Introduction
From reconstructing oncologic defects to cleft palate repair and wisdom tooth extraction, the proper design and application of oral mucosal flaps are crucial for successful surgical outcomes. Oral flaps are broadly categorized into 2 types—flaps raised for surgical exposure, which are repositioned after the procedure, and flaps elevated for reconstruction, which are transferred to nearby soft tissue defects. Within these categories, various basic flap designs are tailored to specific clinical situations, each with its own advantages and limitations. Thus, clinicians must understand the different flap options, their indications and contraindications, technical considerations, and how to select the most appropriate flap for each clinical scenario to improve surgical outcomes and minimize complications.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
A thorough understanding of oral cavity anatomy is essential for effective flap design. Key structures include the gingiva, alveolar bone, mucosa, and underlying muscles. Protecting innervation, particularly branches of the trigeminal nerve, is critical to prevent postoperative complications such as numbness or paresthesia. However, preserving the blood supply to the soft tissues is paramount in flap surgery. Maintaining the integrity of the primary vascular structures, including branches of the maxillary and facial arteries derived from the external carotid system, is crucial to ensuring flap viability and successful outcomes.[1]
Many oral flaps, particularly those used for surgical access, depend on submucosal microvasculature for perfusion and are often referred to as "random pattern" flaps due to their nonspecific blood supply. In contrast, flaps containing a named vessel, such as the facial artery musculomucosal (FAMM) flap, are classified as "axial" flaps because the primary vasculature runs along the flap's long axis. Axial flaps are frequently transferred to sites not immediately adjacent to the donor location, making them "regional" flaps. This differs from local flaps, which are moved to defects bordering the donor site. An axial arterial supply may or may not have accompanying axial venous outflow. In the case of oral flaps, venous drainage typically occurs through submucosal venules. Please see StatPearls' companion resource, "Basic Flap Design," for more information.
Anatomical Structures of the Maxilla
Important anatomical structures in the maxilla include:
Maxillary artery: The maxillary artery, a terminal branch of the external carotid artery, courses posterior to the mandible, through the parotid gland, and enters the pterygopalatine fossa via the pterygomaxillary fissure (see Image. Maxillary Artery Branches).
- The mandibular segment: This is the proximal portion of the maxillary artery, and it gives off the middle meningeal and inferior alveolar arteries, among other branches.
- The pterygoid segment: This is the second portion of the maxillary artery, and it gives off multiple branches, including the buccal artery, which provides the blood supply to the buccinator musculomucosal flap.
- The pterygopalatine segment: This is the distal portion of the maxillary artery that traverses the pterygopalatine fossa and gives off the sphenopalatine, infraorbital, descending palatine, and superior alveolar arteries (see Image. Plan of Maxillary Artery Branches).
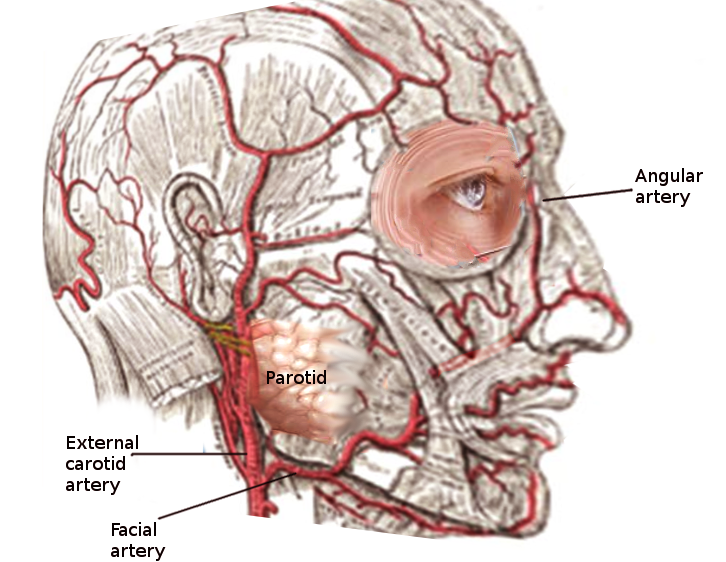
The facial artery, a proximal branch of the external carotid system, supplies the superficial structures of the face, including facial expression muscles, skin, and facial fat and fascia. This artery crosses the mandible at the gonial notch to enter the face, traveling deeply along the surfaces of the buccinator and levator anguli oris muscles as it approaches the oral commissure. At this point, it divides into the inferior and superior labial arteries, with the superior labial artery giving rise to the angular artery, which supplies the lateral nose (see Image. Anatomy of Facial Artery).
Buccinator muscle and fat pad: The buccinator muscle is located just beneath the oral mucosa, with the buccal fat pad lying deeper. Both the buccinator muscle and its overlying mucosa are essential elements of certain oral flaps, while the buccal fat pad can also be utilized in reconstructive procedures (see Image. Buccinator Muscle, Anatomy and Function).
Greater palatine neurovascular bundle: The greater palatine neurovascular bundle comprises the greater palatine nerve and artery. The nerve, descending from the sphenopalatine ganglion, supplies sensation to the hard palate and maxillary gingiva and innervates minor salivary glands in the region (see Image. Trigeminal Nerve, Nasopalatine Distribution). The bundle carries both sensory fibers from the maxillary division of the trigeminal nerve and parasympathetic fibers from the Vidian nerve.
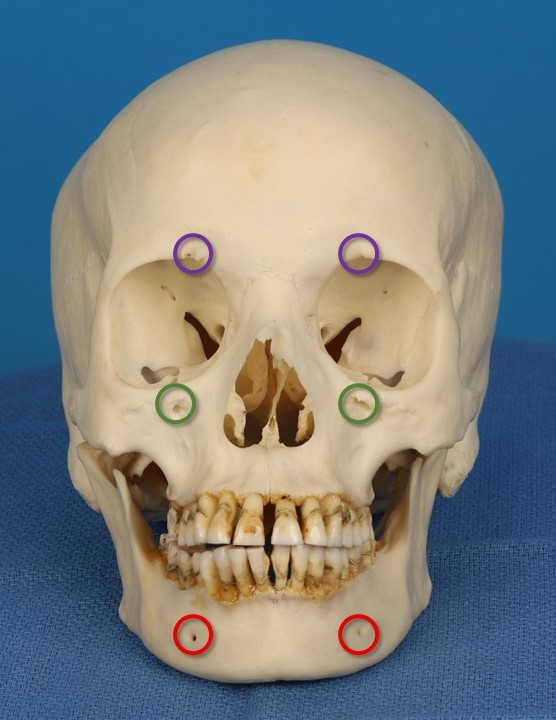
The greater palatine nerve is accompanied by the greater palatine artery, a branch of the descending palatine artery, which originates from the maxillary artery. The greater palatine neurovascular bundle traverses the pterygopalatine fossa through the greater palatine canal and emerges onto the posterolateral hard palate via the greater palatine foramen (see Image. Foramina of the Palate, Inferior View). Therefore, palatal flaps should be elevated in a way that the posterolateral aspect remains connected to the bone, preserving the neurovascular pedicle. Please see StatPearls' companion resource, "Anatomy, Head and Neck, Maxilla," for more information.
Nasopalatine nerve: This nerve is a branch of the maxillary division of the trigeminal nerve, and it emerges through the incisive foramen onto the hard palate. The nasopalatine nerve provides sensation to the mucosa and gingiva of the premaxilla and a portion of the nasal septum. If exposure to the primary palate is necessary, the neurovascular bundle can be ligated at the foramen, and the nerve typically regenerates. If permanent hypesthesia remains, it is generally not noticeable due to the small area innervated by the nerve (see Image. Nasopalatine Region Innervation). Please see StatPearls' companion resource, "Anatomy, Head and Neck, Maxilla," for more information.
Key Anatomical Structures in the Mandible
Important anatomical structures in the mandible include:
Inferior alveolar nerve: The inferior alveolar nerve (IAN) is a major branch of the mandibular division of the trigeminal nerve, encased within the bony mandibular canal, making it unlikely to be injured during soft tissue flap surgery. However, when procedures such as mandibular osteotomy, ostectomy, or complex dental extractions are planned, computed tomography (CT) of the mandible helps reveal the nerve's course and assess whether it is at risk during the planned procedure (see Image. Trigeminal Nerve, Mandibular Division). The IAN provides sensation to the teeth and gingiva of the mandible and gives rise to the mental nerve at its distal end. Please see StatPearls' companion resource, "Anatomy, Head and Neck, Mandible," for more information.
Mental nerve: The mental nerve is the distal aspect of the IAN, and it emerges from the mental foramen, typically located between the lower first and second premolars or roughly in the midpupillary line. Please see StatPearls' companion resource, "Anatomy, Head and Neck, Mandible," for more information. The mental nerve provides sensation to the anterior mandibular gingiva, chin, and lower lip. Injury to the mental nerve can lead to drooling, as affected patients may be unable to sense saliva or other liquids passing over the lower lip (see Image. Trigeminal Foramina of the Face).
Lingual nerve: The lingual nerve is a branch of the mandibular division of the trigeminal nerve, and it travels anterior to the IAN and runs along the medial aspect of the mandible, between the periosteum and the gingiva. This nerve provides sensation to the mucosa overlying the medial mandible, particularly in the region of the third molars. This positioning places the nerve at risk of injury if mucoperiosteal flaps are raised carelessly during third molar extractions.[2] The nerve continues anteromedially within the floor of the mouth, crossing beneath the submandibular duct before reaching the ventral aspect of the tongue (see Image. Trigeminal Nerve). The submandibular ganglion, which is attached to the lingual nerve, supplies parasympathetic innervation to the submandibular gland. The lingual nerve also innervates the sublingual salivary glands.
Long buccal nerve: This nerve is also a branch of the mandibular division of the trigeminal nerve and runs along the lateral aspect of the mandible. The superficial branch traverses the buccinator muscle, providing sensation to the skin of the cheek, and it anastomoses with the buccal branch of the facial nerve. The deep branch runs between the periosteum and mucosa of the posterolateral mandible, supplying sensation to the buccal gingiva near the second and third mandibular molars. When exposing the mandible, such as with an envelope flap, careful elevation of the mucoperiosteum as a unit helps preserve the integrity of the nerve's branches. Although hypesthesia resulting from injury to the buccal nerve is possible, it is typically well tolerated.[3]
Indications
Local and regional flaps in the oral cavity are used for various indications, including:
- Extraction of impacted teeth
- Apicoectomy
- Periodontal surgical access
- Implant placement
- Access and reconstruction after cyst or tumor removal
- Management of oroantral communications
- Repair of traumatic tissue defects
- Cleft palate repair
In addition to the specific clinical context, oral flaps serve 2 primary purposes—to provide greater access and exposure than a simple incision allows and to supply soft tissue for reconstructing defects.
Contraindications
Contraindications to the use of local and regional flaps in the oral cavity include:
- Inability to adhere to the postoperative care regimen, particularly for interpolated flaps with pedicles at risk of being bitten.
- Ongoing use of tobacco or vasoconstrictive drugs (such as nicotine and cocaine), which can impair microvascular perfusion.
- Scarring or fibrosis at the planned flap donor site, especially following prior radiation therapy.
- Insufficient tissue for transfer, such as in cases of previous trauma during flap harvest.
- Active infection at the operative site.
- Other medical comorbidities that may impair the patient's ability to tolerate surgery.
Equipment
The following equipment is essential for performing oral flap surgeries:
- Scalpel with blades (commonly, #15 blade on a #3 or #7 Bard-Parker handle)
- Monopolar electrocautery with insulated needle tip
- Periosteal elevators (eg, Molt #9 and Freer)
- Hemostats
- Surgical scissors (eg, Metzenbaum and iris)
- Needle holders (eg, Halsey and Heaney)
- Suture (eg, 3-0 and 4-0 chromic gut or polyglactin)
- Suction apparatus (Yankauer or Goodhill)
- High-capacity syringes and normal saline for irrigation
- Retractors (eg, Minnesota and Langenbeck)
- Tissue forceps (eg, De Bakey and Gerald)
- 22-Gauge angiocatheter for parotid duct cannulation, if necessary
- Doppler probe for identification of the arterial pedicle, if necessary [4]
Personnel
A skilled surgical team is necessary for successful flap surgery, typically including:
- Oral and maxillofacial surgeon, periodontist, endodontist, or otolaryngologist
- Surgical assistants
- Anesthesia clinicians, if sedation is required
- Operating room nurse or dental assistant
Preparation
Preparing for oral flap surgery requires a detailed understanding of the relevant regional anatomy and a thorough knowledge of the patient's medical and dental history. The physical examination is critical in determining the appropriate flap, especially when reconstructive surgery is needed. Preoperative imaging, such as CT scans or panoramic x-rays, may be required for certain pathologies. After obtaining written informed consent and addressing all of the patient's questions, local anesthesia is administered and given time to take effect.[5]
Lidocaine typically takes effect within 1 to 2 minutes when infiltrated locally, but it may require several minutes if injected as a regional block. Bupivacaine, on the other hand, may take a few minutes to achieve anesthesia even when infiltrated locally, but its effects last longer than those of lidocaine.[6] Articaine is another commonly used option for intraoral local anesthesia, with a faster onset than lidocaine (<1 minute) and a longer duration (4 hours versus 3 hours).[7] Regardless of the local anesthetic agent chosen, epinephrine typically takes 7 to 33 minutes to induce sufficient vasoconstriction to effectively reduce bleeding.[8]
Technique or Treatment
Essential considerations for oral flaps include:
- The size of the planned flap relative to the exposure needed or the defect to be reconstructed should be double-checked before making any incisions.
- The flap should have a base broader than its height when using a random pattern blood supply. This ensures adequate perfusion and venous drainage, helps prevent ischemic necrosis, and improves surgical exposure.[2]
- Flaps for exposure should have incisions made on healthy bone to reduce the risk of wound dehiscence after closure.
- When mucoperiosteal flaps are raised in the correct plane, the periosteum is included, thereby improving their strength and perfusion.
- Trauma to the underlying bone and disruption of periosteal microvasculature during flap elevation may lead to bone resorption and necrosis.[9]
- The interdental papillae should be spared, and incisions over bony prominences should be avoided to ensure a tension-free flap closure, thereby reducing the risks of necrosis and dehiscence.[2]
- Vital anatomical structures in the area should be protected and, if necessary, identified visually during surgery.
Flaps for Surgical Exposure
Envelope flap: The envelope flap is a widely used design that involves a horizontal incision along the gingival margin, including the interdental papillae.[10] This flap is indicated for minor surgical procedures, such as tooth extractions and small bone grafts. This flap is particularly advantageous in palate surgery due to the concavity of the bone (see Image. Envelope Flap).[2]
The technical considerations and risks associated with this flap are listed below.
- Technique
- A horizontal incision is made along the gingival margin, extending to adjacent teeth if necessary.
- The mucoperiosteal flap is then elevated using a periosteal elevator, exposing the surgical site.
- The flap is repositioned and secured with interrupted sutures after the procedure.
- Risks
- The envelope flap is not ideal for exposing large areas or multiple teeth.
- This flap may lead to a deeper probing depth, as its design restricts thorough postoperative cleaning of the area.
- A risk of flap tearing during retraction is present.[11]
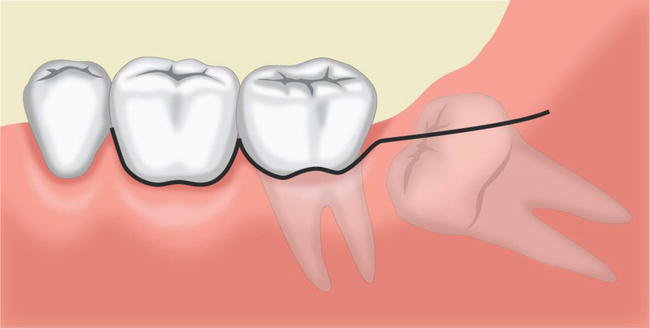
Two-sided (triangular) flap: The 2-sided flap combines a horizontal incision, similar to the envelope flap, with a vertical releasing incision, thereby providing greater surgical access and tissue mobility (see Image. Two-Sided Flap).[2]
The technical considerations and risks associated with this flap are listed below.
- Technique
- A horizontal incision is made along the gingival margin.
- A vertical releasing incision is then made at one end of the horizontal incision.
- A mucoperiosteal flap is elevated to expose the surgical area.
- The flap is repositioned and secured with sutures when the procedure is complete.
- Risks
- Uneven tension distribution can lead to wound dehiscence.
- Improperly raised mucoperiosteal flaps are at risk of tearing.[11]
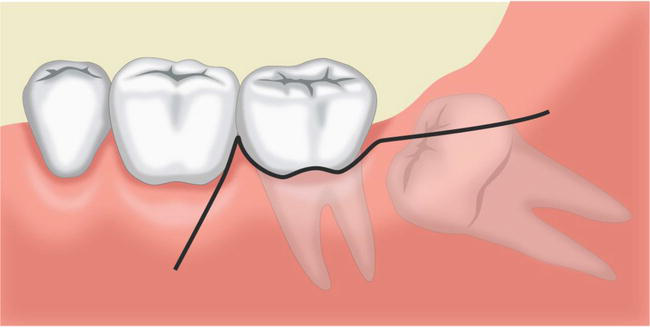
Three-sided (trapezoidal) flap: The 3-sided flap offers greater surgical access than the 2-sided flap, making it suitable for more extensive procedures. This involves a horizontal incision and 2 vertical releasing incisions (see Image. Three-Sided Flap).[2]
- Technique
- A horizontal incision is made along the gingival margin.
- Two vertical releasing incisions are created, 1 at each end of the horizontal incision.
- The mucoperiosteal flap is elevated to provide maximum exposure.
- The flap is repositioned and secured with sutures after the surgery.
- Risks
- This flap carries a higher risk of compromising blood supply, increasing the potential for necrosis due to the greater number of incisions compared to 2-sided or envelope flaps.[11]
- Postoperative swelling and discomfort are typically more pronounced than those associated with 2-sided or envelope flaps.
Semilunar flap: The semilunar flap has been used for procedures involving the apical region of the teeth, such as apicoectomy and removal of impacted anterior maxillary teeth.[12] This flap features a crescentic incision in the mucosa, away from the gingival margin, which may improve the cosmesis of the scar (see Image. Semilunar Flap). However, the semilunar flap has largely fallen out of favor due to its limited exposure to more extensive procedures and a high risk of complications, particularly in patients with excellent oral hygiene postoperatively.
- Technique
- A curvilinear incision is created in the mucosa, positioned away from the gingival margin, with the apex of the flap directed toward the crowns of the teeth.
- A mucoperiosteal flap is elevated to expose the apical region.
- The flap is repositioned and secured with sutures following the surgical procedure.
- Risks
- This approach offers limited exposure to the periapical area, making it unsuitable for extensive procedures.
- An increased risk of dehiscence of the incision line relative to other flaps is present, potentially leading to delayed healing and scarring.[12]
Luebke-Ochsenbein flap: The Luebke-Ochsenbein flap is primarily used in periodontal surgery and involves a submarginal incision that preserves the gingival margin (see Image. Luebke-Ochsenbein Flap).[13]
- Technique
- A horizontal submarginal incision is made approximately 3 mm away from and parallel to the gingival margin, avoiding the gingival crevice.
- Two vertical releasing incisions are made—one at each end of the horizontal incision.
- A mucoperiosteal flap is elevated to gain access to the underlying structures.
- The flap is then repositioned and sutured after completing the surgical procedures.
- Risks
- This flap is unsuitable for areas with insufficient attached gingiva.
- Gingival recession may occur if the flap is not designed correctly.
- The flap may scar and shrink postoperatively.
- The risk of flap necrosis is increased due to the number of incisions required, which may compromise the blood supply.[12]
Flaps for Reconstruction
Buccal advancement flap: The buccal advancement flap commonly involves a broad-based 2- or 3-sided flap to cover defects or augment soft tissue by advancing the buccal mucosa (see Image. Buccal Advancement Flap).[14]
- Technique
- An incision is made in the buccal mucosa.
- The flap is elevated in a submucosal plane, ensuring the base remains attached for adequate blood supply.
- The flap is advanced to cover the defect or augment tissue, then secured with sutures.
- Risks
- The advancement of buccal mucosa may efface the vestibule, potentially affecting aesthetics or the fit of prostheses.
- Excessive advancement may cause tension, leading to flap necrosis or dehiscence.
- This technique may be challenging in patients with severe periodontal disease.[15]
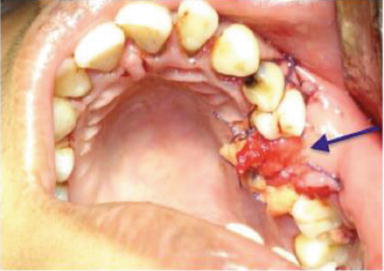
Buccal fat pad with buccal advancement flap: Utilizing the buccal fat pad in combination with a buccal advancement flap is particularly effective for closing large oroantral communications or defects. This technique provides more bulk than the flap alone and enhances blood flow to the flap (see Image. Buccal Fat Pad With Buccal Advancement Flap).[15]
- Technique
- An incision is made in the buccal mucosa, and the flap is elevated in a submucosal plane.
- The buccal fat pad is carefully mobilized and advanced into the defect. Optimal access is achieved when the incision is placed superior to the papilla of the parotid duct (see Image. Buccal Fat Pad).
- The buccal fat pad and flap are sutured in place with a layered closure.
- Risks
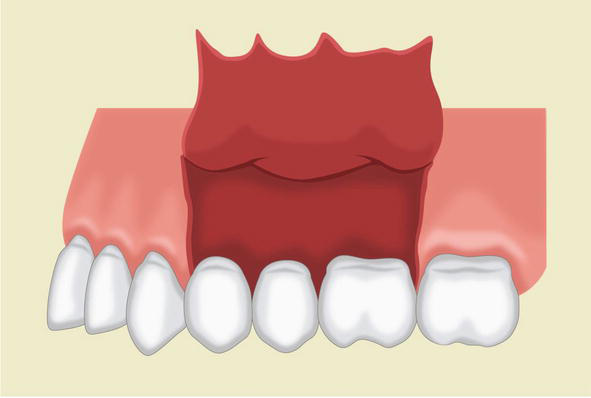
Palatal advancement flaps: Palatal advancement flaps are typically used for maxillary reconstruction, particularly for repairing cleft palate defects and closing oroantral communications (see Image. Palatal Advancement Flap).[15]
- Technique
- An incision is made along the palatal mucosa at the junction of the superior alveolar ridge and the hard palate.
- Another incision is made along the margin of the cleft or at the desired location of the medial extent of the flap. Depending upon the flap design, these incisions may or may not connect. If the incisions connect, the vascular pedicle runs through the greater palatine foramen; if not, the flap is bipedicled.
- The flap is elevated carefully in a subperiosteal plane to avoid damage to the palatine vessels.
- The flap is advanced to cover and secure the defect and then sutured into place.
- Transposition flaps can be used in the soft palate to close a cleft or elongate the soft palate using the double-opposing Z-plasty technique described by Furlow.[17] This technique uses posteriorly based flaps containing muscle and mucosa, while the anteriorly based flaps contain only mucosa. This configuration facilitates the reconstruction of the levator sling and enhances palatal mobility.
- Risks
- The risk of necrosis is increased due to limited vascularity, especially if the greater palatine vessels are damaged.
- Postoperative pain and difficulty maintaining oral hygiene can arise, as bare bone is often left exposed after palatal flap transfer.
- These flaps are prone to dehiscence when closed under tension, while closure without tension can be difficult, particularly with wide defects.[15]
Buccinator flap: The buccinator flap, first described by Bozola et al, contains the buccinator muscle and overlying buccal mucosa, with its pedicle based posteriorly on the buccal artery—a branch of the maxillary artery.[18] This flap is commonly used to reconstruct intraoral defects resulting from oncologic resections or osteomyelitis or to repair a cleft palate.[19] Due to its axial blood supply, the buccinator flap allows for the transfer of a larger volume of tissue, making it suitable for reconstructing larger defects compared to random pattern flaps, such as buccal advancement flaps.
- Technique
- A Doppler probe is used to identify the buccal artery, and the parotid duct is cannulated to prevent damage to these structures.
- The flap is outlined and incised, with the anterior extent positioned just posterior to the oral commissure if that length is necessary, and the upper extent placed just below the parotid duct.
- The inferior incision may be as low as necessary, but care should be taken to avoid effacing the gingivobuccal sulcus if the flap is too broad.
- The flap is elevated from the underlying buccopharyngeal fascia and may include fat, as needed. Elevation proceeds from anterior to posterior, ensuring the buccal artery and venous plexus of the buccinator are preserved.
- If the exposed pedicle could pose a problem due to its course, the posterior mucosa and muscle may be divided, creating a narrower pedicle that can be tunneled instead of crossing over the teeth.
- Once the flap is transposed into the defect, the donor site can be closed primarily and allowed to heal by secondary intention, or a combination of both approaches may be used.[19]
- Risks
- Excessive tension or torsion on the pedicle may lead to flap necrosis. Injury to the buccal artery or venous drainage can also compromise the flap's survival.
- Violation of the buccopharyngeal fascia during flap elevation may cause fat herniation into the mouth.
- The parotid duct is at risk for injury during flap elevation.
Facial artery musculomucosal flap: The FAMM flap, developed by Pribaz in 1992, is an alternative to the buccinator flap for significant soft tissue reconstruction.[20] The flap is commonly used for reconstructing pharyngeal, palatal, labial, lingual, and eyelid defects.[21] The blood supply for the FAMM flap is derived from the facial artery, which ascends lateral to the oral commissure and approaches the lateral aspect of the nose. Due to excellent collateral blood flow in this area, the flap can be harvested with either a superiorly or inferiorly based pedicle, utilizing retrograde or anterograde flow within the facial artery, respectively. This provides greater flexibility in design compared to the buccinator flap. While the buccinator flap is oriented horizontally, the FAMM flap is oriented vertically.
- Technique
- The facial artery is identified using a Doppler probe to ensure it is incorporated into the flap.[22]
- The anterior extent of the flap is marked at least 1 cm from the oral commissure to prevent distortion, while the posterior extent is marked anterior to the parotid duct.
- Once the location of the pedicle is determined based on the geometry of the planned transposition, either the superior or inferior aspect of the flap is incised, and the facial artery is ligated accordingly.
- The flap is elevated from distal to proximal, deep to the facial artery, with arterial branches (eg, superior and inferior labial and angular) divided as necessary. The buccinator muscle is included in the flap.
- The flap may be inset as an interpolated flap, with planned pedicle division 2 to 4 weeks later, or it may be inset via a tunnel in a single stage, similar to the buccinator flap.
- After the flap is transposed into the defect, the donor site can be closed primarily or covered with a skin graft.
- Risks
- Excessive tension or torsion on the pedicle may lead to flap necrosis. Injury to the facial artery or disruption of submucosal venous drainage can also result in necrosis.
- The parotid duct is at risk of injury during flap elevation.
- Harvesting the flap too close to the oral commissure may cause noticeable soft tissue distortion, which can affect cosmesis.
Complications
Flap necrosis, resulting from compromised blood supply or infection, can lead to wound dehiscence, especially if the flap is transferred under tension or if suturing is insufficient to secure the flap.[2] Similarly, positioning an interpolated vascular pedicle, such as in a buccinator or FAMM flap, near teeth may cause it to be bitten, leading to significant intraoral bleeding and flap loss. Overly aggressive flap elevation can also result in bone resorption due to the loss of periosteal perfusion, triggering osteoclastic activity.[23]
Many systemic conditions, including diabetes, peripheral vascular disease, and tobacco use disorder, negatively affect flap perfusion and should be optimized, when possible, before surgery.[24][25] Additionally, poor flap design, such as placing incisions across the planned blood supply, can also predispose a flap to necrosis.
Postoperative infection, often resulting from poor oral hygiene or immunocompromise, can significantly impair healing.[5] An ongoing infection at the site of the planned flap is a contraindication for proceeding with surgery. Nerve damage, which leads to numbness or paresthesia, is a risk, particularly in procedures occurring near the mental, long buccal, or IANs. Inappropriate flap design or execution may also result in undesirable scarring or aesthetic deformities.[26] Meticulous planning, precise surgical execution, and attentive postoperative care are vital to minimizing complications and achieving successful surgical outcomes.[5]
Clinical Significance
Oral flap design is critical in diverse surgical contexts, including oncologic reconstruction, cleft palate repair, and wisdom tooth extraction. A well-designed flap in intraoral surgery improves surgical outcomes by enhancing access to operative sites, preserving vital structures, and promoting healing. Additionally, effective flap design minimizes postoperative complications, including infection, dehiscence, and scarring.[26] Mastery of diverse flap techniques enables clinicians to customize their approach to each patient’s unique needs, thereby enhancing surgical outcomes and improving patient satisfaction.
Enhancing Healthcare Team Outcomes
The use of oral flaps in intraoral surgery necessitates an interprofessional approach to deliver patient-centered care and achieve optimal results. Physicians and advanced practitioners, such as oral surgeons and otolaryngologists, take the lead in selecting appropriate flap designs, performing surgical techniques, and managing complications. Nurses are critical in preoperative preparation, intraoperative assistance, and postoperative monitoring, emphasizing wound care and patient education to support recovery. Pharmacists enhance outcomes by optimizing medication regimens, including antibiotics and pain management, to ensure patient safety and minimize infection risks. The collaboration of these specialized professionals ensures surgical success and comprehensive patient care throughout the treatment process.
Interprofessional communication and care coordination are essential, especially in complex cases such as oral cancer resection, where prolonged recovery necessitates collaboration beyond the surgical team. Effective communication among surgeons, anesthesiologists, operating room staff, and outpatient caregivers ensures continuity of care and holistic management of patient needs. Postoperative recovery often involves speech-language pathologists for swallowing rehabilitation and outpatient nurses for wound care and progress monitoring. Interprofessional healthcare teams can enhance patient outcomes, minimize complications, and optimize team performance by fostering clear communication and shared responsibility. This collaborative approach highlights the value of integrating diverse expertise to achieve excellence in patient-centered care for oral flap designs.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
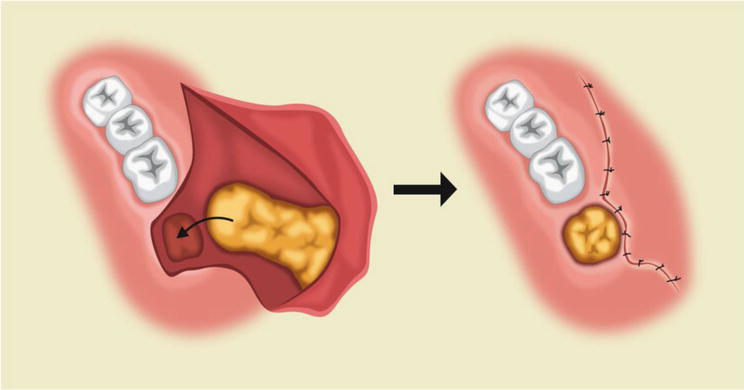
Buccal Fat Pad With Buccal Advancement Flap. The combination of the buccal fat pad and buccal advancement flap is highly effective for closing large oroantral communications or defects. This technique provides greater bulk than a buccal advancement flap alone, while the fat pad also enhances blood flow to the flap.
Contributed by R Alfotawi, MD
(Click Image to Enlarge)
(Click Image to Enlarge)
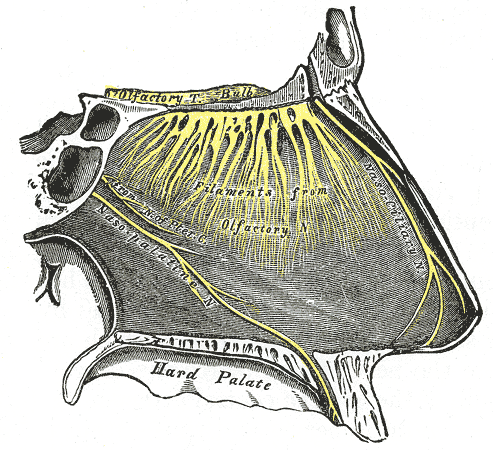
Nasopalatine Region Innervation. This image illustrates the innervation of the nasopalatine region, including the olfactory tract, bulb, and filaments. This image also highlights the nasociliary, nasopalatine, and pterygoid canal nerves. The nasopalatine nerve is shown entering the hard palate anteriorly.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
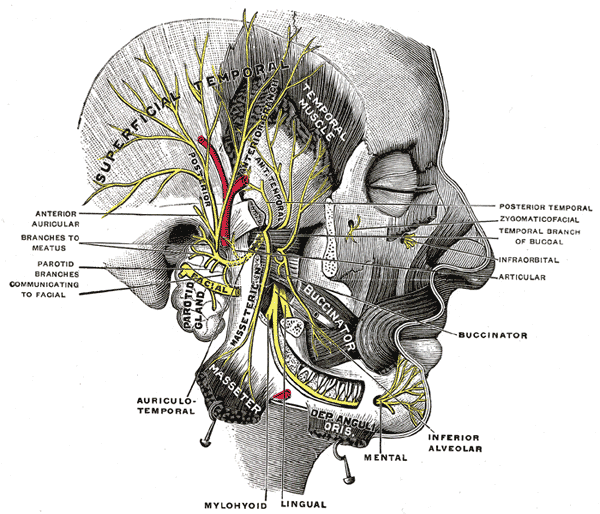
Trigeminal Nerve, Mandibular Division. The inferior alveolar nerve (IAN), a major branch of the mandibular division of the trigeminal nerve, is enclosed within the bony mandibular canal.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
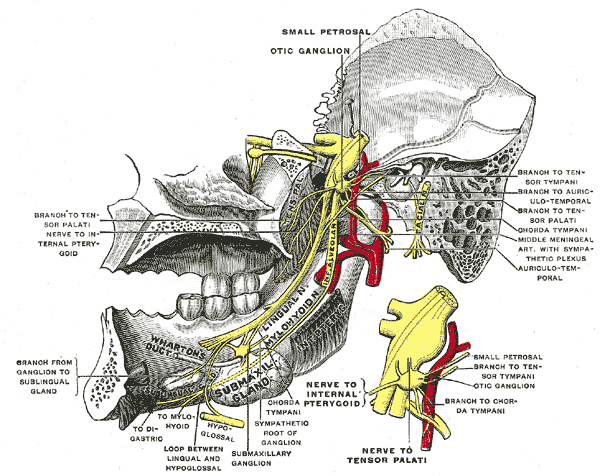
Trigeminal Nerve. The image shows the mandibular division of the trigeminal nerve from the midline. The small figure provides an enlarged view of the otic ganglion.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
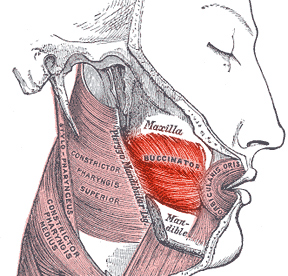
Buccinator Muscle, Anatomy and Function. The buccinator muscle maintains cheek tone during mastication. The muscle is innervated on its superficial surface by the facial nerve and receives blood supply from the facial artery. The muscle, along with its underlying mucosa, is often used in buccal artery and facial artery musculomucosal flaps for oral reconstruction.
Havaska, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)

Trigeminal Nerve, Nasopalatine Distribution. This image illustrates the course of the trigeminal nerve in the nasopalatine region, highlighting the termination of the nasopalatine nerve, the sphenopalatine ganglion, and its branches.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
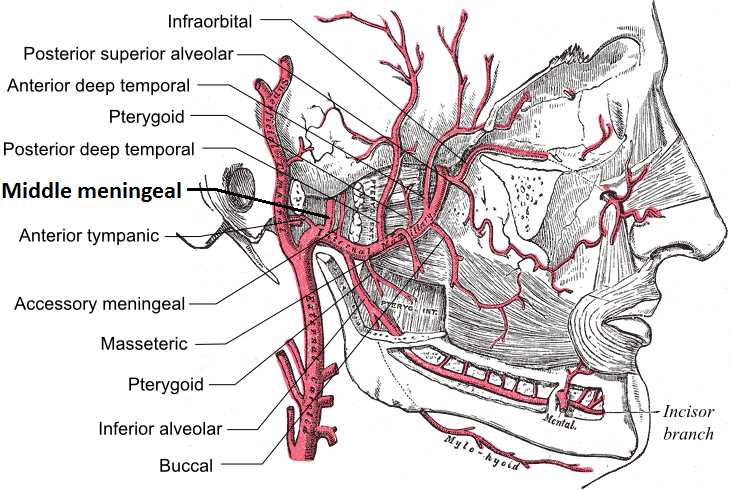
Maxillary Artery Branches. The maxillary artery, a terminal branch of the external carotid artery, runs posterior to the mandible, passes through the parotid gland, and enters the pterygopalatine fossa via the pterygomaxillary fissure.
Mikael Häggström, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
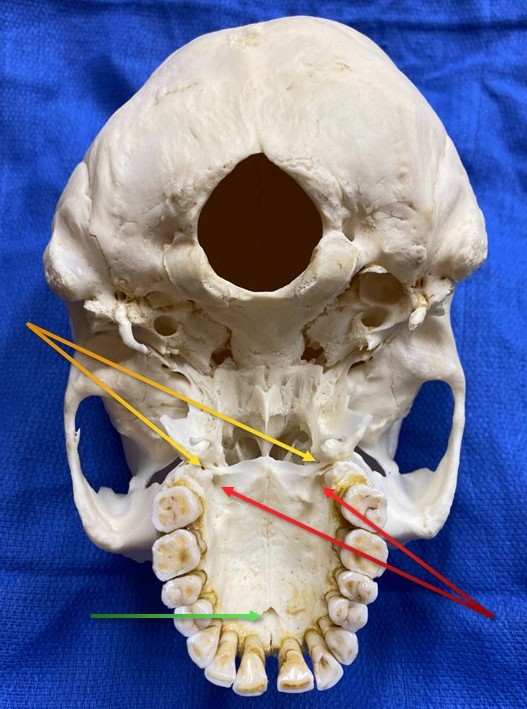
Foramina of the Palate, Inferior View. Red arrows indicate the greater palatine foramina, which transmits the descending palatine vessels and greater palatine nerves. Yellow arrows highlight the lesser palatine foramina (2 on each side), which transmit the lesser palatine nerves and vessels. The green arrow points to the incisive foramen, which separates the primary and secondary palates and transmits the nasopalatine nerve along with a communicating branch between the greater palatine and sphenopalatine arteries.
Contributed by MH Hohman, MD, FACS
(Click Image to Enlarge)
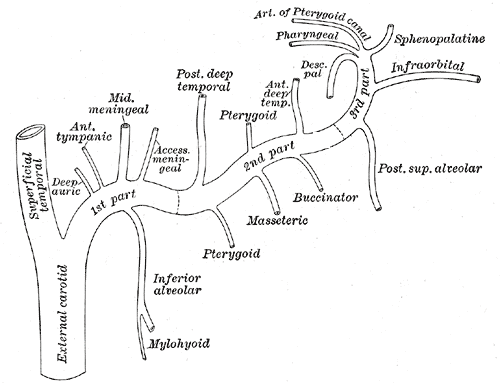
Plan of Maxillary Artery Branches. The mandibular segment (proximal portion) of the maxillary artery gives off the middle meningeal and inferior alveolar arteries. The pterygoid segment (second portion) gives off multiple branches, including the buccal artery, which supplies blood to the buccinator musculomucosal flap. The pterygopalatine segment (final portion) runs through the pterygopalatine fossa, giving off the sphenopalatine artery, infraorbital artery, superior alveolar arteries, and descending palatine artery.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Lee HJ, Won SY, O J, Hu KS, Mun SY, Yang HM, Kim HJ. The facial artery: A Comprehensive Anatomical Review. Clinical anatomy (New York, N.Y.). 2018 Jan:31(1):99-108. doi: 10.1002/ca.23007. Epub 2017 Nov 16 [PubMed PMID: 29086435]
Jephcott A. The surgical management of the oral soft tissues: 1. Flap design. Dental update. 2007 Oct:34(8):518-20, 522 [PubMed PMID: 18019490]
Takezawa K, Ghabriel M, Townsend G. The course and distribution of the buccal nerve: clinical relevance in dentistry. Australian dental journal. 2018 Mar:63(1):66-71. doi: 10.1111/adj.12543. Epub 2017 Sep 8 [PubMed PMID: 28646596]
Jephcott A. The surgical management of the oral soft tissues: 2. Surgical technique. Dental update. 2007 Nov:34(9):590-2, 594 [PubMed PMID: 18087931]
Dolan S, Rae E. What are the implications of flap design on post-operative complications when carrying out third molar surgery? Evidence-based dentistry. 2021 Jan:22(3):104-105. doi: 10.1038/s41432-021-0198-7. Epub [PubMed PMID: 34561661]
Velioglu O, Calis AS, Koca H, Velioglu E. Bupivacaine vs. lidocaine: a comparison of local anesthetic efficacy in impacted third molar surgery. Clinical oral investigations. 2020 Oct:24(10):3539-3546. doi: 10.1007/s00784-020-03224-5. Epub 2020 Feb 17 [PubMed PMID: 32065309]
Jain NK, John RR. Anesthetic efficacy of 4% articaine versus 2% lignocaine during the surgical removal of the third molar: A comparative prospective study. Anesthesia, essays and researches. 2016 May-Aug:10(2):356-61. doi: 10.4103/0259-1162.171445. Epub [PubMed PMID: 27212774]
Level 2 (mid-level) evidenceBajwa MS, Bashir MM, Bajwa MH, Iqbal Z, Salahuddin MA, Hussain A, Shahzad F. How long to wait after local infiltration anaesthesia: systematic review. BJS open. 2023 Sep 5:7(5):. doi: 10.1093/bjsopen/zrad089. Epub [PubMed PMID: 37768699]
Level 1 (high-level) evidenceSaleh MHA, Couso-Queiruga E, Ravidà A, Dukka H, Paiva De Andrade N, Ou A, Wang HL. Impact of the periodontal phenotype in premolar and molar sites on bone loss following full-thickness mucoperiosteal flap: A 1-year prospective clinical trial. Journal of periodontology. 2022 Jul:93(7):966-976. doi: 10.1002/JPER.21-0591. Epub 2022 Mar 4 [PubMed PMID: 35137413]
Plonka AB, Sheridan RA, Wang HL. Flap Designs for Flap Advancement During Implant Therapy: A Systematic Review. Implant dentistry. 2017 Feb:26(1):145-152. doi: 10.1097/ID.0000000000000510. Epub [PubMed PMID: 27893512]
Level 1 (high-level) evidenceDE Marco G, Lanza A, Cristache CM, Capcha EB, Espinoza KI, Rullo R, Vernal R, Cafferata EA, DI Francesco F. The influence of flap design on patients' experiencing pain, swelling, and trismus after mandibular third molar surgery: a scoping systematic review. Journal of applied oral science : revista FOB. 2021:29():e20200932. doi: 10.1590/1678-7757-2020-0932. Epub 2021 Jun 4 [PubMed PMID: 34105693]
Chong BS, Rhodes JS. Endodontic surgery. British dental journal. 2014 Mar:216(6):281-90. doi: 10.1038/sj.bdj.2014.220. Epub [PubMed PMID: 24651333]
Jamal S, Gul M, Khan FR, Ghafoor R. Effect of full sulcular versus papilla-sparing flap on periodontal parameters in periradicular surgeries: A systematic review and meta-analysis. Journal of Indian Society of Periodontology. 2021 May-Jun:25(3):186-192. doi: 10.4103/jisp.jisp_290_20. Epub 2021 May 3 [PubMed PMID: 34158683]
Level 1 (high-level) evidenceKwon MS, Lee BS, Choi BJ, Lee JW, Ohe JY, Jung JH, Hwang BY, Kwon YD. Closure of oroantral fistula: a review of local flap techniques. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2020 Feb:46(1):58-65. doi: 10.5125/jkaoms.2020.46.1.58. Epub 2020 Feb 26 [PubMed PMID: 32158682]
Khandelwal P, Hajira N. Management of Oro-antral Communication and Fistula: Various Surgical Options. World journal of plastic surgery. 2017 Jan:6(1):3-8 [PubMed PMID: 28289607]
Alcântara MT, Ribeiro NR, Abreu DF. Complications associated with bichectomy surgery: a literature review. Minerva dental and oral science. 2021 Aug:70(4):155-160. doi: 10.23736/S2724-6329.20.04415-5. Epub 2020 Nov 3 [PubMed PMID: 33138350]
Furlow LT Jr. Cleft palate repair by double opposing Z-plasty. Plastic and reconstructive surgery. 1986 Dec:78(6):724-38 [PubMed PMID: 3786527]
Bozola AR, Gasques JA, Carriquiry CE, Cardoso de Oliveira M. The buccinator musculomucosal flap: anatomic study and clinical application. Plastic and reconstructive surgery. 1989 Aug:84(2):250-7 [PubMed PMID: 2748738]
Remangeon F, Hivelin M, Maurice D, Lantieri L, Laccourreye O. The posterior-based buccinator myomucosal flap (Bozola's flap). European annals of otorhinolaryngology, head and neck diseases. 2017 Feb:134(1):59-62. doi: 10.1016/j.anorl.2016.09.002. Epub 2016 Sep 30 [PubMed PMID: 27697402]
Pribaz J, Stephens W, Crespo L, Gifford G. A new intraoral flap: facial artery musculomucosal (FAMM) flap. Plastic and reconstructive surgery. 1992 Sep:90(3):421-9 [PubMed PMID: 1513887]
Fatani B, Alhilal AI, Alzahrani HH, Alkhattabi RR, Alhindi M. Facial Reconstruction Using Facial Artery Myomucosal Flap: A Comprehensive Review. Cureus. 2023 Jul:15(7):e42060. doi: 10.7759/cureus.42060. Epub 2023 Jul 18 [PubMed PMID: 37602111]
Rabbani CC, Lee AH, Desai SC. Facial Artery Musculomucosal Flap Operative Techniques. Plastic and reconstructive surgery. 2022 Mar 1:149(3):511e-514e. doi: 10.1097/PRS.0000000000008859. Epub [PubMed PMID: 35196693]
PFEIFER JS. THE REACTION OF ALVEOLAR BONE TO FLAP PROCEDURES IN MAN. Periodontics. 1965 May-Jun:3():135-40 [PubMed PMID: 14279364]
Hom DB, Ostrander BT. Reducing Risks for Local Skin Flap Failure. Facial plastic surgery clinics of North America. 2023 May:31(2):275-287. doi: 10.1016/j.fsc.2023.01.006. Epub [PubMed PMID: 37001930]
Hwang K, Son JS, Ryu WK. Smoking and Flap Survival. Plastic surgery (Oakville, Ont.). 2018 Nov:26(4):280-285. doi: 10.1177/2292550317749509. Epub 2018 Jan 9 [PubMed PMID: 30450347]
Bailey E, Kashbour W, Shah N, Worthington HV, Renton TF, Coulthard P. Surgical techniques for the removal of mandibular wisdom teeth. The Cochrane database of systematic reviews. 2020 Jul 26:7(7):CD004345. doi: 10.1002/14651858.CD004345.pub3. Epub 2020 Jul 26 [PubMed PMID: 32712962]
Level 1 (high-level) evidence