Introduction
Onchocerciasis, also known as the African river blindness, is the second most important cause of infectious blindness worldwide after trachoma.
It is caused by the filarial nematode, Onchocerca volvulus, and transmitted by repeated bites of the vector, female black fly of the genus Simulium damnosum. The vector breeds in fast-flowing and oxygen-rich rivers in affected areas with transmission and disease prevalence usually stretching along these river basins and thereby the name river blindness.[1] Aside from blindness, onchocerciasis results in a troubling chronic dermatitis.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
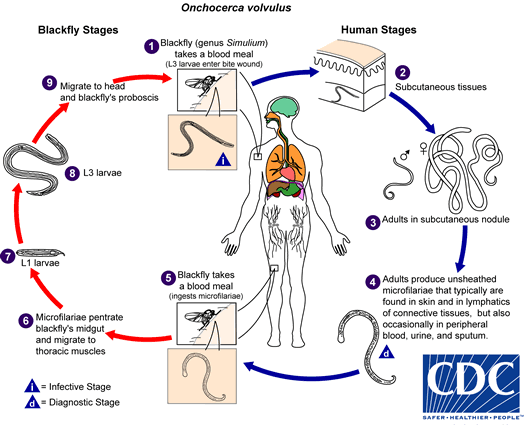
The definitive hosts of Onchocerca volvulus are humans, while the larval stages grow exclusively in the Simulium black fly, of which there are several cyto-species based on their flying characteristics and chromosomal banding patterns.[2][3]
Further classifications into savanna, rainforest, and transitional zone clades are done based on their habitats and mitochondrial gene sequencing. These show different biting characteristics and propensity towards causing blinding disease.[2]
Infective microfilariae larvae (L3 stage) are injected into a host during the blood meal of the female black fly. For 6 to 12 months, these larvae would develop into adult worms (microfilariae) that reside in fibrous sub-cutaneous nodules, located commonly around the iliac crest, the head, and torso [see figures]. Each nodule may contain one or two female worms and a single male that is usually smaller in size. Fertilized adult worms produce about 1000 to 1,500 microfilariae (L1 stages) daily and have a life span of 10 to 15 years.[4]
These baby worms measure 250 to 300 microns and 8 microns in cross-section and live for 1 to 2 years.[5]
At any given time, millions of microfilariae are moving through subcutaneous tissues and, to a lesser extent, the lymphatic system of an affected patient.[6] During a subsequent blood meal, these L1 forms are ingested by a biting fly. They then transform over 1 to 3 weeks first by migrating from the gut into the thoracic flight muscles as an L2 larval stage. From here, they develop into an infective L3 larval stage and migrate into the salivary gland for subsequent transmission during the next blood meal. Once in the human body, the injected larvae transform into the L4 stage from where they mature in about one year.
Epidemiology
The disease is endemic in 31 sub-Saharan African countries, the Arabian peninsula, and a small locality in Latin America that stretches across the Bolivarian Republic of Venezuela and Brazil. About 90% of the disease occurs in sub-Saharan Africa.
The World Health Organization (WHO) estimates that at least 25 million people are infected worldwide, and another 90 million are at risk, with more than 99% of them in Africa. Vision loss is estimated to affect 1.15 million population.
Worldwide ongoing mass drug administration (MDA) with ivermectin has significantly reduced the burden of infection and associated ocular disease.[7] A recent study (in 2018) from Togo with the identification of ocular disease in children and young adults despite ongoing MDA programs with a reduction of microfilariae rates is creating concerns.[8] Onchocerciasis is more likely to be found in persons involved in the agricultural industry and especially so in those living closer to rivers that serve as breeding grounds for the Simulium black fly. In a risk factors assessment study in Ethiopia, the male gender, a distance less than 2 km from the riverbank, noncompliance to ivermectin therapy, and age of above 35 years were all associated with a higher prevalence of onchocerciasis.
Pathophysiology
Route of Entry
The actual route of entry into the eye is not clearly understood. Proposed routes include the bloodstream, sheaths of the posterior ciliary arteries, and nerves, cerebrospinal fluid, and sheath of the optic nerve.[9][10]
Anterior Segment[11]
Ocular pathology involves both anterior and posterior segments, and the mechanisms are not completely understood. The presence of microfilariae in the eye and indeed in the skin usually does not cause much problem. On the other hand, dead or dying microfilariae trigger an inflammatory cascade that leads to tissue damage associated with the disease. Specifically, it is known that the sclerosing keratitis that leads to cornea blindness is mediated through modification of ICAM-1 expression and production of IL-4 and IL-13.[12] The anterior chamber can be affected as well by dead microfilariae, causing uveitis, with the formation of synechiae, secondary cataract, and glaucoma, which may be of open-angle or closed-angle forms.[12] While cataract is a common complication seen in onchocerciasis as a result of induced changes in anterior chamber physiology, only a handful of cases have reported glaucoma as an independent complication of onchocerciasis. [11] In one case-control study that related to patients undergoing cataract and glaucoma filtering surgery, the authors calculated that onchocerciasis was a potential risk factor for developing Glaucoma.[11] There is also strong evidence to suggest that a bacteria endosymbiont of Onchocerca volvulus, Wolbachia plays a central role in the immunogenic response to dead microfilariae.[13][14]
Posterior Segment[15]
It, however, appears that mechanisms leading to chorioretinal and optic nerve damage may be mediated along a different pathway. Past literature has confirmed the evidence of persistent deterioration in posterior segment pathologies in some patients despite clearance of microfilariae from the anterior chamber of the eye or after years of repeated ivermectin treatment.[16][17] Whether these progressive ocular changes result from autoimmune responses or persistence of microfilariae or their products in the posterior segment has not been fully established. Additionally, several studies suggest that cross-reactive antibodies induced by O. volvulus antigens (Ov39) and the retinal pigment epithelial (RPE) antigen (hr44) may contribute to posterior segment diseases.[18][19] It should be noted that Onchocercal damage to structures of the posterior segment is generally difficult to differentiate from other end-stage pathologies of the optic nerve, retina, and choroid. In one study using fundus fluorescein angiogram to study posterior segment changes during treatment with diethylcarbamazine, the authors reported transient fluorescein leakage at the posterior pole that lasted only a few days.[20] This was, however, more likely due to the toxic effects of the treatment agent rather than structural damage caused by the presence of microfilariae.[20]
Histopathology
Ophthalmological
Histological findings in advanced stages of ocular onchocerciasis are characterized by chronic sclerosing keratitis and pannus formation, chronic uveitis, and secondary glaucoma. The presence of microfilariae, both dead and viable, was demonstrated in all ocular tissues from the cornea to the optic disc, except the crystalline lens.[21] The microfilariae were readily identifiable in the cornea and sclera, but less so in other intraocular tissues.[21]
Inflammatory cells, including eosinophils, plasma cells, and to a lesser extent, lymphocytes have been identified to be present in the acute response to dead microfilariae in the cornea and elsewhere in the eye.[22]
Pannus formation is seen as a direct consequence of the sclerosing keratitis and the mobilization of new capillaries, fibroblasts, and inflammatory cells, including abundant plasma cells and eosinophils. Typically the pannus exists above the Bowman’s membrane.[22]
Dermatological
Histology of the early stages of the onchocerciasis dermal lesion will reveal microfilariae concentrated within the papillary dermis. This is often associated with clusters of inflammatory cells. Dying larvae induces a response typified by microabscess formation and granuloma. Advanced stages of onchocerciasis typically manifest with acanthosis, parakeratosis, melanophagocytosis, and pigment incontinence.
Onchocercal nodule represents a subcutaneous ball of the Onchocerca worms, which is embedded in an inflammatory granuloma. It is also known as an onchocercoma. Onchocerca worms can become calcified or degenerated in the dermis and cause scarring and atrophy. Cutaneous onchocerciasis may feature an acute or chronic papular onchodermatitis, lichenified onchodermatitis, atrophy, and depigmentation.[23]
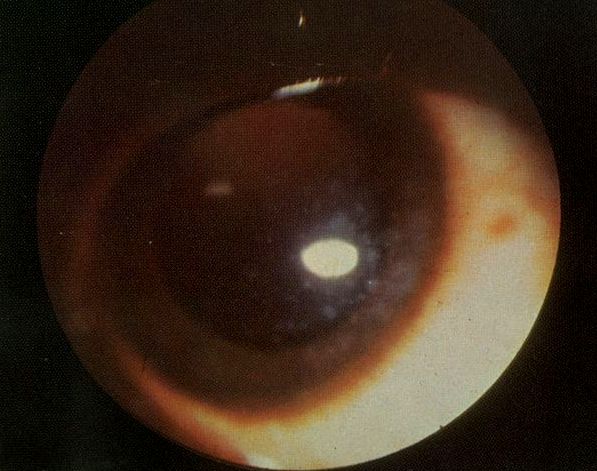
History and Physical
The most common presentation is one of recurrent severe pruritus, papular dermatitis, lichenified dermatitis, and areas of skin depigmentation, especially around the shins, giving rise to the name "leopard skin." Skin depigmentation happens as a result of chronic rubbing of the skin (which may involve the use of stones and other coarse materials) in response to severe itchiness induced by an immunological response to dying or dead microfilariae. These normally present years before ocular manifestations ensue.[24] Ocular features include recurrent conjunctivitis, punctate keratitis, photophobia, and progressive visual loss from either anterior(cornea scarring) or posterior segment pathologies (optic nerve and chorioretinal atrophies) or both.[25] Typically dead microfilariae induce focal corneal reaction (snowflake keratitis, see figure) that mimics stage 3 adenoviral keratitis. Continuous corneal insult and healing result in progressive corneal scarring that starts from the limbal areas in the interpalpebral fissure, and eventually leading to corneal blindness. Posterior segment diseases are related to the optic nerve and chorioretinal atrophy.[26]
Evaluation
The slit-lamp examination may show non-specific punctate, and snow-flake keratitis [figure], which represent a local reaction to dead microfilariae and rarely limbal global infiltrates, especially if treatment has been initiated. Recurrent corneal reactions end up with progressive corneal scarring. Other anterior segment features are those associated with uveitis, cataract, and glaucoma.
Occasionally microfilariae may be visualized in the corneal stroma and more commonly in the anterior chamber (AC) where they are seen actively swimming in the aqueous, and these can be captured on videography. To increase the chance of identifying microfilariae in the AC, patients are made to sit with their heads bent between their knees for at least 3 minutes.
Posterior segment features are equally non-specific and include chorioretinitis, progressive RPE, and optic nerve atrophy. The evaluation may require fundus photo, optical coherence tomography (OCT) of the macula and/or optic disc, fundus autofluorescence, fundus fluorescein angiogram, and Humphrey visual fields.
The diagnosis of onchocerciasis can be clinical. The presence of microfilariae in the anterior chamber can readily be observed using the slit lamp biomicroscope at high magnification. Skin snips are the gold standard for the diagnosis of onchocerciasis.[27] Skin microfilariae may be directly observed in a skin snip biopsy. This involves taking bloodless skin snips from the scapula, iliac crest areas, and over the calf muscles. These are then incubated in normal saline for 24 hours and examined under the microscope. This allows the identification and differentiation of the observed motile elements under the microscope. For example, Onchocerca volvulus microfilariae have no sheath nor nuclei in their tails, and these differentiate them from other worms like Wuchereria bancrofti, Brugia malayi, and Brugia timori.
Serological tests involving ELISA (enzyme-linked immunosorbent assay) and Western Blot techniques are currently available for detecting antibodies to Onchocerca volvulus antigens in the skin, tears, and urine. [28], [20] Other tests based on polymerase chain reaction (PCR) amplification and ultrasound scanning of the subcutaneous nodules exist, but these tests are hardly used in the clinical management of onchocerciasis.[29]
How to Perform a Skin Snip
This is a specialized way of obtaining a biopsy specimen to examine for the presence of microfilariae. First, an area of skin is wiped with alcohol. Then it is elevated with the tip of a needle. Shave the small segment of tented skin with a razor blade or scalpel (measures about 3mm in diameter). This usually results in a harvest of about 2 mg of skin. This piece of skin is placed on a slide under a coverslip and immersed in normal saline at room temperature for 24 hours. This process allows the microfilariae, if present, to emerge. In an Onchocerca infected patient, this preparation when examined using a microscope, motile microfilariae emerging from the tissue will be identified.[23]
Treatment / Management
In the past, treatment had involved the use of diethylcarbamazine, which was effective but also caused very serious systemic and ocular complications, especially in patients with high microfilaridermia.[30] The current standard of care is oral ivermectin 150 mcg/kg given once or twice a year for 10 to 15 years, corresponding to the life span of the adult worm, or as long as the infected patient has evidence of active infection. It paralyzes or kills the microfilariae but has no effects on the life of an adult worm, though it reduces the fertility of female adult worm at least temporarily. Ivermectin reduces the occurrence of blindness and skin disease due to onchocerciasis. Prolonged daily treatments are not needed as there is no evidence that it offers benefits compared to annual or 6 monthly treatments. A higher dose than the recommendation may be harmful. Evidence of active infection includes microfilaria on skin examination or skin biopsy and skin symptoms like pruritus. The presence of the adult worm in skin nodules may not necessarily need continued treatment, as adult worms are not killed by ivermectin, and these do not cause symptoms. More frequent dosage of ivermectin (every 6 months or every 3 months) can reduce the duration of symptoms and cause more rapid sterilization of the adult worm, especially in persons who are not returning to live in an endemic region.
The clearance of microfilariae from the skin and the anterior chamber has been studied extensively. A previous meta-analysis has shown that skin microfilariae are reduced by half in 24 hours, 94% in one week, and 98% to 99% by 1 to 2 months, following a single dose of ivermectin.[31] Similar clearance happens in the anterior chamber, but this lags behind the skin clearance by several months.[32] Microfilariae repopulation of skin and eye resumes in a few months, and this is due to continuous production by the adult worm. [32](A1)
A major limitation of currently available treatment is the absence of good and safe drugs to kill the adult worm, which causes the persistence of infection. Tablet doxycycline is promising in this regard, and may kill the adult worm by killing Wolbachia; however, doxycycline does not kill the microfilaria for which another drug has to be used concurrently.[28] Wolbachia is endosymbiotic, rickettsia-like bacteria, which is important for the survival of adult worm and embryogenesis. The used dose is oral 100mg or 200mg once daily for 6 weeks. Ivermectin should be started at least 1 week before doxycycline for optimal benefits.[33] Doxycycline can sterilize up to 90% of adult female worms and kill at least 60% adult female worms 20 months after treatment. (B3)
Older treatments, including suramin and diethylcarbamazine, are avoided as less toxic and effective alternative treatments are available. Diethylcarbamazine may accelerate the development of blindness. Patients coinfected with Loa loa can have a life-threatening encephalitic reaction to ivermectin, and the opinion of infectious disease specialists or experts on loiasis is a must before starting therapy. Doxycycline has only been tested in coinfected persons with a Loa microfilariae load of less than 8000/ml.
Differential Diagnosis
Since onchocerciasis presents with both dermatological and ophthalmological manifestations, differentiating each of them in isolation is sometimes very challenging. Skin features like pruritus may be due to allergic reactions from several sources.
- Subcutaneous nodules may be due to other subcutaneous cystic or non-cystic lesions. A list of some subcutaneous nodules includes the following (this is by no means exhaustive)
- Inflammatory or reactive
- Granulomatous: rheumatoid arthritis, juvenile rheumatoid arthritis
- Panniculitis: erythema nodosum, nodular panniculitis
- Systemic vasculitis: polyarteritis nodosum, granulomatosis with polyangiitis
- Metabolic and storage disorders: gout, calcinosis
- Others: osteoarthritis, foreign bodies[34]
- Inflammatory or reactive
- Infectious
- Bacterial: treponemes, subacute bacterial endocarditis
- Fungal: sporotrichosis, coccidioidomycosis
- Mycobacterial: tuberculosis, leprosy
- Viral: hepatitis B, hepatitis C
- Parasitic: amebiasis, Chagas disease[34]
- Tumors
- Benign: lipoma, neuroma, nevus, ganglion cyst, bony exostosis, schwannoma
- Malignant: sarcoma, leukemia, lymphoma, melanoma, basal cell carcinoma [34]
- Ocular lesions seen in onchocerciasis are not unique to the disease. Uveitis, cataract, glaucoma, and other posterior segment changes may all be due to causes other than onchocerciasis. Other helminthic infestations are important differential diagnoses of onchocerciasis and include hookworm infestations, schistosomiasis, sparganosis, and cestodes.
Pertinent Studies and Ongoing Trials
Various Control Programs started in the seventies (Onchocerciasis Control Program-OCP:1974, African Program for Onchocerciasis Control-APOC:1995, Onchocerciasis Elimination for the Americas-OEPA: 1991 [35], Expanded Special Project for Elimination of Neglected Tropical Diseases-ESPEN-2016), have helped to reduce the burden of Onchocerciasis, elimination, however, remains elusive. This is partly due to recurrent civil conflicts in endemic zones and the inability to eliminate the adult worm in current treatment programs coupled with an incomplete understanding of pathomechanisms relating to Onchocercal ocular disease.
Several studies have recently been completed and others underway. One such study looked into moxidectin, a drug that is more effective and slows down microfilariae repopulation has recently been completed with promising outcomes. [32]
Other studies are using high-resolution retinal cameras and optical coherence tomography (OCT) to study the possibility of finding microfilariae in tissues of the anterior segment and more importantly, the posterior segment. This is based on the structural morphology of the microfilariae which measures 250 to 300 microns in length and 8 microns in cross-section.[5] Other clinical trials are looking into a combination therapy made up of ivermectin, diethylcarbamazine, and albendazole that aim at either killing or permanently sterilizing the adult worm.[36]
Treatment Planning
The current standard of care for onchocerciasis is the use of ivermectin 150 mcg/kg given once or twice a year depending on the level of individual disease burden and community endemicity. Currently, ivermectin is distributed as a community-directed mass drug administration (MDA) and more than 100 million people are treated each year under a donation program. Ocular complications associated with onchocerciasis were treatable, are managed by standard ophthalmic treatment protocols.
Toxicity and Adverse Effect Management
In some patients infected with onchocerciasis, there is coinfection with Loa loa, another parasite that is predominantly seen in the west and central Africa, where Onchocerca volvulus also exists.[37][38] Treatment with ivermectin in patients with this coinfection can cause severe life-threatening adverse effects, including encephalitic reaction as a result of the Loa loa infection contributing to the heavy burden of microfilariae.[37][39]
Because of the possibility of severe adverse effects following ivermectin treatment in areas of co endemicity, epidemiological surveys have been advocated.[40] This is aimed at assessing the intensity of infection with Loa loa microfilariae before ivermectin is distributed for onchocerciasis control in areas where loiasis is endemic.
The Mazzotti reaction, which was first described in 1948, is a potentially life-threatening allergic response seen in patients with onchocerciasis patients, who are on microfilaricidal treatment with diethylcarbamazine (DEC).[41]
DEC, however, is no longer in use for the treatment of onchocerciasis. Clinical features of this Mazzotti reaction typically occur within 7 days of treatment with DEC and includes hypotension, fever, adenitis, urticaria, arthralgia, malaise, eosinophilia, tachycardia, edema, abdominal pain, and elevated liver enzymes.[41] There are also reports of Mazzotti reaction occurring after treatment with ivermectin. The incidence of Mazzotti reaction with ivermectin is about 10%, and about 25% have only fever or pruritus. There are no reports yet of Mazzotti like reaction with albendazole.
The Mazzotti reaction is the basis of the Mazzotti test, which is a test for onchocerciasis using an oral test dose of DEC (50 to 100 mg). This results in an acute rash in 2 to 24 hours from the death of microfilariae in the skin. This test can now be done with the DEC delivery via a skin patch (OCP-patch) and gives a more localized skin reaction.[42]
To manage a Mazzotti reaction, administration of low dose dexamethasone, i.e., 3 mg/day, commenced after the beginning of the reaction modifies the progression of the Mazzotti reaction without interfering with the microfilaricidal effect of DEC. Pretreatment with low dose dexamethasone before commencing DEC therapy has been found to prevent the development of the Mazzotti reaction and reduces the microfilaricidal activity. Therefore, it is recommended that low-dose steroids be used in conjunction with DEC, at the onset of a Mazzotti reaction. Steroids should be tapered rapidly.[43] It is, however, stressed that standard recommendation is to avoid DEC in onchocerciasis, and it is no longer used to treat this disease.
It is important to mention that serious neurological adverse events have been rarely observed with the use of ivermectin in the treatment of onchocerciasis. This adverse event has not been entirely explained by concomitant high burden loiasis infections.[44]
Prognosis
Often ocular and dermatologic complications of onchocerciasis improve with ivermectin treatment, especially if the disease is not advanced. When the disease is advanced, blindness due to optic atrophy or cornea scarring and vascularization is often irreversible. Also, the dermatological manifestations of advanced diseases such as skin depigmentation and atrophy are irreversible.
Complications
Ocular complications of onchocerciasis include blindness as a result of keratitis, the formation of pannus, and corneal scarring. Other causes of blindness include optic atrophy, open-angle glaucoma, and chorioretinitis, as previously stated. Posterior segment complications have been noted to be responsible for over half of the blindness from onchocerciasis in a report. Specific posterior segment complications reported in this study include; chorioretinal changes including intraretinal pigment (IRP) clumping and retinal pigment epithelium atrophy, retinitis, subretinal fibrosis, and optic neuritis.[45]
Other ocular complications include live and dead microfilariae presence in anterior chamber and cornea, punctate cornea opacity, sclerosis keratitis, pannus formation, and uveitis (iridocyclitis).[45][46]
Deterrence and Patient Education
Onchocerciasis infection can be avoided by avoiding exposure or bites from the vector. This can be achieved by the use of protective clothing or applying repellants on the skin. Travelers to endemic regions should receive advice on this.[28]
There are efforts targeted at deterring infection by abolishing vector habitats through the promotion of vector habitat control programs.
Also, population-based strategies in some endemic regions are targeted at vector elimination and yearly mass ivermectin treatment.
Patients with a high load of microfilaria should be informed of the risk of severe reaction following treatment. This can often be associated with coinfection from Loa loa and can result in severe morbidity and a threat to life. Also, when there is a heavy burden of microfilariae and ocular involvement, patients should be informed of the potential complications that can occur from ivermectin use.
Pearls and Other Issues
Between 1975 and 2002, global elimination programs were focused on vector control, and this has largely been very successful in West Africa where it started. Following this in 1995, the focus was shifted to the use of ivermectin as the standard of care. A key drawback, however, is that ivermectin has only a temporary effect on the adult worms. Microfilariae repopulation occurs in a few months with microfilaridermia preceding the ocular presentation of microfilariae. This underscores the need for repeated treatments for at least 10 to 15 years, the life span of the adult worm. To overcome these, better treatments that have direct effects on the adult worm would need to be developed, and several such studies are already underway. One such study is looking into a combination of benzimidazole and benzoxaborole.[47] While others are looking into a combination of ivermectin, diethylcarbamazine, and albendazole.[36]
Promising microfilaricidal drugs like moxidectin, when approved, would likely reduce the current number of times and length of treatment for onchocerciasis.[32]
It is needed to deepen the understanding of ocular pathomechanisms in onchocerciasis. In the past, these have been difficult as the only ways to do these were the use of fundus fluorescein angiography, which is invasive with considerable side effects in some patients. With the advent of high definition optical coherence tomography and other retinal imaging technologies, there are safer ways of probing the posterior segment involvement in onchocerciasis.
Enhancing Healthcare Team Outcomes
Management of onchocerciasis is an interprofessional and intersectoral project. It involves ophthalmologist who take care of the ocular complications, dermatologists, general surgeons who may perform nodulectomy in some cases, public health physicians and nurses involved in program management and supervision and community health workers who undertake MDA activities. Others include Community leadership and opinion leaders, governments, and non-governmental organizations that provide funding, logistics, and donation of Ivermectin. Beyond these are collaborative research works involving local institutions/governments and colleges outside the respective countries. Several such collaborative research is conducted by the Death to Onchocerciasis and Lymphatic Filariasis (DOLF). It is based in Washington University, St. Louis, USA, and is currently undertaking several ground-breaking research in Ghana and other African countries like Congo DR and Ivory Coast. One of the studies in Ghana is in collaboration with the University of Allied Health and involves a novel study of Onchocercal chorioretinitis using optical coherence tomography (OCT).
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Herricks JR,Hotez PJ,Wanga V,Coffeng LE,Haagsma JA,Basáñez MG,Buckle G,Budke CM,Carabin H,Fèvre EM,Fürst T,Halasa YA,King CH,Murdoch ME,Ramaiah KD,Shepard DS,Stolk WA,Undurraga EA,Stanaway JD,Naghavi M,Murray CJL, The global burden of disease study 2013: What does it mean for the NTDs? PLoS neglected tropical diseases. 2017 Aug; [PubMed PMID: 28771480]
Post RJ,Onyenwe E,Somiari SA,Mafuyai HB,Crainey JL,Ubachukwu PO, A guide to the Simulium damnosum complex (Diptera: Simuliidae) in Nigeria, with a cytotaxonomic key for the identification of the sibling species. Annals of tropical medicine and parasitology. 2011 Jun; [PubMed PMID: 21871165]
Level 3 (low-level) evidenceDuke BO, The population dynamics of Onchocerca volvulus in the human host. Tropical medicine and parasitology : official organ of Deutsche Tropenmedizinische Gesellschaft and of Deutsche Gesellschaft fur Technische Zusammenarbeit (GTZ). 1993 Jun; [PubMed PMID: 8367667]
Level 3 (low-level) evidenceSchulz-Key H, Observations on the reproductive biology of Onchocerca volvulus. Acta Leidensia. 1990; [PubMed PMID: 2378210]
Level 3 (low-level) evidenceUdall DN, Recent updates on onchocerciasis: diagnosis and treatment. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2007 Jan 1; [PubMed PMID: 17143815]
Level 3 (low-level) evidenceMackenzie CD,Huntington MK,Wanji S,Lovato RV,Eversole RR,Geary TG, The association of adult Onchocerca volvulus with lymphatic vessels. The Journal of parasitology. 2010 Feb; [PubMed PMID: 19803543]
Level 3 (low-level) evidenceTaylor MJ,Awadzi K,Basáñez MG,Biritwum N,Boakye D,Boatin B,Bockarie M,Churcher TS,Debrah A,Edwards G,Hoerauf A,Mand S,Matthews G,Osei-Atweneboana M,Prichard RK,Wanji S,Adjei O, Onchocerciasis Control: Vision for the Future from a Ghanian perspective. Parasites [PubMed PMID: 19154624]
Level 3 (low-level) evidenceKomlan K,Vossberg PS,Gantin RG,Solim T,Korbmacher F,Banla M,Padjoudoum K,Karabou P,Köhler C,Soboslay PT, Onchocerca volvulus infection and serological prevalence, ocular onchocerciasis and parasite transmission in northern and central Togo after decades of Simulium damnosum s.l. vector control and mass drug administration of ivermectin. PLoS neglected tropical diseases. 2018 Mar; [PubMed PMID: 29494606]
Budden FH, Route of entry of Onchocerca volvulus microfilariae into the eye. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1976; [PubMed PMID: 982529]
Level 3 (low-level) evidenceBasak SK,Hazra TK,Bhattacharya D, Persistent corneal edema secondary to presumed dead adult filarial worm in the anterior chamber. Indian journal of ophthalmology. 2007 Jan-Feb; [PubMed PMID: 17189893]
Level 3 (low-level) evidenceEgbert PR,Jacobson DW,Fiadoyor S,Dadzie P,Ellingson KD, Onchocerciasis: a potential risk factor for glaucoma. The British journal of ophthalmology. 2005 Jul; [PubMed PMID: 15965151]
Level 2 (mid-level) evidenceBerger RB,Blackwell NM,Lass JH,Diaconu E,Pearlman E, IL-4 and IL-13 regulation of ICAM-1 expression and eosinophil recruitment in Onchocerca volvulus keratitis. Investigative ophthalmology [PubMed PMID: 12202520]
Level 3 (low-level) evidenceKeiser PB,Reynolds SM,Awadzi K,Ottesen EA,Taylor MJ,Nutman TB, Bacterial endosymbionts of Onchocerca volvulus in the pathogenesis of posttreatment reactions. The Journal of infectious diseases. 2002 Mar 15; [PubMed PMID: 11920298]
Higazi TB,Filiano A,Katholi CR,Dadzie Y,Remme JH,Unnasch TR, Wolbachia endosymbiont levels in severe and mild strains of Onchocerca volvulus. Molecular and biochemical parasitology. 2005 May; [PubMed PMID: 15811532]
Level 3 (low-level) evidenceHall LR,Pearlman E, Pathogenesis of onchocercal keratitis (River blindness). Clinical microbiology reviews. 1999 Jul; [PubMed PMID: 10398675]
Level 3 (low-level) evidenceSemba RD,Murphy RP,Newland HS,Awadzi K,Greene BM,Taylor HR, Longitudinal study of lesions of the posterior segment in onchocerciasis. Ophthalmology. 1990 Oct; [PubMed PMID: 2243684]
Level 3 (low-level) evidenceBanla M,Tchalim S,Karabou PK,Gantin RG,Agba AI,Kére-Banla A,Helling-Giese G,Heuschkel C,Schulz-Key H,Soboslay PT, Sustainable control of onchocerciasis: ocular pathology in onchocerciasis patients treated annually with ivermectin for 23 years: a cohort study. PloS one. 2014; [PubMed PMID: 24887413]
Level 2 (mid-level) evidenceBraun G,McKechnie NM,Connor V,Gilbert CE,Engelbrecht F,Whitworth JA,Taylor DW, Immunological crossreactivity between a cloned antigen of Onchocerca volvulus and a component of the retinal pigment epithelium. The Journal of experimental medicine. 1991 Jul 1; [PubMed PMID: 2056276]
Level 3 (low-level) evidenceChandrashekar R,Ogunrinade AF,Alvarez RM,Kale OO,Weil GJ, Circulating immune complex-associated parasite antigens in human onchocerciasis. The Journal of infectious diseases. 1990 Nov; [PubMed PMID: 2230240]
Level 3 (low-level) evidenceBird AC,el-Sheikh H,Anderson J,Fuglsang H, Changes in visual function and in the posterior segment of the eye during treatment of onchocerciasis with diethylcarbamazine citrate. The British journal of ophthalmology. 1980 Mar; [PubMed PMID: 7387952]
Paul EV,Zimmerman LE, Some observations on the ocular pathology of onchocerciasis. Human pathology. 1970 Dec; [PubMed PMID: 5535426]
RODGER FC, The pathogenesis and pathology of ocular on-chocerciasis. Part IV. The pathology. American journal of ophthalmology. 1960 Mar; [PubMed PMID: 14438157]
Lupi O,Downing C,Lee M,Pino L,Bravo F,Giglio P,Sethi A,Klaus S,Sangueza OP,Fuller C,Mendoza N,Ladizinski B,Woc-Colburn L,Tyring SK, Mucocutaneous manifestations of helminth infections: Nematodes. Journal of the American Academy of Dermatology. 2015 Dec; [PubMed PMID: 26568337]
Ali MM,Baraka OZ,AbdelRahman SI,Sulaiman SM,Williams JF,Homeida MM,Mackenzie CD, Immune responses directed against microfilariae correlate with severity of clinical onchodermatitis and treatment history. The Journal of infectious diseases. 2003 Feb 15; [PubMed PMID: 12599094]
Level 3 (low-level) evidenceTamarozzi F,Halliday A,Gentil K,Hoerauf A,Pearlman E,Taylor MJ, Onchocerciasis: the role of Wolbachia bacterial endosymbionts in parasite biology, disease pathogenesis, and treatment. Clinical microbiology reviews. 2011 Jul; [PubMed PMID: 21734243]
Level 3 (low-level) evidenceSemba RD,Donnelly JJ,Young E,Green WR,Scott AL,Taylor HR, Experimental ocular onchocerciasis in cynomolgus monkeys. IV. Chorioretinitis elicited by Onchocerca volvulus microfilariae. Investigative ophthalmology [PubMed PMID: 2016131]
Level 3 (low-level) evidenceEnk CD, Onchocerciasis--river blindness. Clinics in dermatology. 2006 May-Jun; [PubMed PMID: 16714198]
Showler AJ,Nutman TB, Imported onchocerciasis in migrants and travelers. Current opinion in infectious diseases. 2018 Oct; [PubMed PMID: 30113326]
Level 3 (low-level) evidenceUnnasch TR,Golden A,Cama V,Cantey PT, Diagnostics for onchocerciasis in the era of elimination. International health. 2018 Mar 1; [PubMed PMID: 29471336]
Anderson J,Fuglsang H, Further studies on the treatment of ocular onchocerciasis with diethylcarbamazine and suramin. The British journal of ophthalmology. 1978 Jul; [PubMed PMID: 678497]
Basáñez MG,Pion SD,Boakes E,Filipe JA,Churcher TS,Boussinesq M, Effect of single-dose ivermectin on Onchocerca volvulus: a systematic review and meta-analysis. The Lancet. Infectious diseases. 2008 May; [PubMed PMID: 18471776]
Level 3 (low-level) evidenceOpoku NO,Bakajika DK,Kanza EM,Howard H,Mambandu GL,Nyathirombo A,Nigo MM,Kasonia K,Masembe SL,Mumbere M,Kataliko K,Larbelee JP,Kpawor M,Bolay KM,Bolay F,Asare S,Attah SK,Olipoh G,Vaillant M,Halleux CM,Kuesel AC, Single dose moxidectin versus ivermectin for Onchocerca volvulus infection in Ghana, Liberia, and the Democratic Republic of the Congo: a randomised, controlled, double-blind phase 3 trial. Lancet (London, England). 2018 Oct 6; [PubMed PMID: 29361335]
Level 1 (high-level) evidenceHoerauf A,Mand S,Volkmann L,Büttner M,Marfo-Debrekyei Y,Taylor M,Adjei O,Büttner DW, Doxycycline in the treatment of human onchocerciasis: Kinetics of Wolbachia endobacteria reduction and of inhibition of embryogenesis in female Onchocerca worms. Microbes and infection. 2003 Apr; [PubMed PMID: 12706439]
Level 3 (low-level) evidenceEvangelisto A,Werth V,Schumacher HR, What is that nodule? A diagnostic approach to evaluating subcutaneous and cutaneous nodules. Journal of clinical rheumatology : practical reports on rheumatic [PubMed PMID: 17023809]
Sauerbrey M, The Onchocerciasis Elimination Program for the Americas (OEPA). Annals of tropical medicine and parasitology. 2008 Sep; [PubMed PMID: 18718151]
Level 3 (low-level) evidenceFischer PU,King CL,Jacobson JA,Weil GJ, Potential Value of Triple Drug Therapy with Ivermectin, Diethylcarbamazine, and Albendazole (IDA) to Accelerate Elimination of Lymphatic Filariasis and Onchocerciasis in Africa. PLoS neglected tropical diseases. 2017 Jan; [PubMed PMID: 28056015]
Vinkeles Melchers NVS,Coffeng LE,Boussinesq M,Pedrique B,Pion SDS,Tekle AH,Zouré HGM,Wanji S,Remme JH,Stolk WA, Projected number of people with onchocerciasis-loiasis co-infection in Africa, 1995 to 2025. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2019 Jul 13; [PubMed PMID: 31304961]
Wanji S,Kengne-Ouafo JA,Esum ME,Chounna PW,Tendongfor N,Adzemye BF,Eyong JE,Jato I,Datchoua-Poutcheu FR,Kah E,Enyong P,Taylor DW, Situation analysis of parasitological and entomological indices of onchocerciasis transmission in three drainage basins of the rain forest of South West Cameroon after a decade of ivermectin treatment. Parasites [PubMed PMID: 25886166]
Kelly-Hope L,Paulo R,Thomas B,Brito M,Unnasch TR,Molyneux D, Loa loa vectors Chrysops spp.: perspectives on research, distribution, bionomics, and implications for elimination of lymphatic filariasis and onchocerciasis. Parasites [PubMed PMID: 28381279]
Level 3 (low-level) evidenceGardon J,Gardon-Wendel N,Demanga-Ngangue,Kamgno J,Chippaux JP,Boussinesq M, Serious reactions after mass treatment of onchocerciasis with ivermectin in an area endemic for Loa loa infection. Lancet (London, England). 1997 Jul 5; [PubMed PMID: 9217715]
Level 3 (low-level) evidenceFrancis H,Awadzi K,Ottesen EA, The Mazzotti reaction following treatment of onchocerciasis with diethylcarbamazine: clinical severity as a function of infection intensity. The American journal of tropical medicine and hygiene. 1985 May; [PubMed PMID: 4003668]
Awadzi K,Opoku NO,Attah SK,Lazdins-Helds JK,Kuesel AC, Diagnosis of O. volvulus infection via skin exposure to diethylcarbamazine: clinical evaluation of a transdermal delivery technology-based patch. Parasites [PubMed PMID: 26452723]
Stingl P,Pierce PF,Connor DH,Gibson DW,Straessle T,Ross MA,Ribas JL, Does dexamethasone suppress the Mazzotti reaction in patients with onchocerciasis? Acta tropica. 1988 Mar; [PubMed PMID: 2896449]
Level 3 (low-level) evidenceChandler RE, Serious Neurological Adverse Events after Ivermectin-Do They Occur beyond the Indication of Onchocerciasis? The American journal of tropical medicine and hygiene. 2018 Feb; [PubMed PMID: 29210346]
Newland HS,White AT,Greene BM,Murphy RP,Taylor HR, Ocular manifestations of onchocerciasis in a rain forest area of west Africa. The British journal of ophthalmology. 1991 Mar; [PubMed PMID: 2012784]
Level 3 (low-level) evidenceCooper PJ,Proaño R,Beltran C,Anselmi M,Guderian RH, Onchocerciasis in Ecuador: ocular findings in Onchocerca volvulus infected individuals. The British journal of ophthalmology. 1995 Feb; [PubMed PMID: 7696237]
Level 3 (low-level) evidenceAkama T,Freund YR,Berry PW,Carter DS,Easom EE,Jarnagin K,Lunde CS,Plattner JJ,Rock F,Stefanakis R,Fischer C,Bulman CA,Lim KC,Suzuki BM,Tricoche N,Mansour A,DiCosty U,McCall S,Carson B,McCall JW,McKerrow J,Hübner MP,Specht S,Hoerauf A,Lustigman S,Sakanari JA,Jacobs RT, Macrofilaricidal Benzimidazole-Benzoxaborole Hybrids as an Approach to the Treatment of River Blindness: Part 1. Amide Linked Analogs. ACS infectious diseases. 2020 Feb 14; [PubMed PMID: 31876154]