Anatomy, Bony Pelvis and Lower Limb, Foot Fascia
Anatomy, Bony Pelvis and Lower Limb, Foot Fascia
Introduction
The fascia in the foot is composed of fibrous connective tissue that serves to separate, support, and attach muscles. It can be divided into the superficial fascia and the deep fascia. The superficial fascia is located just beneath the skin and varies in strength depending on where it is in the foot. On the dorsal side of the foot, the superficial fascia is thin and mobile. In contrast, the superficial fascia of the plantar side is thick and has multiple septations that contain fat to provide a cushion for the foot. It also has thick connections with the underlying deep fascia. [1]
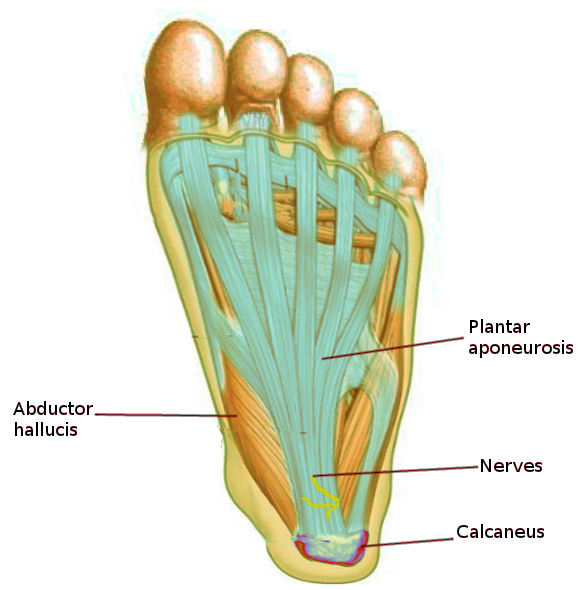
The deep fascia is stronger than the superficial fascia. On the dorsal side of the foot, the deep fascia is thin and connected to the inferior extensor retinaculum. It continues laterally and posteriorly to connect with the plantar fascia, which is the name of the deep fascia on the plantar side. Similar to the superficial fascia, the deep fascia is much thicker on the plantar side. The central part of the plantar fascia forms the plantar aponeurosis, which starts proximally at the calcaneus and extends distally into five separate bands that become the digital sheaths. It is supported inferiorly by the superficial transverse metatarsal ligament. [2]
The fascia acts as a border for the five anatomic compartments of the foot, which include the medial compartment, the central compartment, the lateral compartment, the dorsal compartment, and the interosseous compartment. The medial compartment is bordered inferiorly by the medial plantar fascia, the central compartment is bordered inferiorly by the plantar aponeurosis, and the lateral compartment is bordered inferiorly by the lateral plantar fascia. The plantar aponeurosis also has intermuscular septa that extend superiorly through the foot to divide the medial, central, and lateral compartments. The interosseous compartment is bordered by the plantar and dorsal interosseous fascia. The dorsal compartment is bordered by the dorsal fascia superiorly and by the tarsal bones and dorsal interosseous fascia inferiorly.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The fascia has multiple important roles in the foot. These roles, in general, can be extrapolated from all other regions of the body[3].
The fascial elements in the foot separate the various muscles into organized compartments that optimize static and dynamic function. The fascial compartments also influence the shape of the muscles, optimize movement, and function the regional nerves and blood vessels, ultimately influencing the overall physiologic function in the foot. Mechanically, the fascia provides the ideal shock-absorbing characteristics to help provide a soft, yet supportive, balanced cushion of support to allow for pedal movement.
Windlass mechanism
The "windlass mechanism" is a well-known mechanical model described throughout the literature to depict the plantar fascia's critical role in providing dynamic support to the foot during weight-bearing activities. The term "windlass" refers to the tightening of a rope or cable [4][5].
Originally described by Hicks in the 1950s[6], the plantar fascia forms the supportive truss (or tie rod), with its corresponding arch consisting of the calcaneus, midtarsal joint, and the metatarsals (the medial longitudinal arch). This dynamic mechanism can also be depicted as a triangle, with the plantar fascia represented by the hypotenuse of the triangle. The plantar fascia runs from the calcaneus to the phalanges. Utilizing its inherent tensile strength, it prevents the collapse of the arch of the foot upon vertical load transmission from the weight of the body. Additionally, as the ankle dorsiflexes in preparation for the "toe-off" phase of the gait cycle, this winds the plantar fascia around the head of the metatarsal to further tighten the fascia and prevents an increase in the distance between the calcaneus and metatarsals (from anterior to posterior), which ultimately prevents the collapse of the medial longitudinal arch.
Embryology
Like all fascia in the body, the fascia in the foot is derived from the mesoderm. Some anatomists believe the plantar fascia shares its origin with the Achilles tendon. A connection that they believe diminishes with age. [7][8]
Intrauterine packaging phenomenon
During fetal development, the position of the fetus in the uterus can influence the development of certain conditions, most notably:
- Metatarsus adductus (MA)
- Developmental dysplasia of the hip (DDH)
- Acetabular dysplasia
- Congenital hip dislocation
- Congenital torticollis
This phenomenon influences not only the osseous development of these aforementioned anatomic structures, but these conditions can also implicate soft-tissue deformity, pathologic function, and a varying spectrum of flexibility versus rigid contractures. For example, the position of the fetus in babies born with MA is thought to contribute to the increasing pressures and compression of the forefoot as the legs are crossed over the body. Moreover, as the fetus continues to grow during late gestation, the incidence of MA increases in babies born at full-, late-, or post-term compared to infants delivered prior to 30 weeks of gestation[9].
Blood Supply and Lymphatics
The blood supply to the fascia in the foot is supplied by smaller vessels that branch off the dorsalis pedis artery and the posterior tibial artery. The dorsalis pedis artery supplies the fascia on the dorsal aspect of the foot, and the posterior tibial artery supplies the fascia on the plantar aspect of the foot.
There are both superficial and deep lymphatic vessels in the foot that travel through the fascia. The superficial lymphatic vessels are more prominent medially. They converge next to the great saphenous vein and eventually drain into the superficial inguinal lymph nodes while the lateral lymphatic vessels converge next to the small saphenous vein and eventually drain into the popliteal lymph nodes. The deep lymphatic vessels follow the major blood vessels in the foot and drain into the popliteal lymph nodes.
Nerves
The nerves that supply the fascia of the foot can be classified regionally. The dorsal fascia is supplied by the superficial fibular nerve, the lateral fascia is supplied by the sural nerve, the medial fascia is supplied by the saphenous nerve, and the plantar fascia is supplied by the lateral and medial plantar nerves.
Muscles
The fascia plays a key role in dividing and attaching muscles in the foot. The relationship of the fascia with the muscles can be further described by the compartment they are in.
- Medial compartment: The medial plantar fascia overlies the abductor hallucis, flexor hallucis brevis, and the flexor hallucis longus tendon.
- Central compartment: The central plantar fascia overlies the flexor digitorum brevis, the tendon of the flexor hallucis longus, the tendons and musculature of the flexor digitorum longus, the quadratus plantae, the lumbricals, and the adductor hallucis.
- Lateral compartment: The lateral plantar fascia overlies the abductor and flexor digiti minimi brevis.
- Interosseous compartment: The plantar and dorsal interosseous fascias border the interosseous muscles.
- Dorsal compartment: The dorsal fascia overlies the extensors hallucis brevis and extensor digitorum brevis.
Surgical Considerations
If conservative treatment has failed, plantar fasciotomy can be considered. This technique is performed by using minimally invasive and endoscopic approaches to cut the plantar fascia and relieve tension. [10][11]
Clinical Significance
Plantar Fasciitis
Plantar fasciitis presents as sharp, unilateral pain at the proximal, plantar aspect of the foot. The pain is often most severe after long periods of rest. While the pathophysiology is not completely understood, recent evidence suggests that plantar fasciitis is due to a disruption in normal biomechanics that results in repetitive small tears in the plantar fascia. It is most common in obese individuals who have to stand or walk on hard surfaces. Plantar fasciitis can be diagnosed clinically by reproducing tenderness with palpation of the inner heel. A lateral radiograph of the foot may also show calcaneal spurring where the plantar fascia attaches proximally to the calcaneus. Treatment of plantar fasciitis generally involves rest, ice, massage, and calf-strengthening exercises [10][12][13].
Plantar Fascial Tear
Plantar fascial tears can occur acutely or chronically. If acute, it will present with a sudden popping sensation on the plantar aspect of the foot that is associated with acute pain, ecchymosis, and edema. If chronic, it will present with ecchymosis and edema in a patient with underlying plantar fasciitis. Plantar fascial tears can be diagnosed clinically by palpating a painful lump on the sole. Imaging with diagnostic ultrasound can aid in the diagnosis. Treatment is usually conservative and begins by immobilizing the foot with a boot initially, including the use of pre-fabricated shoe and cushioned heel inserts. The literature supports the utilization of a non-weight bearing plantar fascia-specific stretching program as opposed to a weight-bearing Achilles tendon stretching program. The former yields the highest patient satisfaction scores at 8-week follow-up [14][15][16].
Plantar Fibromatosis
Plantar fibromatosis is a non-malignant disorder that causes nodular thickening of the plantar fascia. It presents as a painless lump on the medial border of the plantar surface of the foot. While the cause is not well understood, there is believed to be a genetic component to the disorder. Clinical assessment and imaging with MRI or diagnostic ultrasound are used to make the diagnosis. Treatment is unnecessary if there are no symptoms. If symptomatic, insoles can be used to redistribute weight off of the area of thickening. Further intervention includes radiotherapy and even surgery if necessary [17].
Foot Deformities
Many different types of foot deformities can implicate increasing plantar pressures throughout different areas of the foot. For example, metatarsus adductus (MA) is a congenital foot condition resulting in adduction of the forefoot at the tarsometatarsal joint, medial metatarsal deviation, supination of the hindfoot through the subtalar joint, and a plantarflexed first ray[18]. A recent study investigated the peak plantar pressures during adult gait analysis utilizing a pedobarograph. The authors reported statistically significant greater peak plantar pressures in the region of the heel, lateral midfoot, and lateral forefoot compared to normal adult controls. This condition represents an example of the pathologic impact on the plantar fascia (and the entire plantar aspect of the foot) consistent with lateral column overload and developing various types of chronic pain syndromes consistent with abnormal gait patterns. MA is an under-recognized clinical condition, especially in the setting of subtle degrees of deformity. Thus, it is imperative for clinicians to recognize this condition in newborns to help prevent propagating long-term ensuing foot deformities and chronic pain conditions.
Media
(Click Image to Enlarge)
References
Hernández-Díaz C, Saavedra MÁ, Navarro-Zarza JE, Canoso JJ, Villaseñor-Ovies P, Vargas A, Kalish RA. Clinical anatomy of the ankle and foot. Reumatologia clinica. 2012 Dec-2013 Jan:8 Suppl 2():46-52. doi: 10.1016/j.reuma.2012.10.005. Epub 2012 Dec 8 [PubMed PMID: 23228530]
Mitchell IR, Meyer C, Krueger WA. Deep fascia of the foot. Anatomical and clinical considerations. Journal of the American Podiatric Medical Association. 1991 Jul:81(7):373-8 [PubMed PMID: 1941581]
Bordoni B, Mahabadi N, Varacallo M. Anatomy, Fascia. StatPearls. 2023 Jan:(): [PubMed PMID: 29630284]
Lee SY, Hertel J, Lee SC. Rearfoot eversion has indirect effects on plantar fascia tension by changing the amount of arch collapse. Foot (Edinburgh, Scotland). 2010 Jun-Sep:20(2-3):64-70. doi: 10.1016/j.foot.2010.06.003. Epub 2010 Jul 24 [PubMed PMID: 20656471]
Bolgla LA, Malone TR. Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice. Journal of athletic training. 2004 Jan:39(1):77-82 [PubMed PMID: 16558682]
HICKS JH. The mechanics of the foot. II. The plantar aponeurosis and the arch. Journal of anatomy. 1954 Jan:88(1):25-30 [PubMed PMID: 13129168]
Stecco C, Corradin M, Macchi V, Morra A, Porzionato A, Biz C, De Caro R. Plantar fascia anatomy and its relationship with Achilles tendon and paratenon. Journal of anatomy. 2013 Dec:223(6):665-76. doi: 10.1111/joa.12111. Epub 2013 Sep 12 [PubMed PMID: 24028383]
Shaw HM, Vázquez OT, McGonagle D, Bydder G, Santer RM, Benjamin M. Development of the human Achilles tendon enthesis organ. Journal of anatomy. 2008 Dec:213(6):718-24. doi: 10.1111/j.1469-7580.2008.00997.x. Epub [PubMed PMID: 19094187]
Fishco WD, Ellis MB, Cornwall MW. Influence of a metatarsus adductus foot type on plantar pressures during walking in adults using a pedobarograph. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2015 May-Jun:54(3):449-53. doi: 10.1053/j.jfas.2014.11.007. Epub 2015 Jan 30 [PubMed PMID: 25648273]
Level 2 (mid-level) evidenceGoff JD, Crawford R. Diagnosis and treatment of plantar fasciitis. American family physician. 2011 Sep 15:84(6):676-82 [PubMed PMID: 21916393]
Cutts S, Obi N, Pasapula C, Chan W. Plantar fasciitis. Annals of the Royal College of Surgeons of England. 2012 Nov:94(8):539-42. doi: 10.1308/003588412X13171221592456. Epub [PubMed PMID: 23131221]
Orchard J. Plantar fasciitis. BMJ (Clinical research ed.). 2012 Oct 10:345():e6603. doi: 10.1136/bmj.e6603. Epub 2012 Oct 10 [PubMed PMID: 23054045]
Tahririan MA, Motififard M, Tahmasebi MN, Siavashi B. Plantar fasciitis. Journal of research in medical sciences : the official journal of Isfahan University of Medical Sciences. 2012 Aug:17(8):799-804 [PubMed PMID: 23798950]
Rolf C, Guntner P, Ericsäter J, Turan I. Plantar fascia rupture: diagnosis and treatment. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 1997 Mar-Apr:36(2):112-4 [PubMed PMID: 9127213]
Level 3 (low-level) evidenceLouwers MJ, Sabb B, Pangilinan PH. Ultrasound evaluation of a spontaneous plantar fascia rupture. American journal of physical medicine & rehabilitation. 2010 Nov:89(11):941-4. doi: 10.1097/PHM.0b013e3181f711e2. Epub [PubMed PMID: 20962604]
Level 3 (low-level) evidenceNeufeld SK, Cerrato R. Plantar fasciitis: evaluation and treatment. The Journal of the American Academy of Orthopaedic Surgeons. 2008 Jun:16(6):338-46 [PubMed PMID: 18524985]
Espert M, Anderson MR, Baumhauer JF. Current Concepts Review: Plantar Fibromatosis. Foot & ankle international. 2018 Jun:39(6):751-757. doi: 10.1177/1071100718768051. Epub 2018 Apr 5 [PubMed PMID: 29619843]
Loh B, Chen JY, Yew AK, Chong HC, Yeo MG, Tao P, Yeo NE, Koo K, Rikhraj Singh I. Prevalence of Metatarsus Adductus in Symptomatic Hallux Valgus and Its Influence on Functional Outcome. Foot & ankle international. 2015 Nov:36(11):1316-21. doi: 10.1177/1071100715595618. Epub 2015 Jul 22 [PubMed PMID: 26202480]