Introduction
Anthracycline toxicity describes the toxic consequences of anthracycline-class medications. Anthracyclines, such as doxorubicin and epirubicin, are potent chemotherapy agents employed in managing various hematological and solid malignancies.[1] Anthracyclines are a key component in hematological chemotherapy regimens treating lymphoma, where doxorubicin, arguably the widest-used anthracycline, features in the CHOP (cyclophosphamide, hydroxydaunorubicin [doxorubicin], Oncovin® [vincristine], prednisone) and ABVD (Adriamycin® [doxorubicin], bleomycin, vinblastine, dacarbazine) protocols.[2]
The primary anticancer mechanism of action of anthracyclines is disruption of the topoisomerase-II enzyme (TOP2) stable intermediates, leading to a state of ever-increasing DNA damage. Other mechanisms, including the impact of reactive oxygen species, interference within intercalation, and chromatin damage, have also been proposed as anticancer mechanisms.[3] All the proposed mechanisms lead to preferential apoptosis in rapidly replicating cells, impacting slowly replicating or quiescent cell types less significantly.
The most prominent, well-studied, and clinically concerning toxicity associated with anthracycline chemotherapy is type-1 cardiotoxicity, a dose-dependent, irreversible, cumulative cardiomyocyte cell death that leads to the development of dilated cardiomyopathy and subsequent cardiac failure.[4][5] Likely, anthracycline exposure may also increase the risk of secondary cancer and lead to gonadal failure, but these impacts are not as well documented.[6] Liver, gastrointestinal tract, renal, and bone marrow toxicity may also occur but are often reversible; it is likely some degree of hepatic necrosis does occur with anthracycline administration, which may develop chronicity, but this occurs in doses well above that of cardiomyocyte death.[7]
With increasing cancer survivorship, the impact of anthracycline toxicity is growing, and the comorbidity and mortality associated with anthracycline toxicity are increasing. This activity reviews the proposed etiologic mechanisms, epidemiology, evaluation, and management of patients with anthracycline-induced cardiotoxicity and highlights the role of the interprofessional team in caring for patients exposed to anthracycline chemotherapeutics.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The specific mechanisms of anthracycline toxicity are still being elucidated; the underlying pathways will likely be complex, multifactorial, and interconnected. The currently accepted etiological mechanisms can be separated into a nuclear-mediated pathway and a mitochondrial-mediated pathway. Anthracycline toxicity appears to be dose-dependent and cumulative. This may be due to mitochondrial-mediated bioenergetic failures, the cumulative effect of cardiomyocyte death, the epigenetic disruption of gene expression through a combination of nuclear-mediated and mitochondrial-mediated cellular damage, or a combination of these mechanisms.[8]
Nuclear-Mediated Cardiomyocyte Death
The proposed primary anticancer mechanism of anthracycline chemotherapy is the disruption of topoisomerase II (TOP2) stable intermediates, specifically TOPIIβ. Given the role of TOP2 in managing double-stranded DNA breaks, this disruption can lead to escalating unresolved DNA damage, inhibiting normal cellular processes. There is also downstream induction of mitochondrial dysfunction due to altered gene expression, which, when combined with DNA damage from TOP2 and direct intercalation of anthracycline into the DNA helix, instigates p53-mediated apoptosis.[9] However, if the anthracycline molecule cannot enter the cell nucleus and cannot interfere with genetic expression, a reduction in toxicity and apoptosis occurs. Interestingly, restricting anthracycline from the nucleus does not prevent apoptosis, demonstrating how nuclear-mediated and mitochondrial-mediated pathways co-contribute to cardiomyocyte death.[10]
Mitochondrial-Mediated Cardiomyocyte Death
The role of reactive oxygen species (ROS), which may also determine some of the anticancer properties of the anthracycline class, may cause mitochondrial dysfunction in highly metabolic cells that display reduced antioxidant networks, such as the cardiomyocyte. As the cardiomyocyte rapidly takes up an anthracycline molecule, it undergoes a redox cycle via the NADH pathway, generating ROS and semiquinone free radicals.[11] Redox cycling, mainly when accumulated within the abundant cardiomyocyte mitochondria, significantly increases oxidative stress. The Fenton cycle, which occurs in the presence of mitochondrial iron, can further propagate this cycle. The downstream peroxidation of lipids and proteins due to increased oxidative stress increases cellular dysfunction and enzyme failure and impairs oxidative phosphorylation.[12] Specifically, anthracyclines in the mitochondrion promote the dissociation of cardiolipin from cytochrome-C, which in turn causes mitochondrion-initiated apoptosis.[13]
Anthracyclines demonstrate a dose-dependent ability to alter the mitochondrial membrane permeability (MMP). This process is calcium- and redox-dependent, with mitochondrial iron playing a pivotal role. As MMP increases, the inability to maintain electrochemical gradients impairs mitochondrial function, promoting cellular respiration failure and necroptosis.[14] The increase in MMP also induces the release of apoptosis-inducing factor (AIF) and promotes cellular death through caspase-independent mechanisms separate from the cytochrome-C mechanism previously described; this is known as ferroptosis.
Epidemiology
The epidemiological data on anthracycline toxicity is impacted by the dose-dependent nature of the toxicity and the variable presence of risk factors associated with its development, including many environmental and genetic factors. The data are further compounded by clinician variance in echocardiographic determination of left ventricular ejection fraction (LVEF) and a need for survivorship to demonstrate disease.[15] As a result, there is a high degree of variance between studies demonstrating anthracycline toxicity. The consensus is to define anthracycline toxicity as an LVEF that falls below 40% or reduces more than 10% from the pretreatment baseline. When doses are mentioned, these are considered equivalent doses of doxorubicin, the most commonly administered anthracycline chemotherapeutic agent.
Children
More than 50% of children with cancer receive anthracycline chemotherapy; exposure above 250 mg/m2 is associated with a 10% incidence of anthracycline toxicity, rising to a 30% incidence when accumulated doses exceed 600 mg/m2.[16] When the risk is grouped, a low-risk patient with less than a 250 mg/m2 accumulative dose has a 0.5% incidence of heart failure by age 40 years, compared to a high-risk patient with more than a 250 mg/m2 accumulative dose who has an 11.7% incidence of heart failure at the age of 40. Notable risk factors for developing anthracycline toxicity include patient age at treatment younger than 5 years, female gender, chest radiation, diabetes, or hypertension.[17] If the incidence of childhood cancer were estimated at 15 per 100,000 per annum, this would lead to a population incidence of less than 1 per 100,000 children per annum developing significant anthracycline toxicity in the United States.
Adults
The use of anthracycline chemotherapy in adults is gradually declining with the development of newer agents. However, anthracycline-containing chemotherapeutic regimens remain commonplace; up to 70% of older adults with lymphoma receive anthracycline chemotherapy.[18] Anthracycline-associated heart failure develops in adults, most notably between cumulative anthracycline doses of 400 to 550 mg/m2. At cumulative doses between 250 and 400 mg/m2, the incidence of heart failure is between 3% and 5%. At cumulative doses of 550 mg/m2, the incidence of heart failure rises to between 7% and 26%, and at a cumulative dose of 700 mg/m2, the incidence is as high as 48%.[19] The currently recommended maximum safe anthracycline dose for any patient is 400 to 450 mg/m2; most treatment protocols advise against higher doses.
Enhanced cardiac imaging may identify changes resulting from anthracycline chemotherapy in patients who do not develop symptoms. More than 90% of patients treated with an anthracycline medication manifest myocardial changes on biopsy at cumulative doses above 240 mg/m2, and the most significant asymptomatic changes in cardiac function occur at cumulative doses greater than 400 mg/m2.[20] If LVEF is assessed via multi-gated acquisition (MUGA) in asymptomatic patients when the cumulative dose is less than 400 mg/m2, the average LVEF reduction is 4%. Where doses exceed 400 mg/m2, the average LVEF reduction is 15%.
The incidence of anthracycline-induced cardiotoxicity at similar cumulative exposures increases with age; 14.9% of patients between 40 and 59 years of age receiving a cumulative doxorubicin dose of 600mg/m2 develop cardiotoxicity, but 22.4% of adults greater than 60 years of age develop cardiotoxicity at the same cumulative dose.[21] Significant risk factors for the development of anthracycline-induced cardiotoxicity include patient age, male gender, concurrent or historical chest radiation therapy, the presence of the classic predictors of heart disease, a prior reduction in LVEF, or concurrent treatment with cyclophosphamide, paclitaxel, or human epidermal growth factor receptor 2 (HER2) therapies.[22]
Pathophysiology
Anthracycline toxicity induces myocardial cell death via multiple mechanisms, resulting in globalized systolic and diastolic dysfunction and dilated cardiomyopathy. This ionotropic failure reduces cardiac output, increases cardiac preload, and causes pulmonary and systemic circulatory congestion. Decreased renal perfusion activates the renin-angiotensin-aldosterone (RAAS) pathway, resulting in compensatory vasoconstriction and increased blood volume, exacerbating vascular congestion.[23]
Histopathology
Endomyocardial biopsy with histological evaluation is seldom required to evaluate and manage anthracycline-induced cardiotoxicity. Reduced left ventricular mass and dilated cardiac chambers are often appreciated macroscopically. However, a microscopic assessment of the anthracycline-damaged heart will reveal diffuse myocardial fibrosis, interstitial edema, myocyte vacuolization, and atrophy; evidence of thrombosis and vascular dysfunction may also be seen.[24] The presence of normal coronary vasculature excludes ischemic cardiomyopathy and the lack of typical inflammatory infiltrates excludes myocarditis, facilitating a diagnosis of anthracycline-induced cardiotoxicity as a diagnosis of exclusion in the proper clinical context.[25]
Toxicokinetics
Anthracyclines demonstrate an apparent volume of distribution of approximately 25 L/kg, indicative of extensive tissue uptake.[26] Anthracyclines have a triphasic half-life and are predominately metabolized by the liver; 80% of the anthracycline dose is excreted in bile.[26] Patients with concomitant liver disease may have a reduced rate of anthracycline excretion and an increased risk of toxicity; liver dysfunction is commonly seen in various malignancies. If serum bilirubin levels are elevated, the anthracycline dose may need to be reduced.[27]
The recommended maximum cumulative exposure to anthracycline chemotherapy is 450 mg/m2; patients with risk factors for anthracycline toxicity should receive a maximum cumulative dose of 400 mg/m2 or less. The inadvertent administration of a single toxic dose of anthracyclines is associated with increased myelosuppressive side effects without anthracycline cardiotoxicity.[28] The delivery method, be it a continuous or bolus infusion, does not affect the toxicity outcomes significantly.[29]
The formulation of anthracycline notably affects its pharmacokinetics; liposomal formulations have a significantly longer half-life of greater than 70 hours compared to approximately 30 hours for conventional formulations. However, liposomal formulations are associated with a lower incidence of cardiotoxicity despite the longer half-life.
History and Physical
History
The manifestations of anthracycline cardiotoxicity are consistent with the typical symptoms of heart failure—those of congestion and those of reduced ionotropy. Symptoms of congestion include but are not limited to weight gain, dyspnea, paroxysmal nocturnal dyspnea, peripheral edema, ascites, cough, and orthopnea. Symptoms of reduced inotropy are typically more constitutional, including reduced exercise tolerance, decreased appetite, and fatigue. However, anthracycline cardiotoxicity may be asymptomatic. In patients with anthracycline cardiotoxicity, it is imperative to establish the cumulative exposure dose and when the drug was administered.
It can be challenging to distinguish symptoms of cancer or chemotherapy treatment from those of anthracycline toxicity. Ascertaining associated cardiac risk factors is essential, and significant confounding differentials such as myocardial ischemia, pulmonary embolism, and myocarditis must be excluded. Palpitations can be a component of anthracycline toxicity; atrial fibrillation is potentially an early manifestation.
Physical Examination
Patients with subclinical anthracycline cardiotoxicity typically present without significant physical examination findings. Early and often subtle signs of cardiotoxicity include elevated jugular venous pressure, modest weight gain, and pedal edema. Cardiac congestion may result in hypertension or tachycardia; patients without congestion may be normo- or hypotensive. Daytime oliguria with nocturia may be reported. A recent weight increase secondary to fluid retention and third spacing is common.
A diagnosis of anthracycline-induced cardiotoxicity is more forthcoming in the presence of frank cardiac failure characterized by elevated jugular venous pressure, tachypnea, tachycardia, and pedal edema. Sacral edema, ascites, pleural effusions, and pulmonary edema with respiratory compromise and cyanosis may be present. An S3 or S4 may be heard during cardiac auscultation. Point-of-care ultrasound may reveal globally reduced myocardial contractility with dilated cardiac chambers; the characteristic features of elevated central venous pressure, including a dilated or plethoric inferior vena cava without inspiratory collapse, increased portal vein pulsatility, and reversal of the hepatic Doppler waveform, may be present.
Evaluation
Specific patient cohorts are at increased risk of anthracycline cardiotoxicity. Before commencing anthracycline chemotherapy, all patients must undergo baseline investigations for risk stratification. At a minimum, these investigations include an electrocardiogram, transthoracic echocardiogram, serum troponin, and serum N-terminal pro-brain natriuretic peptide (NT-proBNP). All patients must also undergo some form of cardiac imaging; 3-dimensional (3D) transthoracic echocardiography, cardiac computed tomography (CT), or cardiac magnetic resonance imaging (cMRI) with strain-encoding are preferred. Multi-gated acquisition (MUGA) scanning is considered a fourth-line option due to its lack of structural detail.[30] It is unsafe to proceed with anthracycline chemotherapy before definitive cardiac imaging is obtained.
Determining the Risk of Anthracycline-Induced Cardiotoxicity
Online resources such as the calculator developed by the Cardio-Oncology Study Group of the Heart Failure Association of the European Society of Cardiology in collaboration with the International Cardio-Oncology Society (HFA-ICOS) are available to assist in determining anthracycline toxicity risk.
Category 1: Moderate-Risk (Assign 1 point per risk factor)
- Active smoker
- Obesity
- Prior non-anthracycline chemotherapy exposure
- Diabetes
- Hypertension
- Chronic kidney disease
- Elevated baseline troponin or NT-proBNP
Category 2: Moderate-Risk (Assign 2 points per risk factor)
- Low-normal left ventricular ejection fraction (50-54%)
- Prior non-anthracycline chemotherapy exposure
- Age between 65 and 79 years
High-Risk
- Subclinical or impaired left ventricular ejection fraction impairment (<50%)
- Severe valvular heart disease
- Prior ischemic cardiac disease
- Stable angina
- History of radiotherapy to the mediastinum
- Age greater than 80 years
Very-High-Risk
- Heart failure
- Prior anthracycline toxicity
A patient at low risk of anthracycline-induced cardiotoxicity presents with no more than a single Category 1 risk factor. A patient with a total score of 2, 3, or 4 points after assessment of risk factors is considered to be at moderate risk of anthracycline-induced cardiotoxicity. A patient with a total score of 5 points or greater or the presence of any single high-risk factor is deemed to be at high risk of anthracycline-induced cardiotoxicity. Patients who have any very high-risk factors are considered to be at very high risk of anthracycline-induced cardiotoxicity.[31]
Continuing Evaluation During and After Anthracycline Chemotherapy
The diagnostic consensus is that a reduction of left ventricular ejection fraction (LVEF) of greater than 10% in the presence of anthracycline chemotherapy or an absolute reduction of LVEF to less than 40% is consistent with a diagnosis of anthracycline toxicity. Further evaluation, such as angiography or cMRI, may be required to exclude disease processes that may mimic anthracycline-induced cardiotoxicity.[32]
Consideration of repeat cardiac imaging is imperative for all patients after they exceed a cumulative anthracycline chemotherapy dose of 250 mg/m2. Repeat cardiac imaging should be performed for any patients who develop symptoms suggestive of anthracycline-induced cardiotoxicity at any point during treatment. Repeat cardiac imaging should be performed on all patients 12 months after completion of anthracycline chemotherapy, regardless of cumulative dose. Of patients who develop anthracycline-induced cardiotoxicity, 98% will have an abnormal transthoracic echocardiogram, and 71% of them will not recover completely.[33] However, the data about how best to evaluate patients for anthracycline-induced cardiotoxicity is sparse and of low quality; high-quality evidence exists only for patients deemed to be at high or very high risk before initiation of anthracycline chemotherapy.
Patients initially deemed to be at low or moderate risk for anthracycline-induced cardiotoxicity should undergo laboratory evaluation of serum cardiac biomarkers every 2 cycles. Patients initially considered to be at moderate risk for anthracycline-induced cardiotoxicity should also undergo repeat cardiac imaging 3 months following the initiation of anthracyline chemotherapy. However, there is low-quality evidence to support the use of biomarkers in low- to moderate-risk patients.[34] Patients initially deemed to be at high or very high risk for anthracycline-induced cardiotoxicity should undergo serum cardiac biomarker testing at every cycle and cardiac imaging every other cycle. Rising serum biomarkers during routine monitoring should prompt cardiac imaging in all cases.
Patients who undergo hematopoietic stem-cell transplantation and anthracycline chemotherapy have a significantly increased rate of delayed-onset anthracycline-induced cardiotoxicity, with presentations frequently occurring more than 1 year after completion of anthracycline chemotherapy. These patients should undergo cardiac imaging every 3 to 5 years regardless of symptomatology.[35] Additionally, patients who have received more than 250 mg/m2 of anthracycline should undergo cardiac imaging with transthoracic echocardiography every 5 years for their lifetime. Transthoracic echocardiography should include global longitudinal strain (GLS) with speckle tracking whenever possible; this advanced modality sensitively assesses longitudinal contraction, and a reduction in GLS of 15% or more strongly correlates with an impending significant reduction in LVEF.[36]
Unique Populations
Evaluating the risk of anthracycline-induced cardiotoxicity in adults treated with anthracycline without toxicity as children is complex and patient-dependent. For most patients, annual risk screening focusing on primary prevention is recommended, with immediate cardiology consultation when pregnancy occurs. Adults who received a cumulative dose of anthracycline greater than 250 mg/m2 in childhood should undergo cardiac imaging every 2 years; those with a lower cumulative dose should undergo cardiac imaging every 5 years.[30]
Regular cardiac imaging during childhood cancer treatment with anthracycline chemotherapy is recommended, as is performing cardiac imaging every 5 years, with the first imaging study within 2 years of therapy or when pregnancy occurs, whichever happens first. These recommendations are based mainly on evaluation consensus.[16]
Treatment / Management
Patients undergoing anthracycline chemotherapy who are deemed to be at high or very high risk of anthracycline-induced cardiotoxicity should be prescribed the minimum dose of anthracycline. Pretreatment initiation of high-dose statin therapy and angiotensin-converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARB), or beta-blockers in high- or very-high-risk patients should be considered to reduce anthracycline toxicity, LVEF impairment, and mortality.[37] This strategy can also be employed when a rise in serum cardiac biomarkers is noted. Beta-blockers with antioxidant activity, such as nebivolol and carvedilol, may be preferable.[38] Additional preventative therapies may be indicated in patients with significant toxicity risk and are discussed in the Toxicity and Adverse Effect Management section.(A1)
The clinical symptomatology and cardiac imaging results dictate the management of anthracycline toxicity. Toxicity is deemed mild, moderate, or severe and defined as:
- Mild toxicity: LVEF is reduced but remains above 50%, or GLS is decreased by more than 15%
- Moderate toxicity: LVEF is between 40% and 50%
- Severe toxicity: LVEF is less than 40%
Asymptomatic Anthracycline Toxicity
- Mild toxicity should be managed with cardioprotective therapy in the form of ACEi/ARB and beta-blockers. Escalated monitoring should be considered while anthracycline chemotherapy continues.
- Moderate toxicity should prompt an interruption in anthracycline chemotherapy and the commencement of heart failure therapy.
- Severe toxicity should prompt an interruption in anthracycline chemotherapy and the commencement of heart failure therapy.
Symptomatic Anthracycline Toxicity
- Mild toxicity should prompt consideration of interrupting anthracycline chemotherapy; heart failure therapy should be initiated.
- Moderate toxicity should lead to the immediate interruption of anthracycline chemotherapy and should not be reinitiated until there is an improvement in LVEF with heart failure therapy.
- Severe toxicity should initiate the immediate cessation of anthracycline chemotherapy; the medication should not be reconsidered.
Heart failure therapy should be commenced in any symptomatic patient or asymptomatic patient with a significant LVEF reduction. In addition to ACEi/ARB and beta-blocker therapy that alters the RAAS pathway and neurohormonal dysregulation in cardiac failure, patients should begin the following therapy unless otherwise contraindicated; this therapy does not include diuretic treatment, which may be required to manage additional symptoms of cardiac congestion.[39]
- Mineralocorticoid receptor antagonists
- Angiotensin receptor-neprilysin inhibitors - these should not be co-administered with ACEi/ARB therapy.
- Sodium-glucose transport protein 2 inhibitors (SGLT2i)
Patients with severe cardiac failure require specialist consultation. Alternative medical therapy with medications such as ivabradine or digoxin may be necessary. Patients with severe cardiac failure and conduction abnormalities, including bundle branch blocks with wide QRS intervals, may require device implantation for cardiac resynchronization therapy, although this is atypical. Left ventricular assist devices and heart transplantation are rarely offered to patients with anthracycline toxicity due to their ongoing risk of malignancy.[40] To date, less than 5% of heart transplants have been provided to patients with anthracycline toxicity, albeit long-term outcomes when transplantation is performed are comparable.[41]
Cardiac rehabilitation in high-intensity interval training can improve cardiovascular outcomes in patients with anthracycline toxicity and can be offered to all suitable patients.[42] Cardiac rehabilitation programs specific to anthracycline toxicity are not available. Controlling modifiable risk factors before, during, and after anthracycline toxicity improves outcomes. All patients should be informed of the benefits of tobacco and alcohol cessation, optimal control of chronic diseases such as hypertension and diabetes, and diet and exercise. (B2)
Differential Diagnosis
Dilated cardiomyopathy resulting from anthracycline toxicity is diagnostically nonspecific if not correlated with clinical history, as are the associated endomyocardial biopsy and cMRI findings. It is essential to consider concomitant and potentially reversible causes of cardiomyopathy that may confound a diagnosis; these include but are not limited to myocarditis and thyrotoxic, ischemic, and alcohol-induced cardiomyopathy.
The differential diagnosis of anthracycline toxicity may be confounded by the concomitant use of alternative cardiotoxic chemotherapy agents, including HER2 therapy and immune checkpoint inhibitors. Anthracycline-containing chemotherapy regimens may include cyclophosphamide, which is also associated with potent cardiotoxicity. Radiotherapy to the chest cavity may cause various cardiac complications, including changes to the pericardium, the cardiac valves, and dilated cardiomyopathy. Anticancer therapy is often given in close succession; determining the root cause of dilated cardiomyopathy may be challenging and require specialist and multidisciplinary input.
In clinical practice, recent anthracycline exposure with a reduction in cardiac function compared to prior cardiac imaging strongly supports the clinical diagnosis of anthracycline toxicity. Due to the improved utilization of cardiac evaluation before, during, and after anthracycline therapy, the presentation of undiagnosed anthracycline toxicity long after the initial treatment is rare, excluding underlying genetic or idiopathic causes. The diagnosis of idiopathic dilated cardiomyopathy should not be made if cardiotoxic medications have recently been administered and prior cardiac imaging revealed no abnormalities.
Toxicity and Adverse Effect Management
Given the potentially significant consequences of anthracycline toxicity, efforts have been made to create less toxic analogs that still provide anthracycline anticancer properties to the tumor.
Molecular Modification
Likely, the anthracycline molecule cannot be significantly altered to prevent toxicity without impacting anticancer function. Camsirubicin is a synthetic doxorubicin analog that exhibits some selectivity for the TOPIIα isoform; clinical studies have demonstrated similar profiles in cancer cytotoxicity with reduced anthracycline-induced cardiotoxicity. Annamycin is a highly lipophilic anthracycline that has shown preferential accumulation in the lungs and reduced cardiotoxicity in early trials.[43]
Anthracycline formulations can be modified through liposomal infusion, restricting the ability of the molecule to cross tighter vascular junctions, such as those found in the myocardium, reducing anthracycline exposure and the risk of toxicity. Liposomal infusions may, however, limit anthracycline anticancer properties, and toxicity may still occur in high-risk patients.[44] Prescribing liposomal anthracycline preparations is the next best option after reducing the cumulative dose to reduce the incidence of anthracycline toxicity.
Iron Chelation
Dexrazoxane employs iron chelation to prevent ROS formation and disturb anthracycline-induced TOP2 binding. Dexrazoxane, in combination with anthracycline chemotherapy, has been shown to significantly lower the incidence of LVEF reduction compared to anthracycline therapy alone; this medication remains reserved for high-risk patients when anthracycline chemotherapy is essential.[45] Although other iron-chelating agents have been shown to provide similar effects, dexrazoxane is the only medication regularly used to prevent anthracycline-induced cardiotoxicity. Iron chelation may lower the anticancer benefit of anthracyclines, and dexrazoxane is associated with myelosuppression when combined with a wide variety of anticancer agents.
Prognosis
Patients exposed to anthracycline chemotherapy are much more likely to die from their underlying malignancy before anthracycline toxicity presents a threat to life. More than 95% of patients with cancer treated with anthracycline chemotherapy die from their underlying malignancy rather than developing anthracycline toxicity, and cardiac death contributes to 0.7% all-cause mortality.[33] At 1 year following anthracycline treatment, 98% of cases where toxicity develops will be clinically apparent. Approximately 11% of patients note a full recovery of their cardiac function, significantly increased by early and proactive intervention; 71% see an incomplete recovery, and the remaining 18% see no significant recovery in cardiac function. Patients with partial to no recovery in cardiac function have higher New York Heart Association classifications, impacts on quality of life, and incidence of cardiac death.[33] In high-dose anthracycline chemotherapy, where severe symptoms of cardiotoxicity present during treatment, cardiac failure is an associated cause of death in up to 38% of patients, with a median survival of 162 days.[46]
Concerning longer-term cancer versus cardiac outcomes, only after 9 years following the first presentation with cancer does the cardiac cause of death overtake malignancy, including relapse and secondary cancer. Patients with lower cancer stages have an increased relative incidence of death due to reduced cancer mortality.[47] The overall prognosis of a patient with anthracycline-induced cardiotoxicity is similar to that of dilated cardiomyopathy of any cause, in which 5-year survival is quoted at 86%, compared to 88% in idiopathic cardiomyopathy. Patients with anthracycline toxicity are affected more significantly by refractory heart failure with reduced incidence of sudden death than those with idiopathic cardiomyopathy.[48]
In cases of childhood cancer, cardiac cause of death in anthracycline toxicity remains rare at less than 0.5% incidence during anthracycline chemotherapy; this includes patients exposed to high doses when anthracycline toxicity on cardiac imaging is noted, and patients also appear to require fewer cardiac devices.[49] To this end, cardiac cause of death has an incidence of 0.14% following 30-year survivorship for childhood cancer, even in cases of high-dose anthracycline and impaired cardiac function.[50]
Complications
The complications associated with anthracycline-induced cardiotoxicity are consistent with those of dilated cardiomyopathy of other etiology.
Pericardial effusions have been noted in patients who have received anthracycline chemotherapy, although the incidence is low. The exact etiology of these effusions is unclear. Anthracycline toxicity can predispose to supraventricular tachyarrhythmias, including atrial fibrillation and atrial flutter. The incidence of these tachyarrhythmias is 10% to 15% in subclinical anthracycline toxicity and is similar to other forms of dilated cardiomyopathy when reductions in LVEF are significant.[19] The risk of arrhythmia increases with the severity of anthracycline toxicity; severe and life-threatening ventricular arrhythmias are rare. There appears to be no significant increase in the risk of ischemic or valvular heart disease as found in other chemotherapy toxicity syndromes.
Pregnant patients with anthracycline-induced cardiotoxicity have a very high incidence of cardiovascular events. However, the complication rates in those with all-cause peripartum cardiomyopathy are notably high. There is no increase in maternal deaths associated with anthracycline toxicity compared to other causes of peripartum cardiomyopathy.[51]
Deterrence and Patient Education
All patients undergoing chemotherapeutic treatment, including anthracycline chemotherapy, should understand the risks and benefits of such therapy; it is the responsibility of the multidisciplinary team to engage in shared decision-making with patients when developing therapeutic plans. If an anthracycline-class medication is to be administered, the patient should be educated on the symptoms of cardiotoxicity and informed of the importance of regular evaluations and adherence to prescribed medicines. Optimizing control of associated risk factors for anthracycline toxicity, including diabetes, tobacco cessation, and weight reduction, can improve overall outcomes. The importance of modifiable risk factors should be emphasized.
Enhancing Healthcare Team Outcomes
The evaluation and management of anthracycline toxicity is complex. The multidisciplinary team is vital to the close observation that aids in identifying anthracycline toxicity and promoting early treatment, which is essential to achieving the best patient outcomes. Close adherence to evaluation programs with an accurate patient risk assessment and determination of baseline investigations is critical. The physician performs the initial consultation and confirmation of the malignancy, followed by baseline investigations. Based on this, a multidisciplinary team can proceed with anthracycline chemotherapy if it is safe. In complex cases presenting a high risk, the involvement of a cardiologist or cardio-oncologist is essential.
There are detailed guidelines to improve outcomes for patients undergoing anthracycline chemotherapy, particularly in those with risk factors for poorer outcomes.[30] The highest quality evidence primarily focuses on patients with high or very high risk of developing anthracycline toxicity; the cardiac physiologist is critical in deriving cardiac imaging for further decision-making, with regular cardiac imaging recommended for those at the highest risk. The formulation of additional evidence is challenged by the high mortality rate associated with the primary malignancy. In all patients with significant anthracycline toxicity, the early commencement of heart failure therapy aids significantly in reducing morbidity and mortality. Newer anticancer derivatives of anthracycline-class medications and liposomal formulations can reduce the incidence of adverse outcomes in anthracycline chemotherapy.
Following anthracycline chemotherapy, cardiac physiologists, nursing, and pharmacist teams are crucial to facilitating optimal evaluation and treatment. The cardiac physiologist is critical in accurately determining the cardiac imaging vital to informing multidisciplinary management. Nursing teams, with their regular patient interfacing, can play an essential role in supporting patients in identifying anthracycline toxicity and providing holistic support to ensure the patient's needs are met. The pharmacist's role is to ensure optimal delivery of heart failure medication and safe administration of anthracycline chemotherapy with a mindful awareness of the accumulative dose. A well-informed and engaged multidisciplinary team in the form of a cardio-oncology team consisting of physicians, pharmacists, cardiac physiologists, and nurses is highly recommended to optimize outcomes for patients undergoing anthracycline chemotherapy to reduce the impact of anthracycline toxicity.[52]
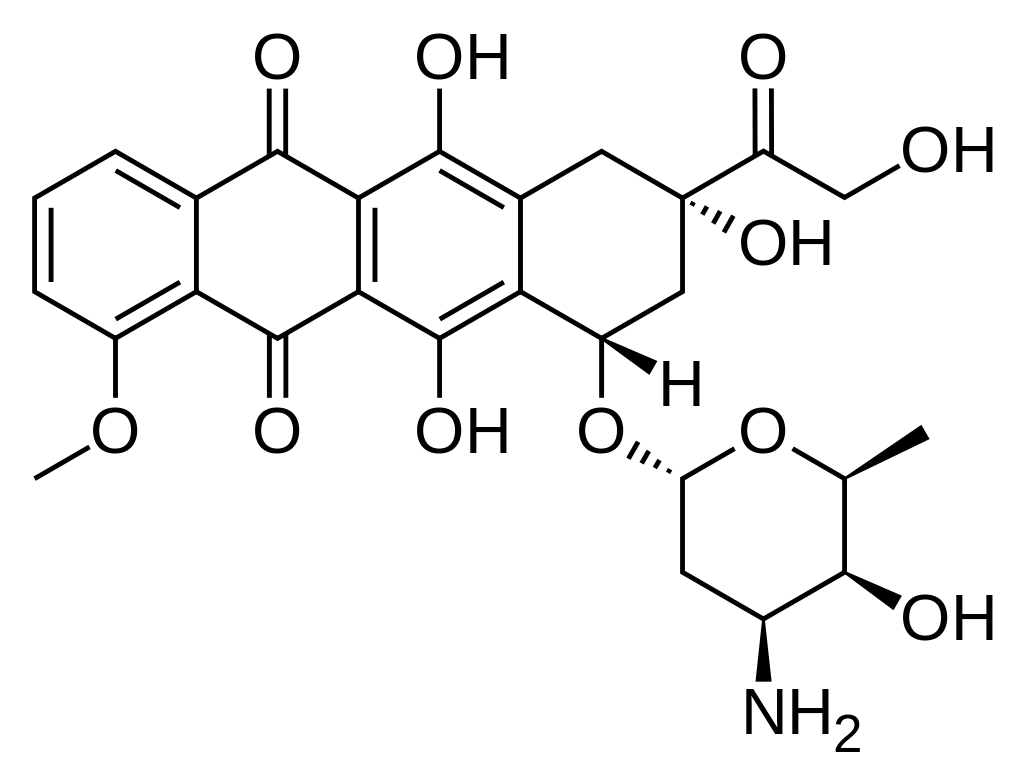
Media
(Click Image to Enlarge)
References
Venkatesh P, Kasi A. Anthracyclines. StatPearls. 2024 Jan:(): [PubMed PMID: 30844214]
Lewis WD, Lilly S, Jones KL. Lymphoma: Diagnosis and Treatment. American family physician. 2020 Jan 1:101(1):34-41 [PubMed PMID: 31894937]
Marinello J, Delcuratolo M, Capranico G. Anthracyclines as Topoisomerase II Poisons: From Early Studies to New Perspectives. International journal of molecular sciences. 2018 Nov 6:19(11):. doi: 10.3390/ijms19113480. Epub 2018 Nov 6 [PubMed PMID: 30404148]
Level 3 (low-level) evidenceBansal N, Adams MJ, Ganatra S, Colan SD, Aggarwal S, Steiner R, Amdani S, Lipshultz ER, Lipshultz SE. Strategies to prevent anthracycline-induced cardiotoxicity in cancer survivors. Cardio-oncology (London, England). 2019:5():18. doi: 10.1186/s40959-019-0054-5. Epub 2019 Dec 2 [PubMed PMID: 32154024]
Perez IE, Taveras Alam S, Hernandez GA, Sancassani R. Cancer Therapy-Related Cardiac Dysfunction: An Overview for the Clinician. Clinical Medicine Insights. Cardiology. 2019:13():1179546819866445. doi: 10.1177/1179546819866445. Epub 2019 Jul 29 [PubMed PMID: 31384135]
Level 3 (low-level) evidenceBen-Aharon I, Granot T, Meizner I, Hasky N, Tobar A, Rizel S, Yerushalmi R, Ben-Haroush A, Fisch B, Stemmer SM. Long-Term Follow-Up of Chemotherapy-Induced Ovarian Failure in Young Breast Cancer Patients: The Role of Vascular Toxicity. The oncologist. 2015 Sep:20(9):985-91. doi: 10.1634/theoncologist.2015-0044. Epub 2015 Jun 22 [PubMed PMID: 26099742]
Bayles CE, Hale DE, Konieczny A, Anderson VD, Richardson CR, Brown KV, Nguyen JT, Hecht J, Schwartz N, Kharel MK, Amissah F, Dowling TC, Nybo SE. Upcycling the anthracyclines: New mechanisms of action, toxicology, and pharmacology. Toxicology and applied pharmacology. 2023 Jan 15:459():116362. doi: 10.1016/j.taap.2022.116362. Epub 2022 Dec 30 [PubMed PMID: 36592899]
Wallace KB, Sardão VA, Oliveira PJ. Mitochondrial Determinants of Doxorubicin-Induced Cardiomyopathy. Circulation research. 2020 Mar 27:126(7):926-941. doi: 10.1161/CIRCRESAHA.119.314681. Epub 2020 Mar 26 [PubMed PMID: 32213135]
Zhang S, Liu X, Bawa-Khalfe T, Lu LS, Lyu YL, Liu LF, Yeh ET. Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nature medicine. 2012 Nov:18(11):1639-42. doi: 10.1038/nm.2919. Epub 2012 Oct 28 [PubMed PMID: 23104132]
Level 3 (low-level) evidenceJean SR, Tulumello DV, Riganti C, Liyanage SU, Schimmer AD, Kelley SO. Mitochondrial Targeting of Doxorubicin Eliminates Nuclear Effects Associated with Cardiotoxicity. ACS chemical biology. 2015 Sep 18:10(9):2007-15. doi: 10.1021/acschembio.5b00268. Epub 2015 Jun 18 [PubMed PMID: 26038829]
Doroshow JH, Locker GY, Myers CE. Enzymatic defenses of the mouse heart against reactive oxygen metabolites: alterations produced by doxorubicin. The Journal of clinical investigation. 1980 Jan:65(1):128-35 [PubMed PMID: 7350193]
Level 3 (low-level) evidenceIchikawa Y, Ghanefar M, Bayeva M, Wu R, Khechaduri A, Naga Prasad SV, Mutharasan RK, Naik TJ, Ardehali H. Cardiotoxicity of doxorubicin is mediated through mitochondrial iron accumulation. The Journal of clinical investigation. 2014 Feb:124(2):617-30. doi: 10.1172/JCI72931. Epub 2014 Jan 2 [PubMed PMID: 24382354]
Level 3 (low-level) evidenceGoormaghtigh E, Huart P, Brasseur R, Ruysschaert JM. Mechanism of inhibition of mitochondrial enzymatic complex I-III by adriamycin derivatives. Biochimica et biophysica acta. 1986 Sep 25:861(1):83-94 [PubMed PMID: 3019400]
Level 3 (low-level) evidenceMontaigne D, Marechal X, Preau S, Baccouch R, Modine T, Fayad G, Lancel S, Neviere R. Doxorubicin induces mitochondrial permeability transition and contractile dysfunction in the human myocardium. Mitochondrion. 2011 Jan:11(1):22-6. doi: 10.1016/j.mito.2010.06.001. Epub 2010 Jun 23 [PubMed PMID: 20599629]
Thavendiranathan P, Grant AD, Negishi T, Plana JC, Popović ZB, Marwick TH. Reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection fraction and volumes: application to patients undergoing cancer chemotherapy. Journal of the American College of Cardiology. 2013 Jan 8:61(1):77-84. doi: 10.1016/j.jacc.2012.09.035. Epub 2012 Nov 28 [PubMed PMID: 23199515]
Armenian SH, Hudson MM, Mulder RL, Chen MH, Constine LS, Dwyer M, Nathan PC, Tissing WJ, Shankar S, Sieswerda E, Skinner R, Steinberger J, van Dalen EC, van der Pal H, Wallace WH, Levitt G, Kremer LC, International Late Effects of Childhood Cancer Guideline Harmonization Group. Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. The Lancet. Oncology. 2015 Mar:16(3):e123-36. doi: 10.1016/S1470-2045(14)70409-7. Epub [PubMed PMID: 25752563]
Armenian S, Bhatia S. Predicting and Preventing Anthracycline-Related Cardiotoxicity. American Society of Clinical Oncology educational book. American Society of Clinical Oncology. Annual Meeting. 2018 May 23:38():3-12. doi: 10.1200/EDBK_100015. Epub [PubMed PMID: 30231396]
Chihara D, Westin JR, Oki Y, Ahmed MA, Do B, Fayad LE, Hagemeister FB, Romaguera JE, Fanale MA, Lee HJ, Turturro F, Samaniego F, Neelapu SS, Rodriguez MA, Fowler NH, Wang M, Davis RE, Nastoupil LJ. Management strategies and outcomes for very elderly patients with diffuse large B-cell lymphoma. Cancer. 2016 Oct 15:122(20):3145-3151. doi: 10.1002/cncr.30173. Epub 2016 Jun 28 [PubMed PMID: 27351173]
McGowan JV, Chung R, Maulik A, Piotrowska I, Walker JM, Yellon DM. Anthracycline Chemotherapy and Cardiotoxicity. Cardiovascular drugs and therapy. 2017 Feb:31(1):63-75. doi: 10.1007/s10557-016-6711-0. Epub [PubMed PMID: 28185035]
Bristow MR, Mason JW, Billingham ME, Daniels JR. Doxorubicin cardiomyopathy: evaluation by phonocardiography, endomyocardial biopsy, and cardiac catheterization. Annals of internal medicine. 1978 Feb:88(2):168-75 [PubMed PMID: 626445]
Neuendorff NR, Loh KP, Mims AS, Christofyllakis K, Soo WK, Bölükbasi B, Oñoro-Algar C, Hundley WG, Klepin HD. Anthracycline-related cardiotoxicity in older patients with acute myeloid leukemia: a Young SIOG review paper. Blood advances. 2020 Feb 25:4(4):762-775. doi: 10.1182/bloodadvances.2019000955. Epub [PubMed PMID: 32097461]
Level 3 (low-level) evidenceVolkova M, Russell R 3rd. Anthracycline cardiotoxicity: prevalence, pathogenesis and treatment. Current cardiology reviews. 2011 Nov:7(4):214-20 [PubMed PMID: 22758622]
Chatterjee K, Zhang J, Honbo N, Karliner JS. Doxorubicin cardiomyopathy. Cardiology. 2010:115(2):155-62. doi: 10.1159/000265166. Epub 2009 Dec 11 [PubMed PMID: 20016174]
Narezkina A, Narayan HK, Zemljic-Harpf AE. Molecular mechanisms of anthracycline cardiovascular toxicity. Clinical science (London, England : 1979). 2021 May 28:135(10):1311-1332. doi: 10.1042/CS20200301. Epub [PubMed PMID: 34047339]
Saltiel E, McGuire W. Doxorubicin (adriamycin) cardiomyopathy. The Western journal of medicine. 1983 Sep:139(3):332-41 [PubMed PMID: 6356608]
Speth PA, van Hoesel QG, Haanen C. Clinical pharmacokinetics of doxorubicin. Clinical pharmacokinetics. 1988 Jul:15(1):15-31 [PubMed PMID: 3042244]
Lai C, Cole DE, Steinberg SM, Lucas N, Dombi E, Melani C, Roschewski M, Balis F, Widemann BC, Wilson WH. Doxorubicin pharmacokinetics and toxicity in patients with aggressive lymphoma and hepatic impairment. Blood advances. 2023 Feb 28:7(4):529-532. doi: 10.1182/bloodadvances.2022007431. Epub [PubMed PMID: 35882475]
Level 3 (low-level) evidenceSavani M, Skubitz KM. Long-term Outcome After Doxorubicin and Ifosfamide Overdose in a Patient With Osteosarcoma and BARD1 Mutation. Journal of pediatric hematology/oncology. 2019 Mar:41(2):e94-e96. doi: 10.1097/MPH.0000000000001264. Epub [PubMed PMID: 30045149]
Cranmer LD, Lu Y, Heise RS, Ballman KV, Loggers ET, Pollack SM, Wagner MJ, Reinke DK, Schöffski P, Tap WD. Bolus versus Continuous Intravenous Delivery of Doxorubicin in Soft-Tissue Sarcomas: Post Hoc Analysis of a Prospective Randomized Trial (SARC021/TH CR-406). Clinical cancer research : an official journal of the American Association for Cancer Research. 2023 Mar 14:29(6):1068-1076. doi: 10.1158/1078-0432.CCR-22-1564. Epub [PubMed PMID: 36622694]
Level 1 (high-level) evidenceLyon AR, López-Fernández T, Couch LS, Asteggiano R, Aznar MC, Bergler-Klein J, Boriani G, Cardinale D, Cordoba R, Cosyns B, Cutter DJ, de Azambuja E, de Boer RA, Dent SF, Farmakis D, Gevaert SA, Gorog DA, Herrmann J, Lenihan D, Moslehi J, Moura B, Salinger SS, Stephens R, Suter TM, Szmit S, Tamargo J, Thavendiranathan P, Tocchetti CG, van der Meer P, van der Pal HJH, ESC Scientific Document Group. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). European heart journal. 2022 Nov 1:43(41):4229-4361. doi: 10.1093/eurheartj/ehac244. Epub [PubMed PMID: 36017568]
Lyon AR, Dent S, Stanway S, Earl H, Brezden-Masley C, Cohen-Solal A, Tocchetti CG, Moslehi JJ, Groarke JD, Bergler-Klein J, Khoo V, Tan LL, Anker MS, von Haehling S, Maack C, Pudil R, Barac A, Thavendiranathan P, Ky B, Neilan TG, Belenkov Y, Rosen SD, Iakobishvili Z, Sverdlov AL, Hajjar LA, Macedo AVS, Manisty C, Ciardiello F, Farmakis D, de Boer RA, Skouri H, Suter TM, Cardinale D, Witteles RM, Fradley MG, Herrmann J, Cornell RF, Wechelaker A, Mauro MJ, Milojkovic D, de Lavallade H, Ruschitzka F, Coats AJS, Seferovic PM, Chioncel O, Thum T, Bauersachs J, Andres MS, Wright DJ, López-Fernández T, Plummer C, Lenihan D. Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies: a position statement and new risk assessment tools from the Cardio-Oncology Study Group of the Heart Failure Association of the European Society of Cardiology in collaboration with the International Cardio-Oncology Society. European journal of heart failure. 2020 Nov:22(11):1945-1960. doi: 10.1002/ejhf.1920. Epub 2020 Aug 6 [PubMed PMID: 32463967]
Michel L, Mincu RI, Mahabadi AA, Settelmeier S, Al-Rashid F, Rassaf T, Totzeck M. Troponins and brain natriuretic peptides for the prediction of cardiotoxicity in cancer patients: a meta-analysis. European journal of heart failure. 2020 Feb:22(2):350-361. doi: 10.1002/ejhf.1631. Epub 2019 Nov 12 [PubMed PMID: 31721381]
Level 1 (high-level) evidenceCardinale D, Colombo A, Bacchiani G, Tedeschi I, Meroni CA, Veglia F, Civelli M, Lamantia G, Colombo N, Curigliano G, Fiorentini C, Cipolla CM. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015 Jun 2:131(22):1981-8. doi: 10.1161/CIRCULATIONAHA.114.013777. Epub 2015 May 6 [PubMed PMID: 25948538]
Fallah-Rad N, Walker JR, Wassef A, Lytwyn M, Bohonis S, Fang T, Tian G, Kirkpatrick ID, Singal PK, Krahn M, Grenier D, Jassal DS. The utility of cardiac biomarkers, tissue velocity and strain imaging, and cardiac magnetic resonance imaging in predicting early left ventricular dysfunction in patients with human epidermal growth factor receptor II-positive breast cancer treated with adjuvant trastuzumab therapy. Journal of the American College of Cardiology. 2011 May 31:57(22):2263-70. doi: 10.1016/j.jacc.2010.11.063. Epub [PubMed PMID: 21616287]
Armenian SH, Yang D, Teh JB, Atencio LC, Gonzales A, Wong FL, Leisenring WM, Forman SJ, Nakamura R, Chow EJ. Prediction of cardiovascular disease among hematopoietic cell transplantation survivors. Blood advances. 2018 Jul 24:2(14):1756-1764. doi: 10.1182/bloodadvances.2018019117. Epub [PubMed PMID: 30037802]
Level 3 (low-level) evidenceOikonomou EK, Kokkinidis DG, Kampaktsis PN, Amir EA, Marwick TH, Gupta D, Thavendiranathan P. Assessment of Prognostic Value of Left Ventricular Global Longitudinal Strain for Early Prediction of Chemotherapy-Induced Cardiotoxicity: A Systematic Review and Meta-analysis. JAMA cardiology. 2019 Oct 1:4(10):1007-1018. doi: 10.1001/jamacardio.2019.2952. Epub [PubMed PMID: 31433450]
Level 1 (high-level) evidenceCurigliano G, Lenihan D, Fradley M, Ganatra S, Barac A, Blaes A, Herrmann J, Porter C, Lyon AR, Lancellotti P, Patel A, DeCara J, Mitchell J, Harrison E, Moslehi J, Witteles R, Calabro MG, Orecchia R, de Azambuja E, Zamorano JL, Krone R, Iakobishvili Z, Carver J, Armenian S, Ky B, Cardinale D, Cipolla CM, Dent S, Jordan K, ESMO Guidelines Committee. Electronic address: clinicalguidelines@esmo.org. Management of cardiac disease in cancer patients throughout oncological treatment: ESMO consensus recommendations. Annals of oncology : official journal of the European Society for Medical Oncology. 2020 Feb:31(2):171-190. doi: 10.1016/j.annonc.2019.10.023. Epub [PubMed PMID: 31959335]
Level 3 (low-level) evidenceAttar A, Behnagh AK, Hosseini M, Amanollahi F, Shafiekhani P, Kabir A. Beta-Blockers for Primary Prevention of Anthracycline-Induced Cardiac Toxicity: An Updated Meta-Analysis of Randomized Clinical Trials. Cardiovascular therapeutics. 2022:2022():8367444. doi: 10.1155/2022/8367444. Epub 2022 Dec 29 [PubMed PMID: 36687509]
Level 1 (high-level) evidenceMcDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A, ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European heart journal. 2021 Sep 21:42(36):3599-3726. doi: 10.1093/eurheartj/ehab368. Epub [PubMed PMID: 34447992]
Shugh SB, Ryan TD. Heart transplantation in survivors of childhood cancer. Translational pediatrics. 2019 Oct:8(4):314-321. doi: 10.21037/tp.2019.06.02. Epub [PubMed PMID: 31728324]
Bock MJ, Pahl E, Rusconi PG, Boyle GJ, Parent JJ, Twist CJ, Kirklin JK, Pruitt E, Bernstein D. Cancer recurrence and mortality after pediatric heart transplantation for anthracycline cardiomyopathy: A report from the Pediatric Heart Transplant Study (PHTS) group. Pediatric transplantation. 2017 Aug:21(5):. doi: 10.1111/petr.12923. Epub 2017 Apr 4 [PubMed PMID: 28378408]
Adams SC, DeLorey DS, Davenport MH, Fairey AS, North S, Courneya KS. Effects of high-intensity interval training on fatigue and quality of life in testicular cancer survivors. British journal of cancer. 2018 May:118(10):1313-1321. doi: 10.1038/s41416-018-0044-7. Epub 2018 May 8 [PubMed PMID: 29736007]
Level 2 (mid-level) evidenceDempke WCM, Zielinski R, Winkler C, Silberman S, Reuther S, Priebe W. Anthracycline-induced cardiotoxicity - are we about to clear this hurdle? European journal of cancer (Oxford, England : 1990). 2023 May:185():94-104. doi: 10.1016/j.ejca.2023.02.019. Epub 2023 Feb 24 [PubMed PMID: 36966697]
Dioun SM, Vilardo N, Goldberg GL, Gressel GM. Necessity of routine cardiac evaluation in patients receiving pegylated liposomal doxorubicin for gynecologic cancer. Gynecologic oncology. 2019 Nov:155(2):301-304. doi: 10.1016/j.ygyno.2019.09.009. Epub 2019 Sep 28 [PubMed PMID: 31575390]
Asselin BL, Devidas M, Chen L, Franco VI, Pullen J, Borowitz MJ, Hutchison RE, Ravindranath Y, Armenian SH, Camitta BM, Lipshultz SE. Cardioprotection and Safety of Dexrazoxane in Patients Treated for Newly Diagnosed T-Cell Acute Lymphoblastic Leukemia or Advanced-Stage Lymphoblastic Non-Hodgkin Lymphoma: A Report of the Children's Oncology Group Randomized Trial Pediatric Oncology Group 9404. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2016 Mar 10:34(8):854-62. doi: 10.1200/JCO.2015.60.8851. Epub 2015 Dec 23 [PubMed PMID: 26700126]
Ryberg M, Nielsen D, Skovsgaard T, Hansen J, Jensen BV, Dombernowsky P. Epirubicin cardiotoxicity: an analysis of 469 patients with metastatic breast cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1998 Nov:16(11):3502-8 [PubMed PMID: 9817267]
Level 2 (mid-level) evidencePatnaik JL, Byers T, DiGuiseppi C, Dabelea D, Denberg TD. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast cancer research : BCR. 2011 Jun 20:13(3):R64. doi: 10.1186/bcr2901. Epub 2011 Jun 20 [PubMed PMID: 21689398]
Level 2 (mid-level) evidenceFornaro A, Olivotto I, Rigacci L, Ciaccheri M, Tomberli B, Ferrantini C, Coppini R, Girolami F, Mazzarotto F, Chiostri M, Milli M, Marchionni N, Castelli G. Comparison of long-term outcome in anthracycline-related versus idiopathic dilated cardiomyopathy: a single centre experience. European journal of heart failure. 2018 May:20(5):898-906. doi: 10.1002/ejhf.1049. Epub 2017 Nov 16 [PubMed PMID: 29148208]
Creutzig U, Diekamp S, Zimmermann M, Reinhardt D. Longitudinal evaluation of early and late anthracycline cardiotoxicity in children with AML. Pediatric blood & cancer. 2007 Jun 15:48(7):651-62 [PubMed PMID: 17183582]
Level 3 (low-level) evidenceMertens AC, Liu Q, Neglia JP, Wasilewski K, Leisenring W, Armstrong GT, Robison LL, Yasui Y. Cause-specific late mortality among 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. Journal of the National Cancer Institute. 2008 Oct 1:100(19):1368-79. doi: 10.1093/jnci/djn310. Epub 2008 Sep 23 [PubMed PMID: 18812549]
Level 2 (mid-level) evidenceCowgill JA, Francis SA, Sawyer DB. Anthracycline and Peripartum Cardiomyopathies. Circulation research. 2019 May 24:124(11):1633-1646. doi: 10.1161/CIRCRESAHA.119.313577. Epub [PubMed PMID: 31120822]
Johnson MN. Cardio-Oncology and Health Equity: Opportunities for Implementation. JACC. CardioOncology. 2023 Aug:5(4):546-550. doi: 10.1016/j.jaccao.2023.04.006. Epub 2023 Jun 27 [PubMed PMID: 37614577]