Introduction
Pressure injuries, also termed bedsores, decubitus ulcers, or pressure ulcers, are localized skin and soft tissue injuries that form as a result of prolonged pressure and shear, usually exerted over bony prominences.[1][2] These ulcers are present 70% of the time at the sacrum, ischial tuberosity, and greater trochanter. However, they can also occur in the occiput, scapula, elbow, heel, lateral malleolus, shoulder, and ear.[3] Besides bony prominences, they can also occur due to medical or other devices, such as cell phones.[4] Pressure injuries vary in severity and characteristics. Different medical fields have developed various classifications to improve communication. The 2 latest and most acceptable classifications were defined by the NPIAP and the International Statistical Classification of Diseases and Related Health Problems (ICD-11), released in 2019 and 2018, respectively.[4] With the COVID-19 pandemic, pressure ulcers increased, and the national economic burden worsened, shedding light on the topic.
Jean-Martin Charcot was a French doctor in the 19th century who studied many diseases, including decubitus ulcers. He noticed that patients who developed eschar of the buttocks and sacrum died after some time. He named this lesion "decubitus ominous," which meant death was inevitable after developing this lesion.[5]
In 2016, the National Pressure Ulcer Advisory Panel (NPUAP) released new terminology guidelines, and the preferred name is now "pressured injury" to "better reflect all forms of tissue damage, including the stage before skin breakdown." The organization also publically announced the change from NPUAP to the National Pressure Injury Advisory Panel (NPIAP).
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The development of pressure injuries is complex and multifactorial. External and internal factors co-occur to form these ulcers. Externally, prolonged pressure, friction, shear force, and moisture can lead to tissue deformation and ischemia. Internal factors such as malnutrition, anemia, and endothelial dysfunction can speed up the process of tissue damage.[6][7]
Decreased mobility, skin moisture, poor nutritional status, and loss of sensory perception stand out as the most common risk factors. However, researchers have also identified older age, cognitive impairment, and comorbid conditions affecting tissue healing.[1]
Prolonged pressure on tissues can cause capillary bed occlusion, reducing oxygen levels in the area. Over time, the ischemic tissue begins to accumulate toxic metabolites. Subsequently, tissue ulceration and necrosis occur. Immobility of only two hours in a bedridden patient or patient undergoing surgery is sufficient to form the foundation of a decubitus ulcer.[7]
The dysfunction of nervous regulatory mechanisms responsible for regulating local blood flow is also somewhat culpable in forming these ulcers.[8]
Patients with the following conditions exhibit a predisposition to decubitus ulcers:
- Neurologic disease
- Cardiovascular disease
- Prolonged anesthesia
- Dehydration
- Malnutrition
- Hypotension
- Surgical patients
Epidemiology
Pressure ulcers are a significant healthcare problem worldwide, which affects several thousands of people each year.[7] Up to 3 million adults are affected annually in the United States alone.[3] Pressure injury management is a significant source of economic burden. In 2019, Padula and Delarmente estimated that hospital-acquired pressure injury (HAPI) costs could exceed $26.8 billion.[9] Their study simulated an incidence of 8.3 HAPI per 100 acutely ill patients. This number is consistent with previous studies, which showed that 7.9% of at-risk patients had HAPI.[10]
Sacral decubitus ulcers usually occur in elderly patients. Patients who are incontinent, paralyzed, or debilitated are more prone to getting them. Patients with normal sensory status, mobility, and mental status are less likely to form these ulcers because their regular physiologic feedback system leads to frequent physical positional shifts. As stated above, older patients are more prone to sacral decubitus ulcers, and two-thirds of ulcers occur in patients older than 70 years. Some data show that 83% of hospitalized patients developed ulcers within 5 days of hospitalization.[7]
Pathophysiology
Decubitus ulcer formation is multifactorial, but these ulcers result in a common pathway to ischemia and necrosis. Tissues can sustain an abnormal amount of external pressure, but constant pressure exerted over a prolonged period is the main culprit. External pressure must exceed the arterial capillary pressure of 32 mm Hg to impede blood flow. The pressure must be greater than the venous capillary closing pressure of 8 to 12 mm Hg to impair venous blood return. Sustaining pressure above these values leads to tissue ischemia and necrosis.[11] This significant pressure can result from compression by a firm mattress, hospital bed railings, or any hard surface in contact with the patient.
In addition, the EPUAP emphasized the link between the pathophysiology of COVID-19 and the development of pressure ulcers. The panel attributed the pro-inflammatory cytokines interleukin-6 and tumor necrosis factor-alpha, abundant in COVID-19 patients, as a contributor to the onset and maintenance of inflammation following cell death and the formation of a pressure ulcer.[11] Friction caused by skin rubbing against surfaces like clothing or bedding can also lead to the development of ulcers by contributing to breaks in the superficial layers of the skin. Moisture can cause ulcers and worsen existing ulcers via tissue breakdown and maceration.
Histopathology
Histological studies of pressure ulcers reveal a dynamic process, including blanchable and non-blanchable erythema, decubitus dermatitis, decubitus ulcer, and black scab/gangrene. The initial change occurs in the vessels of the papillary dermis, followed by the necrosis of skin structures. The scab/gangrene is a full-thickness defect due to persistent ischemia and anoxemia or a sudden occlusion of large vessels due to shear injury.[12]
Detailed analysis of chronic pressure ulcers showed the presence of densely aggregated bacterial colonies, often present in the extracellular matrix. Still, these findings were not present in acutely developed ulcers.[13] Some studies have also investigated the histopathology of exposed bone in sacral pressure ulcers. Interestingly, there is a low incidence of osteomyelitis in the exposed bone of sacral ulcers, and when present, the disease is focal and restricted to superficial layers of cortical bone.[14]
History and Physical
In patients with normal sensation, mobility, and mental status, prolonged pressure causes discomfort and pain, prompting a change in body position. However, most patients with pressure ulcers lack those characteristics. A patient's attendant typically reports pressure injuries. Due to reduced sensation at the lesion site, patients may be unaware of their injuries. Pus or blood discharge may stain the patient's clothes or bedsheets. The clinical presentation may vary between different body sites as skin, soft tissue, and muscle resist external pressure differently. The most common anatomical locations are the sacrum, ischial tuberosity, and greater trochanter. Other areas at risk include the occiput, scapula, elbow, heel, lateral malleolus, shoulder, and ear.[3] The muscle becomes ischemic and necrotic before skin breakdown can occur, which can be deceiving to the clinician's observation, undermining the depth or extent of the ulcer.
A thorough history and overall assessment of the patient are paramount. Any neurological or cardiovascular disease will increase the predictive risk factor of a pressure ulcer and likely decrease healing potential. In addition, the patient's nutrition and hydration status, cognitive impairment, and mobility should be evaluated.[15]
The initial evaluation of patients with pressure ulcers involves a detailed history. The clinician should gather the following:
- Duration of immobility or being bedridden
- Duration of hospital stay
- Associated medical cause that has caused the injury (eg, paraplegia, quadriplegia, stroke, road traffic accident resulting in immobility)
- The natural history of the injury and the site at which it first developed. Duration of injury and any size increases should also be noted
- A brief history of any systemic diseases is also necessary. Diseases like diabetes mellitus, peripheral vascular disease, and malignancy prevent or slow wound healing
- If the patient can precisely localize the site of the ulcer or any associated pain or if the patient is unaware because of paraplegia or another medical
- Discharge or foul odor from the ulcer site - note it
Evaluation
Examine the following in a patient with a PI:
- Ulcer history, including etiology, duration, and previous treatment
- Staging by thoroughly examining the depth of the wound, which this activity will cover in detail under "staging"
- Size of the affected area
- Sinus tracts, undermining, and tunneling
- The presence of drainage
- The presence of necrotic tissue
When evaluating the wound characteristics, it is also important to keep risk assessment instruments in mind to reduce the risk of a PI incidence. There are 3 risk assessment scales: Waterlow, Norton, and Braden. The Braden scale is the most common and accepted in the current literature. It includes 5 sections worth 4 points and 1 section worth 3 points. Sum the points to provide a risk assessment score.
Braden Scale
- Sensory perception (1-4; completely limited, very limited, slightly limited, or no impairment)
- Mobility (1-4; completely immobile, very limited, slightly limited, or no limitations)
- Moisture (1-4; constantly moist, very moist, occasionally moist, rarely moist)
- Nutrition (1-4; very poor, probably inadequate, adequate, excellent)
- Activity (1-4; bedfast, chairfast, walks occasionally, walks frequently)
- Friction and Shear (1-3; problem, potential problem, no apparent problem)
Scores
- Mild Risk = 15 to 18
- Moderate Risk = 13 to 14
- High Risk = 10 to 12
- Very High Risk = 9 or below
Treatment / Management
Before discussing different treatments for pressure ulcers, it is essential to emphasize that prevention intervention is the best treatment. Prevention consists of maintaining and improving tissue tolerance and appropriate offloading. This could be achieved through excellent skincare, adequate hydration/nutrition, pressure dispersion cushions, turning schedules, and support surfaces. The skin needs to be clean and dry. Good hydration and nutrition are paramount, and nutritional supplements could benefit patients with limited oral intake. Pressure redistribution is possible through beds and chairs that avoid direct pressure on anatomical risk areas. Turning every 4 hours on a viscoelastic foam mattress/surface results in fewer pressure ulcers than turning every 2 hours on a standard mattress. Finally, support surfaces should be chosen according to the level of risk, ulcer stage, mobility, patient comfort, and need for microclimate control.
After forming a pressure ulcer, actively offload the affected anatomical area, ensure adequate drainage if an infection is present, debride devitalized tissue, and provide optimal wound care.[16] Redistribute pressure through active patient repositioning, immersive beds, special dressings, and refitting prosthetics for offloading, similar to the mentioned prevention strategies.[16] Drainage should be performed if an abscess is present. Iodine, silver sulfadiazine, hydrogen peroxide, or Dakin solution can be applied temporarily if an infection is suspected, but they can retard wound healing in the long term. Antibiotics should only be an option if significant cellulitis or systemic signs of infection are present. Counterintuitively, even when an exposed bone is present in sacral decubitus ulcers, studies show a low incidence of osteomyelitis.[14] (B3)
Mechanical debridement is usually necessary to remove devitalized tissue and biofilms that prevent wound healing. Do not recommend it in cases of dry eschar without purulence or fluctuance.[16] Dressings can vary according to the ulcer stage, infection, and presence of exudate. However, according to NPIAP, the recommended dressing is foam silicone dressings. In a comprehensive program to reduce the incidence of hospital-acquired pressure ulcers, Swafford and colleagues obtained great results using Allevyn Life silicone adhesive dressing for any PI with a Braden score of 14 or less.[10](B3)
Algorithm for Dressings of Pressure Injury Management
If the wound is infected, determine the amount of exudate and manage according to the following:
- None: Use silver, honey, foam
- Some: Use alginate, negative pressure wound therapy, silver, gauze, foam
- Copious: Use alginate, negative pressure wound therapy, gauze, foam
If the wound is not infected, determine the amount of the exudate and manage according to the following:
- None: Use hydrogel, transparent film
- Some: Use alginate, hydrocolloid, negative pressure wound therapy, gauze, foam
- Copious: Use alginate, hydrocolloid, negative pressure wound therapy, gauze, foam [16] (B3)
In some cases, urinary and fecal diversion may be necessary depending on the site of the ulcer, being prone to urine or fecal contamination. The depth and severity of the ulcer determine whether surgical management is required. Clean and drain the ulcer to remove dead tissue and debris. Vacuum-assisted closure or negative pressure wound therapy may be a preoperative option to provide a favorable wound for the surgical closer.[17] Surgical management aims to fill the dead space and provide durable skin through flap reconstruction. The ideal reconstructive surgical candidate has stage 1 or 2 wounds without purulence, a well-granulated base, and a region well-protected from soiling. Assess the patient for nutrition, including Prealbumin levels, diabetes control through monitoring sugar levels, and the absence of acute medical conditions. [16](B3)
Surgical treatment options include the following:
- Surgical debridement: devitalized, infected tissue or bone is removed
- Skin graft: high failure rates in later stages due to low long-term durability
- Pedicle muscle, myocutaneous, fasciocutaneous flaps, or free flaps: flap choice depends on the anatomical location, the need for ambulation, and comorbidities[18]
Table. Flap Options for Common Anatomic Sites of Pressure Injuries [18]
| Anatomical Site | Commonly Used Options for Closure |
| Sacral | Gluteal myocutaneous flap, gluteal fasciocutaneous rotation-advancement flap, gluteal fasciocutaneous V-Y advancement flap, superior gluteal Artery perforator flap |
| Ischial | Inferior gluteal myocutaneous flap, gracilis myocutaneous flap, bicep femoris myocutaneous flap, lateral thigh fasciocutaneous flap, anterolateral thigh fasciocutaneous flap, rectus abdominis myocutaneous flap, inferior gluteal artery perforator flap, profunda femoris artery perforator flap |
| Trochanteric | Tensor fascia latae myocutaneous flap, vastus lateralis myocutaneous flap, anterolateral thigh perforator flap, expansive gluteal myocutaneous flap |
| Foot/ankle | Reverse sural artery flap, medial plantar flap, extensor digitorum brevis flap, propellerr flaps, free tissue transfer |
Table Reference [18]
Evidence suggests that hyperbaric oxygen therapy can help with wound healing, as it improves oxygenation in and around the area of the wound.[19](A1)
The treatment of decubitus ulcers has its basis in the following:
- Prevention of additional ulcers
- Decreasing pressure on the wound
- Wound management
- Surgical intervention
- Improving the nutritional status
Generally, stage 1 and 2 ulcers do not require operative measures; stage 3 and 4 ulcers may require surgical intervention.
Differential Diagnosis
The differential diagnosis of pressure ulcers includes the following:
Staging
There are many different ways to stage pressure ulcers. In 2020, Kottner and colleagues reviewed all the most common classifications globally. The study included scientists from 9 different countries. Their main conclusion was the conceptual meaning of different systems is comparable, and clinicians are encouraged to use the classification most used in their geographic region. The most widely accepted classification system in the United States is the NPIAP system,[4] which uses ulcer depth to classify these ulcers.
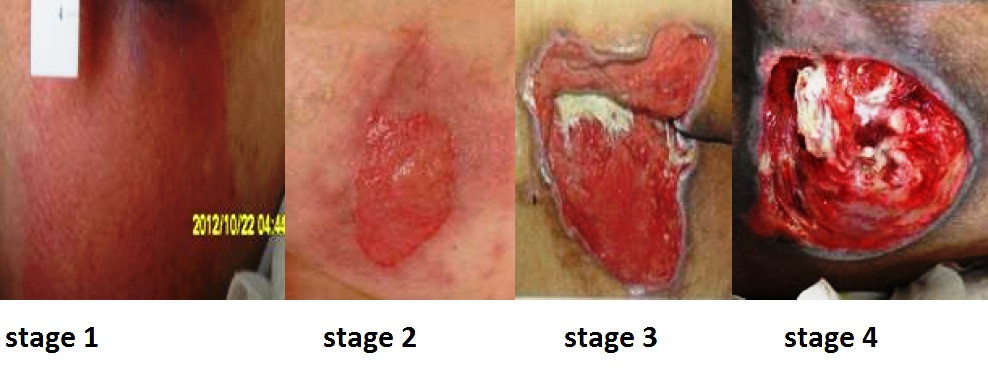
The stages are as follows:
- Stage 1: The skin is intact with nonblanchable erythema.
- Stage 2: There is partial-thickness skin loss involving the epidermis and dermis.
- Stage 3: A full-thickness loss of skin extends to the subcutaneous tissue but does not cross the fascia beneath it. Slough or eschar may be visible, and the lesion may be foul-smelling.
- Stage 4: Full-thickness skin loss extends through the fascia with considerable tissue loss. There may be muscle, bone, tendon, or joint involvement.
- Unstageable: The depth is unknown because slough or eschar obscures the extent of tissue damage.
Deep Tissue Injury (DTI) is another category mentioned in the NPIAP guidelines. This injury occurs with prolonged pressure and shear forces at the bone-muscle interface. The result is intact or non-intact skin with persistent, non-blanched, deep red, maroon, or purple discoloration. DTI cannot be used to describe vascular, traumatic, neuropathic, or dermatologic injuries.
Prognosis
The prognosis for patients with pressure ulcers varies depending on the anatomic location, stage of injury, and treatment regimen. Most study results compare treatment efficacy by measuring the reduction in the incidence of pressure ulcers in a determined facility as a preventive measurement instead of the healing rate after treatment initiation.
However, after 6 months of treatment, stage 2 pressure injuries have been documented to heal over 70% of the time, stage 3 about 50%, and stage 4 approximately 30%.[21] In another study where stages did not separate rates, 41.7% of patients had their pressure ulcers resolved in an average follow-up of 1.8 years.[22] In the same study, they also evaluated the recurrence rate according to the anatomic location: sacral ulcers (57%), ischial (14%), trochanteric (7%), calcaneus (7%), and others (14%).[22]
Factors that affect prognosis include advancing age, the size and stage of PI, nutritional status, and chronic comorbidities.[23] Individuals with a higher mean body mass index, higher mean hemoglobin, and a higher rate of undergoing reconstructive plastic surgical procedures have also shown a better pressure ulcer healing rate.[22] Although outcomes have been difficult to study, there is general agreement that most of the time, lifelong treatment and prevention measures are necessary for these patients.[24]
Complications
Complications often develop with decubitus ulcers. The most common problem is infection. Grade 3 and 4 ulcers require intensive management as their complications can be life-threatening. Microbial analysis has shown that aerobic and anaerobic bacteria are present in the lesions.[25] If the infection spreads to deeper tissues and bone, periostitis, osteomyelitis, septic arthritis, and sinus formation can result. The invasion of the infective agent results in fatal consequences because septicemia is challenging to manage in an already debilitated patient.
These wounds are catabolic, which causes severe fluid and protein loss, which can result in hypoproteinemia or malnutrition. Up to 50 grams of body protein can be lost daily due to a draining ulcer.[25]
Chronic decubitus ulcers can cause chronic anemia or secondary amyloidosis. Anemia also occurs secondary to chronic water loss and bleeding.[25]
If there is inadequate postoperative care, complications secondary to reconstructive surgery can occur. These include hematoma or seroma formation, wound dehiscence, abscess formation, or postoperative wound sepsis.
This condition was also shown to be strongly associated with an increased risk of mortality. Older patients with pressure injuries have a 3.6-fold increased mortality rate within 21 months compared to patients without a pressure injury. However, the literature has debated the relationship between causation and correlation. Thomas et al showed evidence that pressure injuries are not a direct cause of mortality, suggesting that the same comorbidities responsible for the increased risk of death also increase the chance of a pressure injury.[26]
Postoperative and Rehabilitation Care
The same risk factors present before surgery should still be reinforced after surgery, including:
- offloading
- sufficient skincare
- incontinence control
- nutritional status [18]
When medical staff shifts patients from the operating table to their air-fluid beds, they must avoid excessive shearing and stretch on skin flaps. Patients are positioned flat on their support surfaces for the first 4 weeks, after which they can place themselves in a semi-sitting position. The patient only starts to sit for 10 minutes after 6 weeks of the surgical procedure. After these sitting periods, the flap should be examined for discoloration and wound edge separation. Over 2 weeks, the sitting periods will increase to 2 hours in 10-minute increments. Patients will also learn to lift for 10 seconds every 10 minutes to relieve pressure.
The patient, family members, and social support team must agree on the postoperative care plan. If the patient does not have good social support at home, inpatient rehabilitation or a skilled nursing facility is recommended.[18]
Consultations
Managing pressure injuries should always be done with an interprofessional approach. Usually, a general surgery consultation is necessary for patients with sacral decubitus ulcers, especially those with deep ulcers. A wound care specialist or a dermatologist is involved in non-healing ulcers. Podiatrists should be involved with foot and ankle ulcers. If any associated medical conditions affect the wound healing process, an internal medicine specialist should be involved in managing the case. Patients who have contractures or have spastic paralysis have regular physiotherapies.
Deterrence and Patient Education
Patients and their families should understand that preventing recurrence requires commitment and responsibility. They should receive education on how to manage their condition in the hospital and as well as in their homes. They should be familiar with warning signs like skin discoloration, ulceration, discharge, a foul smell from the ulcer site, and body areas with decreased or no sensation.
Diets for patients with pressure injuries should include adequate amounts of protein, vitamins, and minerals.[18] The patient should move or turn every 4 hours; if they cannot turn themselves, they should ask someone to help them. Patients should use air or water mattresses in their homes; active mattress use significantly improves resting blood flow, post-occlusive reactive hyperemia, and baseline skin temperature. These results suggest that active mattress use can improve endothelial function.[27]
Pearls and Other Issues
Pressure injuries occur when there is prolonged pressure on specific body areas susceptible to friction and shear force injuries. Pressure ulcers vary in size, depth, and chronicity. A staging classification system helps with interprofessional team communication and treatment guidance. Consulting with a clinician helps guide treatment and yield better results.
Enhancing Healthcare Team Outcomes
The primary goal is to prevent a pressure injury. This goal requires an interprofessional team, including primary care providers, wound care specialists, surgeons, specialty-trained wound nurses, physical therapists, and nurse aides. Nurses provide care, monitor patients, and notify the team of issues. Nurse aides are often responsible for turning and repositioning patients. Tissue cultures are often necessary. Depending on culture results, managing this condition can also involve the infectious disease and pharmacy team. The patient should be kept pain-free by giving analgesics. They should try to increase physical activity, which a nurse's aide, medical assistant, or rehab nurse can facilitate. Frequent follow-ups are an absolute necessity, and a team approach to patient education and pressure injury management involving the wound care nurse and wound care clinician lead to the best results.
Media
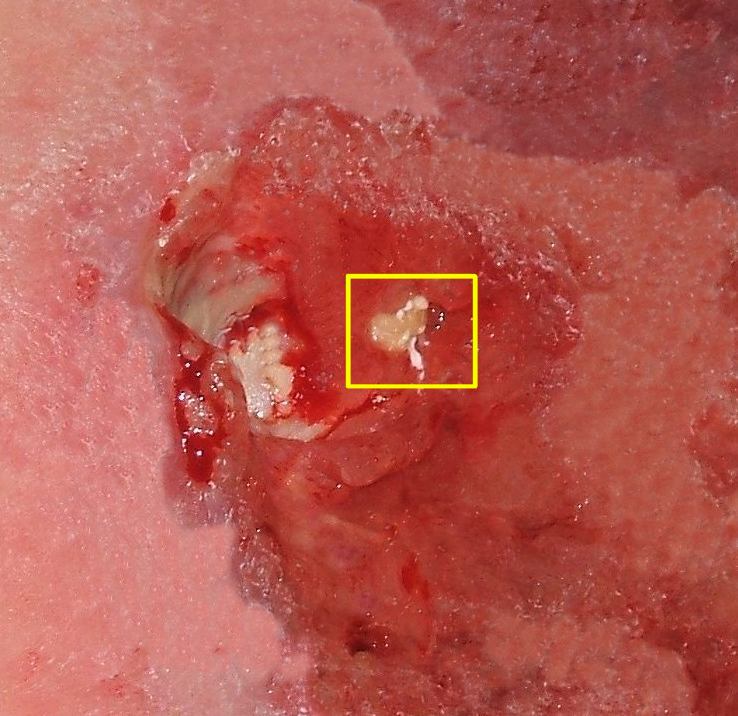
(Click Image to Enlarge)
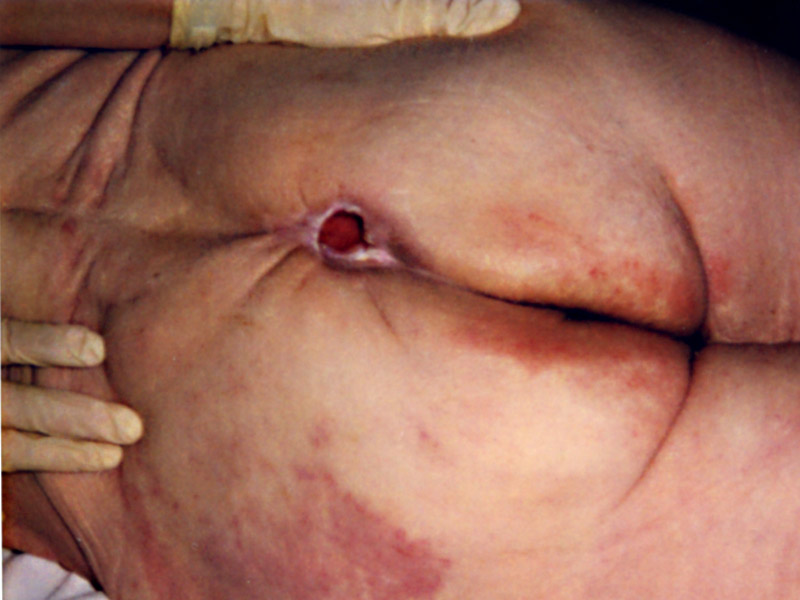
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Chou R, Dana T, Bougatsos C, Blazina I, Starmer AJ, Reitel K, Buckley DI. Pressure ulcer risk assessment and prevention: a systematic comparative effectiveness review. Annals of internal medicine. 2013 Jul 2:159(1):28-38. doi: 10.7326/0003-4819-159-1-201307020-00006. Epub [PubMed PMID: 23817702]
Level 1 (high-level) evidenceGaspar S, Peralta M, Marques A, Budri A, Gaspar de Matos M. Effectiveness on hospital-acquired pressure ulcers prevention: a systematic review. International wound journal. 2019 Oct:16(5):1087-1102. doi: 10.1111/iwj.13147. Epub 2019 Jul 1 [PubMed PMID: 31264345]
Level 1 (high-level) evidenceMervis JS, Phillips TJ. Pressure ulcers: Pathophysiology, epidemiology, risk factors, and presentation. Journal of the American Academy of Dermatology. 2019 Oct:81(4):881-890. doi: 10.1016/j.jaad.2018.12.069. Epub 2019 Jan 18 [PubMed PMID: 30664905]
Kottner J, Cuddigan J, Carville K, Balzer K, Berlowitz D, Law S, Litchford M, Mitchell P, Moore Z, Pittman J, Sigaudo-Roussel D, Yee CY, Haesler E. Pressure ulcer/injury classification today: An international perspective. Journal of tissue viability. 2020 Aug:29(3):197-203. doi: 10.1016/j.jtv.2020.04.003. Epub 2020 May 1 [PubMed PMID: 32414554]
Level 3 (low-level) evidenceLevine JM. Historical perspective on pressure ulcers: the decubitus ominosus of Jean-Martin Charcot. Journal of the American Geriatrics Society. 2005 Jul:53(7):1248-51 [PubMed PMID: 16108947]
Level 3 (low-level) evidenceAnders J, Heinemann A, Leffmann C, Leutenegger M, Pröfener F, von Renteln-Kruse W. Decubitus ulcers: pathophysiology and primary prevention. Deutsches Arzteblatt international. 2010 May:107(21):371-81; quiz 382. doi: 10.3238/arztebl.2010.0371. Epub 2010 May 28 [PubMed PMID: 20539816]
Bansal C, Scott R, Stewart D, Cockerell CJ. Decubitus ulcers: a review of the literature. International journal of dermatology. 2005 Oct:44(10):805-10 [PubMed PMID: 16207179]
van Marum RJ, Meijer JH, Ribbe MW. The relationship between pressure ulcers and skin blood flow response after a local cold provocation. Archives of physical medicine and rehabilitation. 2002 Jan:83(1):40-3 [PubMed PMID: 11782831]
Padula WV, Delarmente BA. The national cost of hospital-acquired pressure injuries in the United States. International wound journal. 2019 Jun:16(3):634-640. doi: 10.1111/iwj.13071. Epub 2019 Jan 28 [PubMed PMID: 30693644]
Swafford K, Culpepper R, Dunn C. Use of a Comprehensive Program to Reduce the Incidence of Hospital-Acquired Pressure Ulcers in an Intensive Care Unit. American journal of critical care : an official publication, American Association of Critical-Care Nurses. 2016 Mar:25(2):152-5. doi: 10.4037/ajcc2016963. Epub [PubMed PMID: 26932917]
Gefen A, Ousey K. COVID-19: pressure ulcers, pain and the cytokine storm. Journal of wound care. 2020 Oct 2:29(10):540-542. doi: 10.12968/jowc.2020.29.10.540. Epub [PubMed PMID: 33052791]
Witkowski JA, Parish LC. Histopathology of the decubitus ulcer. Journal of the American Academy of Dermatology. 1982 Jun:6(6):1014-21 [PubMed PMID: 7096663]
Rhoads DD, Wolcott RD, Percival SL. Biofilms in wounds: management strategies. Journal of wound care. 2008 Nov:17(11):502-8 [PubMed PMID: 18978690]
Wong D, Holtom P, Spellberg B. Osteomyelitis Complicating Sacral Pressure Ulcers: Whether or Not to Treat With Antibiotic Therapy. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2019 Jan 7:68(2):338-342. doi: 10.1093/cid/ciy559. Epub [PubMed PMID: 29986022]
Munoz N, Posthauer ME, Cereda E, Schols JMGA, Haesler E. The Role of Nutrition for Pressure Injury Prevention and Healing: The 2019 International Clinical Practice Guideline Recommendations. Advances in skin & wound care. 2020 Mar:33(3):123-136. doi: 10.1097/01.ASW.0000653144.90739.ad. Epub [PubMed PMID: 32058438]
Level 1 (high-level) evidenceBoyko TV, Longaker MT, Yang GP. Review of the Current Management of Pressure Ulcers. Advances in wound care. 2018 Feb 1:7(2):57-67. doi: 10.1089/wound.2016.0697. Epub [PubMed PMID: 29392094]
Level 3 (low-level) evidenceBatra RK, Aseeja V. VAC Therapy in Large Infected Sacral Pressure Ulcer Grade IV-Can Be an Alternative to Flap Reconstruction? The Indian journal of surgery. 2014 Apr:76(2):162-4. doi: 10.1007/s12262-012-0770-7. Epub 2012 Dec 14 [PubMed PMID: 24891788]
Ricci JA, Bayer LR, Orgill DP. Evidence-Based Medicine: The Evaluation and Treatment of Pressure Injuries. Plastic and reconstructive surgery. 2017 Jan:139(1):275e-286e. doi: 10.1097/PRS.0000000000002850. Epub [PubMed PMID: 28027261]
Kranke P, Bennett MH, Martyn-St James M, Schnabel A, Debus SE, Weibel S. Hyperbaric oxygen therapy for chronic wounds. The Cochrane database of systematic reviews. 2015 Jun 24:2015(6):CD004123. doi: 10.1002/14651858.CD004123.pub4. Epub 2015 Jun 24 [PubMed PMID: 26106870]
Level 1 (high-level) evidenceOkhovati S, Esmaeili M, Shariat E. Effect of Intensive Care Unit Nurses' Empowerment Program on Ability in Visual Differential Diagnosis of Pressure Ulcer Classification. Critical care nursing quarterly. 2019 Jan/Mar:42(1):89-95. doi: 10.1097/CNQ.0000000000000242. Epub [PubMed PMID: 30507669]
Bluestein D,Javaheri A, Pressure ulcers: prevention, evaluation, and management. American family physician. 2008 Nov 15; [PubMed PMID: 19035067]
Walter GP, Seidel W, Giustina RD, Bins-Ely J, Maurici R, Narciso-Schiavon JL. PROGNOSTIC FACTORS IN PATIENTS WITH PRESSURE SORES IN A UNIVERSITY HOSPITAL IN SOUTHERN BRAZIL. Acta ortopedica brasileira. 2017 Nov-Dec:25(6):243-247. doi: 10.1590/1413-785220172506169042. Epub [PubMed PMID: 29375252]
Takahashi PY. Pressure ulcers and prognosis: candid conversations about healing and death. Geriatrics. 2008 Nov:63(11):6-9 [PubMed PMID: 18998761]
Qaseem A, Humphrey LL, Forciea MA, Starkey M, Denberg TD, Clinical Guidelines Committee of the American College of Physicians. Treatment of pressure ulcers: a clinical practice guideline from the American College of Physicians. Annals of internal medicine. 2015 Mar 3:162(5):370-9. doi: 10.7326/M14-1568. Epub [PubMed PMID: 25732279]
Level 1 (high-level) evidenceTeasell R, Dittmer DK. Complications of immobilization and bed rest. Part 2: Other complications. Canadian family physician Medecin de famille canadien. 1993 Jun:39():1440-2, 1445-6 [PubMed PMID: 8324412]
Thomas DR, Goode PS, Tarquine PH, Allman RM. Hospital-acquired pressure ulcers and risk of death. Journal of the American Geriatrics Society. 1996 Dec:44(12):1435-40 [PubMed PMID: 8951312]
Level 2 (mid-level) evidenceBaker G, Bloxham S, Laden J, Gush R. Vascular endothelial function is improved after active mattress use. Journal of wound care. 2019 Oct 2:28(10):676-682. doi: 10.12968/jowc.2019.28.10.676. Epub [PubMed PMID: 31600104]