Introduction
The nose is a significant facial feature for the identification of individuals and is also considered to be an aesthetic feature. Furthermore, it plays a significant role in two vital functions; respiration and olfaction.[1] It is a complicated three– dimensional organ, with various convexities and concavities due to the distinctive characteristics of the underlying soft tissue, which results in differences in form and appearance.[1][2] Therefore, the nose is a cardinal structure in both the craniofacial reconstruction surgeries and the forensic field.[2]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
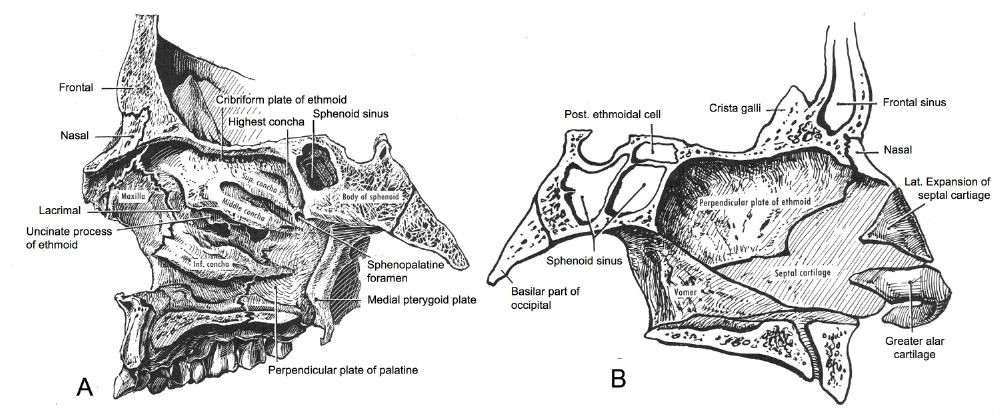
The skull bones (frontal, nasal, and maxillae) take part in forming the temple of the nose, and most of its external appearance is made up by the soft tissue structures underlying rather than the bones.[2]
Two paired nasal bones with the ascending process of the maxilla make up the bony vault (upper third) of the nose. The bony vault is smaller in females. At the nasofrontal suture, the nasal bones fuse with the frontal bone; this is called the nasion. The thickness of the bones differs, but it's the thickest at the nasofrontal suture. The average length of the nasal bones is 2.5 cm.[1][3]
The nose is composed of the root, dorsum tip, and columella (the part between nostrils) externally, while the other parts of the nose are composed of the ala, alar sulcus and nostrils. These are all supported by the underlying structures, which are the bones, cartilage, muscles and subcutaneous fat.[1]
The cartilage supports only the nasal bones, ethmoid bones, maxillae, and vomer. The cartilage is composed of the septal cartilage, the bilateral (greater) alar cartilage, the lateral cartilages, the lesser alar cartilage, and the sesamoid cartilage. The nasal septum supports the cartilage itself.[1]
The nasal septum forms the central part of the nose, and it is composed of the vomer posteriorly, and inferiorly it's composed of the ethmoid and the septal cartilage. It supports the soft tissue of the nose and reinforces the nasal structure by splitting it in two.[1][3]
The septal cartilage is connected superiorly to the lateral cartilages and inferiorly to the anterior nasal spine. The lateral cartilages have the shape of a triangle, and they are connected to the septal cartilage, to the inferior part of the nasal bones and sometimes to the frontal process of the maxilla. Both the lateral and septal cartilages disconnect anteriorly to allow movement at the time of respiration.[1]
The lower third of the nose is carried by the lower lateral cartilages that reside on the upper lateral cartilages, thus forming the tip of the nose and contributing to its round shape.[3]
The nasal vestibule represents the entrance of the nose and is padded with squamous epithelium, sebaceous glands, and hair. The squamous epithelium becomes mucosa after nearly 0.5 cm.[3]
Embryology
The maxillary process fuses with the frontonasal process, thus altering the nasal pits into a primeval nasal cavity, through forming a floor for its posterior part and forming the anterior nares altogether. The development of the nasal cavity can be described in four stages[4]:
- The first stage: nasal placodes formation
- The second stage: nasal placodes convert into nasal grooves
- The third stage: the nasal grooves give rise to the nasal pits
- The fourth stage: the nasal pits deepen, this is associated with the formation of the posterior nares
The nasal placodes are linked to the development of the palate and lip, and often a defect in the placode can lead to the finding of cleft lip or cleft palate. [5]
Interestingly, nasal trauma is detectable since the fourth month of fetal life. Compression of the nose structures in fetal growth depends on the location of fetus extremities.
Additionally, the nasal septum deviation is already be detectable in fetuses, which enables clinicians to estimate the nasal septum growth and symmetry, and therefore, predict the tendency to dysfunction occurring in the upper respiratory tract.[6]
Blood Supply and Lymphatics
The septum receives vascular supply by a branch of sphenopalatine artery posteriorly, a tributary of anterior ethmoid artery superiorly, a branch of the superior labial artery and the greater palatine artery antero-inferiorly. The lateral nasal wall gets its supply from the anterior ethmoid artery anteriorly, and the sphenopalatine artery supplies the rest of the structure. The turbinates, which are the lining of the lateral wall of the nose, are extremely vascular, and have large sinusoids, thus forming a system where both shunting of the blood and venous pooling are possible. A branch of the facial artery provides vascular supply to the vestibule.[3]
Nerves
The ophthalmic and maxillary branches of the trigeminal nerve provide the sensory innervation of the external nose. The ophthalmic branch supplies the nose with its three branches, which are the supratrochlear, the infratrochlear and the external nose nerve. The external nose nerve innervates the tip and the posterior part of the nose. The maxillary branch supplies the nose with its two branches, the infraorbital nerve, and the nasopalatine nerve. The infraorbital nerve innervates the tip, the ala and the lateral parts of the nose, while the nasopalatine nerve innervates the nasal septum.[1]
Muscles
There are eight nasal muscles identified; however, only two of these muscles affect the nasal profile - these are the procerus and the nasalis. The procerus muscle has two parts; only the superior medial part covers the nasal bones which inserts to the skin covering the eyebrow and the forehead. The nasalis muscle originates from the maxilla, which is transverse to the dorsum of the nose, and it inserts in the nostrils and the greater alar cartilages. However, the muscles and the soft tissue is not thought to influence the nose contour, but the cartilages do.[2]
Physiologic Variants
One of the vital functions of the nose is to humidify the air before it enters the lungs. Researchers have noted that there are differences in the nose shape among populations, not only because of genetics but also secondary to evolutionary changes of the nose, to adapt to the environment and climate. For example, the width of the nares is highly related to the temperature and absolute humidity, as wider noses are more prevalent in warm and humid climate and vice versa. The alar base width was found to be largest in West Africans and smallest in North Europeans. Both the alar base width and the nares width have progressed among populations because of divergent selection.[7]
Surgical Considerations
Nasal fractures
Nasal fractures are the most common facial fracture in adults, midface blunt trauma is the most common mechanism, and it is usually the result of road traffic accidents, sports injuries, falls, and physical fights. These injuries generally result in ipsilateral nasal bone fracture and contralateral out-fracture with septal deformation.[8] Males are affected more than females, and the most affected age group are in the thirties.[9] Diagnosis is usually made upon clinical evaluation, by history taking and physical examination, while imaging is rarely needed. Common physical findings in nasal fractures include tenderness, crepitus, nasal shortening/depression, step-offs, and nasal base widening. The presence of rhinorrhea may raise the suspicion of cerebrospinal fluid (CSF) leak, and thus the cerebral fluid must be examined, and neurology consulted. Many researchers have described before classification types for nasal fractures; below is the modified Murray classification system which depends on the clinical findings:
Modified Murray nasal trauma classification[8]:
- Type I: Injury confined to soft tissue
- Type IIa: Simple, unilateral nondisplaced fracture
- Type IIb: Simple, bilateral nondisplaced fracture
- Type III: simple, displaced fracture
- Type IV: closed, comminuted fracture
- Type V: complicated fracture or open comminuted fracture
Complications
The most common complication of nasal bone fractures is nasal deformities. Other complications include septal deviation, nasal obstruction, nasolacrimal duct obstruction with epiphora, diplopia and olfactory disturbances.[10]
If the fracture is simple and noncomminuted, then it is frequently managed by closed reduction.[8] However, 29% of patients report dissatisfaction with this method of management.[10] Open reduction is often necessary for complicated fractures that are associated with soft tissue destruction and loss of nasal support. For bony septal deformities, septal repair and fixation are performed.[8]
Clinical Significance
Nasal bone assessment in prenatal screening
Hypoplasia or absence of the nasal bone is highly associated with Down syndrome. Ultrasound screening for Down syndrome in the first trimester has shown the absence of the nasal bones in 65% of Down syndrome cases, while only 1% in healthy fetuses. Generally, 50% of Down syndrome cases have abnormally short nose root. However, the use of nasal bones as a marker for down syndrome should be done after 11 weeks of gestation, as the nose ossification usually begins at this time.[11]
The absence of the nasal bone is also one of the abnormalities that are detectable during the prenatal ultrasound screening of tetrasomy 9p, which is a very rare chromosomal disorder characterized by the presence of two additional copies of the short arm of chromosome 9.[12]
Nose maldevelopment
Nose maldevelopment can present in many forms; including the isolated absence of the nasal bones, hemi-aplasia, the complete absence of the nose (arrhinia), and others. The effects of these maldevelopments vary from mild aesthetic concerns up to airway obstruction and feeding problems. Establishment of the airway is highly critical in the neonatal period. Later in life, the cases are usually managed individually, and the type of surgical reconstruction done will be based on the type of the deformity. Minor surgeries involving small flaps are often used to correct the defects that are bound only to a small area, while major surgeries with large flaps using bone or cartilage grafts are the choice if the external nose is completely absent.[13]
In addition, deformities of the nasal pathways leading to the nasal cavities can also occur. Chonal atresia is stenosis of the nasal canals and occurs in infants. Pathology of nose formation can also be a sign of CHARGE syndrome. [14]
Nasal deviation
Nasal deviation involves cartilage deviation and, in most cases, bony deviation as well. The etiology may be congenital or due to nasal trauma such as nasal fractures. On the same side of the deviation, the nose is usually shorter, has slanted bone and cartilage sidewalls, while on the contralateral portion, the nose is often longer and has a gradual angularity with the cheeks. As a result, both sides of the nasal airway can be obstructed partially or entirely, which lead to both functional and esthetic problems. To correct this deviation, the nasal bones must be imparted to the midline to straighten it, and this is accomplished by rhinoplasty.[15]
Nasal injuries in sport
The most common nasal injury in sport is epistaxis, followed by lacerations and then fractures. These injuries often happen by the cause of direct blow to the nose in contact sports.[16]
Epistaxis
Epistaxis following nasal trauma can be substantial, however, there is no relationship noted between the severity of the injury and the amount of bleeding.[16] The presence of epistaxis following nasal trauma is highly associated with increased risk of external nasal disfigurement.[17] If there was no other associated injury with the bleeding like a fracture or a laceration, most likely the bleeding will stop spontaneously. Nevertheless, keeping the injured person in sitting position, with head leaning forward, breathing through the mouth and putting an ice bag on the back of the neck to activate the vasoconstriction reflex can also help in stopping the bleeding.[16]
Lacerations
Football helmets or hockey sticks often cause nasal lacerations. They can be associated with fractures, so it is highly important in case of lacerations to palpate the nasal bones to ensure there are no fractures. Lacerations are managed by irrigation and approximation to avoid infection and contamination.[16]
Nasal bone tumors
Nasal tumors are rare, although there are reports of some cases. Osseous hemangiomas are rare benign bone tumors, comprising less than 1% of bone tumors, they mostly involve the vertebra; however, there is a case report of a 16 years old female involving the nose.[18] Moreover, nasal angioma arising from the nasal bones is also a rare benign tumor which has a case report in a 41 years old female. Benign nasal tumors usually undergo management by surgical resection.[19] Ewing sarcoma, which is a malignant bony tumor most commonly affecting the long bones and the pelvis, was also reported to be developed in the nasal bones of a 5 years old female child. Ewing sarcoma treatment is by both chemotherapy and radiotherapy.[20]
Other Issues
Certain organisms have a predilection for the nares. Staph aureus, for instance, colonizes the anterior nares in 20-80% of patients. [21] Congenital syphillis and leprosy may present with a saddle nose deformity. [22] In addition metastasis to the nose are possible, and thus patients should be routinely assessed and monitored for such findings. [23]. The connection between the nasal cavity and pharynx and larynx acts as a route for both viral and bacterial pathogens and can lead to symptoms such as post nasal drip. [24]. Whereas nasal polyps in children are a strong indicator of cystic fibrosis or primary ciliary dyskinesia, in adults they may be a sign of aspirin induced asthma. [25] Kallman syndrome presents with anosmia and is often a key finding for differential diagnoses. [26] Thus, the symtomotolgy and anatomic variations of the in nasal cavity should be carefully examined and assessed as often they can be a sign of a different underlying clinical diagnosis.
Media
(Click Image to Enlarge)
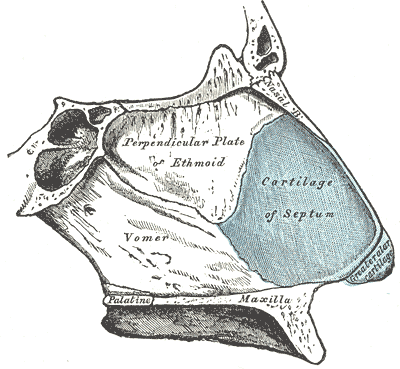
The Organ of Smell, Bones and Cartilage of the Septum of the Nose. Bones and cartilage of the septum of the nose, viewed from the right side: the perpendicular plate of the ethmoid, vomer, maxilla, palatine, septum cartilage, and greater alar cartilage.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Patel RG. Nasal Anatomy and Function. Facial plastic surgery : FPS. 2017 Feb:33(1):3-8. doi: 10.1055/s-0036-1597950. Epub 2017 Feb 22 [PubMed PMID: 28226365]
Anderson KJ, Henneberg M, Norris RM. Anatomy of the nasal profile. Journal of anatomy. 2008 Aug:213(2):210-6 [PubMed PMID: 19172735]
Jones N. The nose and paranasal sinuses physiology and anatomy. Advanced drug delivery reviews. 2001 Sep 23:51(1-3):5-19 [PubMed PMID: 11516776]
Level 3 (low-level) evidenceWARBRICK JG. The early development of the nasal cavity and upper lip in the human embryo. Journal of anatomy. 1960 Jul:94(Pt 3):351-62 [PubMed PMID: 13842854]
Maliha SG, Kantar RS, Gonchar MN, Eisemann BS, Staffenberg DA, Shetye PR, Grayson BH, Flores RL. The Effects of Nasoalveolar Molding on Nasal Proportions at the Time of Nasal Maturity. The Cleft palate-craniofacial journal : official publication of the American Cleft Palate-Craniofacial Association. 2021 Mar:58(3):284-289. doi: 10.1177/1055665620950139. Epub 2020 Aug 27 [PubMed PMID: 32851868]
Teul I, Slawinski G, Lewandowski J, Dzieciolowska-Baran E, Gawlikowska-Sroka A, Czerwinski F. Nasal septum morphology in human fetuses in computed tomography images. European journal of medical research. 2010 Nov 4:15 Suppl 2(Suppl 2):202-5 [PubMed PMID: 21147652]
Zaidi AA, Mattern BC, Claes P, McEvoy B, Hughes C, Shriver MD. Investigating the case of human nose shape and climate adaptation. PLoS genetics. 2017 Mar:13(3):e1006616. doi: 10.1371/journal.pgen.1006616. Epub 2017 Mar 16 [PubMed PMID: 28301464]
Level 3 (low-level) evidenceKelley BP, Downey CR, Stal S. Evaluation and reduction of nasal trauma. Seminars in plastic surgery. 2010 Nov:24(4):339-47. doi: 10.1055/s-0030-1269763. Epub [PubMed PMID: 22550458]
Hwang K, You SH. Analysis of facial bone fractures: An 11-year study of 2,094 patients. Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India. 2010 Jan:43(1):42-8. doi: 10.4103/0970-0358.63959. Epub [PubMed PMID: 20924449]
Hwang K, Yeom SH, Hwang SH. Complications of Nasal Bone Fractures. The Journal of craniofacial surgery. 2017 May:28(3):803-805. doi: 10.1097/SCS.0000000000003482. Epub [PubMed PMID: 28468171]
Sonek JD, Cicero S, Neiger R, Nicolaides KH. Nasal bone assessment in prenatal screening for trisomy 21. American journal of obstetrics and gynecology. 2006 Nov:195(5):1219-30 [PubMed PMID: 16615922]
Podolsky R, Saltzman D, Auerbach M, Roman AS. Absent nasal bone as a marker of tetrasomy 9p. Prenatal diagnosis. 2011 Dec:31(13):1313. doi: 10.1002/pd.2877. Epub 2011 Oct 26 [PubMed PMID: 22031456]
Level 3 (low-level) evidenceFijałkowska M, Antoszewski B. Nose underdevelopment - etiology, diagnosis and treatment. Otolaryngologia polska = The Polish otolaryngology. 2016 Apr 30:70(2):13-8. doi: 10.5604/00306657.1199344. Epub [PubMed PMID: 27386828]
Koppen T, Bartmann D, Jakob M, Bootz F, Müller A, Dresbach T, Send T. Diagnostics and therapy of bilateral choanal atresia in association with CHARGE syndrome. Journal of neonatal-perinatal medicine. 2021:14(1):67-74. doi: 10.3233/NPM-200450. Epub [PubMed PMID: 32741782]
Menger DJ. Surgical Treatment of the Twisted Nose. Clinics in plastic surgery. 2016 Jan:43(1):95-8. doi: 10.1016/j.cps.2015.08.004. Epub 2015 Oct 9 [PubMed PMID: 26616698]
McGrail JS. Nasal injuries in sports. Canadian family physician Medecin de famille canadien. 1972 Jul:18(7):60-1 [PubMed PMID: 20468794]
Daniel M, Raghavan U. Relation between epistaxis, external nasal deformity, and septal deviation following nasal trauma. Emergency medicine journal : EMJ. 2005 Nov:22(11):778-9 [PubMed PMID: 16244333]
Level 2 (mid-level) evidenceHazra TK, Basu SK, Chowdhury S, Deb P. Haemangioma of the nasal bone. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2001 Jul:53(3):239-42. doi: 10.1007/BF03028565. Epub [PubMed PMID: 23119808]
Handra-Luca A, Bisseret D, Gorphe P, Arsenovic N. Nasal angioma with osseous metaplasia. Avicenna journal of medicine. 2015 Oct-Dec:5(4):128-30. doi: 10.4103/2231-0770.165124. Epub [PubMed PMID: 26629468]
Vidyasagar MS, Rao S, Fernandes DJ, Ramanujam AS. A rare case of primary Ewings sarcoma of the nasal bone. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 1998 Jan:50(1):69-72. doi: 10.1007/BF02996777. Epub [PubMed PMID: 23119384]
Level 3 (low-level) evidenceChmielowiec-Korzeniowska A, Tymczyna L, Wlazło Ł, Nowakowicz-Dębek B, Trawińska B. Staphylococcus aureus carriage state in healthy adult population and phenotypic and genotypic properties of isolated strains. Postepy dermatologii i alergologii. 2020 Apr:37(2):184-189. doi: 10.5114/ada.2020.94837. Epub 2020 May 5 [PubMed PMID: 32489352]
Andrade M, Fernandes VS, Boléo-Tomé JP. Saddle nose: our approach to the problem. Aesthetic plastic surgery. 1999 Nov-Dec:23(6):403-6 [PubMed PMID: 10629295]
Bashyam A, Grammatopoulou V, Crook T, Di Palma S, Sunkaraneni VS. Tumour-to-tumour metastasis: breast carcinoma to an olfactory neuroblastoma. Annals of the Royal College of Surgeons of England. 2020 Jul:102(6):e118-e121. doi: 10.1308/rcsann.2020.0038. Epub 2020 May 6 [PubMed PMID: 32374183]
Eren E, Balcı K, Gerçik Ö, Kabadayı G, Akar S. Does Nasal Secretion Decrease in Sjögren Syndrome and Does This Affect Nasal Function? The Laryngoscope. 2021 Feb:131(2):370-373. doi: 10.1002/lary.29022. Epub 2020 Aug 11 [PubMed PMID: 32780886]
del Toro E, Portela J. Nasal Polyps. StatPearls. 2025 Jan:(): [PubMed PMID: 32809581]
Barraud S, Delemer B, Poirsier-Violle C, Bouligand J, Mérol JC, Grange F, Higel-Chaufour B, Decoudier B, Zalzali M, Dwyer AA, Acierno JS, Pitteloud N, Millar RP, Young J. Congenital Hypogonadotropic Hypogonadism with Anosmia and Gorlin Features Caused by a PTCH1 Mutation Reveals a New Candidate Gene for Kallmann Syndrome. Neuroendocrinology. 2021:111(1-2):99-114. doi: 10.1159/000506640. Epub 2020 Feb 20 [PubMed PMID: 32074614]