Introduction
Canaliculitis is inflammation of the lacrimal canaliculus. It is an uncommon condition which ophthalmologists frequently misdiagnose. The condition is challenging to eradicate.[1][2][3] The condition may be misdiagnosed and treated as conjunctivitis, blepharitis, dacryocystitis, mucocele, and chalazion, thus leading to prolonged morbidity to the patient. In Harrison’s Principles of Internal Medicine, authors describe it as the "most misdiagnosed disease." Von Graefe was the first person to recognize the cause of canaliculitis as an infectious entity.
Canaliculitis can be primary or secondary. Secondary canaliculitis is often seen as a complication of punctal or intercanalicular plug insertion for treatment of dry eye.
The canaliculi are an important component of the proximal part of the lacrimal drainage system. They begin at the lacrimal puncta, and in most patients, converge to form the common canaliculus. These canals travel through the eyelids for approximately 8 millimeters. The upper canaliculus is shorter and narrower than the lower, and it has a sharp angulation before merging with the lower canaliculus to form the common canaliculus. The lower canaliculus is almost entirely horizontal.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Traditionally, Actinomyces israelii was thought to be the organism responsible for canaliculitis, causing this condition to be variously named as streptothrix canaliculitis or streptothricosis.[4] This organism was earlier classified as a fungus but is now considered an obligate or facultative anaerobic gram-positive Bacillus. Recent studies, however, demonstrate an increased incidence of Staphylococcus and Streptococcus. Many other organisms like Eikenella, Lactococcus, Nocardia, and fungi also have been isolated from patients with canaliculitis. Studies have demonstrated that Pseudomonas aeruginosa is the most common organism isolated in plug-associated canaliculitis; whereas, other studies implicate Hemophilus species, Actinomyces species along with Pseudomonas.
Epidemiology
Canaliculitis is a relatively uncommon disease.[2] Studies have demonstrated that it accounts for up to 2% to 4% of lacrimal diseases. It can occur at any age ranging from 5 years to 90 years, and the mean age has been estimated to be about 59 years. Most studies have found a female preponderance. This could be due to hormonal factors which can affect tear production rendering the canaliculus prone to microbial invasion. Use of cosmetics and clogging of the canaliculi by cosmetic particles have been postulated in some as a cause. Secondary plug-related canaliculitis also is seen more commonly in females, probably because of a larger number of female patients who are treated with plug placement for dry eye symptoms. Most studies have found a higher incidence of involvement of the lower canaliculus.
Pathophysiology
Canaliculitis can be classified into primary and secondary. [3]Primary canaliculitis is an inflammation of the lacrimal canaliculus, usually caused by an infection. Secondary canaliculitis is an inflammation of the lacrimal canaliculus, secondary to punctal canalicular plug insertion or canalicular intubation.
History and Physical
Because of the varying presentation of this condition, canaliculitis may be misdiagnosed, or there may be a delay in diagnosis. The symptoms are usually unilateral. Patients may present with watering, discharge, a pouting punctum, or a medial canthal swelling; these symptoms may be confused with chronic conjunctivitis, inflamed chalazion or acute dacryocystitis. Mattering on the eyelids, expression of yellowish granules, concretions, and stones by massage are other presentations. These yellowish granules are called sulfur granules, and they are thought to be caused by Actinomyces species. Some studies have shown that watering and ocular discomfort are the most typical symptoms while other studies found ocular discharge to be the most common presentation. One may see other additional symptoms in secondary canaliculitis such as intermittent blood-stained tears, blood-tinged discharge, or presence of a mass protruding from the punctum.[1][2][5]
A thorough examination is mandatory, and a high index of suspicion is needed to arrive at a correct diagnosis of canaliculitis. Historically, the presence of concretions was considered to be firm evidence of canaliculitis, which was later extended to include pericanalicular inflammation and pouting puncta. Various studies demonstrate that the most common signs in primary canaliculitis are punctal swelling, eyelid swelling, and discharge or concretions from the punctum. Concretions are thought to be an indicator of recurrence and require surgical removal to prevent further attacks. Cases of secondary canaliculitis may reveal signs of canalicular inflammation, an inflammatory mass protruding from the punctum, granuloma formation, blood-stained discharge, presence of canaliculitis and dacryoliths, eyelid swelling and erythema. Lacrimal irrigation reveals intact patency of the lacrimal system in canaliculitis, even in the presence of canaliculitis. Irrigation and probing may help localize a migrated punctal plug in patients with secondary canaliculitis.
Evaluation
Clinical examination in cases of canaliculitis should include slit lamp examination of the upper and lower puncta, medial canthal area, conjunctival fornices, and lacrimal syringing. Although the diagnosis of canaliculitis is clinical in most cases, supportive investigations would help to confirm the diagnosis or assist in making a conclusive diagnosis in patients with ambiguous symptoms.[1][6]
The following investigations may be done in patients with canaliculitis.
Microbiological Culture
Cultures of the punctal discharge, concretions, abscesses, and conjunctival swabs may be obtained. Usually, aerobic and anaerobic cultures are requested. However, in recurrent or atypical cases, fungal and mycobacterial cultures may also be done.
Histopathology
Histopathological examination is most commonly performed on the expressed concretions. They may show the presence of actinomyces or may consist of sterile necrotic tissue. In secondary canaliculitis, histopathological examination of an extruded foreign body may show an inflammatory reaction at the margins. Histopathological features of pyogenic granuloma also may be seen.
Ultrasound Biomicroscopy (UBM)
UBM, with a frequency of 50 MHz and a resolution of 40 microns, is one of the best methods for investigating the canalicular system. Its noninvasive nature adds to its advantages. It can demonstrate canalicular changes and canaliculith.
Dacryoendoscopy
This is an important investigation, especially in cases of secondary canaliculitis, to localize migrated punctal plugs.
Dacryocystography
This may demonstrate signs of canaliculitis like filling defects, dilatation, raggedness, beading, and diverticula formation.
Treatment / Management
Medical management of new-onset primary canaliculitis is said to be effective in patients who present early. Conservative medical management includes topical and systemic antibiotics, warm compresses, local massage, syringing, and irrigation. [7][8]Numerous studies have demonstrated conservative management to be ineffective in 80% of cases. The presence of concretions may help to shield the bacteria from the antibiotics, thus promoting resistance and inadequate response to treatment. Many authors now emphasize early diagnosis and prompt institution of surgical management for the management of canaliculitis.(B3)
The different surgical options include punctual dilatation or punctoplasty with curettage, canaliculotomy, canaliculoplasty with intubation, and punctum-sparing canaliculotomy with monocanalicular intubation.[7] Most studies have found canaliculotomy to be a safe and effective procedure. Canaliculotomy involves placing an incision on the posterior aspect of the canaliculus and removing the stones, concretions, necrotic epithelium and other debris, then irrigating with antibiotic solution. The incision may be left open or closed with or without a stent.[2]
Secondary canaliculitis is found to have a very poor response to medical management. Canaliculotomy with the removal of the plug is considered the treatment of choice for plug-related canaliculitis. Recurrent or complicated cases may require dacryocystorhinostomy, removal of any intracanalicular foreign bodies or debris, and stent placement.
Differential Diagnosis
- Carcinoma of the lacrimal canaliculus
- Chronic conjunctivitis
- Dacryocystitis
- Migrated punctal plug
Pearls and Other Issues
Canaliculitis is a condition which is commonly misdiagnosed or diagnosed late. A high index of suspicion is required. An early diagnosis is vital for a complete cure, and chronic cases have more complications and a poorer prognosis.
Enhancing Healthcare Team Outcomes
Canaliculitis is an uncommon condition, which is often challenging to the ophthalmologist as it is frequently misdiagnosed and very difficult to eradicate. Secondary canaliculitis due to punctal plugs is very common. Practitioners should always look for this during follow-up of patients with punctal plug for dry eye. Often, the patient will not remember having had plugs inserted.
Media
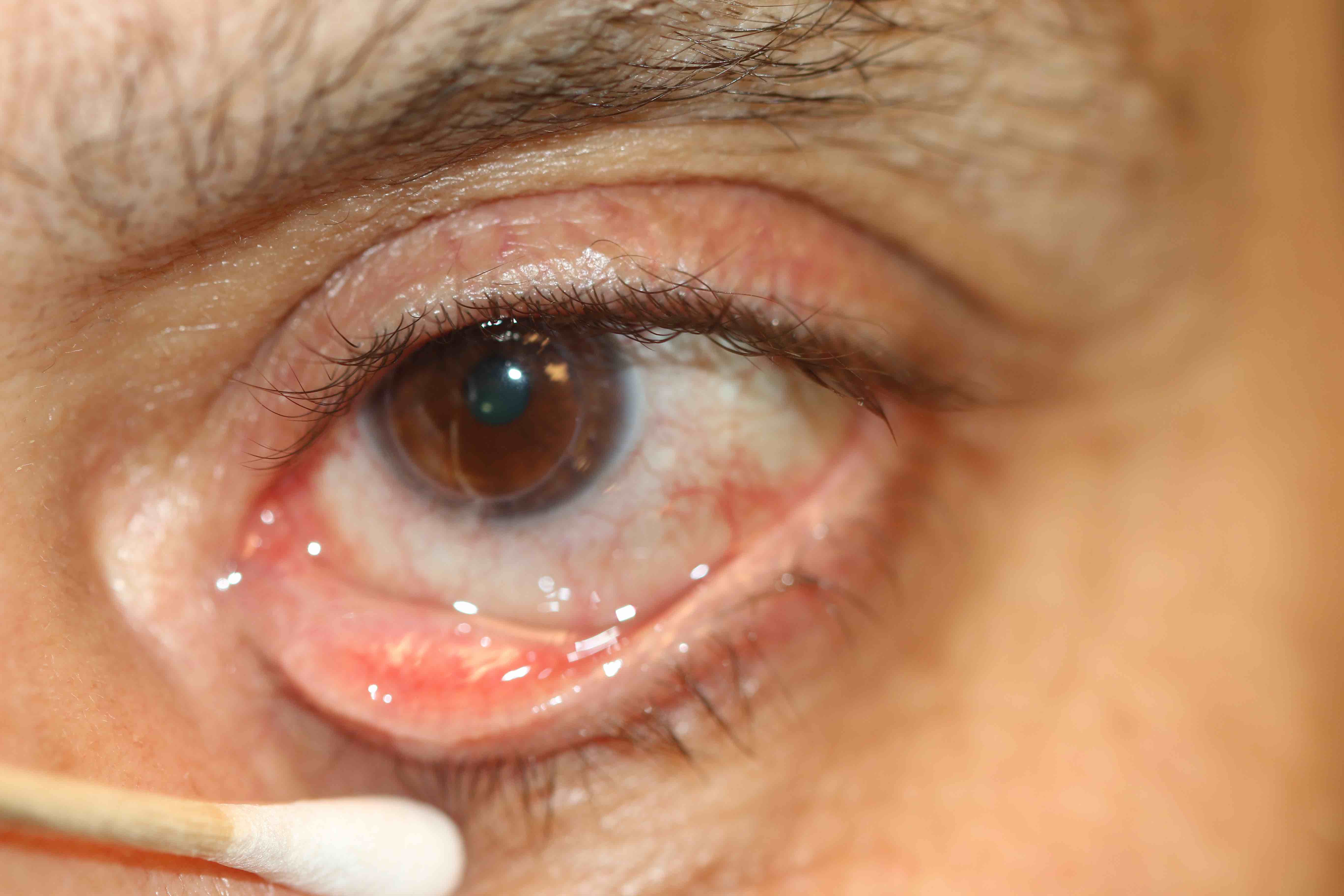
(Click Image to Enlarge)
Upper canaliculitis with swelling of the medial upper eyelid, mucoid discharge from the upper punctum and a history of previous placement of a Herrick intra-canalicular plug. The intracanalicular plug was removed via an open dacryocystorhinostomy and the debris within the canaliculus was removed. Contributed by Prof. BCK Patel MD
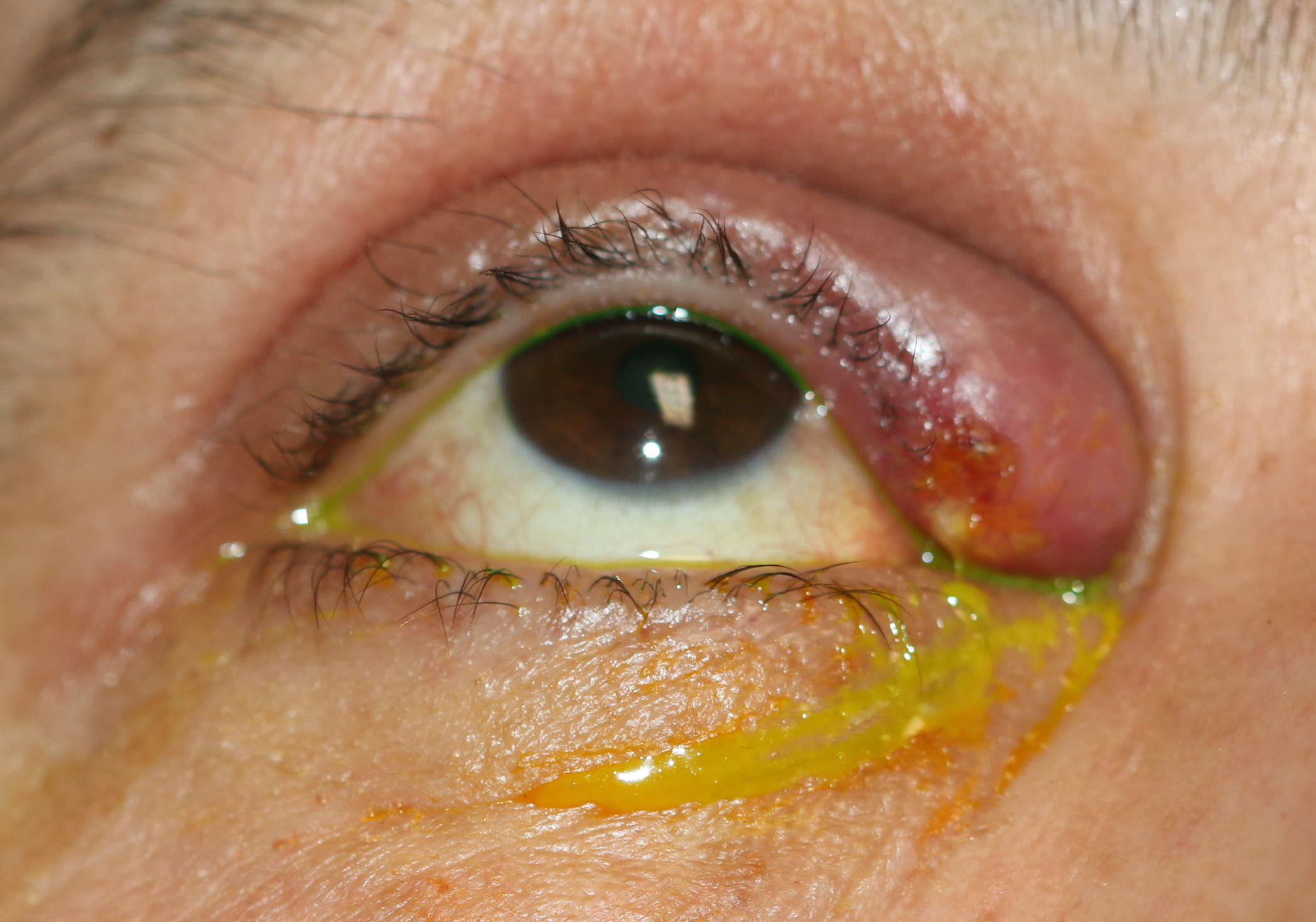
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Gogandy M, Al-Sheikh O, Chaudhry I. Clinical features and bacteriology of lacrimal canaliculitis in patients presenting to a tertiary eye care center in the Middle East. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2014 Jan:28(1):31-5. doi: 10.1016/j.sjopt.2013.09.006. Epub [PubMed PMID: 24526855]
Zaveri J, Cohen AJ. Lacrimal canaliculitis. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2014 Jan:28(1):3-5. doi: 10.1016/j.sjopt.2013.11.003. Epub 2013 Nov 13 [PubMed PMID: 24526851]
Freedman JR, Markert MS, Cohen AJ. Primary and secondary lacrimal canaliculitis: a review of literature. Survey of ophthalmology. 2011 Jul-Aug:56(4):336-47. doi: 10.1016/j.survophthal.2010.12.001. Epub 2011 May 28 [PubMed PMID: 21620429]
Level 3 (low-level) evidenceMehrotra N, Baidya A, Brijwal M, Aggarwal R, Chaudhry R. Actinomycosis of eye: Forgotten but not uncommon. Anaerobe. 2015 Oct:35(Pt B):1-2. doi: 10.1016/j.anaerobe.2015.06.001. Epub 2015 Jun 6 [PubMed PMID: 26057988]
Huang YY, Yu WK, Tsai CC, Kao SC, Kau HC, Liu CJ. Clinical features, microbiological profiles and treatment outcome of lacrimal plug-related canaliculitis compared with those of primary canaliculitis. The British journal of ophthalmology. 2016 Sep:100(9):1285-9. doi: 10.1136/bjophthalmol-2015-307500. Epub 2015 Dec 23 [PubMed PMID: 26701689]
Kaliki S, Ali MJ, Honavar SG, Chandrasekhar G, Naik MN. Primary canaliculitis: clinical features, microbiological profile, and management outcome. Ophthalmic plastic and reconstructive surgery. 2012 Sep-Oct:28(5):355-60. doi: 10.1097/IOP.0b013e31825fb0cd. Epub [PubMed PMID: 22836798]
Level 2 (mid-level) evidenceKim UR, Wadwekar B, Prajna L. Primary canaliculitis: The incidence, clinical features, outcome and long-term epiphora after snip-punctoplasty and curettage. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2015 Oct-Dec:29(4):274-7. doi: 10.1016/j.sjopt.2015.08.004. Epub 2015 Sep 7 [PubMed PMID: 26586978]
Xu J, Liu Z, Mashaghi A, Sun X, Lu Y, Li Y, Wu D, Yang Y, Wei A, Zhao Y, Lu C, Hong J. Novel Therapy for Primary Canaliculitis: A Pilot Study of Intracanalicular Ophthalmic Corticosteroid/Antibiotic Combination Ointment Infiltration. Medicine. 2015 Sep:94(39):e1611. doi: 10.1097/MD.0000000000001611. Epub [PubMed PMID: 26426646]
Level 3 (low-level) evidence