Introduction
Cutaneous lupus erythematosus (CLE) can present in three forms: acute cutaneous lupus erythematosus (ACLE), subacute cutaneous lupus erythematosus (SCLE), and chronic cutaneous lupus erythematosus (CCLE). CCLE can be further be subdivided into chronic subtypes consisting of tumid lupus erythematosus (TLE), discoid lupus erythematosus (DLE), chilblain lupus erythematosus, and lupus panniculitis.[1] Although these forms possess morphologies and histological features distinct from one another, more than one form can co-exist in the same patient.[2][3][4]
Although tumid lupus erythematosus (TLE) is currently considered to be a subtype of cutaneous lupus erythematosus (CLE), TLE differs from the other subtypes of cutaneous lupus erythematosus in that an association with systemic lupus erythematosus (SLE) is rare. Because of this weak association with SLE and a relative lack of serologic abnormalities in patients with TLE, some consider TLE to be an entity separate from lupus. It has also been postulated that TLE is in the same spectrum as lymphocytic infiltrate of Jessner and reticular erythematous mucinosis (REM) due to similar findings on histology.
Tumid lupus erythematosus (TLE) typically presents as annular, indurated, erythematous, edematous papules and plaques without epidermal involvement. If any of these features are recognized, and epidermal involvement is likely, a diagnosis of DLE should be suspected. Typical locations of TLE are the face and trunk, and lesions respond well to photoprotection, topical corticosteroids, and antimalarials.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
To date, no distinct etiology for TLE has been identified. However, triggering factors such as ultraviolet (UV) radiation have been implicated in worsening lesions of TLE. Its association with autoimmune disease has been controversial; if an autoimmune disease is suspected, an autoimmune workup may be initiated.[5][6] Immunity dysregulation with suppression of T cells is hypothesized. [7] Association with smoking and drugs like tumor necrosis factor antagonists, monoclonal antibodies, angiotensin-converting enzyme inhibitors, thiazide diuretics, and highly active antiretroviral therapy was reported.[8][9]
Epidemiology
CCLE, in general, occurs more frequently in the female population. TLE is rare relative to DLE. Incidence and prevalence of TLE among different races and ethnicities is not known. Men and women have almost equal predilection to TLE.[10] The age of onset is usually around thirty to forty years.[11]
Pathophysiology
Cutaneous lupus has a complex pathogenesis that relies on the interplay between genetic and environmental components. For all types of CCLE, including tumid lupus, UV radiation (specifically UVB) serves as a trigger. Immune alterations have also been implicated in the pathogenesis of TLE, specifically the decrease of T-regulatory cells and epidermal Langerhans cells and increased plasmacytoid dendritic cells. There is upregulation of type-1 interferon, tumor necrosis factor-alpha (TNF-alpha), and Th17 cells.[12] It has been postulated that tobacco smoking is a risk factor for TLE. It has also been suggested that rare drug-induced forms of TLE exist in association with TNF-alpha inhibitors, thiazide diuretics, highly active antiretroviral therapy (HAART), angiotensin-converting enzyme (ACE) inhibitors, bortezomib, and ustekinumab therapy.
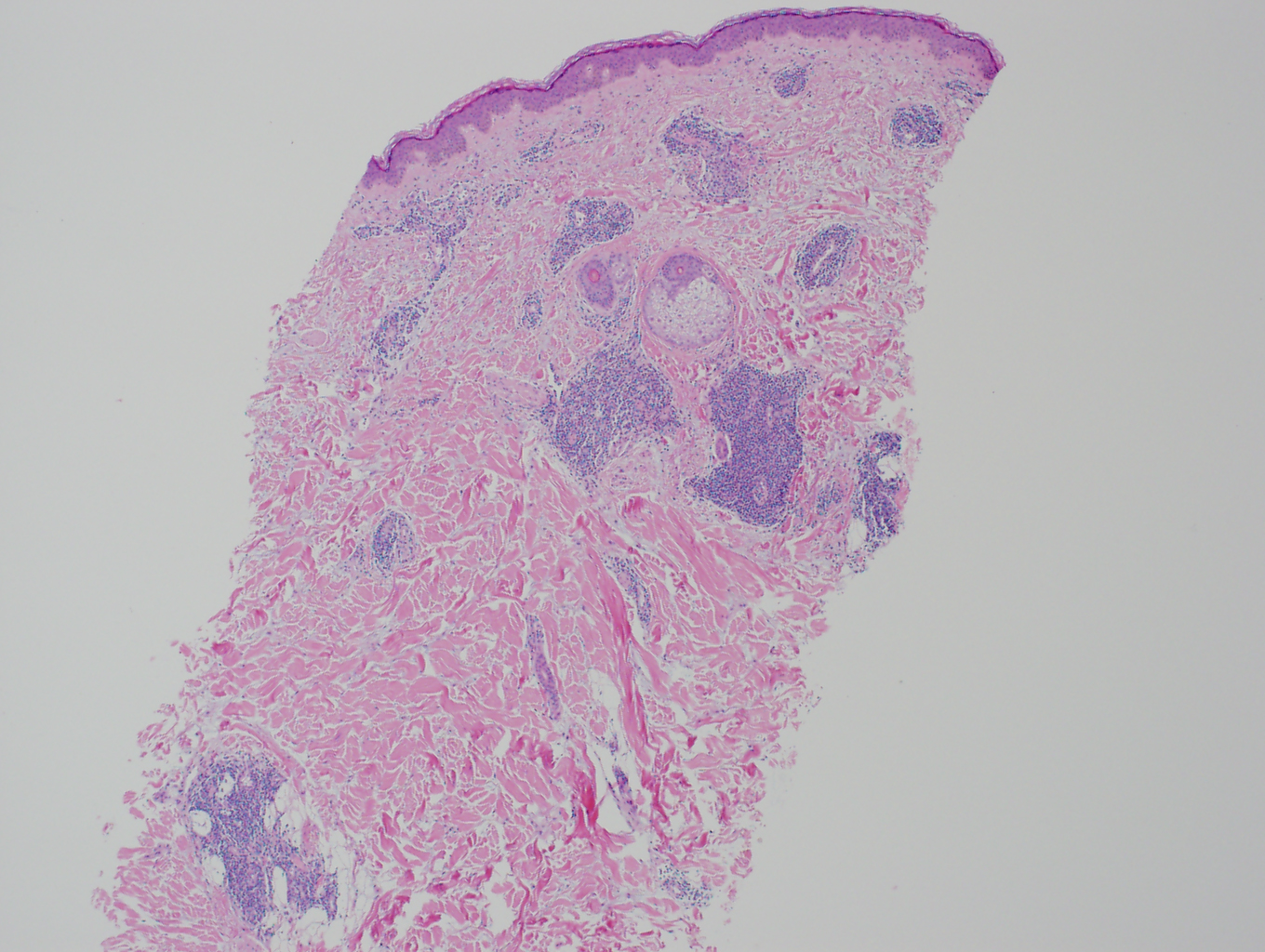
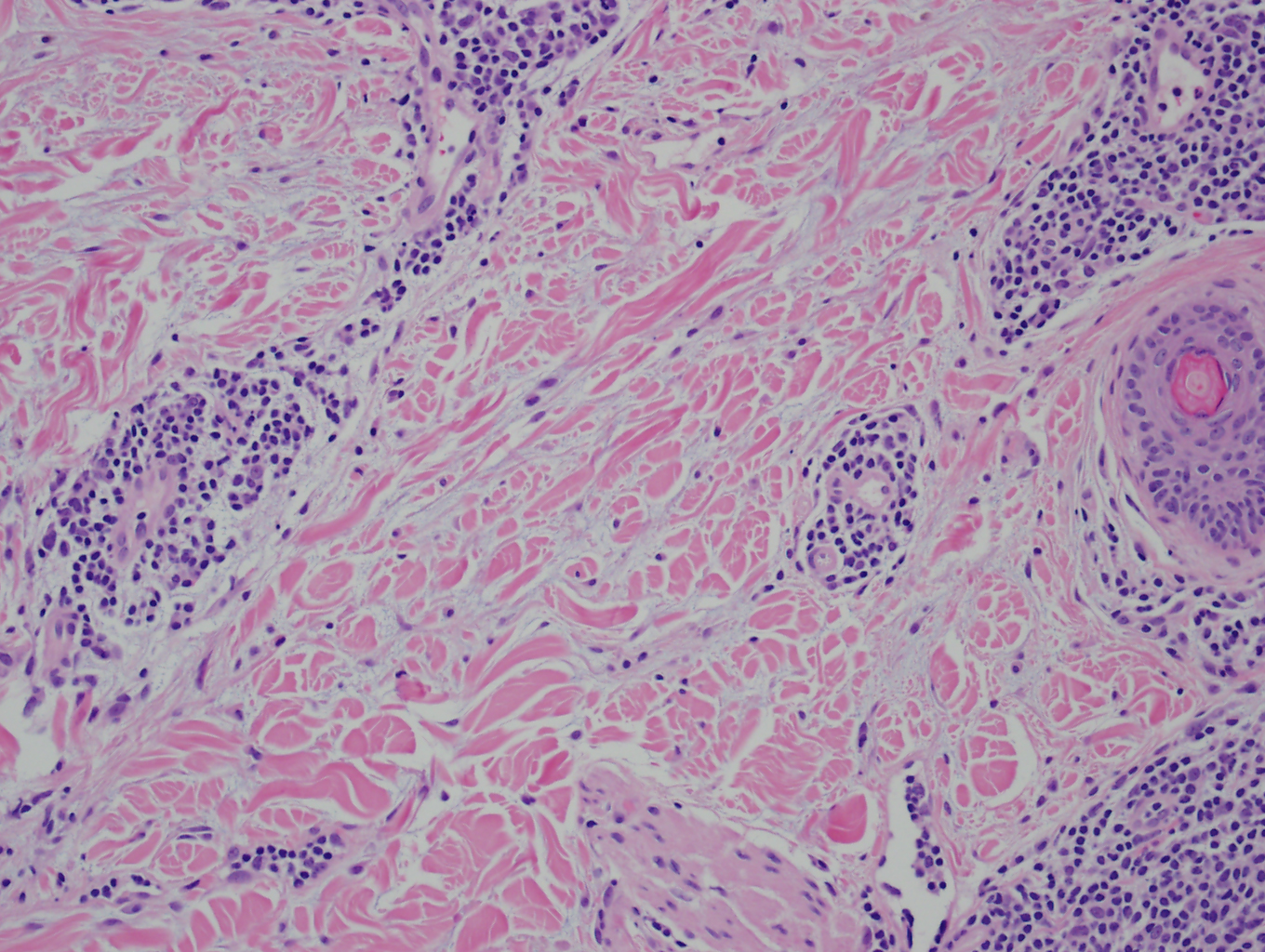
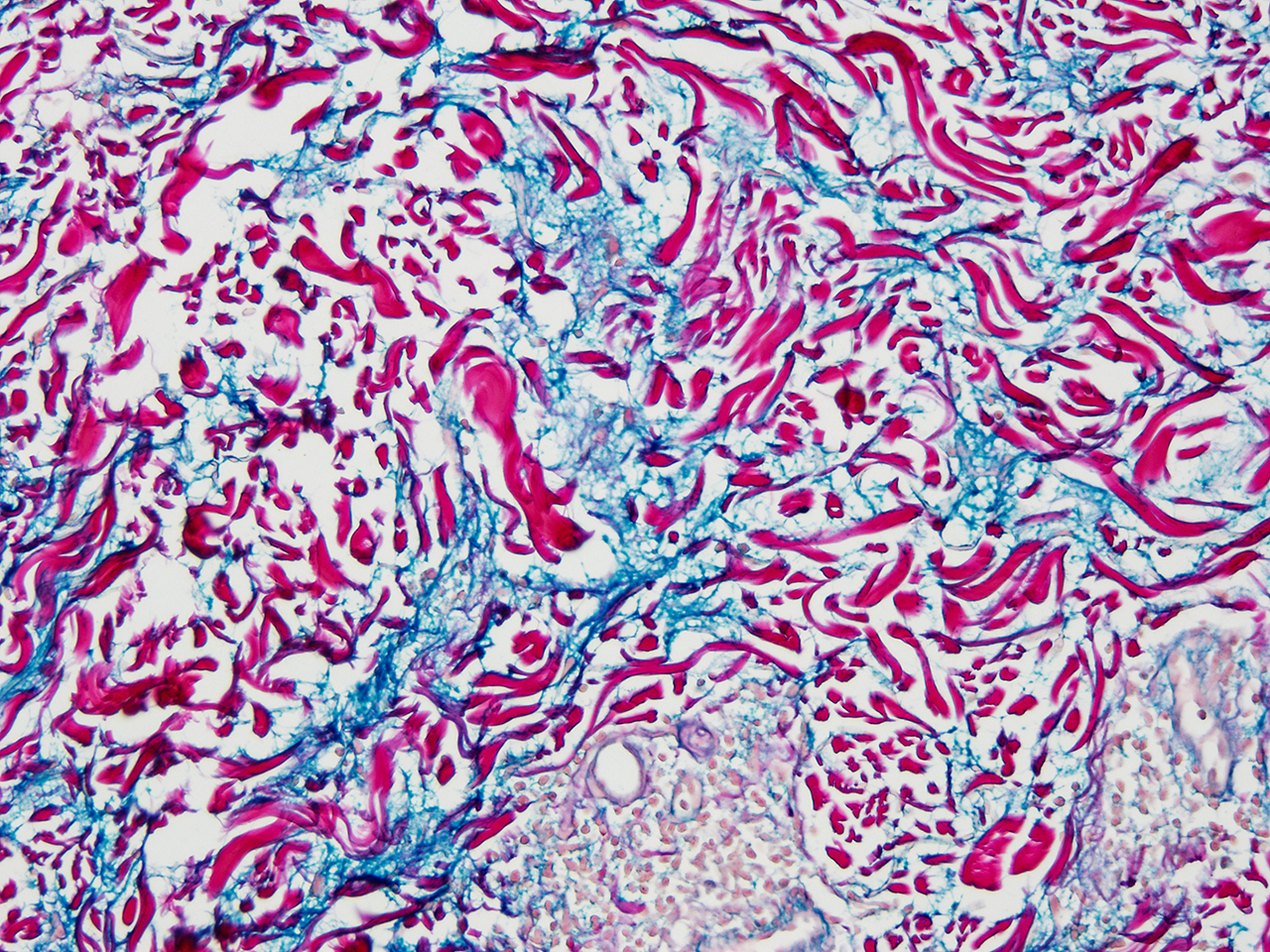
Histopathology
TLE is distinguished by abundant dermal mucin deposition and a superficial and deep perivascular and periadnexal lymphocytic infiltrate. Edema in the papillary dermis is noted. There is no involvement of the epidermis or dermo-epidermal junction. Lack of atrophy, scarring, follicular plugging, and dyspigmentation are the salient features of TLE. Direct immunofluorescence studies are usually negative. It is important to note that reticular erythematous mucinosis (REM), and Jessner's lymphocytic infiltrate are indistinguishable histologically from TLE.[13] See images 1, 2, and 4.
History and Physical
History is a valuable tool in evaluating a patient for TLE. Worsening of the eruption with sun exposure supports a diagnosis of TLE, although this finding is not specific to TLE. A full-body skin exam should be performed when a diagnosis of TLE is suspected. TLE favors the face, neck, chest, and back, so special attention should be given to these body regions. Lesions present as edematous, usually annular, plaques with hues ranging from erythematous to violaceous. See images 3, 5, and 6. Epidermal change virtually excludes a diagnosis of TLE (TLE lesions lack atrophy, ulceration, follicular plugging, scarring, or dyspigmentation, and the presence of these features favors a diagnosis of DLE). Although uncommon, TLE may present with a Blaschkoid distribution, periorbital edema, or scalp involvement that appears similar to alopecia areata.
Lesions of TLE persist for days or weeks and chronically recur. Lesions do have the potential to regress spontaneously; however, patients may report recurrence during the summer months.
Evaluation
If the clinical examination is consistent with cutaneous lupus, a lesional biopsy should be taken from an active, erythematous plaque. A punch biopsy (4 mm is recommended on the trunk or 3 mm on cosmetically sensitive areas such as the face) should be performed to include the full thickness of the dermis. As discussed above, the classic histopathologic findings are abundant interstitial mucin and a dermal perivascular and periadnexal lymphocytic infiltrate.[14][15][16]
If the histopathologic findings definitively support a diagnosis of tumid lupus, the patient should be evaluated for systemic disease, despite the weak association with SLE. The evaluation for systemic lupus includes a full history and review of systems, physical examination with special attention to lymphadenopathy or arthritis, and laboratory tests (ANA with anti-dsDNA and anti-Sm profiles), urinalysis, complete blood count (CBC) with differential, chemistries, ESR, CRP, complement levels (C3, C4), and antiphospholipid antibodies. For a more extensive autoimmune workup, autoantibodies such as SS-A/Ro and SS-B/La, anti-U1RNP, and anti-histone antibodies can be drawn.
If the histology is consistent with lupus but not definitive, a lesional biopsy can be sent for direct immunofluorescence (DIF). The most characteristic DIF finding in cutaneous LE is granular IgG and/or IgM deposition at the dermal-epidermal junction and around hair follicles. However, with tumid lupus specifically, DIF is often negative or nonspecific and therefore may not be as valuable as in other forms of cutaneous lupus.
Phototesting can be beneficial for diagnosing TLE; reproduction of lesions after UVA/UVB irradiation may support a diagnosis of tumid lupus.
Treatment / Management
Photoprotection and topical or intralesional corticosteroids are first-line therapy for localized TLE. Application of water-resistant sunscreen with a sun protection factor of 30 or higher, using protective clothing, avoiding peak sun exposure, and smoking cessation are recommended. Corticosteroids are applied topically twice a day for 2-4 weeks. Clinical improvement is usually observed in about 2 weeks. Moderate to high potency corticosteroids are used for treating lesions on the trunk or extremities and low potency corticosteroids are used for the treatment of facial lesions. Cutaneous atrophy, striae, hypopigmentation, and telangiectasias are adverse effects of topical or intralesional corticosteroids. If there is no improvement in 4 weeks, other therapies should be tried. For solitary and thick TLE lesions, intralesional triamcinolone (2.5 to 5 mg/mL) is often effective. 0.1 ml of triamcinolone acetonide can be injected into the lesion at multiple sites 1 cm apart. Intralesional injection can be repeated in 4 weeks. If there is no improvement in 8-12 weeks, intralesional corticosteroids are discontinued. Topical calcineurin inhibitors (e.g., tacrolimus, pimecrolimus) improve the lesions clinically, while decreasing the topical corticosteroid use.[17] Atrophy of the skin is not caused by topical calcineurin inhibitors, making them ideal for maintenance therapy.(B3)
Patients with limited TLE refractory to topical therapy and patients with extensive TLE should be treated with first line antimalarial therapy. Hydroxychloroquine or chloroquine can be used initially. Hydroxychloroquine is usually well tolerated than chloroquine. Between 200 and 400 mg per day of hydroxychloroquine is a reasonable dose. For chloroquine, a dose of 125 to 250 mg per day (for 5 to 7 days per week) is commonly used. Hydroxychloroquine and chloroquine may not be used in combination due to the risk of retinal toxicity. Their risk of retinal toxicity limits the maximal dose of these antimalarials. It is important to note that it may take 8 to 12 weeks to appreciate the effects of antimalarials.[18] Patients should have an eye exam at baseline and then periodically while on the antimalarials. Patients need to be aware of the skin depigmentation that can occur with both hydroxychloroquine and chloroquine. This presents as a blue-gray discoloration on the shins, palate, nails, or face, and this discoloration may be permanent. Gastrointestinal side effects are the most common reason for discontinuation of antimalarial treatment. Neuromuscular and hematological side effects are also noted.(B3)
TLE refractory to antimalarial therapy is rare. However, second-line therapy includes methotrexate (7.5 to 25 mg once weekly) or mycophenolate mofetil (1 to 3 gm per day). Folic acid 1 mg per day typically lessens the severity of the side effects associated with methotrexate. Side effects of methotrexate include gastrointestinal upset, pulmonary fibrosis, bone marrow suppression, alopecia, apart from being teratogenic. Mycophenolate mofetil’s side effects include gastrointestinal upset, reversible cytopenias, immunosuppression, gastrointestinal perforation or ulcer, hypercholesterolemia, and hypertension. Clinical improvement is usually observed with 2-3 months of therapy.
Third-line treatment options, although uncommonly used, include thalidomide and lenalidomide. Thalidomide (50 to 100 mg daily), lenalidomide (5 to 10 mg daily) are used at least for a month for clinical response. Teratogenicity, neuropathy, thromboembolism, sedation are some of the adverse effects associated with the use. Treatment regimens are usually tapered to the lowest potent dose to maintain remission.
Differential Diagnosis
The differential diagnoses of TLE include lymphocytic infiltrate of Jessner, polymorphic light eruption, pseudolymphoma of the skin, reticular erythematous mucinosis, and granuloma faciale. Jessner's lymphocytic infiltrate presents very similarly to tumid lupus with erythematous papular or nodular lesions without scale, on the upper back or the face. Histopathology also shows dermal mucin deposition.[19] Direct immunofluorescence and antinuclear antibodies may be positive.[20]
Polymorphic light eruption (PMLE) presents as skin-colored or erythematous plaques or papules that are pruritic in the sun-exposed areas of the body. Lesions typically occur within hours of photo exposure and resolve soon than tumid lupus lesions. With progressive exposure to UV light, PMLE lesions do not get worse(hardening effect), which differentiates them from TLE.[21]
Reticular erythematous mucinosis presents as erythematous, reticular macules, or plaques, usually on the upper back and chest. Dermal mucin deposition is more superficial. Lymphocytes are more dispersed and superficial.[22] Complement and immunoglobulin deposition along the dermo-epidermal junction is not commonly seen.
Pseudolymphoma of the skin presents as erythematous nodules in the dermis, usually on the chest, arms, and face. Lesions are not photosensitive. Histopathology differentiates it from TLE, due to the presence of histiocytes and plasma cells along with lymphocytes.[23]
Granuloma faciale presents as a violaceous nodule or plaque on the face. Lesions are usually asymptomatic. Grenz zone is the characteristic histologic finding that distinguishes it from TLE. A thin zone of the uninvolved papillary dermis that divides the dermal inflammatory infiltrate (lymphocytes, histiocytes, plasma cells, neutrophils, and eosinophils) from the epidermis is called the Grenz zone.[24]
Prognosis
Tumid Lupus Erythematosus has a benign course.[25] Solitary lesions are mostly self-limiting, often without any need for topical or systemic therapy. However, recurrence is noted to be high with the disease-free period in between. Long-term remission is observed in some patients.[11] TLE lesions have a favorable prognosis than lesions of discoid lupus erythematosus or subacute cutaneous lupus erythematosus.[11] Spontaneous resolution of the lesions without residual dyspigmentation or scarring may be noted within days or weeks, despite the relapses.[26][27] Photoprotection alone was effective for lesion resolution in more than 50% of patients without any symptoms.[10]
Complications
Association with Systemic Lupus Erythematosus or discoid lupus erythematosus is rare.[25][28][29] Patients might be prone to vitamin D deficiency by avoiding sun exposure. Hence evaluation of the vitamin D deficiency with 25-hydroxyvitamin D level and adequate supplementation with at least 400 IU of cholecalciferol is suggested.[30][31]
Deterrence and Patient Education
Protection from sunlight with protective clothing, reducing overall sun exposure and avoidance of tanning, outdoor jobs, sunbathing, travel toward equatorial regions are strongly recommended.[32][33] Patients are advised to apply sunscreen of 2 mg cm , twenty to thirty minutes before the exposure, with a sun protection factor of at least 50, that has protection against both UVA and UVB light.[25][34] Smoking cessation is emphasized given the reported clinical improvement in the affected area and severity index score of TLE with antimalarial therapy.[35] In people with refractory disease, minimizing the use of photosensitizing medications is suggested.[25] Education on eliminating the offending drug can resolve drug-induced TLE.[36] Patients should be made aware of lesions appearing up to three weeks after photo exposure.[37] Manipulation of TLE lesions should be avoided due to the risk of the Koebner phenomenon.[36]
Enhancing Healthcare Team Outcomes
SLE is a systemic disorder managed by an interprofessional team. The disorder has no cure and is chronic and progressive. Another subtype of chronic LE is TLE. Although tumid lupus erythematosus (TLE) is currently considered to be a subtype of cutaneous lupus erythematosus (CLE), TLE differs from the other subtypes of cutaneous lupus erythematosus in that an association with systemic lupus erythematosus (SLE) is rare. Because of this weak association with SLE and a relative lack of serologic abnormalities in patients with TLE, some consider TLE to be an entity separate from lupus. The disorder is best managed by a dermatologist and/or rheumatologist, but the patient can be followed by the primary care provider and nurse practitioner with the assistance of a specialty trained dermatology nurse. The nurse should assist with the coordination of follow-up, patient and family education, and monitoring for untoward changes and reporting concerns to the team. A pharmacist should assist in the management of the medications required for treatment. Evaluating potential drug-drug interactions, providing patient education, and reporting to the team if any problematic events develop regarding the pharmaceutical therapy. By working as an interprofessional team, the best outcomes can be achieved.
Tumid lupus erythematosus (TLE) typically presents as annular, indurated, erythematous, edematous plaques without epidermal involvement. If any of these features are recognized, and epidermal involvement is likely, a diagnosis of DLE should be suspected. Typical locations of TLE are the face and trunk, and lesions respond well to photoprotection, topical corticosteroids, and antimalarials.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Sontheimer RD. The lexicon of cutaneous lupus erythematosus--a review and personal perspective on the nomenclature and classification of the cutaneous manifestations of lupus erythematosus. Lupus. 1997:6(2):84-95 [PubMed PMID: 9061656]
Level 3 (low-level) evidenceConcha JSS, Werth VP. Alopecias in lupus erythematosus. Lupus science & medicine. 2018:5(1):e000291. doi: 10.1136/lupus-2018-000291. Epub 2018 Oct 25 [PubMed PMID: 30397497]
Abadías-Granado I, Sánchez-Bernal J, Felipo-Berlanga F, Ara-Martín M. Coexistence of Tumid Lupus Erythematosus and Discoid Lupus Erythematosus. Actas dermo-sifiliograficas. 2019 Apr:110(3):253-255. doi: 10.1016/j.ad.2018.02.023. Epub 2018 Jul 30 [PubMed PMID: 30072022]
Powell R,Hile G,Lowe L,Kahlenberg JM, Herpes zoster infection after topical steroid use in the setting of tumid lupus erythematosus. JAAD case reports. 2018 Jan; [PubMed PMID: 29379863]
Level 3 (low-level) evidenceJefferson GD, Aakalu VK, Braniecki M. Tumid lupus: An unexpected diagnosis for the otolaryngologist. American journal of otolaryngology. 2017 Mar-Apr:38(2):257-259. doi: 10.1016/j.amjoto.2017.01.003. Epub 2017 Jan 17 [PubMed PMID: 28122678]
Fogagnolo L, Soares TC, Senna CG, Souza EM, Blotta MH, Cintra ML. Cytotoxic granules in distinct subsets of cutaneous lupus erythematosus. Clinical and experimental dermatology. 2014 Oct:39(7):835-9. doi: 10.1111/ced.12428. Epub [PubMed PMID: 25214407]
Level 2 (mid-level) evidenceGambichler T, Pätzholz J, Schmitz L, Lahner N, Kreuter A. FOXP3+ and CD39+ regulatory T cells in subtypes of cutaneous lupus erythematosus. Journal of the European Academy of Dermatology and Venereology : JEADV. 2015 Oct:29(10):1972-7. doi: 10.1111/jdv.13123. Epub 2015 Mar 25 [PubMed PMID: 25808110]
Böckle BC, Sepp NT. Smoking is highly associated with discoid lupus erythematosus and lupus erythematosus tumidus: analysis of 405 patients. Lupus. 2015 Jun:24(7):669-74. doi: 10.1177/0961203314559630. Epub 2014 Nov 19 [PubMed PMID: 25411260]
Level 2 (mid-level) evidenceSchneider SW, Staender S, Schlüter B, Luger TA, Bonsmann G. Infliximab-induced lupus erythematosus tumidus in a patient with rheumatoid arthritis. Archives of dermatology. 2006 Jan:142(1):115-6 [PubMed PMID: 16415403]
Level 3 (low-level) evidenceVieira V, Del Pozo J, Yebra-Pimentel MT, Martínez W, Fonseca E. Lupus erythematosus tumidus: a series of 26 cases. International journal of dermatology. 2006 May:45(5):512-7 [PubMed PMID: 16700782]
Level 2 (mid-level) evidenceSchmitt V, Meuth AM, Amler S, Kuehn E, Haust M, Messer G, Bekou V, Sauerland C, Metze D, Köpcke W, Bonsmann G, Kuhn A. Lupus erythematosus tumidus is a separate subtype of cutaneous lupus erythematosus. The British journal of dermatology. 2010 Jan:162(1):64-73. doi: 10.1111/j.1365-2133.2009.09401.x. Epub 2009 Jul 7 [PubMed PMID: 19712116]
Yu C, Chang C, Zhang J. Immunologic and genetic considerations of cutaneous lupus erythematosus: a comprehensive review. Journal of autoimmunity. 2013 Mar:41():34-45. doi: 10.1016/j.jaut.2013.01.007. Epub 2013 Feb 1 [PubMed PMID: 23380467]
Braddock SW, Kay HD, Maennle D, McDonald TL, Pirruccello SJ, Masih A, Klassen LW, Sawka AR. Clinical and immunologic studies in reticular erythematous mucinosis and Jessner's lymphocytic infiltrate of skin. Journal of the American Academy of Dermatology. 1993 May:28(5 Pt 1):691-5 [PubMed PMID: 8496412]
Level 3 (low-level) evidenceVerma P, Sharma S, Yadav P, Namdeo C, Mahajan G. Tumid lupus erythematosus: an intriguing dermatopathological connotation treated successfully with topical tacrolimus and hydroxyxhloroquine combination. Indian journal of dermatology. 2014 Mar:59(2):210. doi: 10.4103/0019-5154.127716. Epub [PubMed PMID: 24700961]
Bajaj DR, Devrajani BR, Matlani BL. Discoid lupus erythematosus: a profile. Journal of the College of Physicians and Surgeons--Pakistan : JCPSP. 2010 Jun:20(6):361-4 [PubMed PMID: 20642962]
Goerig R, Vogeler C, Keller M. Atypical presentation of cutaneous lupus mucinosis. The Journal of clinical and aesthetic dermatology. 2013 Apr:6(4):37-40 [PubMed PMID: 23630641]
Abdullah L, Abbas O. Dermacase: Can you identify this condition? Tumid lupus erythematosus. Canadian family physician Medecin de famille canadien. 2012 Jul:58(7):765, 769 [PubMed PMID: 22798463]
Level 3 (low-level) evidenceChang J, Werth VP. Therapeutic options for cutaneous lupus erythematosus: recent advances and future prospects. Expert review of clinical immunology. 2016 Oct:12(10):1109-21. doi: 10.1080/1744666X.2016.1188006. Epub 2016 Jun 1 [PubMed PMID: 27249209]
Level 3 (low-level) evidenceRémy-Leroux V, Léonard F, Lambert D, Wechsler J, Cribier B, Thomas P, Adamski H, Marguery MC, Aubin F, Leroy D, Bernard P. Comparison of histopathologic-clinical characteristics of Jessner's lymphocytic infiltration of the skin and lupus erythematosus tumidus: Multicenter study of 46 cases. Journal of the American Academy of Dermatology. 2008 Feb:58(2):217-23 [PubMed PMID: 18083273]
Level 2 (mid-level) evidenceLipsker D, Mitschler A, Grosshans E, Cribier B. Could Jessner's lymphocytic infiltrate of the skin be a dermal variant of lupus erythematosus? An analysis of 210 cases. Dermatology (Basel, Switzerland). 2006:213(1):15-22 [PubMed PMID: 16778421]
Level 2 (mid-level) evidenceTutrone WD, Spann CT, Scheinfeld N, Deleo VA. Polymorphic light eruption. Dermatologic therapy. 2003:16(1):28-39 [PubMed PMID: 12919124]
Cinotti E, Merlo V, Kempf W, Carli C, Kanitakis J, Parodi A, Rongioletti F. Reticular erythematous mucinosis: histopathological and immunohistochemical features of 25 patients compared with 25 cases of lupus erythematosus tumidus. Journal of the European Academy of Dermatology and Venereology : JEADV. 2015 Apr:29(4):689-97. doi: 10.1111/jdv.12654. Epub 2014 Aug 4 [PubMed PMID: 25087914]
Level 3 (low-level) evidenceCetinözman F, Jansen PM, Willemze R. Expression of programmed death-1 in primary cutaneous CD4-positive small/medium-sized pleomorphic T-cell lymphoma, cutaneous pseudo-T-cell lymphoma, and other types of cutaneous T-cell lymphoma. The American journal of surgical pathology. 2012 Jan:36(1):109-16. doi: 10.1097/PAS.0b013e318230df87. Epub [PubMed PMID: 21989349]
Abbas O, Mahalingam M. The grenz zone. The American Journal of dermatopathology. 2013 Feb:35(1):83-91. doi: 10.1097/DAD.0b013e31824feb4e. Epub [PubMed PMID: 23348142]
Patsinakidis N, Kautz O, Gibbs BF, Raap U. Lupus erythematosus tumidus: clinical perspectives. Clinical, cosmetic and investigational dermatology. 2019:12():707-719. doi: 10.2147/CCID.S166723. Epub 2019 Oct 1 [PubMed PMID: 31632119]
Level 3 (low-level) evidenceKuhn A, Bein D, Bonsmann G. The 100th anniversary of lupus erythematosus tumidus. Autoimmunity reviews. 2009 May:8(6):441-8. doi: 10.1016/j.autrev.2008.12.010. Epub 2009 Jan 20 [PubMed PMID: 19162244]
Choonhakarn C, Poonsriaram A, Chaivoramukul J. Lupus erythematosus tumidus. International journal of dermatology. 2004 Nov:43(11):815-8 [PubMed PMID: 15533063]
Level 2 (mid-level) evidenceKuhn A, Richter-Hintz D, Oslislo C, Ruzicka T, Megahed M, Lehmann P. Lupus erythematosus tumidus--a neglected subset of cutaneous Lupus erythematosus: report of 40 cases. Archives of dermatology. 2000 Aug:136(8):1033-41 [PubMed PMID: 10926740]
Level 3 (low-level) evidenceStead J, Headley C, Ioffreda M, Kovarik C, Werth V. Coexistence of tumid lupus erythematosus with systemic lupus erythematosus and discoid lupus erythematosus: a report of two cases of tumid lupus. Journal of clinical rheumatology : practical reports on rheumatic & musculoskeletal diseases. 2008 Dec:14(6):338-41. doi: 10.1097/RHU.0b013e31817d1183. Epub [PubMed PMID: 18664992]
Level 3 (low-level) evidenceKuhn A, Aberer E, Bata-Csörgő Z, Caproni M, Dreher A, Frances C, Gläser R, Klötgen HW, Landmann A, Marinovic B, Nyberg F, Olteanu R, Ranki A, Szepietowski JC, Volc-Platzer B. S2k guideline for treatment of cutaneous lupus erythematosus - guided by the European Dermatology Forum (EDF) in cooperation with the European Academy of Dermatology and Venereology (EADV). Journal of the European Academy of Dermatology and Venereology : JEADV. 2017 Mar:31(3):389-404. doi: 10.1111/jdv.14053. Epub 2016 Dec 20 [PubMed PMID: 27859683]
Kuhn A, Ruland V, Bonsmann G. Cutaneous lupus erythematosus: update of therapeutic options part I. Journal of the American Academy of Dermatology. 2011 Dec:65(6):e179-93. doi: 10.1016/j.jaad.2010.06.018. Epub 2010 Aug 23 [PubMed PMID: 20739095]
Sanders CJ, Van Weelden H, Kazzaz GA, Sigurdsson V, Toonstra J, Bruijnzeel-Koomen CA. Photosensitivity in patients with lupus erythematosus: a clinical and photobiological study of 100 patients using a prolonged phototest protocol. The British journal of dermatology. 2003 Jul:149(1):131-7 [PubMed PMID: 12890206]
Level 2 (mid-level) evidenceSamotij D, Szczęch J, Werth VP, Furukawa F, Kuhn A, Szepietowski JC, Reich A. Disease severity and prophylactic measures in patients with cutaneous lupus erythematosus: results of a worldwide questionnaire-based study. Postepy dermatologii i alergologii. 2018 Apr:35(2):192-198. doi: 10.5114/ada.2018.75242. Epub 2018 Apr 24 [PubMed PMID: 29760621]
Kuhn A, Gensch K, Haust M, Meuth AM, Boyer F, Dupuy P, Lehmann P, Metze D, Ruzicka T. Photoprotective effects of a broad-spectrum sunscreen in ultraviolet-induced cutaneous lupus erythematosus: a randomized, vehicle-controlled, double-blind study. Journal of the American Academy of Dermatology. 2011 Jan:64(1):37-48. doi: 10.1016/j.jaad.2009.12.053. Epub [PubMed PMID: 21167404]
Level 1 (high-level) evidenceKreuter A, Gaifullina R, Tigges C, Kirschke J, Altmeyer P, Gambichler T. Lupus erythematosus tumidus: response to antimalarial treatment in 36 patients with emphasis on smoking. Archives of dermatology. 2009 Mar:145(3):244-8. doi: 10.1001/archdermatol.2008.592. Epub [PubMed PMID: 19289751]
Okon LG, Werth VP. Cutaneous lupus erythematosus: diagnosis and treatment. Best practice & research. Clinical rheumatology. 2013 Jun:27(3):391-404. doi: 10.1016/j.berh.2013.07.008. Epub [PubMed PMID: 24238695]
Kuhn A, Ruland V, Bonsmann G. Photosensitivity, phototesting, and photoprotection in cutaneous lupus erythematosus. Lupus. 2010 Aug:19(9):1036-46. doi: 10.1177/0961203310370344. Epub [PubMed PMID: 20693197]