Introduction
DNA is the template from which everything inside the human body is built, so it is incredibly important that nothing happens to this code. Unfortunately, the DNA is at constant risk of mutation, which means a change to the genetic information in a cell, and this can happen due to a variety of factors.[1]
Cellular
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Cellular
One must first make the distinction between large-scale mutations, where a whole chunk of a chromosome is lost, relocated, or rearranged, vs. point mutation. A point mutation is typically a change in just one base pair in a DNA molecule, and a difference of even only one nucleotide can be enough to cause significant problems in the body.[2] For example, sickle cell disease is a genetic disorder that results because of a difference in a single nucleotide in the DNA of a carrier when compared to the DNA of a non-carrier. This difference occurs in the gene that codes for one of the subunits of hemoglobin, the protein that carries oxygen through the bloodstream. In this gene, there is an adenine molecule where thymine should be in the template strand of the gene, which will code for uracil instead of adenine in the corresponding mRNA, and then this altered codon will code for valine instead of glutamic acid. The hydrophobic side chain on valine is different enough from glutamic acid that the mutation results in a conformational change, which subsequently causes hemoglobin to aggregate in low-oxygen conditions, forming hemoglobin fibers. As a result, the red blood cells that carry hemoglobin become distorted into a rigid, sickle shape these can clog small blood vessels, which is a severe condition, so one can see that even one point mutation can be disastrous for an organism. When there is a point mutation, one possibility is that a nucleotide pair substitution occurs.[3] The mutation leading to sickle cell disease is an example of this, where one base pair gets replaced with a different base pair.
If this occurs outside of a gene, it is unlikely to have any effect, because these portions of the chromosome do not code for anything, but if this happens within a gene, it can lead to different results. If the resulting change in the template strand results in a new mRNA codon that translates for the same amino acid as before, which is possible since multiple codons can sometimes code for the identical amino acid, termed a silent mutation. In this case, even though the gene changed, the resulting protein will not be any different. If the change in the mRNA codon translates for a new, different amino acid, that is called a missense mutation, which is the most common point mutation.[4] This often will not make a big difference either, as many of the amino acids have similar side chains and changing just one amino acid may have minimal impact on the overall shape and behavior of the protein, but we saw with sickle cell disease that once in a while a missense mutation might make a big difference.
Among other reasons, this can be true if the amino acid that changed was the critical residue in supplying the catalytic activity of an enzyme. The active site might change shape due to new interactions, rendering it unable to bind its substrate. Or it is possible the side chain on this residue was specifically needed to interact chemically on the substrate, which now cannot take place in its absence, and if that enzyme is unable to do what it normally does, it could represent a significant problem for the cell. So missense mutations, while often benign, have the potential to be extremely harmful. Lastly, it is possible that substitution of this nature could cause the corresponding mRNA codon will not be able to code for an amino acid but to become a stop codon instead; the term for this is a nonsense mutation, which means that instead of the ribosome translating the rest of the mRNA strand it will just stop entirely, resulting in a partially complete protein. Unless the new stop codon is exceptionally close to the intended stop codon, it is highly unlikely that this protein fragment will be able to perform its intended function.
Biochemical
Sometimes, instead of substitution, there can be insertion or deletion; this is where one base pair either gets inserted or deleted from the DNA sequence. These kinds of mutations will typically have an enormous impact on the resulting protein because the codons on the resulting mRNA are supposed to translate as groups of three nucleotides. If one of these is suddenly added or deleted, every single codon after this mutation will be altered, resulting in a considerable number of missense mutations, and most likely an eventual premature stop codon. These are called frameshift mutations because the entire reading frame of the genetic code gets shifted. Frameshift mutations almost always lead to a non-functional protein. Having established the extremely grave nature of genetic mutations, what are the factors that precipitate to these mutations?
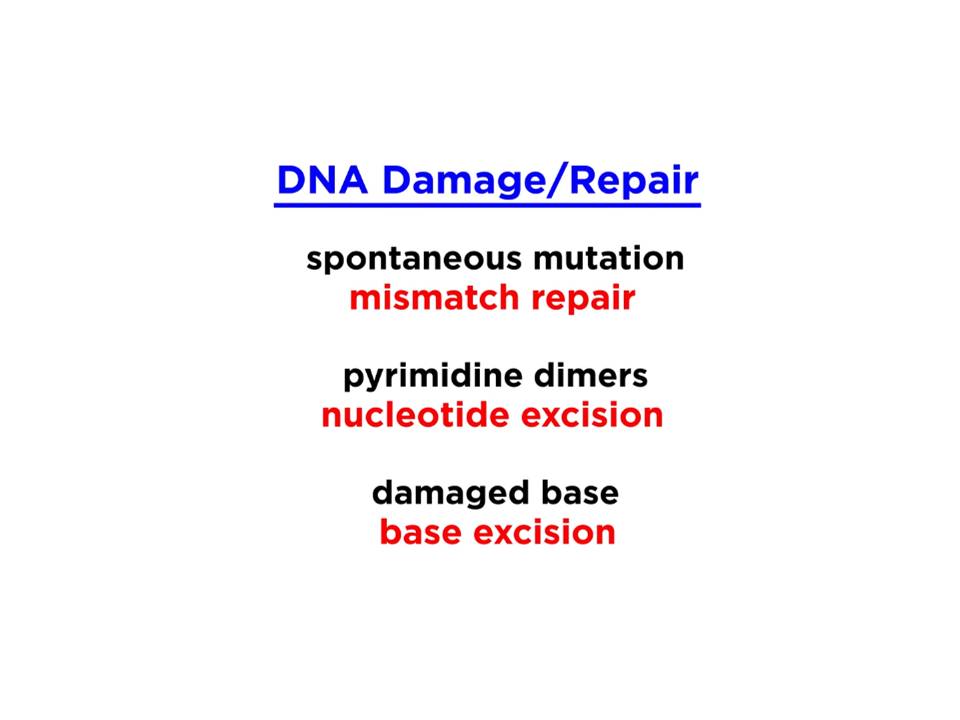
The first real cause of mutations is called spontaneous mutation; this is when the cellular machinery makes a mistake on its own, as not even mother nature is perfect. Once in a while, a polymerase enzyme will cause an error during replication, placing the wrong base across from the template strand. Usually, it will correct itself, but sometimes it will leave the error in the sequence, like for example guanine across from thymine on the template strand. This mismatch is recognizable by one of a variety of DNA repair enzymes that scan DNA hunting for these kinds of errors and knows precisely which base to kick out and the base with which to replace it; this is called DNA mismatch repair.[5]
But the chromosomes are so incredibly long that even these hard-working repair enzymes might miss an error. If the DNA molecule serves as a template for further replication, this strand will do just fine, since nothing happened to it. But when replicating this strand, the guanine was supposed to be adenine, so instead of coding for the thymine that is supposed to go across from it, it will code for cytosine instead. The GC pair that results won't look any different from any other GC pair in the molecule, so no repair enzyme can ever fix it. This type of spontaneous mutation will happen around once in every ten billion base pair, which while very high odds, and hopefully, when it occurs it will be in some random location in the chromosome that does not make a difference, but this is not always the case. It is not just the enzymes that are at fault; there are external causes of mutation too, called mutagens.[6]
Molecular Level
One such mutagen is radiation. Photons of light from the ultraviolet portion of the electromagnetic spectrum are high-energy particles, and if they collide with DNA in specific locations, they can cause pyrimidine dimers, which is when two adjacent thymine or cytosine bases become covalently linked, which distorts DNA, making normal genetic activity impossible. Luckily this distortion, or lesion, can be recognized by a repair enzyme that will initiate nucleotide excision repair. A nuclease enzyme can spot the problem and snip out a section of the DNA strand containing the lesion. Then polymerase puts new bases in the gap, and ligase seals it up, correcting the error; this is why UV light from the sun can be harmful; it may cause mutations like pyrimidine dimers. X-rays and gamma rays can cause mutations too since they are also high-energy photons.[6]
Other mutations involve modifications to a single base, caused by chemical mutagens like oxidizing agents. For example, guanine can be oxidized to become 8-oxoguanine, or oxoG, and because of the difference in orientation and functionality, oxoG does not pair with cytosine as a normal G does, it pairs with adenosine instead. If this error goes uncorrected and the opposite strand is a template for replication, once again the polymerase will have no way of knowing that this A was supposed to be a C. So instead of the G that ought to go on the complementary strand, it will put a T and the mutation is no longer fixable.
Other such modifications arrive in the way of alkylating agents, which add things like methyl groups to existing bases, which will interfere with replication and transcription. These types of mutations do not cause kinks in the DNA strand like thymine dimers do so they are not recognized in the same way that nuclease enzymes operate; they instead get recognized by glycosylase enzymes that will initiate base excision repair. This correction is different from nucleotide excision repair in that the enzyme specifically recognizes the mutant base, pulls that nucleotide out of the helix and removes the base by snipping the glycosidic bond, which is why the enzyme is called a glycosylase. Then polymerase and ligase do their jobs to put things back together. There is a different glycosylase for each kind of mutation of this variety, and they are all constantly scanning DNA for errors. So these are a few examples of the types of damage that can occur in DNA, and while there are many more; most of them fall into one of these categories according to the kind of enzyme that performs the repair. Some enzymes can perform mismatch repair, ones that do nucleotide excision repair, and others that do base excision repair, and there are over 100 different types of DNA repair enzymes in every cell in our body, keeping constant vigil over the sacred genetic code.[7]
Function
The function of the new mutant gene after the damage is different, especially if the repair mechanism failed to fix the problem completely. Some of the damage is lethal to the cell, and some might lead to an arrest of the gene function.
Clinical Significance
Some genodermatosis like basal cell nevus syndrome arises from DNA defective repair mechanisms that allow the cells to get back to normal after sun exposure. These patients tend to have skin cancer in the form of basal cell carcinoma and squamous cell carcinoma in early life. So, DNA repair is a crucial issue that affects the lives of many individuals.[8]
Media
(Click Image to Enlarge)
References
McKay MJ, Craig J, Kalitsis P, Kozlov S, Verschoor S, Chen P, Lobachevsky P, Vasireddy R, Yan Y, Ryan J, McGillivray G, Savarirayan R, Lavin MF, Ramsay RG, Xu H. A Roberts Syndrome Individual With Differential Genotoxin Sensitivity and a DNA Damage Response Defect. International journal of radiation oncology, biology, physics. 2019 Apr 1:103(5):1194-1202. doi: 10.1016/j.ijrobp.2018.11.047. Epub 2018 Nov 30 [PubMed PMID: 30508616]
de Camargo MS, De Grandis RA, da Silva MM, da Silva PB, Santoni MM, Eismann CE, Menegário AA, Cominetti MR, Zanelli CF, Pavan FR, Batista AA. Determination of in vitro absorption in Caco-2 monolayers of anticancer Ru(II)-based complexes acting as dual human topoisomerase and PARP inhibitors. Biometals : an international journal on the role of metal ions in biology, biochemistry, and medicine. 2019 Feb:32(1):89-100. doi: 10.1007/s10534-018-0160-0. Epub 2018 Nov 30 [PubMed PMID: 30506342]
Karzai F, VanderWeele D, Madan RA, Owens H, Cordes LM, Hankin A, Couvillon A, Nichols E, Bilusic M, Beshiri ML, Kelly K, Krishnasamy V, Lee S, Lee MJ, Yuno A, Trepel JB, Merino MJ, Dittamore R, Marté J, Donahue RN, Schlom J, Killian KJ, Meltzer PS, Steinberg SM, Gulley JL, Lee JM, Dahut WL. Activity of durvalumab plus olaparib in metastatic castration-resistant prostate cancer in men with and without DNA damage repair mutations. Journal for immunotherapy of cancer. 2018 Dec 4:6(1):141. doi: 10.1186/s40425-018-0463-2. Epub 2018 Dec 4 [PubMed PMID: 30514390]
Seplyarskiy VB, Akkuratov EE, Akkuratova N, Andrianova MA, Nikolaev SI, Bazykin GA, Adameyko I, Sunyaev SR. Error-prone bypass of DNA lesions during lagging-strand replication is a common source of germline and cancer mutations. Nature genetics. 2019 Jan:51(1):36-41. doi: 10.1038/s41588-018-0285-7. Epub 2018 Dec 3 [PubMed PMID: 30510240]
Akiyama M, Yamaoka M, Ohyama W, Yokoi K, Ashizuka S, Aizawa D, Ikegami M, Suzuki H, Ozaki K, Ida H, Yuza Y. Genetic Profile and Microsatellite Instability in a Case of Secondary Esophageal Squamous Cell Carcinoma 12 Years After Allogeneic Hematopoietic Stem Cell Transplantation for Aplastic Anemia. Journal of pediatric hematology/oncology. 2020 May:42(4):302-306. doi: 10.1097/MPH.0000000000001355. Epub [PubMed PMID: 30499911]
Level 3 (low-level) evidenceMajera D, Skrott Z, Bouchal J, Bartkova J, Simkova D, Gachechiladze M, Steigerova J, Kurfurstova D, Gursky J, Korinkova G, Cwiertka K, Hodny Z, Mistrik M, Bartek J. Targeting genotoxic and proteotoxic stress-response pathways in human prostate cancer by clinically available PARP inhibitors, vorinostat and disulfiram. The Prostate. 2019 Mar:79(4):352-362. doi: 10.1002/pros.23741. Epub 2018 Nov 29 [PubMed PMID: 30499118]
Piazza A, Heyer WD. Homologous Recombination and the Formation of Complex Genomic Rearrangements. Trends in cell biology. 2019 Feb:29(2):135-149. doi: 10.1016/j.tcb.2018.10.006. Epub 2018 Nov 26 [PubMed PMID: 30497856]
Minko IG, Christov PP, Li L, Stone MP, McCullough AK, Lloyd RS. Processing of N(5)-substituted formamidopyrimidine DNA adducts by DNA glycosylases NEIL1 and NEIL3. DNA repair. 2019 Jan:73():49-54. doi: 10.1016/j.dnarep.2018.11.001. Epub 2018 Nov 5 [PubMed PMID: 30448017]