Introduction
Pigmented lesions of the skin are commonly called freckles. They include solar lentigo, congenital nevi, mucosal nevi, and special nevi of the palms and soles. This activity will help to differentiate the various pedal nevi from acral lentiginous melanoma clinically. Plantar melanomas are characteristically late to be diagnosed, have a poorer response to treatment, and have a significantly higher mortality rate when compared to more proximal melanomas.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
A severe childhood burn is strongly associated with an increased risk of melanoma, while more incremental occupational exposure does not confer an increased risk. These findings support the hypothesis that melanoma risk is affected primarily by intermittent intense sun exposure that paralyzes normal immune surveillance and destroys abnormal melanocytes. Sunburn in adolescence damages lifelong immune surveillance and disturbs normal apoptosis of neoplastic cells. Genetic susceptibility also may help account for melanoma in shaded areas. As many as 1 in 10 cases of melanoma may be linked to inherited faulty genes.[2]
Epidemiology
The actual increase in melanoma incidence is most likely due to an overall increase in the ultraviolet (UV) light exposure. Although melanoma, in general, is thought to be rare, the incidence of melanoma worldwide is rising dramatically, and despite increased efforts at screening, mortality rates have not appreciably improved. In the United States, melanoma is the fifth leading cancer in men and the seventh in women, and its incidence has doubled in the last ten years. In a study of data (1992 to 2004), researchers found that the actual incidence of melanoma (all thicknesses and among all socioeconomic levels) is increasing the case burden. The increase is from 4.7 to 7.7 cases per 100,000 older men and from 5.5 to 13.9 cases per 100,000 females. Although 5% of all melanomas are located on foot, pedal melanoma is relatively rare in whites. Among East Asians and darkly pigmented people, acral lentiginous melanoma is the most common subtype.[3]
Pathophysiology
Melanocytes are special dendritic cells derived from the neural crest that has the ability to spread over the entire surface of the body. This spreading ability could help account for melanoma’s ability to metastasize across tissue plains and through blood vessels, nerves, and lymphatics. This metastatic passport helps make melanoma more lethal than other skin cancers that are limited to adjacent spread. Although the foot receives less solar exposure, pedal melanoma is more lethal than even more proximal thigh melanoma. Although the 5-year survival rate for melanoma of the calf is 94%, the 5-year survival rate for foot melanoma is 77%. Acral melanoma has a significantly poorer prognosis than the other subtypes of melanomas.[4]
History and Physical
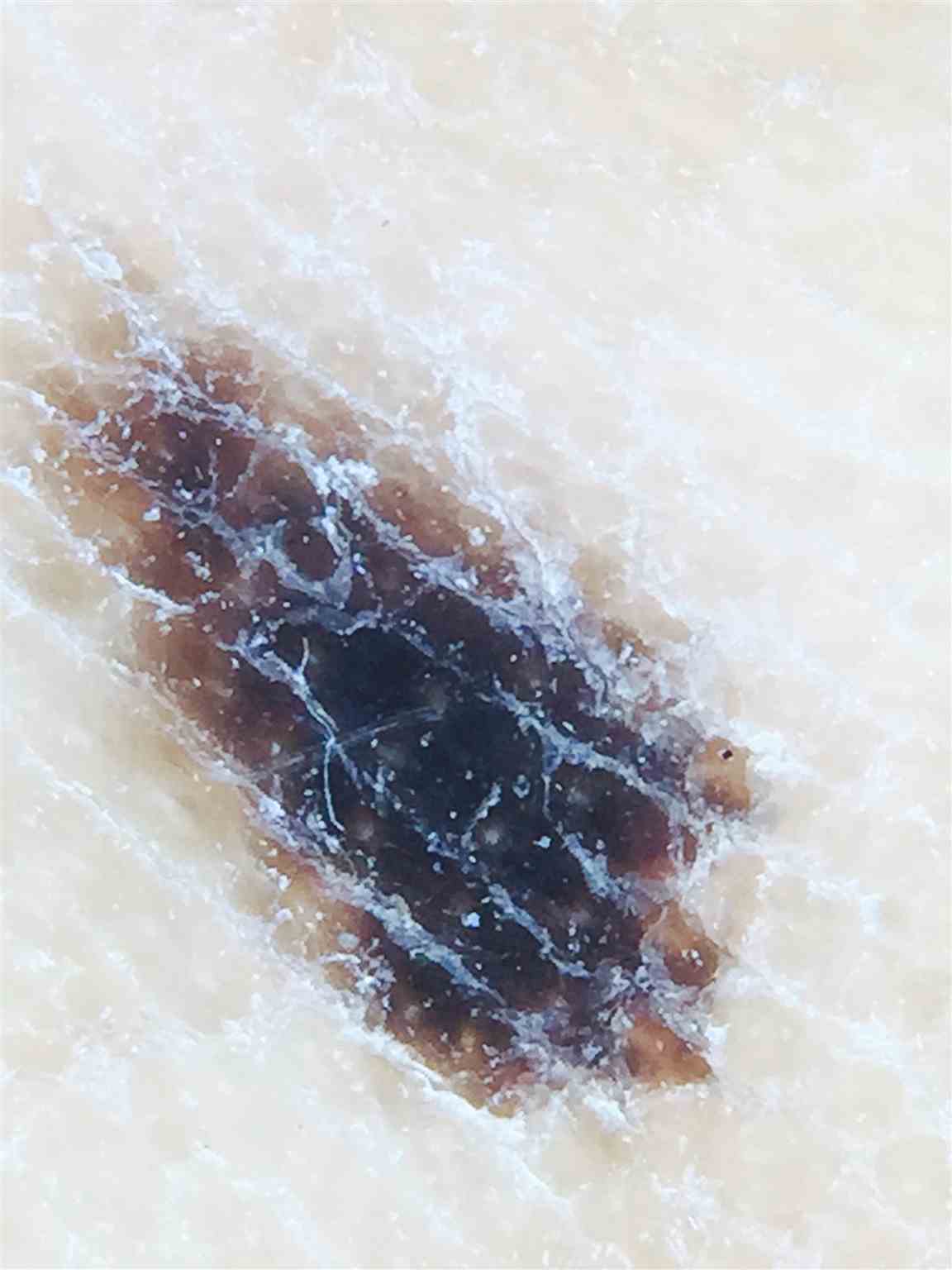
Patients may present with a changing plantar mole. However, acral melanomas typically are discovered only upon focused examination of the soles and toe webs. Anatomically, the palms and soles lack hair follicles and sebaceous glands but have many sweat ducts. The palms and soles are much thicker, and regular patterns are distorted by walking and grasping pressures. Simple clinical evaluation looking for asymmetry, irregular borders, color variation, diameter greater than 6 mm, and change over time or lesion elevation is important. Augmenting these clinical observations with dermoscopy can increase diagnostic acumen by 20%. A complete examination of the soles, toe web spaces, and nail units are important components of a lower extremity examination.[5][6]
Evaluation
In addition to evaluating the A through E characteristics of a pigmented lesion, there are specific dermoscopic patterns to guide examination. There are three benign patterns and one malignant dermoscopic pattern to consider. The parallel furrow pattern of linear pigmentation is benign over 93.2% of the time. The fibrillar pattern with pigmented furrows and fine angulated crossing filamentous, as well as the lattice-like pigment, are benign patterns. Most importantly, the parallel ridge pattern with wide diffuse pigmentation of the ridges predicts melanoma 93.7% of the time. Violation of the normal parallel furrow pattern indicates biopsy.[7]
Treatment / Management
An atypical nevus on the sole can be biopsied with a simple 2 mm punch. If initial wide excision is chosen, a 1 to 2 mm rim of normal-appearing skin, along with a cuff of sub-dermal fat, is recommended. Once melanoma is found by either the punch or total extensional biopsy, wider excision with surgical margins of 1cm for the 0 to 2 mm thick tumors and up to 5 cm for tumors that are over 2.1 mm in thickness can be planned. This may lead to extensive tissue loss that may require amputation. In general, small plantar melanoma excision sites are allowed to granulate. Once primary healing has taken place, plastic skin grafting and flaps can be used to restore weight-bearing function. Mohs microsurgery has been used to minimize tissue loss. An experienced oncology team is important to improve outcomes. The Melanoma Staging database is based on the clinical experiences in over 38,900 melanoma patients and incorporates a tumor, node, metastasis (TNM) system. It relies upon assessments of the primary tumor (T), regional lymph nodes (N), and distant metastatic sites (M). The Breslow thickness primarily determines the T and is modified by the mitotic rate of the tumor. The 10-year survival rate decreases progressively, from 96 percent with primary lesions <0.5 mm thick to 54 percent with lesions 4.01 to 6 mm thick.[8] The N or lymphatic node designation assesses regional lymph node spread and has a major negative impact on long-term survival. The sentinel lymph node biopsy (SLNB) is recommended for tumors equal to or greater than 0.75mm thick. If positive, complete lymph node dissection is recommended. Adjuvant interferon-alpha is then recommended in patients that have a life expectancy greater than ten years. Therapies that target T lymphocyte antigens can induce an anti-tumor immune response. Ipilimumab is an immune checkpoint inhibitor and has extended survival. Complications include exacerbation of pre-existing immune disorders. Anti-programmed cell death (PD-1) monoclonal antibodies like nivolumab and pembrolizumab have demonstrated more effective results than conventional drugs in clinical trials for a variety of advanced solid tumors, including melanoma, non-small cell lung carcinoma, and renal carcinoma. The five-year survival rate for plantar melanoma is 82% for lesions up to 1.49 mm and 0% for lesions over 3.5 mm.[9]
Differential Diagnosis
- Atypical mole
- Basal cell carcinoma
- Café au lait spots
- Cockade nevus
- Cutaneous melanoma
- Nevi of Ota and Ito
- Nevus spilus
- Nodular lesions
- Pyogenic granuloma
Pearls and Other Issues
Advising patients to use sunscreens, perform self-examinations, and avoid tanning beds helps prevent melanoma of all types. Early detection through complete lower extremity examination aided by dermoscopy should reduce the time to acral melanoma diagnosis and improve survival.[10]
Enhancing Healthcare Team Outcomes
The diagnosis and management of melanocytic nevi are best made with an interprofessional team that also includes the pharmacist and nurses; the latter two play a role in educating the public about prevention.
If melanocytic nevi are not diagnosed, the prognosis is poor. Thus to improve patient outcomes, a thorough exam of the skin is vital. Patients may present with a changing plantar mole. Acral melanomas typically are discovered only upon focused examination of the soles and toe webs. Simple clinical evaluation looking for asymmetry, irregular borders, color variation, diameter greater than 6 mm, and change over time or lesion elevation is important. If there is ever a doubt about a skin lesion, a biopsy should be performed.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
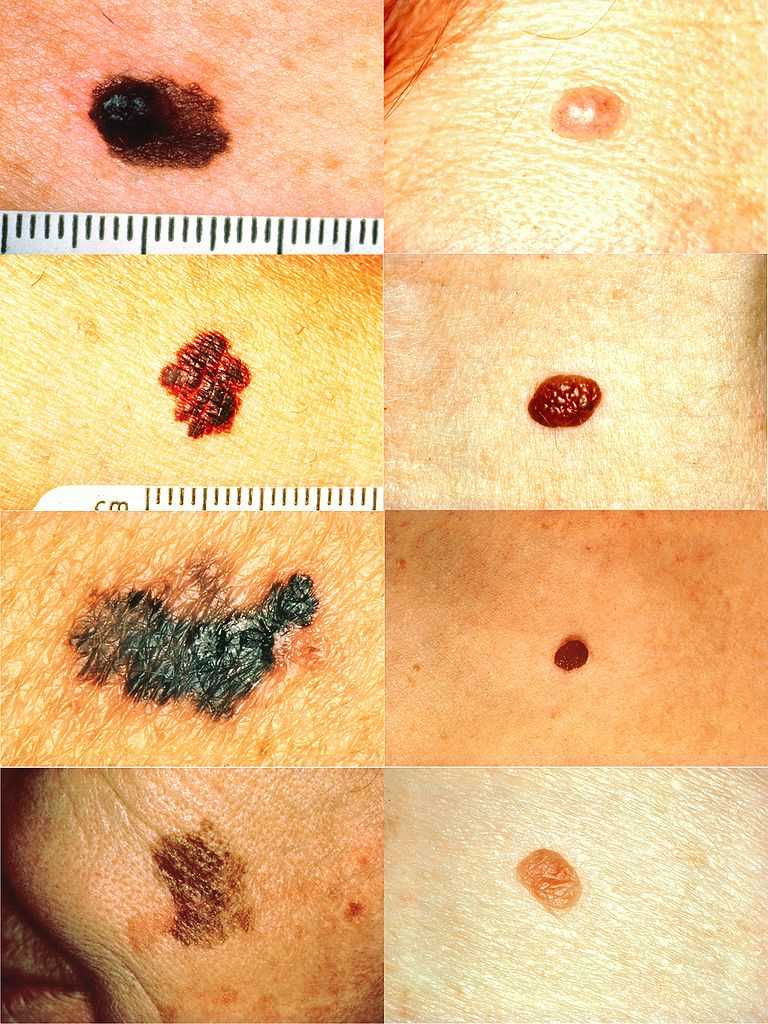
Part of the ABCDs for Detection of Melanoma. On the left side from top to bottom: melanomas showing (A) asymmetry, (B) a border that is uneven, ragged, or notched, (C) coloring of different shades of brown, black, or tan and (D) diameter that had changed in size. The normal moles on the right side do not have abnormal characteristics (no asymmetry, even border, even color, no change in diameter).
National Cancer Institute Skin Cancer Foundation
(Click Image to Enlarge)
References
Wang M, Xu Y, Wang J, Cui L, Wang J, Hu XB, Jiang HQ, Hong ZJ, Yuan SM. Surgical Management of Plantar Melanoma: A Retrospective Study in One Center. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2018 Jul-Aug:57(4):689-693. doi: 10.1053/j.jfas.2017.12.004. Epub 2018 Apr 6 [PubMed PMID: 29631972]
Level 2 (mid-level) evidenceWang B, Qu XL, Chen Y. Identification of the potential prognostic genes of human melanoma. Journal of cellular physiology. 2019 Jun:234(6):9810-9815. doi: 10.1002/jcp.27668. Epub 2018 Nov 30 [PubMed PMID: 30500072]
Bartoš V, Kullová M. Malignant Melanomas of the Skin Arising on the Feet. Klinicka onkologie : casopis Ceske a Slovenske onkologicke spolecnosti. 2018 Summer:31(4):289-292. doi: 10.14735/amko2018289. Epub [PubMed PMID: 30541312]
Palicka GA, Rhodes AR. Acral melanocytic nevi: prevalence and distribution of gross morphologic features in white and black adults. Archives of dermatology. 2010 Oct:146(10):1085-94. doi: 10.1001/archdermatol.2010.299. Epub [PubMed PMID: 20956637]
Bristow I, Bower C. Melanoma of the Foot. Clinics in podiatric medicine and surgery. 2016 Jul:33(3):409-22. doi: 10.1016/j.cpm.2016.02.008. Epub 2016 Apr 13 [PubMed PMID: 27215160]
Lallas A, Kyrgidis A, Koga H, Moscarella E, Tschandl P, Apalla Z, Di Stefani A, Ioannides D, Kittler H, Kobayashi K, Lazaridou E, Longo C, Phan A, Saida T, Tanaka M, Thomas L, Zalaudek I, Argenziano G. The BRAAFF checklist: a new dermoscopic algorithm for diagnosing acral melanoma. The British journal of dermatology. 2015 Oct:173(4):1041-9. doi: 10.1111/bjd.14045. Epub 2015 Oct 1 [PubMed PMID: 26211689]
Bristow IR, de Berker DA, Acland KM, Turner RJ, Bowling J. Clinical guidelines for the recognition of melanoma of the foot and nail unit. Journal of foot and ankle research. 2010 Nov 1:3():25. doi: 10.1186/1757-1146-3-25. Epub 2010 Nov 1 [PubMed PMID: 21040565]
Crompton JG, Gilbert E, Brady MS. Clinical implications of the eighth edition of the American Joint Committee on Cancer melanoma staging. Journal of surgical oncology. 2019 Jan:119(2):168-174. doi: 10.1002/jso.25343. Epub 2018 Dec 21 [PubMed PMID: 30575031]
Richtig E. ASCO Congress 2018: melanoma treatment. Memo. 2018:11(4):261-265. doi: 10.1007/s12254-018-0455-4. Epub 2018 Nov 20 [PubMed PMID: 30595751]
Nevares-Pomales OW, Sarriera-Lazaro CJ, Barrera-Llaurador J, Santiago-Vazquez M, Lugo-Fagundo N, Sanchez JE, Sanchez JL. Pigmented Lesions of the Nail Unit. The American Journal of dermatopathology. 2018 Nov:40(11):793-804. doi: 10.1097/DAD.0000000000001106. Epub [PubMed PMID: 30339563]