 Anatomy, Bony Pelvis and Lower Limb: Calf Common Peroneal Nerve (Common Fibular Nerve)
Anatomy, Bony Pelvis and Lower Limb: Calf Common Peroneal Nerve (Common Fibular Nerve)
Introduction
The common peroneal nerve, or the common fibular nerve, is a major nerve that innervates the lower extremity (see Image. The Sacral and Coccygeal Nerves). As 1 of the 2 major branches of the sciatic nerve, it receives fibers from the posterior divisions of L4 through S2. Specifically, it originates from the sciatic nerve separates from it proximal to the popliteal fossa, and courses its way along the posterolateral aspect of the leg deep to the long head of the biceps femoris and through the popliteal fossa before passing behind the proximal fibular head. Just inferior and lateral to the fibular head, it divides into 2 nerves at the fibular neck–the superficial and deep fibular nerves. The superficial fibular nerve courses anterolaterally between the fibularis longus muscle and extensor digitorum longus muscle within the lateral compartment.
As it moves distally, it terminates within the lateral compartment before reaching the ankle and foot. The deep fibular nerve courses anteriorly and runs adjacent to the anterior tibial artery between the extensor digitorum longus muscle and the tibialis anterior muscle. As the deep fibular nerve travels distally, it runs within the anterior leg compartment between 2 muscles. These muscles include the extensor hallucis longus muscle and the tibialis anterior muscle. As the nerve approaches the foot anteriorly to the talus, it divides into medial and lateral branches. The medial branch travels alongside the dorsalis pedis artery and terminates between the first 2 metatarsals. The lateral branch travels alongside the lateral tarsal artery and terminates near the fifth metatarsal.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The common fibular nerve is ultimately responsible for innervating the muscles that compose the lower extremity's anterior and lateral muscular compartments. The anterior muscular compartment of the lower extremity consists of the tibialis anterior muscle, the extensor hallucis longus muscle, and the extensor digitorum longus muscle. This compartment is responsible primarily for the dorsiflexion of the foot.[2] The lateral muscular compartment of the lower extremity consists of the fibularis longus muscle and the fibularis brevis muscle. This compartment is responsible primarily for the eversion of the foot.
In addition to carrying motor fibers, the common fibular nerve carries afferent cutaneous sensory fibers from the lower extremities that travel proximally to the spinal cord. The superficial fibular nerve carries the most anterior sensation of the leg; however, the deep fibular nerve also carries some. Specifically, the superficial fibular nerve carries sensory fibers from the anterolateral aspect of the lower extremity that extends from midway down the leg to most of the dorsal aspect of the foot and toes. The deep fibular nerve carries sensory fibers between the first and second toes. These nerves also carry some posterolateral sensation, albeit minimal. The common fibular nerve is responsible for sensation inferolateral to the knee via the lateral sural cutaneous nerve, a small cutaneous branch of the common fibular nerve. The superficial fibular nerve is responsible for some lateral leg sensation just below where the sensation from the lateral sural cutaneous nerve ends.[1]
Physiologic Variants
As in most parts of the human anatomy, the course and surrounding anatomy of the common fibular nerve have several variants that should be noted, especially for surgeons who may have to decompress the nerve. These variants may also result in an increase or decrease in the likelihood of compressed nerves.[3] In a study comparing the anatomy in cadavers and the anatomy in surgically decompressed nerves, there were found to be a few major variants. The first one includes fibrous tissue that forms a band-like structure underneath the superficial head of the peroneus longus. The next variant also includes fibrous tissue forming a band-like structure; however, this tissue is located on the superficial surface of the deep head of a muscle known as the peroneus longus. The last variant noted includes 2 muscles and their uncommon junction and origin. Usually, the soleus muscle and the fibularis longus muscle originate separately on the fibular head; however, some people originate together at the fibular head and separate as they move distally.[4]
Clinical Significance
The common fibular nerve is a frequently discussed subject compared to other neuromuscular complaints due to its frequent injury and classic clinical presentation. Because of its location, it is fairly vulnerable to damage. It travels across the lateral aspect of the knee over the neck of the fibula, where its only protection is skin and subcutaneous fat and fascia. Thus, various traumas to the lateral knee often damage the common fibular nerve. For example, if a football player is tackled from the side, the result may be a fibular neck fracture and a common fibular nerve injury.[5] The patient would most likely present with knee pain, loss of foot dorsiflexion, ankle eversion, and loss of sensation down the lateral leg and dorsum of the foot. Because of the patient’s inability to dorsiflex the foot, they are also likely to present with a "foot drop." This condition occurs during the swinging phase of the gait cycle. Because there is a loss of dorsiflexion, the toes drag on the ground rather than clear the ground as in a normal gait. The patient often compensates for their foot-dragging by exaggerating hip abduction to allow for increased foot clearance.[6][7]
Another frequent mechanism of injury to the common fibular nerve is nerve compression as it crosses the fibular head and neck or distal to them. This may occur after a splint or cast is placed incorrectly or too tight or in the case of compartment syndrome after a trauma or burn. These examples would present similarly: the compressed nerve would initially cause paresthesias, followed by loss of sensation and weakness, ultimately resulting in loss of dorsiflexion of the foot and ankle eversion if left untreated. It should be noted that in these cases, there might also be a vascular compromise, so distal pulses should be examined.[2]
There are also clinical presentations that may mimic an injury to the common fibular nerve but are due to proximal injuries at the level of the sciatic nerve. One common example is piriformis syndrome. In some cases or anatomical variants, the sciatic nerve, which carries fibers for the common fibular nerve, may become entrapped within the piriformis muscle. A tight piriformis may cause similar symptoms to the classic common fibular nerve injury: loss of dorsiflexion, loss of foot eversion, and loss of sensation to the anterolateral aspect of the leg and dorsum of the foot. However, in addition to these symptoms, the patient might also experience symptoms proximal to the knee, similar to the classic presentation of sciatica. Thus, it is essential to differentiate between sciatica, piriformis syndrome, or simply an injury to the common fibular nerve to formulate a proper treatment plan.[8]
Media
(Click Image to Enlarge)
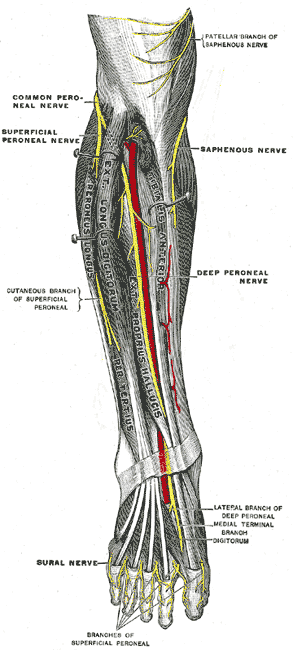
The Sacral and Coccygeal Nerves. Deep nerves of the front of the leg, deep peroneal nerve, saphenous nerve, and dural nerve.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Khan IA, Mahabadi N, D’Abarno A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Leg Lateral Compartment. StatPearls. 2024 Jan:(): [PubMed PMID: 30137811]
Chow AL, Levidy MF, Luthringer M, Vasoya D, Ignatiuk A. Clinical Outcomes After Neurolysis for the Treatment of Peroneal Nerve Palsy: A Systematic Review and Meta-Analysis. Annals of plastic surgery. 2021 Sep 1:87(3):316-323. doi: 10.1097/SAP.0000000000002833. Epub [PubMed PMID: 34397520]
Level 2 (mid-level) evidenceTomaszewski KA, Graves MJ, Vikse J, Pękala PA, Sanna B, Henry BM, Tubbs RS, Walocha JA. Superficial fibular nerve variations of fascial piercing: A meta-analysis and clinical consideration. Clinical anatomy (New York, N.Y.). 2017 Jan:30(1):120-125. doi: 10.1002/ca.22741. Epub 2016 Jul 7 [PubMed PMID: 27271092]
Level 1 (high-level) evidenceDellon AL, Ebmer J, Swier P. Anatomic variations related to decompression of the common peroneal nerve at the fibular head. Annals of plastic surgery. 2002 Jan:48(1):30-4 [PubMed PMID: 11773727]
Walters BB, Constant D, Anand P. Fibula Fractures. StatPearls. 2024 Jan:(): [PubMed PMID: 32310599]
Lezak B, Massel DH, Varacallo M. Peroneal Nerve Injury. StatPearls. 2024 Jan:(): [PubMed PMID: 31751049]
Nori SL, Stretanski MF. Foot Drop. StatPearls. 2024 Jan:(): [PubMed PMID: 32119280]
van Zantvoort APM, Setz MJM, Hoogeveen AR, Scheltinga MRM. Common Peroneal Nerve Entrapment in the Differential Diagnosis of Chronic Exertional Compartment Syndrome of the Lateral Lower Leg: A Report of 5 Cases. Orthopaedic journal of sports medicine. 2018 Aug:6(8):2325967118787761. doi: 10.1177/2325967118787761. Epub 2018 Aug 17 [PubMed PMID: 30148178]
Level 3 (low-level) evidence