6():Doc08 [PubMed PMID: 22073084]
Andrews JE, Jones NN, Moody MP, Vincent AG, Teixeira JC, Thomas RF, Hohman MH. Nasoseptal Surgery Outcomes in Smokers and Nonsmokers. Facial plastic surgery & aesthetic medicine. 2021 Jul-Aug:23(4):283-288. doi: 10.1089/fpsam.2020.0349. Epub 2020 Aug 26 [PubMed PMID: 32856954]
Moubayed SP, Ioannidis JPA, Saltychev M, Most SP. The 10-Item Standardized Cosmesis and Health Nasal Outcomes Survey (SCHNOS) for Functional and Cosmetic Rhinoplasty. JAMA facial plastic surgery. 2018 Jan 1:20(1):37-42. doi: 10.1001/jamafacial.2017.1083. Epub [PubMed PMID: 28880988]
Level 3 (low-level) evidenceAlsarraf R. Outcomes research in facial plastic surgery: a review and new directions. Aesthetic plastic surgery. 2000 May-Jun:24(3):192-7 [PubMed PMID: 10890946]
Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2004 Feb:130(2):157-63 [PubMed PMID: 14990910]
Level 1 (high-level) evidenceMiman MC, Deliktaş H, Ozturan O, Toplu Y, Akarçay M. Internal nasal valve: revisited with objective facts. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2006 Jan:134(1):41-7 [PubMed PMID: 16399179]
Janeke JB, Wright WK. Studies on the support of the nasal tip. Archives of otolaryngology (Chicago, Ill. : 1960). 1971 May:93(5):458-64 [PubMed PMID: 5554881]
Lindsay RW, Bhama P, Hohman M, Hadlock TA. Prospective evaluation of quality-of-life improvement after correction of the alar base in the flaccidly paralyzed face. JAMA facial plastic surgery. 2015 Mar-Apr:17(2):108-12. doi: 10.1001/jamafacial.2014.1295. Epub [PubMed PMID: 25554967]
Level 2 (mid-level) evidenceZito PM, Hohman MH, Mazzoni T. Paramedian Forehead Flaps. StatPearls. 2025 Jan:(): [PubMed PMID: 29763107]
Galarza-Paez L, Marston G, Downs BW. Anatomy, Head and Neck, Nose. StatPearls. 2024 Jan:(): [PubMed PMID: 30422465]
Dinis PB, Dinis M, Gomes A. Psychosocial consequences of nasal aesthetic and functional surgery: a controlled prospective study in an ENT setting. Rhinology. 1998 Mar:36(1):32-6 [PubMed PMID: 9569440]
Level 1 (high-level) evidenceKhan N, Rashid M, Khan I, Ur Rehman Sarwar S, Ur Rashid H, Khurshid M, Khalid Choudry U, Fatima N. Satisfaction in Patients After Rhinoplasty Using the Rhinoplasty Outcome Evaluation Questionnaire. Cureus. 2019 Jul 30:11(7):e5283. doi: 10.7759/cureus.5283. Epub 2019 Jul 30 [PubMed PMID: 31576273]
Persing S, Timberlake A, Madari S, Steinbacher D. Three-Dimensional Imaging in Rhinoplasty: A Comparison of the Simulated versus Actual Result. Aesthetic plastic surgery. 2018 Oct:42(5):1331-1335. doi: 10.1007/s00266-018-1151-9. Epub 2018 May 22 [PubMed PMID: 29789868]
Singh P, Pearlman S. Use of Computer Imaging in Rhinoplasty: A Survey of the Practices of Facial Plastic Surgeons. Aesthetic plastic surgery. 2017 Aug:41(4):898-904. doi: 10.1007/s00266-017-0858-3. Epub 2017 Apr 21 [PubMed PMID: 28432415]
Level 3 (low-level) evidenceMomeni A, Gruber RP. Primary Open Rhinoplasty. Aesthetic surgery journal. 2016 Oct:36(9):983-92. doi: 10.1093/asj/sjw093. Epub [PubMed PMID: 27651480]
Bjornsson AS, Didie ER, Phillips KA. Body dysmorphic disorder. Dialogues in clinical neuroscience. 2010:12(2):221-32 [PubMed PMID: 20623926]
Level 3 (low-level) evidenceThungana Y, Moxley K, Lachman A. Body dysmorphic disorder: A diagnostic challenge in adolescence. The South African journal of psychiatry : SAJP : the journal of the Society of Psychiatrists of South Africa. 2018:24():1114. doi: 10.4102/sajpsychiatry.v24i0.1114. Epub 2018 Jun 28 [PubMed PMID: 30263210]
Goin MK, Rees TD. A prospective study of patients' psychological reactions to rhinoplasty. Annals of plastic surgery. 1991 Sep:27(3):210-5 [PubMed PMID: 1952747]
Vasu TS, Grewal R, Doghramji K. Obstructive sleep apnea syndrome and perioperative complications: a systematic review of the literature. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2012 Apr 15:8(2):199-207. doi: 10.5664/jcsm.1784. Epub 2012 Apr 15 [PubMed PMID: 22505868]
Level 1 (high-level) evidenceSlavin SA, Goldwyn RM. The cocaine user: the potential problem patient for rhinoplasty. Plastic and reconstructive surgery. 1990 Sep:86(3):436-42 [PubMed PMID: 2385660]
Level 3 (low-level) evidenceYazici ZM, Sayin I, Erdim I, Gunes S, Kayhan FT. The effect of tobacco smoking on septoplasty outcomes: a prospective controlled study. Hippokratia. 2015 Jul-Sep:19(3):219-24 [PubMed PMID: 27418780]
Abebe W. Review of herbal medications with the potential to cause bleeding: dental implications, and risk prediction and prevention avenues. The EPMA journal. 2019 Mar:10(1):51-64. doi: 10.1007/s13167-018-0158-2. Epub 2019 Jan 8 [PubMed PMID: 30984314]
Boahene KDO. The African Rhinoplasty. Facial plastic surgery : FPS. 2020 Feb:36(1):46-52. doi: 10.1055/s-0040-1701628. Epub 2020 Mar 19 [PubMed PMID: 32191958]
Cobo R. Non-Caucasian Rhinoplasty. Clinics in plastic surgery. 2022 Jan:49(1):149-160. doi: 10.1016/j.cps.2021.07.008. Epub 2021 Oct 9 [PubMed PMID: 34782133]
Azizzadeh B, Mashkevich G. Middle Eastern rhinoplasty. Facial plastic surgery clinics of North America. 2010 Feb:18(1):201-6. doi: 10.1016/j.fsc.2009.11.013. Epub [PubMed PMID: 20206101]
Dibelius G, Hohman MH. Rhinoplasty Tip-Shaping Surgery. StatPearls. 2024 Jan:(): [PubMed PMID: 33620827]
Hosokawa Y, Miyawaki T, Omura K, Akutsu T, Kimura R, Ikezono T, Otori N. Surgical Treatment for Empty Nose Syndrome Using Autologous Dermal Fat: Evaluation of Symptomatic Improvement. Ear, nose, & throat journal. 2022 Sep 29:():1455613221130885. doi: 10.1177/01455613221130885. Epub 2022 Sep 29 [PubMed PMID: 36174975]
Jo JY, Jung KW, Kim HJ, Park SU, Park H, Ku S, Choi SS. Effect of Total Intravenous Anesthesia vs Volatile Induction With Maintenance Anesthesia on Emergence Agitation After Nasal Surgery: A Randomized Clinical Trial. JAMA otolaryngology-- head & neck surgery. 2019 Feb 1:145(2):117-123. doi: 10.1001/jamaoto.2018.3097. Epub [PubMed PMID: 30489620]
Level 1 (high-level) evidenceSagalow ES, Estephan LE, Kumar AT, Hwang M, Krein H, Heffelfinger R. Recovery Benefit With Total Intravenous Anesthesia in Patients Receiving Rhinoplasty. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2023 Sep:169(3):489-495. doi: 10.1002/ohn.319. Epub 2023 Mar 11 [PubMed PMID: 36906818]
Ghavimi MA, Taheri Talesh K, Ghoreishizadeh A, Chavoshzadeh MA, Zarandi A. Efficacy of tranexamic acid on side effects of rhinoplasty: A randomized double-blind study. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2017 Jun:45(6):897-902. doi: 10.1016/j.jcms.2017.03.001. Epub 2017 Mar 21 [PubMed PMID: 28433518]
Gutierrez RWH, Gobbo HR, Heringer LDFL. Tranexamic Acid in Patients Undergoing Rhinoplasty: An Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials. Aesthetic plastic surgery. 2024 Jun:48(11):2076-2085. doi: 10.1007/s00266-023-03768-3. Epub 2023 Dec 14 [PubMed PMID: 38097691]
Level 1 (high-level) evidenceLocketz GD, Lozada KN, Bloom JD. Tranexamic Acid in Aesthetic Facial Plastic Surgery: A Systematic Review of Evidence, Applications, and Outcomes. Aesthetic surgery journal. Open forum. 2020 Sep:2(3):ojaa029. doi: 10.1093/asjof/ojaa029. Epub 2020 Jun 14 [PubMed PMID: 33791652]
Level 1 (high-level) evidenceBian X, Liu H, Sun J, Zhang X, Li N, Chen M. Efficacy of Dexamethasone for Reducing Edema and Ecchymosis After Rhinoplasty: A Systematic Review and Meta-analysis. Aesthetic plastic surgery. 2020 Oct:44(5):1672-1684. doi: 10.1007/s00266-020-01743-w. Epub 2020 May 7 [PubMed PMID: 32383002]
Level 1 (high-level) evidenceOttoline AC, Tomita S, Marques Mda P, Felix F, Ferraiolo PN, Laurindo RS. Antibiotic prophylaxis in otolaryngologic surgery. International archives of otorhinolaryngology. 2013 Jan:17(1):85-91. doi: 10.7162/S1809-97772013000100015. Epub [PubMed PMID: 25991999]
Nuyen B, Kandathil CK, Laimi K, Rudy SF, Most SP, Saltychev M. Evaluation of Antibiotic Prophylaxis in Rhinoplasty: A Systematic Review and Meta-analysis. JAMA facial plastic surgery. 2019 Jan 1:21(1):12-17. doi: 10.1001/jamafacial.2018.1187. Epub [PubMed PMID: 30489601]
Level 1 (high-level) evidenceMowlavi A, Kim JB, Molinatti N, Saadat S, Sharifi-Amina S, Wilhelmi BJ. Understanding Why Lateral Osteotomy During Rhinoplasty Can Be Performed Safely. Eplasty. 2019:19():e9 [PubMed PMID: 30996764]
Level 3 (low-level) evidenceWick EH, Whipple ME, Hohman MH, Moe KS. Computer-Aided Rhinoplasty Using a Novel "navigated" Nasal Osteotomy Technique: A Pilot Study. The Annals of otology, rhinology, and laryngology. 2021 Oct:130(10):1148-1155. doi: 10.1177/0003489421996846. Epub 2021 Mar 1 [PubMed PMID: 33641434]
Level 3 (low-level) evidenceWilson GC, Dias L, Faris C. A Comparison of Costal Cartilage Warping Using Oblique Split vs Concentric Carving Methods. JAMA facial plastic surgery. 2017 Dec 1:19(6):484-489. doi: 10.1001/jamafacial.2017.0163. Epub [PubMed PMID: 28494068]
Wee JH, Mun SJ, Na WS, Kim H, Park JH, Kim DK, Jin HR. Autologous vs Irradiated Homologous Costal Cartilage as Graft Material in Rhinoplasty. JAMA facial plastic surgery. 2017 May 1:19(3):183-188. doi: 10.1001/jamafacial.2016.1776. Epub [PubMed PMID: 28334327]
Vila PM, Jeanpierre LM, Rizzi CJ, Yaeger LH, Chi JJ. Comparison of Autologous vs Homologous Costal Cartilage Grafts in Dorsal Augmentation Rhinoplasty: A Systematic Review and Meta-analysis. JAMA otolaryngology-- head & neck surgery. 2020 Apr 1:146(4):347-354. doi: 10.1001/jamaoto.2019.4787. Epub [PubMed PMID: 32077916]
Level 1 (high-level) evidenceKridel RW, Ashoori F, Liu ES, Hart CG. Long-term use and follow-up of irradiated homologous costal cartilage grafts in the nose. Archives of facial plastic surgery. 2009 Nov-Dec:11(6):378-94. doi: 10.1001/archfacial.2009.91. Epub [PubMed PMID: 19917899]
Christophel JJ, Hilger PA. Osseocartilaginous rib graft rhinoplasty: a stable, predictable technique for major dorsal reconstruction. Archives of facial plastic surgery. 2011 Mar-Apr:13(2):78-83. doi: 10.1001/archfacial.2010.95. Epub 2010 Nov 15 [PubMed PMID: 21079106]
Gunter JP, Friedman RM. Lateral crural strut graft: technique and clinical applications in rhinoplasty. Plastic and reconstructive surgery. 1997 Apr:99(4):943-52; discussion 953-5 [PubMed PMID: 9091939]
Ballin AC, Kim H, Chance E, Davis RE. The Articulated Alar Rim Graft: Reengineering the Conventional Alar Rim Graft for Improved Contour and Support. Facial plastic surgery : FPS. 2016 Aug:32(4):384-97. doi: 10.1055/s-0036-1585573. Epub 2016 Aug 5 [PubMed PMID: 27494582]
Weir RF. On restoring sunken noses without scarring the face. 1892. Aesthetic plastic surgery. 1988 Nov:12(4):203-6 [PubMed PMID: 3068968]
Ghavami A, Janis JE, Acikel C, Rohrich RJ. Tip shaping in primary rhinoplasty: an algorithmic approach. Plastic and reconstructive surgery. 2008 Oct:122(4):1229-1241. doi: 10.1097/PRS.0b013e31817d5f7d. Epub [PubMed PMID: 18827660]
Level 2 (mid-level) evidenceByrd HS, Andochick S, Copit S, Walton KG. Septal extension grafts: a method of controlling tip projection shape. Plastic and reconstructive surgery. 1997 Sep:100(4):999-1010 [PubMed PMID: 9290671]
Level 3 (low-level) evidenceKridel RW, Scott BA, Foda HM. The tongue-in-groove technique in septorhinoplasty. A 10-year experience. Archives of facial plastic surgery. 1999 Oct-Dec:1(4):246-56; discussion 257-8 [PubMed PMID: 10937111]
Level 3 (low-level) evidenceHohman MH, Teixeira J. Transgender Surgery of the Head and Neck. StatPearls. 2025 Jan:(): [PubMed PMID: 33760488]
Harel M, Leibou L. Interdomal Suture through a Nondelivery Endonasal Approach: A New Technique. Plastic and reconstructive surgery. Global open. 2016 Aug:4(8):e1005. doi: 10.1097/GOX.0000000000001005. Epub 2016 Aug 29 [PubMed PMID: 27622086]
GOLDMAN IB, The importance of the mesial crura in nasal-tip reconstruction. A.M.A. archives of otolaryngology. 1957 Feb; [PubMed PMID: 13393909]
Erol OO. The Turkish delight: a pliable graft for rhinoplasty. Plastic and reconstructive surgery. 2000 May:105(6):2229-41; discussion 2242-3 [PubMed PMID: 10839424]
Tasman AJ. Dorsal Augmentation-Diced Cartilage Techniques: The Diced Cartilage Glue Graft. Facial plastic surgery : FPS. 2017 Apr:33(2):179-188. doi: 10.1055/s-0037-1598185. Epub 2017 Apr 7 [PubMed PMID: 28388795]
Wright JM, Halsey JN, Rottgers SA. Dorsal Augmentation: A Review of Current Graft Options. Eplasty. 2023:23():e4 [PubMed PMID: 36817363]
Lee MR, Unger JG, Rohrich RJ. Management of the nasal dorsum in rhinoplasty: a systematic review of the literature regarding technique, outcomes, and complications. Plastic and reconstructive surgery. 2011 Nov:128(5):538e-550e. doi: 10.1097/PRS.0b013e31822b6a82. Epub [PubMed PMID: 22030516]
Level 1 (high-level) evidenceJung YG, Hong JW, Eun YG, Kim MG. Objective usefulness of thin silastic septal splints after septal surgery. American journal of rhinology & allergy. 2011 May-Jun:25(3):182-5. doi: 10.2500/ajra.2011.25.3584. Epub [PubMed PMID: 21679530]
Level 1 (high-level) evidenceAlameddine KO, Richards BA, Vyas K, Chaudhry A, Millesi E, Hamilton GS, Bite U. Evaluating the Efficacy of Liposomal Bupivacaine in Postoperative Pain Management for Rhinoplasty: A Retrospective Study. Aesthetic plastic surgery. 2024 May:48(9):1722-1727. doi: 10.1007/s00266-023-03656-w. Epub 2023 Sep 29 [PubMed PMID: 37775576]
Level 2 (mid-level) evidenceCochran CS, Landecker A. Prevention and management of rhinoplasty complications. Plastic and reconstructive surgery. 2008 Aug:122(2):60e-67e. doi: 10.1097/PRS.0b013e31817d53de. Epub [PubMed PMID: 18626319]
Lawson W, Kessler S, Biller HF. Unusual and fatal complications of rhinoplasty. Archives of otolaryngology (Chicago, Ill. : 1960). 1983 Mar:109(3):164-9 [PubMed PMID: 6337589]
Level 3 (low-level) evidenceHuang CC, Wu PW, Fu CH, Huang CC, Chang PH, Lee TJ. Impact of Psychologic Burden on Surgical Outcome in Empty Nose Syndrome. The Laryngoscope. 2021 Mar:131(3):E694-E701. doi: 10.1002/lary.28845. Epub 2020 Jul 21 [PubMed PMID: 32692881]
Sumaily IA, Hakami NA, Almutairi AD, Alsudays AA, Abulqusim EM, Abualgasem MM, Alghulikah AA, Alserhani AA. An Updated Review on Atrophic Rhinitis and Empty Nose Syndrome. Ear, nose, & throat journal. 2023 Jul 14:():1455613231185022. doi: 10.1177/01455613231185022. Epub 2023 Jul 14 [PubMed PMID: 37449389]
Downs BW, Sauder HM. Septal Perforation. StatPearls. 2024 Jan:(): [PubMed PMID: 30725893]
Pfaff MJ, Bertrand AA, Lipman KJ, Shah A, Nolan I, Krishna V, Patel H, Roostaeian J, Lee JC. The Effect of Functional Nasal Surgery on Olfactory Function. Plastic and reconstructive surgery. 2021 Mar 1:147(3):707-718. doi: 10.1097/PRS.0000000000007667. Epub [PubMed PMID: 33620941]
Kronenbuerger M, Pilgramm M. Olfactory Training. StatPearls. 2024 Jan:(): [PubMed PMID: 33620818]
Pribitkin EA, Ezzat WH. Classification and treatment of the saddle nose deformity. Otolaryngologic clinics of North America. 2009 Jun:42(3):437-61. doi: 10.1016/j.otc.2009.03.004. Epub [PubMed PMID: 19486741]
Hanasono MM, Kridel RW, Pastorek NJ, Glasgold MJ, Koch RJ. Correction of the soft tissue pollybeak using triamcinolone injection. Archives of facial plastic surgery. 2002 Jan-Mar:4(1):26-30; discussion 31 [PubMed PMID: 11843673]
Level 2 (mid-level) evidenceYoder MG, Weimert TA. Antibiotics and topical surgical preparation solution in septal surgery. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1992 Mar:106(3):243-4 [PubMed PMID: 1589214]
Rohrich RJ, Ahmad J. Rhinoplasty. Plastic and reconstructive surgery. 2011 Aug:128(2):49e-73e. doi: 10.1097/PRS.0b013e31821e7191. Epub [PubMed PMID: 21788798]
Allegranzi B, Bischoff P, de Jonge S, Kubilay NZ, Zayed B, Gomes SM, Abbas M, Atema JJ, Gans S, van Rijen M, Boermeester MA, Egger M, Kluytmans J, Pittet D, Solomkin JS, WHO Guidelines Development Group. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. The Lancet. Infectious diseases. 2016 Dec:16(12):e276-e287. doi: 10.1016/S1473-3099(16)30398-X. Epub 2016 Nov 2 [PubMed PMID: 27816413]
Level 3 (low-level) evidenceKullar R, Frisenda J, Nassif PS. The More the Merrier? Should Antibiotics be Used for Rhinoplasty and Septorhinoplasty?-A Review. Plastic and reconstructive surgery. Global open. 2018 Oct:6(10):e1972. doi: 10.1097/GOX.0000000000001972. Epub 2018 Oct 16 [PubMed PMID: 30534507]
Ishii LE, Tollefson TT, Basura GJ, Rosenfeld RM, Abramson PJ, Chaiet SR, Davis KS, Doghramji K, Farrior EH, Finestone SA, Ishman SL, Murphy RX Jr, Park JG, Setzen M, Strike DJ, Walsh SA, Warner JP, Nnacheta LC. Clinical Practice Guideline: Improving Nasal Form and Function after Rhinoplasty. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2017 Feb:156(2_suppl):S1-S30. doi: 10.1177/0194599816683153. Epub [PubMed PMID: 28145823]
Level 1 (high-level) evidenceSeverson M, Schaurich CG, Strecker-McGraw MK. Cerebrospinal Fluid Leak. StatPearls. 2024 Jan:(): [PubMed PMID: 30844184]
Motamed Shariati M, Meymane Jahromi A. Cavernous sinus and generalized venous thrombosis following rhinoplasty in a young patient. World journal of plastic surgery. 2012 Jul:1(2):107-11 [PubMed PMID: 25734052]
Marshall DR, Slattery PG. Intracranial complications of rhinoplasty. British journal of plastic surgery. 1983 Jul:36(3):342-4 [PubMed PMID: 6860864]
Bilgin E, Say MA, Baklacı D. Assessment of Patient Satisfaction With Primary Septorhinoplasty Using the Rhinoplasty Outcome Evaluation Questionnaire. Cureus. 2020 Nov 29:12(11):e11777. doi: 10.7759/cureus.11777. Epub 2020 Nov 29 [PubMed PMID: 33409024]
Randhawa PS, Watson N, Lechner M, Ritchie L, Choudhury N, Andrews PJ. The outcome of septorhinoplasty surgery on olfactory function. Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2016 Feb:41(1):15-20. doi: 10.1111/coa.12463. Epub [PubMed PMID: 25974245]
Shuaib SW, Undavia S, Lin J, Johnson CM Jr, Stupak HD. Can functional septorhinoplasty independently treat obstructive sleep apnea? Plastic and reconstructive surgery. 2015 Jun:135(6):1554-1565. doi: 10.1097/PRS.0000000000001285. Epub [PubMed PMID: 26017591]
Yamasaki A, Levesque PA, Lindsay RW. Improvement in Snoring-Related Quality-of-Life Outcomes After Functional Nasal Surgery. Facial plastic surgery & aesthetic medicine. 2020 Jan/Feb:22(1):25-35. doi: 10.1089/fpsam.2019.29002.lin. Epub [PubMed PMID: 32053426]
Level 2 (mid-level) evidenceSokoya M, Gonzalez JR, Winkler AA. Effect of allergic rhinitis on nasal obstruction outcomes after functional open septorhinoplasty. American journal of otolaryngology. 2018 May-Jun:39(3):303-306. doi: 10.1016/j.amjoto.2018.03.014. Epub 2018 Mar 5 [PubMed PMID: 29548513]
Standlee AG, Hohman MH. Evaluating the Effect of Spreader Grafting on Nasal Obstruction Using the NOSE Scale. The Annals of otology, rhinology, and laryngology. 2017 Mar:126(3):219-223. doi: 10.1177/0003489416685320. Epub 2017 Jan 5 [PubMed PMID: 28056521]
Pritikin J, Silvers S, Rosenbloom J, Davis B, Signore AD, Sedaghat AR, Tajudeen BA, Schmale I, Lyons J, Corey J, Chandra R. Temperature-controlled radiofrequency device treatment of septal swell bodies for nasal airway obstruction: An open-label, single arm multicenter study. International forum of allergy & rhinology. 2023 Oct:13(10):1915-1925. doi: 10.1002/alr.23156. Epub 2023 Mar 27 [PubMed PMID: 36908245]
Level 2 (mid-level) evidence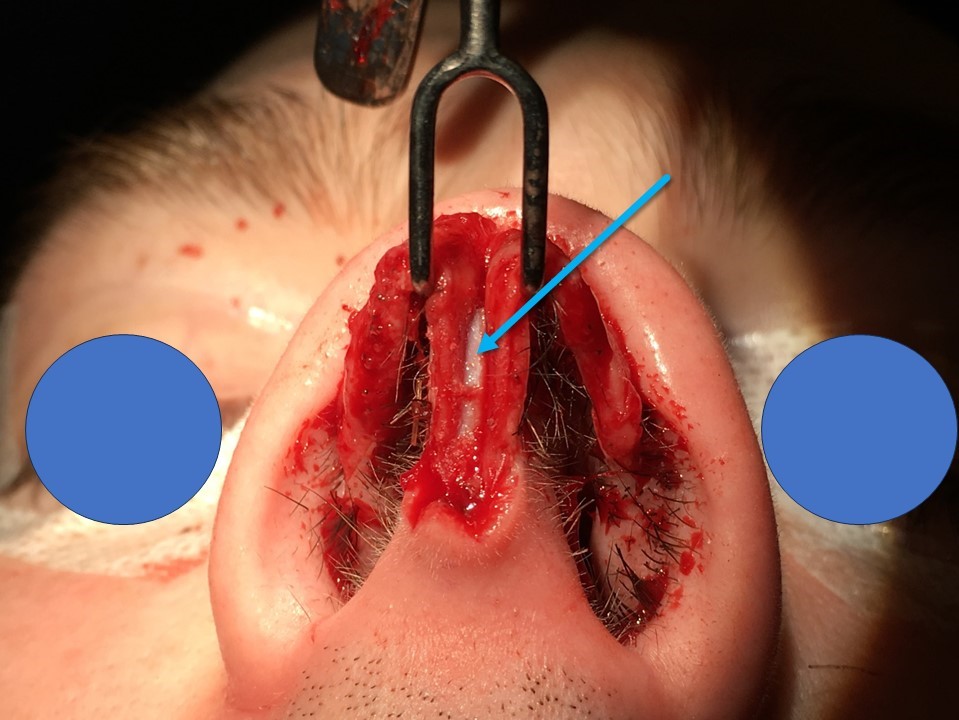
![Saddle nose, [SATA]](/pictures/getimagecontent//6506)