Introduction
Respiratory muscle strength training (RMST) comprises exercises and techniques designed to enhance the strength and endurance of respiratory muscles, such as the diaphragm and intercostal muscles. Various disorders affect the respiratory system and may, directly or indirectly, cause dysfunction of either inspiration, expiration, or both. RMST exercises are particularly beneficial for athletes but are often employed as a treatment or rehabilitation tool for patients with respiratory conditions that affect respiratory muscles, such as critical illness, chronic obstructive pulmonary disease (COPD), asthma, or respiratory muscle weakness. RMST can also be paired with other forms of pulmonary rehabilitation to remedy respiratory dysfunction and improve clinical outcomes. This article reviews the physiology, types of different respiratory muscle training, the indications and contraindications for RMST, and discusses relevant clinical significance for adult patients.
Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Function
Physiology of Respiratory Muscle Strengthening
Respiratory muscles are structurally similar to other skeletal muscles. However, respiratory muscles are distinct because contraction causes changes in chest wall motion during inspiration and expiration.[1] Similar to the musculature of the upper and lower extremities, respiratory muscles demonstrate plasticity during resistance and endurance training by remodeling their cross-sectional area, muscle fiber phenotype (fast twitch, slow twitch), and threshold for activation.[2] Introducing respiratory muscles to resistive loads for prolonged periods and varying these loads in response to tolerance is just one way to provide progressive overload. Improving respiratory muscle strength and endurance enhances chest wall mechanics and lung volumes and reduces the clinical incidence of pulmonary diseases, such as pneumonia and atelectasis. When respiratory muscles are progressively overloaded, their physiologic response is to hypertrophy, improving contractile force.[3]
Definition of Respiratory Muscle Strength Training
RMST is employed in health care settings such as intensive care units and outpatient and inpatient rehabilitation units to improve the strength and endurance of inspiratory and expiratory muscles. During RMST, patients challenge inhalation or expiration to undergo a time-limited scheduled therapy protocol that includes inspiratory muscle strength (IMS) training, expiratory muscle strength (EMS) training, or a combination thereof. IMS training requires patients to use handheld devices to complete exercises intended to improve the strength and endurance of the inspiratory musculature, including, but not limited to, the diaphragm, external intercostal, and parasternal intercostal muscles.[4] EMS training requires patients to complete exercises that improve the strength and endurance of expiratory muscles, including, but not limited to, the internal intercostal and abdominal muscles.[5]
Respiratory Muscle Strength Training Devices and Protocols
EMS and IMS training utilize the following categories of devices: incentive spirometry (IS), pressure threshold devices, and resistance devices. Pressure threshold devices have a spring-loaded, 1-way calibrated valve targeting a certain threshold of maximal pressure on muscles as the patient inhales or exhales; turning the spring increases or decreases the threshold.[6] The target pressure must be reached for air to flow through the device to facilitate exhalation or inspiration. The resistance the device applies during inspiration or expiration is independent of the volume and rate of airflow through the device.[7] Resistance devices provide constant resistance to airflow. Users can increase or decrease resistance by changing the number or size of the openings through which air can flow.[8] Incentive spirometry devices promote natural deep, slow breathing that improves lung volumes based on feedback from the device to the preset airflow during inspiration.[9]
Establishing the initial training load for either IMS or EMS training requires a pressure-measuring device such as a digital manometer, a peak flow meter, or a pressure threshold device. Depending on the goal of the RMST protocol, exercises are initiated at a percentage of the maximum inspiratory/maximum expiratory pressure.[10] Strengthening protocols typically use loads between 55% and 80% of this ratio with fewer repetitions.[11] Endurance protocols can use 30% to 40% of maximum inspiratory/maximum expiratory pressure with more repetitions.[12]
The protocol for RMST considers the clinical indication for training, underlying diagnoses, and tolerance to therapy. Training sessions are typically conducted 2 to 3 times daily, 3 to 5 days per week, for a 5- to 6-week period; patients perform more than 10 repetitions per session under the guidance of a speech-language pathologist. Patients can also perform these exercises individually at home.[13] The training intensity can be changed by varying the number of training sessions, sets, or repetitions and the duration of sessions to promote muscle adaptation and improve respiratory muscle strength or endurance.
Indications for Respiratory Muscle Strength Training
Inspiratory muscle strength training
Conditions for which IMS training is indicated include, but are not limited to:
- Weaning from mechanical ventilation
- Multiple sclerosis
- Spinal cord injury
- Congestive heart failure
- Chronic obstructive pulmonary disease
- Paradoxical vocal fold motion
- Parkinson disease [14][15][16][17][18]
Expiratory muscle strength training
Conditions for which EMS training is indicated include, but are not limited to:
- Amyotrophic lateral sclerosis
- Spinal cord injury
- Swallowing dysfunction and phonation in Parkinson's Disease [19][20][21]
Contraindications to Respiratory Muscle Strength Training
Although RMS training is generally well-tolerated, contraindications for the use of IMS and EMS training include uncontrolled disorders for which exercise is generally contraindicated:
- Acute cerebrovascular accident
- Untreated hypertension
- Acute delirium
- Perforated tympanic membrane
- Spontaneous pneumothorax
- Hemodynamic instability
- Rib fractures
- Osteoporosis
- Recent abdominal surgery [22]
Potential Adverse Effects of Respiratory Muscle Strength Training
There are no formally recognized adverse effects to RMST. However, muscle fatigue may occur when patients breathe at a high proportion of their functional reserve or with a prolonged inspiratory time. Fatigue may explain why adherence to RMST is often low; up to 50% of patients fail to complete the studies. Other symptoms, such as headache or dizziness, have been reported in athletes who underwent RMST.[23]
Respiratory Muscle Strength Training Techniques
During IMS training, patients inhale against a resistive load provided by a handheld pressure threshold or resistance device.[24] Each IMS training protocol is individualized, and variables such as resistive load, repetition, and frequency of attempts may change throughout training. IMS training is indicated when a decreased ability to perform inspiration, characterized by a low maximum inspiratory pressure, is noted or impairment in vocal fold movement is evidenced. IMS training primarily targets the diaphragm and external intercostal muscles.[25]
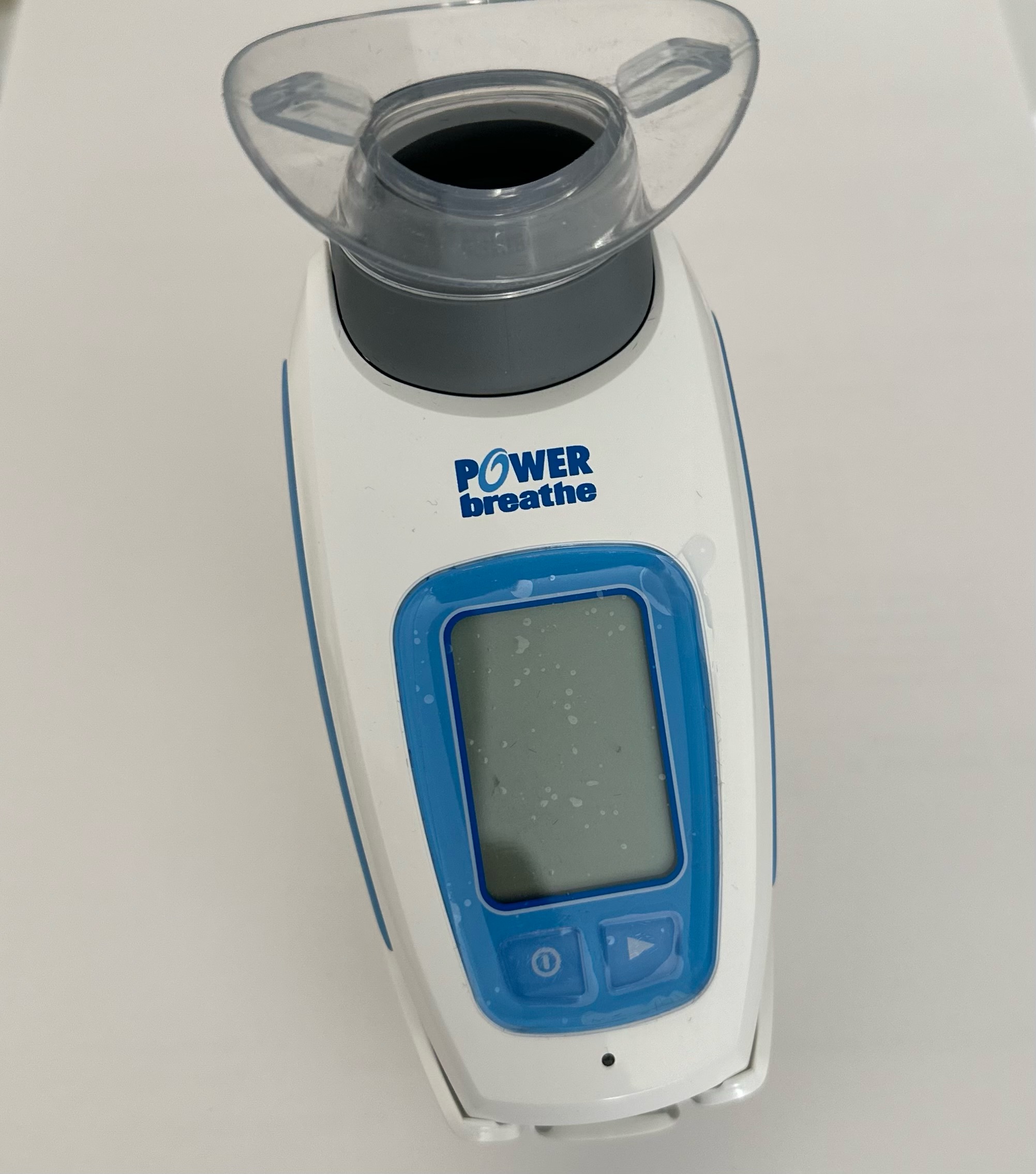
During EMS training, patients exhale against a resistive load provided by a handheld pressure threshold or resistance device (see Image. Example of Expiratory Muscle Trainer Portable Device). EMS training is indicated for patients with weak cough, swallowing dysfunction, poor airway protection or secretion management, and poor vocal intensity to improve maximum expiratory pressure.[26] EMS training primarily targets the internal intercostal and abdominal muscles.[27] The goals of EMS training can include strengthening cough, improving clearance of secretions, and increasing vocal intensity.
Several recent developments in RMST employ new and portable devices, including the digital portable inspiratory muscle trainer device, POWERbreathe™ K3 manufactured by POWERbreathe International Ltd. (see Image. Example Device For Digital Portable Inspiratory Muscle Training). This device includes the Breathe-Link Medic computer software, which provides real-time feedback and measures parameters such as maximum inspiratory pressure and peak inspiratory flow. This type of device has been used in several studies to assess the role of muscle strengthening in respiratory and cardiovascular outcomes.[28][29][30]
Another innovative approach utilizes distinctly sized leaks to simulate various types of muscle training, including power, strength, and endurance. This technique is available through the RT2 (DeVilbiss Healthcare, Wollaston, UK) or TRAINAIR (Project Electronics Limited, Kent, UK) devices.[31]
Clinical Significance
Clinical Efficacy of Respiratory Muscle Strength Training
RMST can alleviate shortness of breath, increase exercise tolerance, and enhance the quality of life for patients with respiratory conditions. The clinical efficacy of RMST is evaluated during rehabilitation in critically ill adults or in outpatient settings by assessing changes in maximal inspiratory and expiratory pressures, lung volumes, and clinical endpoints. The role of RMST has been evaluated in several clinical conditions, including COPD, spinal cord injury, sleep apnea, asthma, various neuromuscular disorders, and exercise-induced paradoxical vocal fold motion.
An examination of the effectiveness of IMS training as a standalone intervention and in combination with pulmonary rehabilitation in patients with COPD revealed that when used in conjunction with pulmonary rehabilitation, IMS training did not significantly improve dyspnea, functional exercise capacity, and quality of life compared to the rehabilitation alone. However, IMS training will likely improve these outcomes when administered as a standalone treatment.[32] In a systematic review of randomized trials, IMS training substantially improved maximal and maximum expiratory pressure compared to control groups. These findings suggested that respiratory RMS positively impacts respiratory function and may improve clinical outcomes in patients with chronic respiratory disorders.[33] Furthermore, IMS training using a resistive loading device can increase maximum inspiratory pressure and improve weaning outcomes in patients with severe COPD who failed to wean off mechanical ventilation. In addition, this intervention improved exercise capacity in patients who have already weaned from mechanical ventilation.[34]
The feasibility and efficacy of RMST were assessed in individuals with impaired respiratory muscle strength secondary to disorders such as spinal cord injury and obstructive sleep apnea. The results of a 3-month pilot feasibility study demonstrated that when combined with oropharyngeal exercises, RMST was feasible and improved maximum inspiratory pressure without significantly affecting maximum expiratory pressure, lung function, or sleep apnea severity.[30]
A systematic research analysis on adults with neuromuscular disorders indicated that maximum expiratory and inspiratory pressures were improved following RMST compared to the control group without significantly affecting cough, dyspnea, physical capacity, or quality of life.[35] Another systematic review of studies on adults with mild-to-moderate asthma revealed a significant improvement in inspiratory muscle strength following an IMS training, without effect on expiratory muscle strength or lung function.[36]
IMS training could potentially treat athletes with paradoxical vocal fold motion induced by exercise. This training has demonstrated potential benefits, such as enhanced respiratory muscle strength and increased inspiratory laryngeal aperture size. However, improving the ability of inspiratory accessory muscles to generate increased flow may not be advantageous if the laryngeal patency remains the limiting factor. Nonetheless, research has indicated that IMS training can result in laryngeal abduction in healthy individuals.[37]
In patients with long-term COVID-19 symptoms, the inspiratory muscle function variables demonstrated an acceptable level of discrimination in evaluating the efficacy of respiratory muscle training programs. Among these variables, maximum inspiratory pressure demonstrated the greatest discriminative ability, with a change of 22.1% in predicted values deemed clinically significant.[38]
Enhancing Healthcare Team Outcomes
Identifying patients who can tolerate and benefit from RNST requires a collaborative effort among healthcare professionals, including physicians, advanced practitioners, nurses, speech-language pathologists, respiratory therapists, and others. Interprofessional team members must possess clinical skills and expertise when diagnosing, evaluating, and treating patients with respiratory muscle weakness. Biosocial barriers that could interfere with program adherence and lead to relapse should be identified. Regardless of the clinical setting where RMST is practiced, consultation with a trained healthcare professional is essential when evaluating respiratory dysfunction and establishing an RMST regimen which, alongside medical management and nursing care, can help prevent adverse outcomes.
Collaboration among interdisciplinary team members improves the safety of patients undergoing RMST through appropriate patient selection, refining evidence-based guidelines, and establishing IMS and EMS training and patient-specific protocols. Healthcare professionals can improve clinical outcomes through care coordination by actively participating in patients' RMST protocols, determining whether adjustments are needed to improve patient tolerance, and evaluating if an underlying process is inhibiting their progress.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Aliverti A. The respiratory muscles during exercise. Breathe (Sheffield, England). 2016 Jun:12(2):165-8. doi: 10.1183/20734735.008116. Epub [PubMed PMID: 27408635]
Gransee HM, Mantilla CB, Sieck GC. Respiratory muscle plasticity. Comprehensive Physiology. 2012 Apr:2(2):1441-62. doi: 10.1002/cphy.c110050. Epub [PubMed PMID: 23798306]
Menezes KK, Nascimento LR, Ada L, Polese JC, Avelino PR, Teixeira-Salmela LF. Respiratory muscle training increases respiratory muscle strength and reduces respiratory complications after stroke: a systematic review. Journal of physiotherapy. 2016 Jul:62(3):138-44. doi: 10.1016/j.jphys.2016.05.014. Epub 2016 Jun 16 [PubMed PMID: 27320833]
Level 1 (high-level) evidenceCraighead DH, Freeberg KA, McCarty NP, Rossman MJ, Moreau KL, You Z, Chonchol M, Seals DR. Inspiratory muscle strength training for lowering blood pressure and improving endothelial function in postmenopausal women: comparison with "standard of care" aerobic exercise. Frontiers in physiology. 2022:13():967478. doi: 10.3389/fphys.2022.967478. Epub 2022 Aug 29 [PubMed PMID: 36105300]
Brooks M, McLaughlin E, Shields N. Expiratory muscle strength training improves swallowing and respiratory outcomes in people with dysphagia: A systematic review. International journal of speech-language pathology. 2019 Feb:21(1):89-100. doi: 10.1080/17549507.2017.1387285. Epub 2017 Nov 1 [PubMed PMID: 29090601]
Level 1 (high-level) evidenceBaker S, Davenport P, Sapienza C. Examination of strength training and detraining effects in expiratory muscles. Journal of speech, language, and hearing research : JSLHR. 2005 Dec:48(6):1325-33 [PubMed PMID: 16478374]
Chen RC, Que CL, Yan S. Introduction to a new inspiratory threshold loading device. The European respiratory journal. 1998 Jul:12(1):208-11 [PubMed PMID: 9701439]
Palermo AE, Butler JE, Boswell-Ruys CL. Comparison of two inspiratory muscle training protocols in people with spinal cord injury: a secondary analysis. Spinal cord series and cases. 2023 Aug 12:9(1):42. doi: 10.1038/s41394-023-00594-2. Epub 2023 Aug 12 [PubMed PMID: 37573384]
Level 3 (low-level) evidenceHristara-Papadopoulou A, Tsanakas J, Diomou G, Papadopoulou O. Current devices of respiratory physiotherapy. Hippokratia. 2008:12(4):211-20 [PubMed PMID: 19158964]
Anand S, El-Bashiti N, Sapienza C. Effect of training frequency on maximum expiratory pressure. American journal of speech-language pathology. 2012 Nov:21(4):380-6. doi: 10.1044/1058-0360(2012/11-0048). Epub 2012 May 24 [PubMed PMID: 22628108]
Rehder-Santos P, Minatel V, Milan-Mattos JC, Signini ÉF, de Abreu RM, Dato CC, Catai AM. Critical inspiratory pressure - a new methodology for evaluating and training the inspiratory musculature for recreational cyclists: study protocol for a randomized controlled trial. Trials. 2019 May 7:20(1):258. doi: 10.1186/s13063-019-3353-0. Epub 2019 May 7 [PubMed PMID: 31064379]
Level 1 (high-level) evidenceÁlvarez-Herms J, Julià-Sánchez S, Corbi F, Odriozola-Martínez A, Burtscher M. Putative Role of Respiratory Muscle Training to Improve Endurance Performance in Hypoxia: A Review. Frontiers in physiology. 2018:9():1970. doi: 10.3389/fphys.2018.01970. Epub 2019 Jan 15 [PubMed PMID: 30697170]
Gonçalo Silva GA, Nogueira IDB, da Silva Chiappa GR, Nogueira PAMS. Efficacy of home-based inspiratory muscle training in patients post-covid-19: Protocol for a randomized clinical trial. PloS one. 2023:18(5):e0279310. doi: 10.1371/journal.pone.0279310. Epub 2023 May 4 [PubMed PMID: 37141260]
Level 1 (high-level) evidenceRietberg MB, Veerbeek JM, Gosselink R, Kwakkel G, van Wegen EE. Respiratory muscle training for multiple sclerosis. The Cochrane database of systematic reviews. 2017 Dec 21:12(12):CD009424. doi: 10.1002/14651858.CD009424.pub2. Epub 2017 Dec 21 [PubMed PMID: 29267988]
Level 1 (high-level) evidenceZhuang J, Jia J. Effects of Respiratory Muscle Strength Training on Respiratory-Related Impairments of Parkinson's Disease. Frontiers in aging neuroscience. 2022:14():929923. doi: 10.3389/fnagi.2022.929923. Epub 2022 Jun 30 [PubMed PMID: 35847666]
Sheel AW, Reid WD, Townson AF, Ayas NT, Konnyu KJ, Spinal Cord Rehabilitation Evidence Research Team. Effects of exercise training and inspiratory muscle training in spinal cord injury: a systematic review. The journal of spinal cord medicine. 2008:31(5):500-8 [PubMed PMID: 19086707]
Level 1 (high-level) evidenceFigueiredo RIN, Azambuja AM, Cureau FV, Sbruzzi G. Inspiratory Muscle Training in COPD. Respiratory care. 2020 Aug:65(8):1189-1201. doi: 10.4187/respcare.07098. Epub 2020 Mar 24 [PubMed PMID: 32209709]
Mathers-Schmidt BA, Brilla LR. Inspiratory muscle training in exercise-induced paradoxical vocal fold motion. Journal of voice : official journal of the Voice Foundation. 2005 Dec:19(4):635-44 [PubMed PMID: 16112543]
Plowman EK, Watts SA, Tabor L, Robison R, Gaziano J, Domer AS, Richter J, Vu T, Gooch C. Impact of expiratory strength training in amyotrophic lateral sclerosis. Muscle & nerve. 2016 Jun:54(1):48-53. doi: 10.1002/mus.24990. Epub 2016 Mar 3 [PubMed PMID: 26599236]
Roth EJ, Stenson KW, Powley S, Oken J, Primack S, Nussbaum SB, Berkowitz M. Expiratory muscle training in spinal cord injury: a randomized controlled trial. Archives of physical medicine and rehabilitation. 2010 Jun:91(6):857-61. doi: 10.1016/j.apmr.2010.02.012. Epub [PubMed PMID: 20510974]
Level 1 (high-level) evidencevan de Wetering-van Dongen VA, Kalf JG, van der Wees PJ, Bloem BR, Nijkrake MJ. The Effects of Respiratory Training in Parkinson's Disease: A Systematic Review. Journal of Parkinson's disease. 2020:10(4):1315-1333. doi: 10.3233/JPD-202223. Epub [PubMed PMID: 32986684]
Jung KM, Bang DH. Effect of inspiratory muscle training on respiratory capacity and walking ability with subacute stroke patients: a randomized controlled pilot trial. Journal of physical therapy science. 2017 Feb:29(2):336-339. doi: 10.1589/jpts.29.336. Epub 2017 Feb 24 [PubMed PMID: 28265169]
Level 1 (high-level) evidenceKowalski T, Kasiak PS, Rebis K, Klusiewicz A, Granda D, Wiecha S. Respiratory muscle training induces additional stress and training load in well-trained triathletes-randomized controlled trial. Frontiers in physiology. 2023:14():1264265. doi: 10.3389/fphys.2023.1264265. Epub 2023 Sep 28 [PubMed PMID: 37841319]
Level 1 (high-level) evidenceBissett B, Gosselink R, van Haren FMP. Respiratory Muscle Rehabilitation in Patients with Prolonged Mechanical Ventilation: A Targeted Approach. Critical care (London, England). 2020 Mar 24:24(1):103. doi: 10.1186/s13054-020-2783-0. Epub 2020 Mar 24 [PubMed PMID: 32204719]
Craighead DH, Freeberg KA, McCarty NP, Seals DR. Time-efficient, high-resistance inspiratory muscle strength training for cardiovascular aging. Experimental gerontology. 2021 Oct 15:154():111515. doi: 10.1016/j.exger.2021.111515. Epub 2021 Aug 10 [PubMed PMID: 34389471]
Troche MS, Rosenbek JC, Okun MS, Sapienza CM. Detraining outcomes with expiratory muscle strength training in Parkinson disease. Journal of rehabilitation research and development. 2014:51(2):305-10. doi: 10.1682/JRRD.2013.05.0101. Epub [PubMed PMID: 24933728]
Sapienza C, Troche M, Pitts T, Davenport P. Respiratory strength training: concept and intervention outcomes. Seminars in speech and language. 2011 Feb:32(1):21-30. doi: 10.1055/s-0031-1271972. Epub 2011 Apr 13 [PubMed PMID: 21491356]
Sankari A, Najjar AA, Maresh SA, Prowting JL, Fung CH, Knack A, Yarandi H, Badr MS. Feasibility of oropharyngeal and respiratory muscle training in individuals with OSA and spinal cord injury or disease: A pilot study. Physiological reports. 2024 Feb:12(3):e15930. doi: 10.14814/phy2.15930. Epub [PubMed PMID: 38325913]
Level 2 (mid-level) evidenceMohammed Yusuf SF, Bhise A, Nuhmani S, Alghadir AH, Khan M. Effects of an incentive spirometer versus a threshold inspiratory muscle trainer on lung functions in Parkinson's disease patients: a randomized trial. Scientific reports. 2023 Feb 13:13(1):2516. doi: 10.1038/s41598-023-29534-8. Epub 2023 Feb 13 [PubMed PMID: 36781936]
Level 1 (high-level) evidenceTavoian D, Ramos-Barrera LE, Craighead DH, Seals DR, Bedrick EJ, Alpert JS, Mashaqi S, Bailey EF. Six Months of Inspiratory Muscle Training to Lower Blood Pressure and Improve Endothelial Function in Middle-Aged and Older Adults With Above-Normal Blood Pressure and Obstructive Sleep Apnea: Protocol for the CHART Clinical Trial. Frontiers in cardiovascular medicine. 2021:8():760203. doi: 10.3389/fcvm.2021.760203. Epub 2021 Nov 24 [PubMed PMID: 34901220]
Level 2 (mid-level) evidenceCahalin LP, Arena R. Novel methods of inspiratory muscle training via the Test of Incremental Respiratory Endurance (TIRE). Exercise and sport sciences reviews. 2015 Apr:43(2):84-92. doi: 10.1249/JES.0000000000000042. Epub [PubMed PMID: 25607279]
Ammous O, Feki W, Lotfi T, Khamis AM, Gosselink R, Rebai A, Kammoun S. Inspiratory muscle training, with or without concomitant pulmonary rehabilitation, for chronic obstructive pulmonary disease (COPD). The Cochrane database of systematic reviews. 2023 Jan 6:1(1):CD013778. doi: 10.1002/14651858.CD013778.pub2. Epub 2023 Jan 6 [PubMed PMID: 36606682]
Level 1 (high-level) evidenceVorona S, Sabatini U, Al-Maqbali S, Bertoni M, Dres M, Bissett B, Van Haren F, Martin AD, Urrea C, Brace D, Parotto M, Herridge MS, Adhikari NKJ, Fan E, Melo LT, Reid WD, Brochard LJ, Ferguson ND, Goligher EC. Inspiratory Muscle Rehabilitation in Critically Ill Adults. A Systematic Review and Meta-Analysis. Annals of the American Thoracic Society. 2018 Jun:15(6):735-744. doi: 10.1513/AnnalsATS.201712-961OC. Epub [PubMed PMID: 29584447]
Level 1 (high-level) evidenceda Silva Guimarães B, de Souza LC, Cordeiro HF, Regis TL, Leite CA, Puga FP, Alvim SH, Lugon JR. Inspiratory Muscle Training With an Electronic Resistive Loading Device Improves Prolonged Weaning Outcomes in a Randomized Controlled Trial. Critical care medicine. 2021 Apr 1:49(4):589-597. doi: 10.1097/CCM.0000000000004787. Epub [PubMed PMID: 33332819]
Level 1 (high-level) evidenceWatson K, Egerton T, Sheers N, Retica S, McGaw R, Clohessy T, Webster P, Berlowitz DJ. Respiratory muscle training in neuromuscular disease: a systematic review and meta-analysis. European respiratory review : an official journal of the European Respiratory Society. 2022 Dec 31:31(166):. doi: 10.1183/16000617.0065-2022. Epub 2022 Nov 29 [PubMed PMID: 36450369]
Level 1 (high-level) evidenceLista-Paz A, Bouza Cousillas L, Jácome C, Fregonezi G, Labata-Lezaun N, Llurda-Almuzara L, Pérez-Bellmunt A. Effect of respiratory muscle training in asthma: A systematic review and meta-analysis. Annals of physical and rehabilitation medicine. 2023 Apr:66(3):101691. doi: 10.1016/j.rehab.2022.101691. Epub 2022 Dec 1 [PubMed PMID: 35843501]
Level 1 (high-level) evidenceSandnes A, Andersen T, Hilland M, Ellingsen TA, Halvorsen T, Heimdal JH, Røksund OD. Laryngeal movements during inspiratory muscle training in healthy subjects. Journal of voice : official journal of the Voice Foundation. 2013 Jul:27(4):448-53. doi: 10.1016/j.jvoice.2013.02.010. Epub 2013 May 15 [PubMed PMID: 23683807]
Level 2 (mid-level) evidenceDel Corral T, Fabero-Garrido R, Plaza-Manzano G, Fernández-de-Las-Peñas C, Navarro-Santana MJ, López-de-Uralde-Villanueva I. Minimal Clinically Important Differences in Inspiratory Muscle Function Variables after a Respiratory Muscle Training Programme in Individuals with Long-Term Post-COVID-19 Symptoms. Journal of clinical medicine. 2023 Apr 5:12(7):. doi: 10.3390/jcm12072720. Epub 2023 Apr 5 [PubMed PMID: 37048804]