Introduction
In optics, incident rays are either refracted or reflected off a surface at an angle constant to the degree of refractivity or reflectivity of the given medium. The eye is essentially an optical focusing system for the refraction of light stimuli onto a complex network of neurons and specialized photoreceptors. This complex system delivers sensory information to the visual cortex for interpretation. These neural impulses are translated from the retina via cone photoreceptors populating the fovea centralis, which depolarize upon exposure to photopic stimuli.[1]
The cones also account for central 10° of peak visual field sensitivity and color sensitivity. The optical function of the eye is directly proportional to its gross focusing power.
The human eye chiefly possesses two convex refractive components, including:
The total refractive power of the human eye is estimated to be about +60 diopters (D).[3] Based on the Gullstrand schematic eye, the dioptric power of the cornea ranges from +43D to +48D. Both the cornea's anterior and posterior surfaces possess refractive properties. The precorneal tear film or air-tear film interface accounts for the refractivity of the anterior cornea.[4][5]
The corneal dioptric powers vary between individuals depending upon the difference between the radii of curvature of anterior corneal and back vertex surfaces.[6][7] Under normal circumstances, corneal curvature is steepest around its apex, about 3 millimeters centrally. Incident paraxial rays of light travel via the corneal apex onto refractive components along the visual axis, including both the anterior and posterior surfaces of the crystalline lens.[8] The power of the crystalline lens varies with density, transparency, and the effect of accommodation.[9]
All visual stimuli consist of photons of light. Visible light exists between wavelengths ranging from 400 nanometers (nm) to about 700 nm of the electromagnetic spectrum. When we view objects, our eyes are exposed to these particles of light (photons), which travel through the visual system as paraxial/parallel 'strings' or rays. The cornea and crystalline lens are essentially two powerful convex (converging) lenses that function to bring incident rays of light to a focal point at the fovea centralis. Due to variations in the power of convergence between central and paracentral corneal and lenticular surfaces, paraxial rays of light may yield differences in the depth of focus. This phenomenon is called spherical aberration and occurs mostly under dim illumination.[10]
Several defects in clarity and regularity of the cornea and lens also result in light scattering phenomena and other forms of induced aberrations. Other examples include chromatic aberrations and higher-order aberrations.[11][12][13]
An interaction of axial length (AL), corneal power (K), and power of the anatomic crystalline lens account for the ocular refractive state.[2] The vitreous humor possesses a lower refractive index than the crystalline lens. The role of the vitreous in refraction tends to be minimal under normal conditions. Optimal vitreous clarity and optical transparency propagate light transmission to the sensory retina. Physiological changes in the homogeneity of the posterior media do not impact the eye's refracting power. These alterations, however, can alter the refractivity of vitreous media and bring about a light-scattering phenomenon.[14]
Morphologically, the eye's total convergent power varies from person to person. This depends upon the interaction of the abovementioned factors (AL, K, and lens power).[2] Optical defocus can result when light rays are not focused at the fovea. Such variations in the focal point of images are termed 'errors of refraction' or ametropias. Besides innate conditions, refractive errors also develop due to degenerative or transient anatomical and physiological changes secondary to disease states. Uncomplicated refractive errors can be corrected optimally via spectacle lenses, prescription contact lenses, or refractive surgery. Uncorrected refractive errors rank among the leading causes of avoidable visual impairment.[15]
Refractive errors are classified as:
- Hyperopia
- Myopia
- Astigmatism
In the absence of refractive errors, the eye's refractive state is classified as emmetropic. The developmental process via which the human eye tends towards emmetropia is termed emmetropization. Emmetropization takes place between early childhood and teenage years. Endogenous factors which influence emmetropization include alterations in lens thickness and axial length extension. Multiple hypothesized innate or environmental stimuli which interfere with the process of emmetropization bring about ametropia.
Hyperopia
A hyperopic eye under-converges incident rays of light while being devoid of the effect of accommodation. The point of focus thus falls beyond the retinal plane. The resultant blur is termed hyperopic defocus. The hyperopic or far-sighted optical system possesses either lesser gross dioptric power or a shorter axial length. The dioptric equivalent of a convex lens is expressed as a plus (+) numerical factor.[16]
Myopia
A myopic eye over-converges incident rays, thus causing the focal point to fall in front of the fovea. This mainly occurs due to greater crystalline lens thickness (correlating to higher lens dioptric power) and longer than average axial length with normal optics.[17] The dioptric equivalent of a concave lens is expressed in a minus (-) unit.[18]
Hyperopia and myopia make up spherical ametropias. They are corrected using spherical lenses. A spherical lens possesses even thickness circumferentially and has the same power at different angles when positioned in the trial frames. Concave (minus) lenses are thinner at the center and thicker near their edges, which provides greater image divergence. Convex (or plus) lenses are thickest around the optical center and thinner peripherally. This enables greater image convergence for hyperopic correction.
Astigmatism
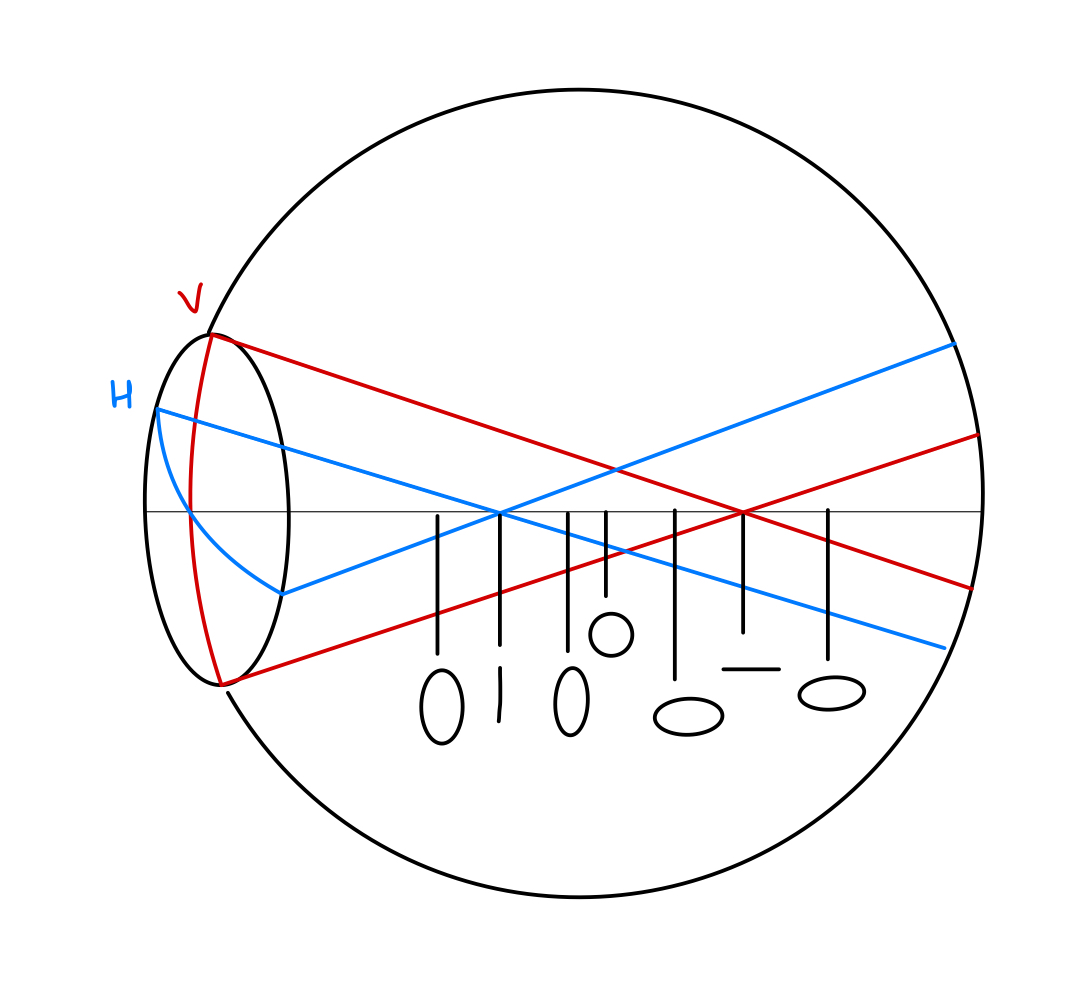
For an astigmatic eye, incident light rays do not converge onto a focal point. Instead, they are refracted to several foci. Astigmatic errors can be either simple, compound, or mixed in nature. If one focal point is incident at the fovea while the other point converges anteriorly to the foveal plane, it is termed simple myopic astigmatism (See image). With simple hyperopic astigmatism, one point is focused on the fovea, and the other lies behind the retina (see image).[19]
When both focal points are incident anterior to the fovea, it is termed compound myopic astigmatism. In instances where the principal foci of both meridians are incident beyond the retinal plane, this condition is termed a compound hyperopic astigmatism. For the scenario of mixed astigmatism, one focus point is incident in front of the retina, while the other focuses beyond the retinal plane (See image).
A schematic representation of astigmatism can be best described by the 'conoid of Sturm' (See image). In this model, incident rays on a curved surface refract along two orthogonal meridians (with different curvatures) until they converge on separate focal points.[20] The refractive surface forms a cone base while the focal point becomes the apex, yielding a conoid plane diagram.
Manifest astigmatic errors are mostly representative of corneal astigmatism. In with-the-rule astigmatism, the meridian of highest corneal power (the power meridian) lies along 90 degrees, which places the axis of correction along 180°. While with against-the-rule astigmatism (See image), the power meridian lies along 180 degrees, thus placing the axis of cylindrical correction along 90 degrees.
Astigmatic errors are corrected with the use of sphero-cylindrical spectacle lenses or toric contact lenses. The term 'toric' indicates varying degrees of curvature along the meridians of a curved surface. Before spectacle dispensing, the power and axis of a cylinder are refined during subjective refraction. The cylindrical axis must be localized with 15 degrees for moderate errors and within 3 degrees to 5 degrees for high errors.
For conditions that can cause variability or unspecificity of cylindrical (chiefly axis) refinement or in patients that do not tolerate toric corrections, spherical equivalent prescriptions can provide an adequate alternative when dispensing corrective lenses. The spherical equivalent typifies the optical (spherical) prescription, which places the astigmatic eye in a refractive state of meridional balance within the circle of least confusion (See image).
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
The spherical equivalent prescription aids in the determination of refractive correction needs (especially high absolute spherical components on refractive findings) among both non-verbal and verbal pre-schooling young children without manifest ocular deviations.[21]
Spherical equivalent determination can assist the subjective refraction procedure in instances when patient-doctor interaction is inhibited by very steep or non-negotiable communication barriers. Spherical equivalents are effectively employed for individuals who fail to adapt to the best minimal sphero-cylindrical spectacle correction. It can be utilized for the correction of aphakic errors, particularly those with low amounts of corneal astigmatism manifest via keratometry.[22]
Other cases for which spherical equivalents are recommended include:
- For ordering a soft contact lens prescription for patients with very low or no manifest subjective astigmatism, especially mild with-the-rule astigmatism.[23]
- Patients implanted with toric intraocular lenses[24][25]
- Patients triaged for prismatic correction via the Prentice rule[26]
- Refractive conditions secondary to ocular developmental anomalies such as high hyperopia in nanophthalmic eyes and high axial myopia due to buphthalmos.[27][28]
- Pseudo-astigmatic errors due to tear film anomalies, use of corneal indentation/applanation devices, and patients with regular astigmatic errors preceding pterygium excision.[29]
- Employed for the correction of sphero-cylindrical errors among patients with atypical/anomalous head posture (e.g., torticollis) or certain forms of compensatory head tilt (such as marked chin-up posture among individuals with globe elevation deficits).[30] Off-axis postural prototypes can result in inadvertent alteration of the axis meridian on sphero-cylindrical spectacle correction.
- Temporary correction of spherical defocus (in the form of myopic or hyperopic shift) is secondary to the effects of either cholinergic or adrenergic agents and sulfonamide pharmacologics.[31][32]
- Transient refractive changes attributable to physiological and pathophysiophysologic changes such as hyperglycemia, pregnancy, nuclear cataract formation, ciliary muscle spasm, ciliary rotation, variable retinal edema, etc.[33]
- Longitudinal changes in the cycloplegic spherical equivalent refractive error are employed in monitoring myopia progression (along with changes in the axial length measurement) in juvenile-onset myopia.[34][35]
- For quantitative determination of the outcomes of myopia control therapies.[36]
Contraindications
Prescribing spherical equivalents is contraindicated for the following classes of individuals:
- Young children with moderate to high astigmatic errors, which have been proven to pose a great risk of amblyogenesis[21]
- In cases of accommodative anomalies, especially accommodative infacility and accommodative excess, neglecting manifest astigmatism. The recommendation of equivalent spherical correction would only fail to account for innate accommodative impulses like blur and diplopia.[37]
- Conditions that precipitate visual impairment via irregular astigmatism require consideration of their cylindrical errors for rigid contact lens fitting. This includes individuals with clinically evident corneal ectasia, as well as subclinical cases that are only observed via keratometry or keratography.[38]
- Cases of refractable (early-to-moderate) pathological myopia also require a full sphero-cylindrical prescription.
- Refractive correction in the presence of co-existent moderate or large angle ocular deviations (chiefly strabismus).
- Correction of refractive error prior to ptosis surgery.[39]
- Individuals fitting the low vision criteria that gain better LogMAR visual acuity with full sphero-cylindrical correction.[40]
- Spherical equivalent prescriptions are also contraindicated for correcting moderate to high oblique astigmatic errors, even amongst adults.
Technique or Treatment
The spherical equivalent (SE) can be determined via the following formulae: Optimal subjective spherical component (S) plus half of [the subjective cylindrical component (C)]
Algebraically, the formula is:
- SE = S + C/2
Example: A complete refraction shows right eye (RE): +2.50 DS - 0.50 DC x 90, and left eye (LE): +1.50 DS +1.00 DC x 90.
The spherical equivalent is calculated as SE(RE)=+2.50 + (-0.50/2)=+2.25 DS; and SE(LE)=+1.50 + (+1.00/2)=+2.00 DS
Clinical Significance
The spherical equivalent method is used when the optometrist and ophthalmologist deal with patients that probably cannot tolerate lenses with a cylindric lens correction. Spherical corrected lenses may not provide the best corrected visual acuity. However, they can provide enhanced vision without problems related to toric lenses. The clinician needs to decide when to use this method for prescribing lenses based on the special needs of each individual patient and consider pertinent indications and contraindications on a case-to-case basis.
Enhancing Healthcare Team Outcomes
When patients are referred for spherical equivalent correction, clinicians must be on the lookout for signs suggesting underlying disease. In such cases, patients gain more quality care from a multifaceted assessment. The timely adoption of an interprofessional approach is critical for these individuals. People with diabetes with poor glucose control regimens, for example, may be first seen by the optometrist or ophthalmologist with complaints of transient blurry vision. These individuals may require multiple changes to spectacle prescription without timely referral to endocrinology for the underlying metabolic disorder.
For patients who may have logged multiple visits to the eye clinic before presenting with similar complaints, the spherical equivalent also enables delineating acute changes in the ocular refractive state. The clinician must have a thorough approach when assessing refractive errors, considering that several pathologic conditions may masquerade as changes in refractive defects.[Level 3] Moreover, the optometrist and ophthalmologist must select which patients are not suited for toric correction and can benefit from spherical equivalent lens prescriptions.
Media
(Click Image to Enlarge)
References
Bonelli R, Woods SM, Lockwood S, Bishop PN, Khan KN, Bahlo M, Ansell BRE, Fruttiger M. Spatial distribution of metabolites in the retina and its relevance to studies of metabolic retinal disorders. Metabolomics : Official journal of the Metabolomic Society. 2023 Feb 6:19(2):10. doi: 10.1007/s11306-022-01969-6. Epub 2023 Feb 6 [PubMed PMID: 36745234]
Mutti DO, Mitchell GL, Jones LA, Friedman NE, Frane SL, Lin WK, Moeschberger ML, Zadnik K. Axial growth and changes in lenticular and corneal power during emmetropization in infants. Investigative ophthalmology & visual science. 2005 Sep:46(9):3074-80 [PubMed PMID: 16123404]
Vojniković B, Tamajo E. Gullstrand's optical schematic system of the eye--modified by Vojniković & Tamajo. Collegium antropologicum. 2013 Apr:37 Suppl 1():41-5 [PubMed PMID: 23841130]
Koh S, Tung CI, Inoue Y, Jhanji V. Effects of tear film dynamics on quality of vision. The British journal of ophthalmology. 2018 Dec:102(12):1615-1620. doi: 10.1136/bjophthalmol-2018-312333. Epub 2018 Jun 15 [PubMed PMID: 29907632]
Level 2 (mid-level) evidenceAtchison DA, Thibos LN. Optical models of the human eye. Clinical & experimental optometry. 2016 Mar:99(2):99-106. doi: 10.1111/cxo.12352. Epub 2016 Mar 10 [PubMed PMID: 26969304]
Lu LW, Rocha-de-Lossada C, Rachwani-Anil R, Flikier S, Flikier D. The role of posterior corneal power in 21st century biometry: A review. Journal francais d'ophtalmologie. 2021 Sep:44(7):1052-1058. doi: 10.1016/j.jfo.2020.11.031. Epub 2021 Jun 17 [PubMed PMID: 34148699]
Hasegawa A, Kojima T, Yamamoto M, Kato Y, Tamaoki A, Ichikawa K. Impact of the anterior-posterior corneal radius ratio on intraocular lens power calculation errors. Clinical ophthalmology (Auckland, N.Z.). 2018:12():1549-1558. doi: 10.2147/OPTH.S161464. Epub 2018 Aug 27 [PubMed PMID: 30214138]
Jonas JB, Ohno-Matsui K, Panda-Jonas S. Myopia: Anatomic Changes and Consequences for Its Etiology. Asia-Pacific journal of ophthalmology (Philadelphia, Pa.). 2019 Sep-Oct:8(5):355-359. doi: 10.1097/01.APO.0000578944.25956.8b. Epub [PubMed PMID: 31425168]
Manns F, Ho A. Paraxial equivalent of the gradient-index lens of the human eye. Biomedical optics express. 2022 Oct 1:13(10):5131-5150. doi: 10.1364/BOE.464121. Epub 2022 Sep 6 [PubMed PMID: 36425626]
Artal P, Schwarz C, Cánovas C, Mira-Agudelo A. Night myopia studied with an adaptive optics visual analyzer. PloS one. 2012:7(7):e40239. doi: 10.1371/journal.pone.0040239. Epub 2012 Jul 2 [PubMed PMID: 22768343]
Piñero DP, Ortiz D, Alio JL. Ocular scattering. Optometry and vision science : official publication of the American Academy of Optometry. 2010 Sep:87(9):E682-96. doi: 10.1097/OPX.0b013e3181e87da6. Epub [PubMed PMID: 20601914]
Hughes RP, Vincent SJ, Read SA, Collins MJ. Higher order aberrations, refractive error development and myopia control: a review. Clinical & experimental optometry. 2020 Jan:103(1):68-85. doi: 10.1111/cxo.12960. Epub 2019 Sep 6 [PubMed PMID: 31489693]
Harris WF, Evans T. Chromatic aberration in heterocentric astigmatic systems including the eye. Optometry and vision science : official publication of the American Academy of Optometry. 2012 Nov:89(11):e37-43 [PubMed PMID: 23096492]
Kokavec J, Wu Z, Sherwin JC, Ang AJ, Ang GS. Nd:YAG laser vitreolysis versus pars plana vitrectomy for vitreous floaters. The Cochrane database of systematic reviews. 2017 Jun 1:6(6):CD011676. doi: 10.1002/14651858.CD011676.pub2. Epub 2017 Jun 1 [PubMed PMID: 28570745]
Level 1 (high-level) evidenceGBD 2019 Blindness and Vision Impairment Collaborators, Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. The Lancet. Global health. 2021 Feb:9(2):e144-e160. doi: 10.1016/S2214-109X(20)30489-7. Epub 2020 Dec 1 [PubMed PMID: 33275949]
Majumdar S, Tripathy K. Hyperopia. StatPearls. 2023 Jan:(): [PubMed PMID: 32809551]
Dogan M, Elgin U, Sen E, Tekin K, Yilmazbas P. Comparison of anterior segment parameters and axial lengths of myopic, emmetropic, and hyperopic children. International ophthalmology. 2019 Feb:39(2):335-340. doi: 10.1007/s10792-017-0816-8. Epub 2017 Dec 29 [PubMed PMID: 29285706]
Saluja G, Kaur K. Childhood Myopia And Ocular Development. StatPearls. 2023 Jan:(): [PubMed PMID: 36508524]
Gurnani B, Kaur K. Astigmatism. StatPearls. 2023 Jan:(): [PubMed PMID: 35881747]
Parthasarathi P, Stokkermans TJ. The Conoid of Sturm. StatPearls. 2023 Jan:(): [PubMed PMID: 36508529]
Leat SJ. To prescribe or not to prescribe? Guidelines for spectacle prescribing in infants and children. Clinical & experimental optometry. 2011 Nov:94(6):514-27. doi: 10.1111/j.1444-0938.2011.00600.x. Epub 2011 Jul 3 [PubMed PMID: 21722183]
Tian L, Zhao P, Zhu H, Kang X, Wei Y, Chen L, Li J. Vergence Formula for Estimating the Refractive Status of Aphakic Eyes in Pediatric Patients. Frontiers in medicine. 2022:9():861745. doi: 10.3389/fmed.2022.861745. Epub 2022 Apr 8 [PubMed PMID: 35463009]
Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye & contact lens. 2011 Jan:37(1):20-5. doi: 10.1097/ICL.0b013e3182048fb9. Epub [PubMed PMID: 21178696]
Song XD, Hao YS, Bao YZ, Li ZH, Zhang H, Yu AY, Zhao MS, Huang YS, Fang J, Liu Y, Sun YX, Wang NL. [Safety and efficacy of toric intraocular lens implantation for more than 5 years]. [Zhonghua yan ke za zhi] Chinese journal of ophthalmology. 2023 Feb 11:59(2):118-128. doi: 10.3760/cma.j.cn112142-20220826-00417. Epub [PubMed PMID: 36740441]
Goggin M. Toric intraocular lenses: Evidence-based use. Clinical & experimental ophthalmology. 2022 Jul:50(5):481-489. doi: 10.1111/ceo.14106. Epub 2022 May 29 [PubMed PMID: 35584257]
Radhakrishnan H, Charman WN. Optical characteristics of Alvarez variable-power spectacles. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2017 May:37(3):284-296. doi: 10.1111/opo.12361. Epub 2017 Feb 17 [PubMed PMID: 28211160]
Sasaki K, Sasaki K, Hirota M, Hayashi T, Mizota A. Comparisons of size of foveal avascular zone area among children with posterior microphthalmos, high hyperopia, and normal eyes. International ophthalmology. 2022 Aug:42(8):2599-2607. doi: 10.1007/s10792-022-02250-4. Epub 2022 Apr 2 [PubMed PMID: 35366136]
Jonas JB, Holbach L, Panda-Jonas S. Histologic differences between primary high myopia and secondary high myopia due to congenital glaucoma. Acta ophthalmologica. 2016 Mar:94(2):147-53. doi: 10.1111/aos.12937. Epub 2015 Dec 23 [PubMed PMID: 26695106]
Jain AK, Pandey DJ. Evaluation of change in pterygium induced keratometric astigmatism in patients following pterygium excision with autologous graft surgery. Nepalese journal of ophthalmology : a biannual peer-reviewed academic journal of the Nepal Ophthalmic Society : NEPJOPH. 2020 Jul:12(24):191-200. doi: 10.3126/nepjoph.v12i2.28287. Epub [PubMed PMID: 33978613]
Yang C, Huang W, Cui Y, Zhang G, Wang D, Xie W, Wiederhold M, Wiederhold B, Chu H, Yan L, Zeng J. Binocular integration and stereopsis in children with television torticollis. BMC ophthalmology. 2021 Feb 24:21(1):102. doi: 10.1186/s12886-021-01850-5. Epub 2021 Feb 24 [PubMed PMID: 33627106]
Montés-Micó R, Charman WN. Pharmacological Strategies for Presbyopia Correction. Journal of refractive surgery (Thorofare, N.J. : 1995). 2019 Dec 1:35(12):803-814. doi: 10.3928/1081597X-20191010-04. Epub [PubMed PMID: 31830297]
Park YM, Lee TE. Isotretinoin-induced Angle Closure and Myopic Shift. Journal of glaucoma. 2017 Nov:26(11):e252-e254. doi: 10.1097/IJG.0000000000000779. Epub [PubMed PMID: 29099437]
Ikeda N, Ikeda T, Kohno T. Traumatic myopia secondary to ciliary spasm after blunt eye trauma and reconsideration of its pathogenesis. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2016 Jul:254(7):1411-7. doi: 10.1007/s00417-016-3282-5. Epub 2016 Feb 10 [PubMed PMID: 26860527]
Zadnik K. 2020 Charles F. Prentice Lecture: I Can See Clearly Now. Optometry and vision science : official publication of the American Academy of Optometry. 2023 Jan 1:100(1):17-22. doi: 10.1097/OPX.0000000000001968. Epub 2022 Dec 6 [PubMed PMID: 36705711]
Picotti C, Sanchez V, Fernandez Irigaray L, Iurescia A, Iribarren R. Rapid progression of myopia at onset during home confinement. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2022 Apr:26(2):65.e1-65.e4. doi: 10.1016/j.jaapos.2021.11.014. Epub 2022 Mar 18 [PubMed PMID: 35314313]
Wu PC, Chuang MN, Choi J, Chen H, Wu G, Ohno-Matsui K, Jonas JB, Cheung CMG. Update in myopia and treatment strategy of atropine use in myopia control. Eye (London, England). 2019 Jan:33(1):3-13. doi: 10.1038/s41433-018-0139-7. Epub 2018 Jun 11 [PubMed PMID: 29891900]
Shukla Y. Accommodative anomalies in children. Indian journal of ophthalmology. 2020 Aug:68(8):1520-1525. doi: 10.4103/ijo.IJO_1973_18. Epub [PubMed PMID: 32709767]
Niazi S, Moshirfar M, Alizadeh F, Doroodgar F, Baradaran-Rafii A, Filutowski O, Niazi F, Ambrósio R Jr. Association of 2 Lysyl Oxidase Gene Single Nucleotide Polymorphisms with Keratoconus: A Nationwide Registration Study. Ophthalmology science. 2023 Jun:3(2):100247. doi: 10.1016/j.xops.2022.100247. Epub 2022 Nov 9 [PubMed PMID: 36748061]
Mongkolareepong N, Mekhasingharak N, Pimpha O. Factors associated with corneal astigmatism change after ptosis surgery. International journal of ophthalmology. 2022:15(4):576-580. doi: 10.18240/ijo.2022.04.08. Epub 2022 Apr 18 [PubMed PMID: 35450188]
Baskaran K, Rosén R, Lewis P, Unsbo P, Gustafsson J. Benefit of adaptive optics aberration correction at preferred retinal locus. Optometry and vision science : official publication of the American Academy of Optometry. 2012 Sep:89(9):1417-23. doi: 10.1097/OPX.0b013e318264f2a7. Epub [PubMed PMID: 22842306]
Level 3 (low-level) evidence