Introduction
Subclavian artery trauma requires expedient diagnosis and quick technical skills by the trauma surgeon. Strong knowledge of anatomy will help to augment diagnostic modalities and facilitate decisions for the operative approach. Newer studies suggest that endovascular management has a potential role in the management of these injuries. This activity will discuss various aspects of subclavian artery injury.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Subclavian artery injury is rare as it occurs in less than 5% of trauma patients.[1][2] The subclavian vessels are well-protected behind the clavicle, and therefore a significant mechanism is required to cause injury. Data from autopsies suggest that the majority of patients expire from subclavian or proximal axillary artery injuries before arriving at the hospital.[3] In-hospital mortality remains significant and is approximately 10% in modern reports.[4] Patients who arrive hypotensive on arrival had greater in-hospital mortality compared to normotensive patients. One study reported a mortality rate of 46% in patients with blunt subclavian artery injuries arriving in shock.[5] Isolated subclavian artery injuries have a lower mortality rate than isolated subclavian venous injuries.[6][7]
Epidemiology
Due to the protected anatomic location of the subclavian vessels, most subclavian artery trauma is usually caused by a penetrating mechanism secondary to firearm injuries or knife wounds.[2][8] While blunt mechanisms are less common than penetrating, subclavian artery injuries caused by blunt trauma are being reported in the literature more frequently due to the increasing use of imaging for diagnosis.[9][10][11][5][12] Associated injuries also vary by mechanism. Penetrating trauma more commonly results in the formation of a pseudoaneurysm.[13] In blunt trauma, complete brachial plexus injuries are more common, usually secondary to a fall on an outstretched hand. Subclavian artery injuries from penetrating trauma are associated with an increased mortality rate, whereas blunt trauma has a higher morbidity rate due to injury to surrounding structures. Iatrogenic injury of the subclavian artery can also occur due to a failed central venous catheter placement attempt. This type of injury will not be discussed in this review.
Pathophysiology
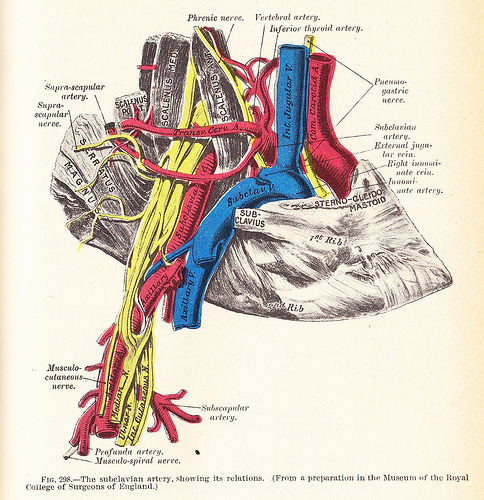
The subclavian arteries are protected by the skin, the clavicle, the superficial fascia, platysma, the supraclavicular nerves, and deep cervical fascia. Subclavian injuries from trauma are rarely reported in the pediatric population due to the increased elasticity of the chest wall and vessels. However, the presence of a scapular fracture in a pediatric patient should raise the suspicion of a subclavian artery injury.[14] The significant anatomic protection of the subclavian arteries makes operative intervention challenging. It is important to understand the anatomic variability in the origin of the subclavian arteries to undertake the optimal surgical approach. Despite differences in the anatomic course and origin of the right and left subclavian arteries, the branches are similar bilaterally and include the vertebral artery, the internal thoracic artery, the thyrocervical trunk, the costocervical trunk, and the dorsal scapular artery. Distally, at the lateral border of the first rib, the subclavian artery becomes the axillary artery. Each subclavian artery is divided into three parts: the first portion includes the vessel origin from the aorta to the medial border of the anterior scalene muscle, the second portion is behind the anterior scalene muscle, and the third portion extends from the lateral anterior scalene muscle to the lateral border of the first rib. The first portion of the subclavian artery lies near the internal jugular vein, carotid artery, vagus nerve, and the phrenic nerve. Injury to the proximal portion of the artery is rarely caused by blunt trauma due to its location deep within the chest cavity. The third portion of the artery is the most accessible surgically.
The embryologic origin of the right subclavian artery is from the right fourth aortic arch, the right dorsal aorta, and the right 7th intersegmental arteries. The right subclavian artery arises from the innominate artery typically above the sternoclavicular joint, where it branches into the right subclavian artery and the carotid artery. Common anatomic variations include the artery arises below the sternoclavicular joint and the right subclavian artery arising directly from the aorta.
The left subclavian artery has a different anatomic pattern, which influences the surgical approach. The embryologic origin of the left subclavian artery is the left seventh intersegmental artery. It arises directly from the arch of the aorta, and it typically does not traverse above the clavicle into the neck as the right subclavian artery does. The first part of the artery lies deep, and it is difficult to access surgically. The third portion of the left subclavian artery is lateral to the posterior border of the sternocleidomastoid muscle.
History and Physical
Advanced trauma support protocols should be initiated upon patient arrival. Patients suffering from subclavian artery injuries can have minimal initial symptoms on presentation, in particular for patients with a blunt trauma mechanism. Less than 25% of patients with subclavian artery injuries have “hard signs” of vascular trauma on physical exam.[15] Physical exam findings that raise suspicion for subclavian artery injury include absent upper extremity pulses, brachial plexus palsy, audible bruit, supraclavicular hematoma, first rib fracture, and active hemorrhage. A patient with evidence of an ischemic arm likely has an associated brachial plexus injury that should be explored and potentially repaired by an expert on brachial plexus repairs. However, the presence of collateral circulation from the thyrocervical trunk can mask physical signs of ischemia in patients with a subclavian injury. The presence of a distal upper extremity pulse does not eliminate the possibility of subclavian artery injury. Glasgow coma scale (GCS) less than 12, abbreviated injury score (AIS) of the head greater than 3, and the presence of clavicular or scapular fractures have been identified as independent risk factors for subclavian artery trauma in patients with thoracic trauma.[16] Abdominal trauma was found to be associated with a lower incidence of subclavian artery trauma. However, it remains imperative to have a subclavian artery injury as part of the differential diagnosis for any patient with chest, neck, or shoulder trauma. Misdiagnosis or late diagnosis of subclavian artery injury can result in delayed hemorrhage, pseudoaneurysm formation, or arteriovenous fistula.
Evaluation
An unstable patient should be taken without delay in the operating room. Obtaining adequate intravenous access to initiate massive transfusion is essential. In addition to expedient resuscitation with blood, immediate control of the bleeding is necessary. In patients with obvious neck or chest trauma and hard signs of vascular trauma, direct pressure to the site can be applied with a single digit to occlude the bleeding until operative intervention can commence. A Foley catheter with the balloon inflated into the wound can also be used to temporarily tamponade the bleeding vessel. Patients in extremis may require resuscitative thoracotomy in the emergency department for temporary vascular control through direct pressure at the thoracic cavity.
The identification of subclavian artery injuries is often made intra-operatively due to the hemodynamic instability of the patient precluding the ability to obtain imaging. In a stable patient with soft signs of vascular injury, imaging can be obtained to help elucidate the diagnosis. A chest radiograph in patients with associated subclavian artery injury may show a first rib fracture, widened mediastinum, apical pleural hematoma, or opacification along the expected course of the subclavian artery.
Angiography is important for appropriate preoperative planning. Once considered to be the gold standard for diagnosis, invasive arteriography has fallen out of favor due to possible complications and increased procedure time. Computed tomography angiography (CTA) provides the best diagnostic information on subclavian artery injuries.[9][17][4][17] Penetrating injuries resulting in a traumatic vessel occlusion will demonstrate a lack of enhancement at the injured artery site. Vessel transection will demonstrate contrast extravasation. Non-occlusive dissection of the artery, often secondary to blunt trauma, will show focal, linear, intraluminal filling defects with contrast filling the lumen distal to the injury.
Treatment / Management
Low-grade intimal injuries or arterial occlusions in selected patients with no signs of limb ischemia can be managed with observation with serial CTAs or ultrasounds and anticoagulation with anticoagulation or antiplatelet agents.[4] However, the mainstay of the management of high-grade subclavian trauma focuses on the optimal strategy for operative intervention. Non-operative management of these severe injuries is associated with poor outcomes; therefore, it is essential to consider either an open or an endovascular approach, which will both be discussed. However, operative management is challenging due to the complicated anatomic considerations and surgeon inexperience due to lack of experience with these injuries.[2] Operative mortality is most commonly secondary to rapid exsanguination. These issues will be discussed in detail in this section.(B2)
The subclavian vessels can be challenging to repair due to their location. It is imperative to understand the anatomical differences between the right and left subclavian vessels to have the optimal surgical approach. Basic vascular surgery principles of expedient proximal and distal control are crucial to avoid massive blood loss. In an unstable patient, the subclavian artery can be ligated, or a temporary shunt can be placed. If necessary, these patients can then be returned to the operating room for definitive repair once the patient has been appropriately resuscitated with a normal coagulation profile, correction of acidosis, and rewarmed. However, this practice should be avoided in patients with a history of radiation therapy to the shoulder or in patients with extensive soft tissue injury. These patients are at risk for serious morbidities, such as limb loss. The carotid-to-subclavian bypass should be avoided due to increased perioperative stroke risk.
All patients with suspected subclavian artery trauma should be placed supine on the operating room table. The patient’s chest and neck should be prepped along with the groin if a saphenous vein needs to be harvested for vascular repair. There are several different operative incisions, including median sternotomy, limited sternotomy, thoracotomy, supraclavicular, infraclavicular, or trap door incisions. The optimal incision must be tailored to the location of the injury. The advantages and disadvantages of these approaches will be discussed further.
The proximal right subclavian artery is optimally approached via median sternotomy.[6] Obtaining distal control requires an extension of the incision to a supraclavicular incision. First, the subclavian vein is exposed by first dividing the sternocleidomastoid muscle approximately 1 cm above the clavicle. The anterior scalene muscle is then divided to expose the subclavian artery. The phrenic nerve, which traverses laterally and in a superior to the inferior direction from the anterior scalene muscle and the vertebral artery, which lies posterior medial, must carefully be avoided. An aberrant right subclavian artery arising directly from the thoracic aorta occurs in 0.5% to 2.0% of the population and is an important consideration for the operative approach.[18] (B2)
The proximal left subclavian artery is optimally approached from a left posterolateral thoracotomy. However, this approach is time-consuming for a trauma patient and should not be used if the patient has suspected abdominal trauma as it would require the patient to be moved for exploratory laparotomy. In the emergent setting, the optimal approach to the proximal left subclavian artery is via an anterolateral thoracotomy in the third or fourth intercostal space. A supraclavicular approach or median sternotomy can help to gain access to the proximal left subclavian artery.[6] Exposure of the axillary artery via the extension of the infraclavicular incision to the deltopectoral groove is occasionally necessary to obtain distal subclavian artery control. A “trap door” incision or upper median sternotomy to connect the anterolateral thoracotomy and supraclavicular incisions should be avoided due to the high morbidity of this incision. (B2)
The sternocleidomastoid and scalene muscles must be ligated when exposing the subclavian artery above the clavicle. If necessary, the clavicle can be resected to help obtain adequate exposure of the subclavian vessels. This approach will also expose the common carotid arteries, the vertebral arteries, innominate vessels, and the superior vena cava. This procedure, however, results in significant morbidity from chest wall deformities, wound complications, and pain. Thus, removal of the clavicle should be avoided if possible.
The most common indications for the open approach are vessel transactions or greater than 50% vessel lacerations.[4] The subclavian arteries can be repaired primarily with debridement and end-to-end anastomosis or with a vein patch. A large segment transaction will require the placement of a prosthetic or autologous vein interposition graft. Interposition grafts are commonly required for patients with subclavian artery injuries from gunshot wounds.
Endovascular options for subclavian artery trauma are being reported more frequently in recent years.[12][13][19][17][20][21][22][23][24] Modern endovascular approaches include balloon-expandable or self-expanding endoprosthetic stent-grafts covered with polytetrafluoroethylene (PTFE). Criteria for endovascular repair of subclavian artery injury are an injury segment less than 3 cm and partial disruption of the arterial wall.[23][25] Endovascular repair is most common for pseudoaneurysms and also more commonly for left subclavian artery injuries due to its thoracic location compared to the extrathoracic location of the right subclavian artery. Frequent access sites are the femoral, brachial, or axillary arteries. Contraindications to the endovascular approach include vessel transaction, brachial plexus compression by a hematoma, and tracheal or esophageal injuries.[26] Hemodynamic instability is no longer considered an absolute contraindication to endovascular approach, and this largely depends on expedient access to the hybrid suite and availability of trained personnel.[26][24][4] Endovascular balloon occlusion can be utilized to obtain temporary vascular control, especially in an unstable patient before definitive operative repair. These hybrid approaches that combine the operative and endovascular approaches have also been successfully described in the literature and have expanded the applicability of the endovascular approach.[11][5][4] The most common hybrid procedure for this type of injury was open brachial artery exposure with retrograde covered stent placement.[4](B2)
Differential Diagnosis
Injuries to the chest, neck, or shoulder area can cause non-specific symptoms that can damage significant vessels, including the subclavian arteries, carotid arteries, axillary arteries, and the great vessels of the heart.
Prognosis
In patients who survive to the hospital with subclavian injuries, the overall prognosis is favorable for patients who undergo successful vascular repair. The most common injury with significant comorbidity following subclavian artery trauma is brachial plexus injuries. Despite successful revascularization and hematoma evacuation, most patients experience long-term neurologic sequelae resulting in disability secondary to brachial plexus injury. In a case series of 28 patients with concomitant repair of brachial nerve and artery injuries, only 50% of patients had a good functional recovery.[27]
Patients with arterial subclavian and axillary injuries have an estimated limb loss rate of 2.4% to 2.9%.[1][4] A review of the National Trauma Data Bank (NTDB) from 2007 to 2015 evaluated risk factors for limb loss in patients with arterial axillary/subclavian injuries.[1] Patients with combined arterial and venous injury, blunt trauma, and open repair were found to have a higher incidence of limb loss. Brachial plexus injury was not an independent risk factor for limb loss.
Patients with subclavian artery trauma likely have associated injuries that also must be identified and managed appropriately. Common associated injuries include spinal fractures, clavicular fracture, rib fractures, tracheobronchial injuries, and compressive hematomas. Associated humerus fracture was found to be associated with an increased risk of limb loss.[1] Ideally, the patient will be placed in a supine position during the operative intervention to allow easy access to the abdomen, neck, and extremities to identify and manage any additional injuries.
Compared with open repair, the endovascular approach has the reported advantages of decreased post-operative recovery time, limited dissection of the injured site, less pain, lower incidence of bleeding, and infectious complications.[28][13] Despite these early successful results, current evidence for the endovascular approach remains limited to case reports and small case series. Long-term results from the endovascular approach, including graft patency rates, also remain largely unknown, which could be a particular issue for younger trauma patients.[13][17] Prospective randomized studies directly comparing the open and endovascular approaches are needed.
Complications
Neural injuries are common sequelae following subclavian artery trauma. Patients with brachial plexus injuries have significant long-term complications, even with early recognition and repair of the nerve. Therefore, expectations and possible long-term complications should be discussed extensively with patients. The recurrent laryngeal nerve can be damaged during dissection and clamping the right subclavian artery in the neck and left subclavian artery in the thorax. This nerve damage can result in hoarseness, which could be permanent. Care should be taken to try to avoid inadvertently damaging this nerve. The phrenic nerve and vertebral arteries are also at risk of injury. The thoracic duct at its distal location may be inadvertently injured when clamping the distal left subclavian vein. The thoracic duct should be ligated, and drains should be placed if it is injured during the dissection.
Reported procedural complications from the endovascular approach include access site hematoma, pseudoaneurysm formation, stent-graft stenosis, endoleak, thrombosis, and decreased cerebral blood flow due to an endovascular stent covering the vertebral artery.[17][22][29][24] These patients often require long-term antiplatelet therapy and thus are susceptible to bleeding complications due to chronic anticoagulation. Occlusions of the vertebral artery may cause vertebrobasilar embolization. The endovascular approach was also associated with an increased need for a secondary procedure.[28] However, few patients ultimately require conversion to open procedures.[12]
Deterrence and Patient Education
Increasing pre-hospital and in-hospital provider awareness of the prompt clinical diagnosis of subclavian artery injuries could help get patients transferred to the appropriate trauma centers for prompt treatments.
Enhancing Healthcare Team Outcomes
The mortality rate for subclavian artery trauma is high as these injuries are difficult to diagnose. As pre-hospital protocols and trauma systems improve, mortality rates from subclavian trauma could also improve. Early recognition of subclavian artery trauma is imperative to the appropriate management of this injury. Trauma management principles need to be initiated rapidly with an emphasis on rapid blood transfusion and control of bleeding. As endovascular approaches continue to become more prevalent, it is important to continue to evaluate the long-term outcomes of this approach.
Media
(Click Image to Enlarge)

Branches of the Aorta. This illustration includes the right common carotid artery, right vertebral artery, right subclavian artery, brachiocephalic artery, ascending aorta, left coronary artery, right coronary artery, left common carotid artery, left vertebral artery, left subclavian artery, left axillary artery, left brachial artery, arch of aorta, and descending aorta.
Contributed by Beckie Palmer
(Click Image to Enlarge)
References
Grigorian A, Wilson SE, de Virgilio C, Kabutey NK, Fujitani RM, Gabriel V, Schubl SD, Joe V, Nahmias J. Humerus fracture and combined venous injury increases limb loss in axillary or subclavian artery injury. Vascular. 2019 Jun:27(3):252-259. doi: 10.1177/1708538118811231. Epub 2018 Nov 14 [PubMed PMID: 30426848]
Sobnach S, Nicol AJ, Nathire H, Edu S, Kahn D, Navsaria PH. An analysis of 50 surgically managed penetrating subclavian artery injuries. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2010 Feb:39(2):155-9. doi: 10.1016/j.ejvs.2009.10.013. Epub 2009 Nov 11 [PubMed PMID: 19910223]
Level 2 (mid-level) evidenceMcKinley AG, Carrim AT, Robbs JV. Management of proximal axillary and subclavian artery injuries. The British journal of surgery. 2000 Jan:87(1):79-85 [PubMed PMID: 10606915]
Waller CJ, Cogbill TH, Kallies KJ, Ramirez LD, Cardenas JM, Todd SR, Chapman KJ, Beckman MA, Sperry JL, Anto VP, Eriksson EA, Leon SM, Anand RJ, Pearlstein M, Capano-Wehrle L, Cothren Burlew C, Fox CJ, Cullinane DC, Roberts JC, Harrison PB, Berg GM, Haan JM, Lightwine K. Contemporary management of subclavian and axillary artery injuries-A Western Trauma Association multicenter review. The journal of trauma and acute care surgery. 2017 Dec:83(6):1023-1031. doi: 10.1097/TA.0000000000001645. Epub [PubMed PMID: 28715360]
Elkbuli A, Shaikh S, McKenney M, Boneva D. Subclavian artery avulsion following blunt trauma: A case report and literature review. International journal of surgery case reports. 2019:61():157-160. doi: 10.1016/j.ijscr.2019.07.061. Epub 2019 Jul 25 [PubMed PMID: 31376736]
Level 3 (low-level) evidenceDemetriades D, Chahwan S, Gomez H, Peng R, Velmahos G, Murray J, Asensio J, Bongard F. Penetrating injuries to the subclavian and axillary vessels. Journal of the American College of Surgeons. 1999 Mar:188(3):290-5 [PubMed PMID: 10065818]
Level 2 (mid-level) evidenceDemetriades D, Rabinowitz B, Pezikis A, Franklin J, Palexas G. Subclavian vascular injuries. The British journal of surgery. 1987 Nov:74(11):1001-3 [PubMed PMID: 3690221]
Level 2 (mid-level) evidenceDebakey ME, Simeone FA. Battle Injuries of the Arteries in World War II : An Analysis of 2,471 Cases. Annals of surgery. 1946 Apr:123(4):534-79 [PubMed PMID: 17858758]
Level 3 (low-level) evidenceQueiroz RM, Santana DBF, Roque D, Bernardes Filho F, Febronio EM, Valentin MVN. Blunt thoracic trauma with the formation of pseudoaneurysm with the junction of the right subclavian artery. Revista da Associacao Medica Brasileira (1992). 2018 Nov:64(11):987-989. doi: 10.1590/1806-9282.64.11.987. Epub [PubMed PMID: 30570048]
Ipaktchi R, Dettmer S, Vogt PM, Knobloch K. Subclavian artery and jugular vein rupture after a blunt thoracic trauma due to a BMX handlebar. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2010 Jan:37(1):235. doi: 10.1016/j.ejcts.2009.07.015. Epub 2009 Aug 22 [PubMed PMID: 19700337]
Level 3 (low-level) evidenceDiaz-Gutierrez I, Rana MA, Ali B, Marek JM, Langsfeld M. Hybrid Repair of Complex Left Subclavian Artery Injury with Partial Transection and Complete Thrombosis in an Unstable Patient following Blunt Trauma. Annals of vascular surgery. 2017 Apr:40():298.e11-298.e14. doi: 10.1016/j.avsg.2016.08.026. Epub 2016 Nov 27 [PubMed PMID: 27903481]
Ismazizi Z, Zainal AA, Naresh G. Traumatic right proximal subclavian artery pseudoaneurysm treated with a hybrid procedure: A case report. The Medical journal of Malaysia. 2016 Aug:71(4):220-222 [PubMed PMID: 27770128]
Level 3 (low-level) evidenceAlawneh K, Raffee L, Hamouri S. Delayed Endovascular Stenting of Right Subclavian Artery Pseudoaneurysm Caused by Gunshot Accident in a Syrian Refugee: A Case Report. Vascular and endovascular surgery. 2017 Aug:51(6):386-389. doi: 10.1177/1538574417710412. Epub 2017 Jun 13 [PubMed PMID: 28606011]
Level 3 (low-level) evidenceAbd El-Shafy I, Rosen LM, Prince JM, Letton RW, Rosen NG. Blunt traumatic scapular fractures are associated with great vessel injuries in children. The journal of trauma and acute care surgery. 2018 Nov:85(5):932-935. doi: 10.1097/TA.0000000000001980. Epub [PubMed PMID: 29787531]
Aksoy M, Tunca F, Yanar H, Guloglu R, Ertekin C, Kurtoglu M. Traumatic injuries to the subclavian and axillary arteries: a 13-year review. Surgery today. 2005:35(7):561-5 [PubMed PMID: 15976953]
Level 2 (mid-level) evidenceKou HW, Liao CH, Huang JF, Hsu CP, Wang SY, Ou Yang CH, Kang SC, Hsu YP, Hsieh CH, Kuo IM. Eighteen years' experience of traumatic subclavian vascular injury in a tertiary referral trauma center. European journal of trauma and emergency surgery : official publication of the European Trauma Society. 2019 Dec:45(6):973-978. doi: 10.1007/s00068-018-01070-5. Epub 2019 Jan 9 [PubMed PMID: 30627733]
Jacks R, Degiannis E. Endovascular Therapy And Controversies In The Management Of Vascular Trauma. Scandinavian journal of surgery : SJS : official organ for the Finnish Surgical Society and the Scandinavian Surgical Society. 2014 Jun:103(2):149-155 [PubMed PMID: 24809355]
Coppi G, Tshomba Y, Psacharopulo D, Marone EM, Chiesa R. Aberrant right subclavian artery in blunt aortic injury: implication for treatment and review of the literature. Annals of vascular surgery. 2012 Aug:26(6):861.e1-6. doi: 10.1016/j.avsg.2012.01.012. Epub [PubMed PMID: 22794343]
Level 3 (low-level) evidenceDuBose JJ, Rajani R, Gilani R, Arthurs ZA, Morrison JJ, Clouse WD, Rasmussen TE, Endovascular Skills for Trauma and Resuscitative Surgery Working Group. Endovascular management of axillo-subclavian arterial injury: a review of published experience. Injury. 2012 Nov:43(11):1785-92. doi: 10.1016/j.injury.2012.08.028. Epub 2012 Aug 22 [PubMed PMID: 22921384]
Günday M, Ozülkü M, Yıldırım E, Güven A, Ciftçi O. Successful endovascular treatment of subclavian artery dissection after compression trauma. The American journal of emergency medicine. 2013 Feb:31(2):457.e1-3. doi: 10.1016/j.ajem.2012.07.030. Epub 2012 Oct 5 [PubMed PMID: 23041483]
Level 3 (low-level) evidenceMatsagkas M, Kouvelos G, Peroulis M, Xanthopoulos D, Bouris V, Arnaoutoglou E. Endovascular repair of blunt axillo-subclavian arterial injuries as the first line treatment. Injury. 2016 May:47(5):1051-6. doi: 10.1016/j.injury.2016.02.003. Epub 2016 Feb 13 [PubMed PMID: 26905594]
Naidoo NG, Navsaria P, Beningfield SJ, Natha B, Cloete N, Gill H. Stent graft repair of subclavian and axillary vascular injuries: The Groote Schuur experience. South African journal of surgery. Suid-Afrikaanse tydskrif vir chirurgie. 2015 Oct 8:53(1):5-9 [PubMed PMID: 26449598]
Biagioni RB,Burihan MC,Nasser F,Biagioni LC,Ingrund JC, Endovascular treatment of penetrating arterial trauma with stent grafts. VASA. Zeitschrift fur Gefasskrankheiten. 2018 Feb; [PubMed PMID: 29082822]
Carrick MM, Morrison CA, Pham HQ, Norman MA, Marvin B, Lee J, Wall MJ Jr, Mattox KL. Modern management of traumatic subclavian artery injuries: a single institution's experience in the evolution of endovascular repair. American journal of surgery. 2010 Jan:199(1):28-34. doi: 10.1016/j.amjsurg.2008.11.031. Epub 2009 Jun 11 [PubMed PMID: 19520356]
Level 2 (mid-level) evidenceDesai SS, DuBose JJ, Parham CS, Charlton-Ouw KM, Valdes J, Estrera AL, Safi HJ, Azizzadeh A. Outcomes after endovascular repair of arterial trauma. Journal of vascular surgery. 2014 Nov:60(5):1309-1314. doi: 10.1016/j.jvs.2014.05.016. Epub 2014 Jul 3 [PubMed PMID: 24997806]
Gilani R, Tsai PI, Wall MJ Jr, Mattox KL. Overcoming challenges of endovascular treatment of complex subclavian and axillary artery injuries in hypotensive patients. The journal of trauma and acute care surgery. 2012 Sep:73(3):771-3. doi: 10.1097/TA.0b013e318265cdec. Epub [PubMed PMID: 22929506]
Level 2 (mid-level) evidenceShaw AD, Milne AA, Christie J, Jenkins AM, Murie JA, Ruckley CV. Vascular trauma of the upper limb and associated nerve injuries. Injury. 1995 Oct:26(8):515-8 [PubMed PMID: 8550137]
Murad MH, Rizvi AZ, Malgor R, Carey J, Alkatib AA, Erwin PJ, Lee WA, Fairman RM. Comparative effectiveness of the treatments for thoracic aortic transection [corrected]. Journal of vascular surgery. 2011 Jan:53(1):193-199.e1-21. doi: 10.1016/j.jvs.2010.08.028. Epub 2010 Oct 29 [PubMed PMID: 21035988]
Level 1 (high-level) evidenceBranco BC, DuBose JJ. Endovascular solutions for the management of penetrating trauma: an update on REBOA and axillo-subclavian injuries. European journal of trauma and emergency surgery : official publication of the European Trauma Society. 2016 Dec:42(6):687-694 [PubMed PMID: 27853843]