Introduction
Achilles tendon rupture is the most common tendon rupture in the lower extremity.[1][2][3][4][5] The injury most commonly occurs in adults in their third to fifth decade of life.[6] Acute ruptures often present with sudden onset of pain associated with a "snapping" or audible "pop" heard at the injury site. Patients can describe the sensation of being kicked in the lower leg. The injury causes significant pain and disability.
Achilles tendon injuries predominantly occur in individuals who engage in sporadic physical activity, often referred to as "weekend warrior" athletes, and they most frequently occur during soccer, racket games, or basketball.[1] These injuries are reportedly misdiagnosed as ankle sprains in 20% to 25% of patients. The age group most commonly affected by Achilles tendon injuries falls within the third to fifth decade of life. Approximately 10% of patients report experiencing prodromal symptoms before the injury. Additionally, several recognized risk factors include prior intratendinous degeneration (eg, tendinosis), fluoroquinolone use, steroid injections, and inflammatory arthritides.[2][3][4][5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Causes of Achilles tendon rupture include sudden forced plantar flexion of the foot, direct trauma, and long-standing tendinopathy or intratendinous degenerative conditions. Sports often associated with Achilles tendon rupture include soccer, basketball, and racquet games.[1] Risk factors for a rupture of the Achilles tendon include poor conditioning before exercise, prolonged use of corticosteroids, overexertion, fluoroquinolone antibiotics, oral bisphosphonates, and previous Achilles tendinopathy, diabetes, hyperparathyroidism, and genetic factors.[7][8][9][10]
End-stage kidney disease (ESRD) is also highly associated with an increased incidence of Achilles tendon rupture due to a combination of factors. This population group is commonly prescribed fluoroquinolones and corticosteroids before or after a kidney transplant. In addition, when ESRD leads to weekly dialysis, it creates multiple metabolic abnormalities, such as hyperparathyroidism, which increases the risk of tendon ruptures even more.[11]
Systemic Factors
Systemic diseases that may be associated with Achilles tendon injuries include the following:
- Chronic renal failure
- Collagen deficiency
- Diabetes mellitus
- Gout
- Infections
- Lupus
- Parathyroid disorders
- Rheumatoid arthritis
- Thyroid disorders
Foot problems that increase the risk of Achilles tendon injuries include the following:
- Cavus foot
- Insufficient gastroc-soleus flexibility and strength
- limited ability to perform ankle dorsiflexion
- Tibia vara
- Varus alignment with functional hyperpronation
Epidemiology
The incidence of Achilles tendon ruptures varies in the literature, with recent studies reporting a rate of up to 40 patients per 100,000 patient population annually.[12] The significant increase in ruptures this past decade is thought to be linked to the increased number of individuals engaging in sporting activities, particularly adults older than 30. During recreational sports, 75% of ruptures occur in men between the third and fourth decades of life.[13]
The true incidence of Achilles tendinosis is unknown, but more than 20% of ruptures are misdiagnosed.[13] Reported incidence rates among athletes are 7% to 18% in runners, 9% in dancers, 5% in gymnasts, 2% in tennis players, and less than 1% in American football players. Achilles disorders affect approximately 1 million athletes per year.[9]
Pathophysiology
The pathophysiology of Achilles tendon ruptures involves a combination of mechanical, structural, and biomechanical factors.
- Mechanical factors: The Achilles tendon is the strongest tendon in the body, in part due to its configuration. As it descends from its origin, it twists counterclockwise on the right and clockwise on the left, rotating 90°.[14] However, it can rupture when the tendon is suddenly exposed to excessive tensile loads.[15]
- Structural factors: The Achilles tendon comprises mainly dense, parallel, type 1 collagen fibers organized into fascicles.[16][17] As people age, parallel collagen fibers become less organized and more prone to degeneration. Additionally, certain conditions, such as diabetes and chronic kidney disease, can compromise the tendon's structural integrity and increase the risk of rupture.[18]
- Biomechanical factors: Stiffness is associated with potential risk factors for Achilles injuries, while high foot arches decrease the risk of Achilles injuries.[19] When the tendon is exposed to chronic stress or repeated microtrauma, biomechanical factors combined with a compromised blood supply can lead to the degeneration of tendon fibers and potential rupture.[19]
The Achilles tendon typically ruptures 2 to 6 cm above the calcaneal insertion. This area is where its tendon fibers twist and blood supply is diminished. Studies have found reduced capillary oxygenation and microperfusion at 5 cm above the calcaneal tubercle compared with 1 cm above the tendon insertion.[20]
Histopathology
A healthy tendon is predominately composed of 90% collagen type I.[16][17] Following a tendon rupture, a notable alteration occurs involving the rupture of strong collagen type I fibers and an increased amount of collagen type III, which are less resistant to tensile strength. This pathological change causes the previous healthy tendon to lose its biomechanical properties.[16]
In the initial phases of healing, inflammatory cells infiltrate the rupture site with neutrophils and macrophages. In the later stages of recovery, fibroblasts, responsible for producing collagen, proliferate within the tendon tissue.[21]
Furthermore, specific comorbidities can significantly influence the histology of the Achilles tendon. For instance, patients with diabetes patients have increased stiffness of the muscle-tendon unit, severe thickening of the Achilles tendon and plantar fascia, and disorganized distribution of tendon fibers.[18]
History and Physical
Patients often present with acute, sharp pain in the Achilles tendon region, typically following a sport. The physician will inquire about patients’ symptoms, including their onset and how they have progressed. Asking about previous injuries, social and medical history is also paramount. For example, athletic versus non-athletic patients may be treated differently due to their lifestyle and potential for a re-rupture.
On physical examination, patients with Achilles tendon rupture cannot stand on their toes or may demonstrate significant weakness in ankle plantar flexion. Palpation may reveal a tendon discontinuity or signs of bruising around the posterior ankle.
The examiner should perform the Thompson test to assess for Achilles tendon continuity in the setting of suspected rupture. The patient is positioned in the prone position with the ipsilateral knee flexed to about 90 degrees while the foot and ankle rest. By squeezing the calf, the examiner observes the presence and degree of plantarflexion at the foot and ankle. This should be compared to the contralateral side. A positive (abnormal) test is strongly associated with Achilles rupture.
Evaluation
Following a thorough history and physical exam, the physician should determine whether the patient sustained an Achilles rupture, particularly when a positive Thompson test is 96% to 100% sensitive and 93% to 100% specific.[22] Nevertheless, as previously mentioned, over 20% of Achilles tendon ruptures are misdiagnosed.[13]
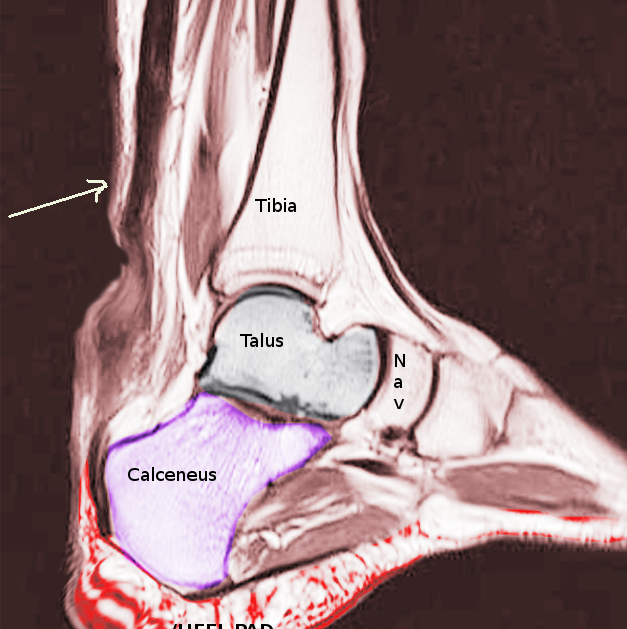
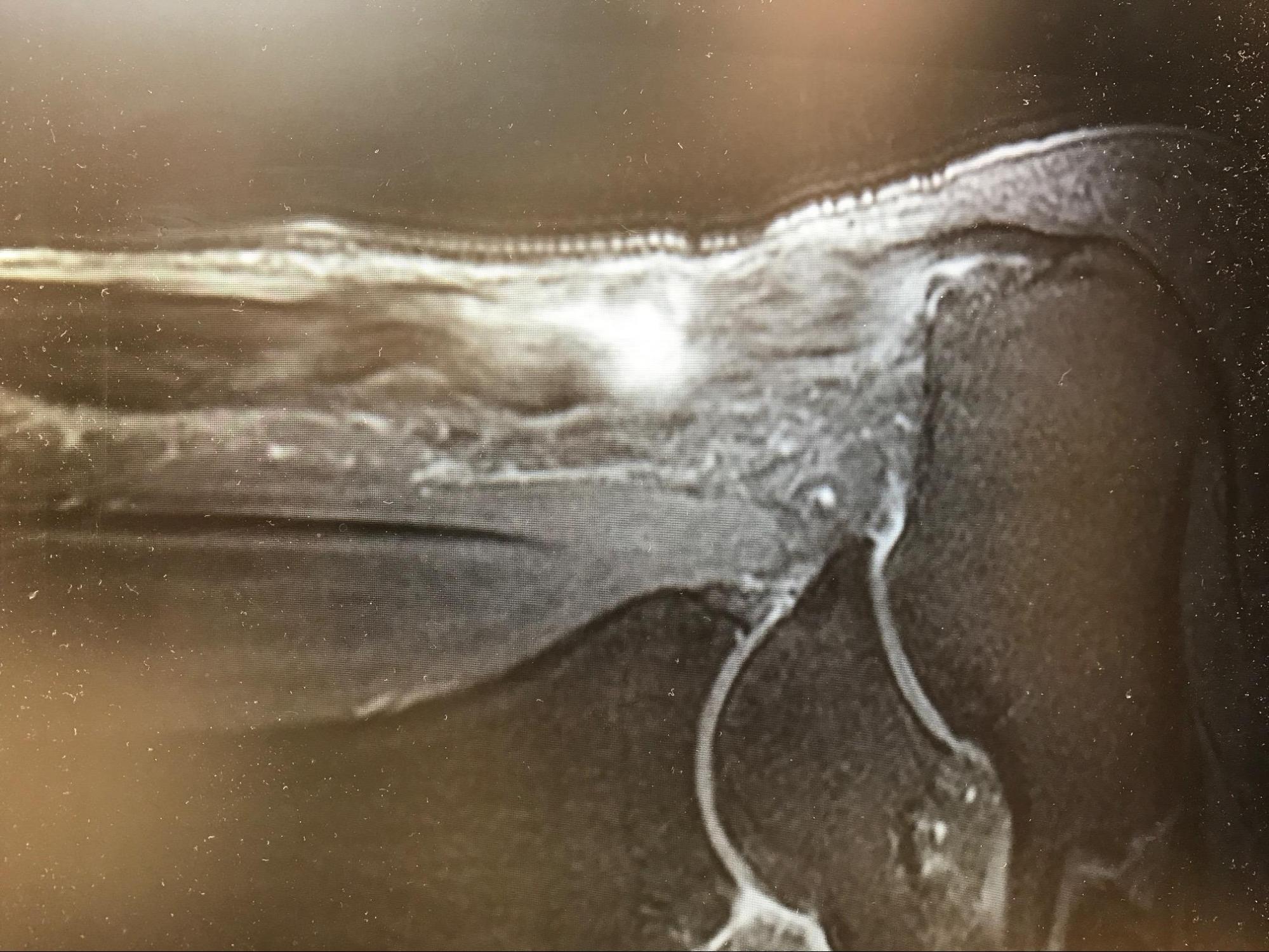
Imaging tests, such as plain radiograph, MRI, or ultrasound, may be ordered to rule out other injuries and confirm the diagnosis of Achilles tendon rupture. In the setting of trauma to the lower leg, radiographs are obtained to rule out the presence of a fracture. MRI and ultrasound can confirm clinical suspicion of Achilles tendon ruptures.[10]
The clinical diagnostic criteria for evaluating Achilles tendon ruptures are more sensitive than MRI studies. In addition, MRI studies can be expensive, time-consuming, and delay surgical treatment. For these reasons, MRI should only be obtained in ambiguous presentations and subacute or chronic injuries for preoperative planning.[23]
Treatment / Management
There is still debate surrounding the potential benefits versus risks of surgical intervention for Achilles tendon ruptures. Studies have demonstrated good functional results and patient satisfaction with operative and nonoperative modalities.[4][11][12] Historically, conservative management has shown a higher re-rupture rate when compared to surgical interventions. However, with the advancement of rehabilitation programs, the difference in re-rupture rates between these groups is much lower (risk difference 1.6%), while operative treatment results in higher complications such as wound dehiscence and infection.[24](A1)
Nonoperative Management
The initial management of Achilles tendon rupture is rest, elevation, pain control, and functional bracing. Healing rates with serial casting/functional bracing are no different compared to the surgical anastomosis of the tendon, but return to work may be slightly prolonged in patients treated medically. All patients require physical and orthotic therapy to help strengthen the muscles and improve the ankle's range of motion.[4][11][12](A1)
Patients with significant medical comorbidities or relatively sedentary lifestyles are often recommended for nonoperative management. Chronicity of the injury and soft tissue or skin integrity is also considered. Benefits of a nonsurgical approach include no hospital admission costs, no wound complications, and no risk of anesthesia. The most significant disadvantage is the risk of re-rupture.[4][11][12](A1)
Operative Management
Several techniques for Achilles tendon repair exist, but they all involve the reapproximation of torn ends.
- Open repair: These techniques involve making incisions that can vary between a straight line, lazy S, or inverted L. The Achilles tendon is debrided until only healthy tendon fibers are seen. A Kessler, Bunnel, Krakow, or Giftbox technique could directly repair the tendon. The Krakow and Giftbox techniques (a modified Krakow) are interlocking stitches that provide the strongest outcome.
- Mini open repair: A small incision is made proximally to debride the proximal portion of the tendon and interlock stitches, usually in a Krakow fashion. Additionally, 2 small incisions are made in the calcaneal for bone anchors. A suture passer connects the proximal and distal ends into a bone anchor on each side of the calcaneus.
- Minimally invasive repair: This technique was pioneered by the PARS system (Arthrex). A small incision is made transversely on the posterior aspect of the leg. A gig device is used to allow suture passage through minimal puncture incisions.
Although minimally invasive surgery gained popularity when it entered the market, there is an 18% rate of sural nerve injury when the nerve is not exposed intraoperatively.[25] In addition, most research articles about percutaneous Achilles tendon surgeries are authored by individuals who serve as paid consultants for the sales company that owns the device, which is a conflict of interest essential to keep in mind.
The plantaris tendon, gastroc-soleus aponeurosis, or the flexor hallucis tendon sometimes reinforce the repair. In chronic ruptures with the flexor hallucis tendon, the muscle gains 52% hypertrophy, showing strong adaptation capacity after transfer.[26](B2)
Overall, the healing rates between casting and surgical repair are similar.[24][27] The main benefit of a surgical repair is an early return to activity and reduced risk of re-rupture; the greatest risk is surgical complications such as wound dehiscence, infection, and deep vein thrombosis.[24][27][28][29] Due to the increased efficacy in strength and outcome following a surgical repair, there is a consensus that athletes should opt for this management.[29](A1)
The Role of Biologics
The use of regenerative medicine has been studied extensively in the last decade with contradictory results. Zou and colleagues found that patients undergoing Achilles tendon rupture augmented by Platelet-Rich Plasma (PRP) had better isokinetic muscle, higher functional scores, and improved ankle range of motion compared to the control group. Other articles found no significant difference in the outcome of patients treated with PRP compared to control.[30] More consistency is found in studies including sport-active patients, as this population group recovers their range of motion earlier and takes less time to return to activity.[30]
Bone Marrow Aspirate Concentrate (BMAC) has also improved clinical function and reduced foot and ankle pain without serious adverse effects.[31][32](B2)
Final Thoughts
The patient-surgeon discussion should include a detailed discussion concerning the current literature reporting satisfactory outcomes with both treatment plans and the following topics:
- Possibility of quicker return to work with operative intervention
- Equivalent plantar flexion strength at long-term followup
- Possibility of an increased risk of re-rupture and re-injury with nonoperative management (compared to operative management)
- Lower complication rates for nonoperative treatment compared to operative management
Differential Diagnosis
Differential diagnoses for Achilles tendon rupture include the following:
- Achilles bursitis
- Ankle fracture
- Ankle impingement syndrome
- Ankle osteoarthritis
- Ankle sprain
- Calf injuries
- Calcaneofibular ligament injury
- Calcaneus fractures
- Deep venous thrombosis (DVT)
- Exertional compartment syndrome
- Fascial tears
- Gastrocnemius or soleus muscle strain or rupture
- Haglund deformity
- Plantaris tendon tear
- Psoriatic arthritis
- Reiter syndrome
- Retrocalcaneal bursitis
- Ruptured Baker cyst
- Syndesmosis
- Talofibular ligament injury
Prognosis
For most patients with Achilles tendon rupture, the prognosis is excellent. But in some nonathletes, there may be some residual deficits like a reduced range of motion. Most athletes can resume their previous sporting activity without any limitations. However, non-surgical treatment has a rerupture rate of nearly 40% compared to only 0.5% for those treated surgically.
Complications
Rerupture
- While newer level 1 evidence has reported no difference in rerupture rates, prior studies have suggested a 10% to 40% re-rupture rate with nonoperative management compared to 1% to 2% after surgery.
- Lantto et al recently demonstrated the following in a randomized controlled trial of 60 patients from 2009 to 2013 at 18-month follow-up:
- Similar Achilles tendon performance scores
- Slightly increased calf muscle strength differences favoring the operative cohort (10% to 18% strength difference) at 18-month follow-up
- Slightly better health-related quality of life scores in the domains of physical functioning and bodily pain favored the operative cohort[33]
- Lantto et al recently demonstrated the following in a randomized controlled trial of 60 patients from 2009 to 2013 at 18-month follow-up:
Wound Healing Complications
- Overall, a 5% to 10% risk following surgery
- Risk factors for postoperative wound complications include the following:
- Smoking (most common and most significant risk factor)
- Female sex
- Steroid use
- Open technique (vs percutaneous procedures)
Sural Nerve Injury
- Increased rate of injury associated with the percutaneous procedure (compared to open technique)
Postoperative and Rehabilitation Care
Regardless of the specific treatment method for tendon rupture, participating in an exercise program is vital. Engaging in swimming, cycling, jogging, or walking can effectively enhance muscle strength and range of motion.
Rehabilitation
Rehabilitation will vary based on whether a surgical versus nonsurgical approach is taken and referring physician’s protocol. This highlights the importance of close collaboration between the therapist and referring physician to optimize care. This is particularly important for managing brace use and determining weight-bearing status, as these aspects often exhibit the most significant variations in therapy management for this condition.
The duration of immobilization can vary depending on whether an operative or non-operative approach is chosen. In the operative approach, immobilization typically lasts for approximately 2 to 4 weeks, while in operative management, it can range from 3 to 9 weeks conservative, with the use of orthotics, according to the referring orthopedic protocol. Varying degrees of plantarflexion to neutral positioning are utilized during this time, with specifics on the optimal positioning still widely debated.[34][35][36] Emphasizing the need to avoid hyper dorsiflexion during this time has been noted as an important component in avoiding elongation of the Achilles tendon and long-term functional deficits.[34]
If conservative methods are used, therapy begins during the immobilization phase of cast wear, focusing on weight-bearing mobilization training and exercises to preserve strength in the remaining portions of the affected limb. More recent studies have shown the benefits of initiating functional casts combined with early weight bearing in conservative treatment, resulting in a faster return to activity and improved ankle dorsiflexion. Traditionally, these benefits were associated with operative treatment, which allowed for earlier weight-bearing and exercise initiation, but this continues to vary and will be determined by the referring physician.[34][35][36]
Functional rehabilitation program for nonsurgical patients following an acute Achilles tendon rupture, according to Glazebrook & Rubinger:
- 0 to 2 weeks: non-weight bearing with crutches.
- 2 to 4 weeks: walking boot with maximum heel lifts, gradual protected weight bearing with crutches (25% increments every week), active plantar and dorsiflexion range of motion exercises to neutral, inversion and eversion below neutral, modalities to control swelling, physical therapy 2 to 3 times a week, non-weight bearing cardio exercises such as biking.
- 4 to 6 weeks: weight bearing as tolerated in the boot, maintain activities from previous weeks with the progression of electrical muscle stimulation, physical therapy 2 to 3 times a week.
- 6 to 8 weeks: remove heel lifts gradually (1 lift daily as tolerated), 100% weight bear in the boot now, physical therapy 2 times per week.
- 8 to 12 weeks: wean off the boot.[37]
For surgical patients, rehabilitation exercises typically begin 2 to 4 weeks postop.[17] In the past decade, there has been a trend towards less rigid immobilization, earlier weight-bearing, and accelerated functional rehabilitation following surgery.[38] Post-immobilization therapy consists of exercise progression, including ankle range of motion exercises, resistive and progressive strengthening exercises, isometric exercises, cardiovascular exercises, and balance exercises as appropriate.[18] A standardized accelerated protocol following a surgical repair of the Achilles tendon has not been published, and a better level of evidence studies is needed to evaluate risks vs. benefits.
Exercise focus is typically low impact for the first 6 months, with high-impact exercises incorporated after 6 months, emphasizing a return to sport as appropriate. Data has shown a need for a heavy focus on calf strengthening within the first year of injury as a reduction in strength gain potential has been demonstrated beyond the one-year post-injury date.[34]
Deterrence and Patient Education
While active patients and recreational athletes often return to baseline activity levels and work following nonoperative and operative management of these injuries. High-level professional athletes often report inferior results and return to play regardless of the chosen management plan.
A 2017 study from the American Journal of Sports Medicine reported professional athletes' follow-up performance (NBA, NFL, MLB, and NHL) at 1- and 2-year follow-ups after surgery performed between 1989 and 2013:
- >30% failure to return to play
- Athletes returning noted (at 1-year follow-up) the following:
- Fewer games played, overall
- Less playing time, overall
- Suboptimal performance level, overall
- Athletes able to return to play by 2-year follow-up show no statistically significant difference in performance level[39]
Thus, athletes demonstrating the ability to return to play in 1 year should expect to achieve continuous improvement to baseline performance by the following season.
Pearls and Other Issues
To prevent Achilles tendon rupture, adequate warming and stretching before physical activity is recommended.
Enhancing Healthcare Team Outcomes
Even though there are several treatments for Achilles tendon rupture, there is no consensus on which to undertake. The management of Achilles tendon injury widely varies among orthopedic surgeons and sports physicians. Furthermore, there is no uniformity in postoperative rehabilitation. Experts recommend that an interprofessional approach may help achieve better outcomes.[40][41]
The team should include a trauma surgeon, an orthopedic surgeon, a rehabilitation specialist, and a sports physician. The pharmacist must ensure the patient is not on any medications that can affect healing. The nurse should educate the patient on the importance of stretching before any exercise and participating in a regular exercise program after repair.
Outcomes
Conservative treatment is usually preferred for nonathletes, but the risk of rerupture is high. While surgery offers a lower risk of re-rupture, it is also associated with postsurgical complications that may delay recovery. Overall, the outcomes for Achilles tendon rupture are good to excellent after treatment.[42][43][44]
Media
(Click Image to Enlarge)
References
Holm C, Kjaer M, Eliasson P. Achilles tendon rupture--treatment and complications: a systematic review. Scandinavian journal of medicine & science in sports. 2015 Feb:25(1):e1-10. doi: 10.1111/sms.12209. Epub 2014 Mar 20 [PubMed PMID: 24650079]
Level 1 (high-level) evidenceCarmont MR. Achilles tendon rupture: the evaluation and outcome of percutaneous and minimally invasive repair. British journal of sports medicine. 2018 Oct:52(19):1281-1282. doi: 10.1136/bjsports-2017-099002. Epub 2018 Jun 23 [PubMed PMID: 29936431]
Noback PC, Freibott CE, Tantigate D, Jang E, Greisberg JK, Wong T, Vosseller JT. Prevalence of Asymptomatic Achilles Tendinosis. Foot & ankle international. 2018 Oct:39(10):1205-1209. doi: 10.1177/1071100718778592. Epub 2018 Jun 1 [PubMed PMID: 29855207]
Haapasalo H, Peltoniemi U, Laine HJ, Kannus P, Mattila VM. Treatment of acute Achilles tendon rupture with a standardised protocol. Archives of orthopaedic and trauma surgery. 2018 Aug:138(8):1089-1096. doi: 10.1007/s00402-018-2940-y. Epub 2018 May 3 [PubMed PMID: 29725765]
Yasui Y, Tonogai I, Rosenbaum AJ, Shimozono Y, Kawano H, Kennedy JG. The Risk of Achilles Tendon Rupture in the Patients with Achilles Tendinopathy: Healthcare Database Analysis in the United States. BioMed research international. 2017:2017():7021862. doi: 10.1155/2017/7021862. Epub 2017 Apr 30 [PubMed PMID: 28540301]
Järvinen TA, Kannus P, Maffulli N, Khan KM. Achilles tendon disorders: etiology and epidemiology. Foot and ankle clinics. 2005 Jun:10(2):255-66 [PubMed PMID: 15922917]
Xergia SA, Tsarbou C, Liveris NI, Hadjithoma Μ, Tzanetakou IP. Risk factors for Achilles tendon rupture: an updated systematic review. The Physician and sportsmedicine. 2023 Dec:51(6):506-516. doi: 10.1080/00913847.2022.2085505. Epub 2022 Jun 10 [PubMed PMID: 35670156]
Level 1 (high-level) evidenceAlušík Š, Paluch Z. [Drug induced tendon injury]. Vnitrni lekarstvi. 2018 Winter:63(12):967-971 [PubMed PMID: 29334747]
Ahmad J, Jones K. The Effect of Obesity on Surgical Treatment of Achilles Tendon Ruptures. The Journal of the American Academy of Orthopaedic Surgeons. 2017 Nov:25(11):773-779. doi: 10.5435/JAAOS-D-16-00306. Epub [PubMed PMID: 28957986]
Egger AC, Berkowitz MJ. Achilles tendon injuries. Current reviews in musculoskeletal medicine. 2017 Mar:10(1):72-80. doi: 10.1007/s12178-017-9386-7. Epub [PubMed PMID: 28194638]
Humbyrd CJ, Bae S, Kucirka LM, Segev DL. Incidence, Risk Factors, and Treatment of Achilles Tendon Rupture in Patients With End-Stage Renal Disease. Foot & ankle international. 2018 Jul:39(7):821-828. doi: 10.1177/1071100718762089. Epub 2018 Mar 27 [PubMed PMID: 29582683]
Meulenkamp B, Stacey D, Fergusson D, Hutton B, Mlis RS, Graham ID. Protocol for treatment of Achilles tendon ruptures; a systematic review with network meta-analysis. Systematic reviews. 2018 Dec 23:7(1):247. doi: 10.1186/s13643-018-0912-5. Epub 2018 Dec 23 [PubMed PMID: 30580763]
Level 1 (high-level) evidenceMaffulli N, Via AG, Oliva F. Chronic Achilles Tendon Rupture. The open orthopaedics journal. 2017:11():660-669. doi: 10.2174/1874325001711010660. Epub 2017 Jul 31 [PubMed PMID: 29081863]
Edama M, Takabayashi T, Yokota H, Hirabayashi R, Sekine C, Maruyama S, Otani H. Classification by degree of twisted structure of the fetal Achilles tendon. Surgical and radiologic anatomy : SRA. 2021 Oct:43(10):1691-1695. doi: 10.1007/s00276-021-02803-9. Epub 2021 Jul 14 [PubMed PMID: 34263342]
Hijazi KM, Singfield KL, Veres SP. Ultrastructural response of tendon to excessive level or duration of tensile load supports that collagen fibrils are mechanically continuous. Journal of the mechanical behavior of biomedical materials. 2019 Sep:97():30-40. doi: 10.1016/j.jmbbm.2019.05.002. Epub 2019 May 7 [PubMed PMID: 31085458]
Winnicki K, Ochała-Kłos A, Rutowicz B, Pękala PA, Tomaszewski KA. Functional anatomy, histology and biomechanics of the human Achilles tendon - A comprehensive review. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2020 May:229():151461. doi: 10.1016/j.aanat.2020.151461. Epub 2020 Jan 21 [PubMed PMID: 31978571]
Ho JO, Sawadkar P, Mudera V. A review on the use of cell therapy in the treatment of tendon disease and injuries. Journal of tissue engineering. 2014:5():2041731414549678. doi: 10.1177/2041731414549678. Epub 2014 Sep 18 [PubMed PMID: 25383170]
Nichols AEC, Oh I, Loiselle AE. Effects of Type II Diabetes Mellitus on Tendon Homeostasis and Healing. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2020 Jan:38(1):13-22. doi: 10.1002/jor.24388. Epub 2019 Jun 24 [PubMed PMID: 31166037]
Lorimer AV, Hume PA. Achilles tendon injury risk factors associated with running. Sports medicine (Auckland, N.Z.). 2014 Oct:44(10):1459-72. doi: 10.1007/s40279-014-0209-3. Epub [PubMed PMID: 24898814]
Cao S, Teng Z, Wang C, Zhou Q, Wang X, Ma X. Influence of Achilles tendon rupture site on surgical repair outcomes. Journal of orthopaedic surgery (Hong Kong). 2021 Jan-Apr:29(1):23094990211007616. doi: 10.1177/23094990211007616. Epub [PubMed PMID: 33845659]
Freedman BR, Gordon JA, Soslowsky LJ. The Achilles tendon: fundamental properties and mechanisms governing healing. Muscles, ligaments and tendons journal. 2014 Apr:4(2):245-55 [PubMed PMID: 25332943]
Reiman M, Burgi C, Strube E, Prue K, Ray K, Elliott A, Goode A. The utility of clinical measures for the diagnosis of achilles tendon injuries: a systematic review with meta-analysis. Journal of athletic training. 2014 Nov-Dec:49(6):820-9. doi: 10.4085/1062-6050-49.3.36. Epub [PubMed PMID: 25243736]
Level 1 (high-level) evidenceGarras DN, Raikin SM, Bhat SB, Taweel N, Karanjia H. MRI is unnecessary for diagnosing acute Achilles tendon ruptures: clinical diagnostic criteria. Clinical orthopaedics and related research. 2012 Aug:470(8):2268-73. doi: 10.1007/s11999-012-2355-y. Epub 2012 Apr 27 [PubMed PMID: 22538958]
Level 2 (mid-level) evidenceOchen Y, Beks RB, van Heijl M, Hietbrink F, Leenen LPH, van der Velde D, Heng M, van der Meijden O, Groenwold RHH, Houwert RM. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ (Clinical research ed.). 2019 Jan 7:364():k5120. doi: 10.1136/bmj.k5120. Epub 2019 Jan 7 [PubMed PMID: 30617123]
Level 1 (high-level) evidenceCarmont MR, Rossi R, Scheffler S, Mei-Dan O, Beaufils P. Percutaneous & Mini Invasive Achilles tendon repair. Sports medicine, arthroscopy, rehabilitation, therapy & technology : SMARTT. 2011 Nov 14:3():28. doi: 10.1186/1758-2555-3-28. Epub 2011 Nov 14 [PubMed PMID: 22082172]
Oksanen MM, Haapasalo HH, Elo PP, Laine HJ. Hypertrophy of the flexor hallucis longus muscle after tendon transfer in patients with chronic Achilles tendon rupture. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2014 Dec:20(4):253-7. doi: 10.1016/j.fas.2014.06.003. Epub 2014 Jul 2 [PubMed PMID: 25457661]
Level 2 (mid-level) evidenceMyhrvold SB, Brouwer EF, Andresen TKM, Rydevik K, Amundsen M, Grün W, Butt F, Valberg M, Ulstein S, Hoelsbrekken SE. Nonoperative or Surgical Treatment of Acute Achilles' Tendon Rupture. The New England journal of medicine. 2022 Apr 14:386(15):1409-1420. doi: 10.1056/NEJMoa2108447. Epub [PubMed PMID: 35417636]
Deng S, Sun Z, Zhang C, Chen G, Li J. Surgical Treatment Versus Conservative Management for Acute Achilles Tendon Rupture: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2017 Nov-Dec:56(6):1236-1243. doi: 10.1053/j.jfas.2017.05.036. Epub [PubMed PMID: 29079238]
Level 1 (high-level) evidenceMansfield K, Dopke K, Koroneos Z, Bonaddio V, Adeyemo A, Aynardi M. Achilles Tendon Ruptures and Repair in Athletes-a Review of Sports-Related Achilles Injuries and Return to Play. Current reviews in musculoskeletal medicine. 2022 Oct:15(5):353-361. doi: 10.1007/s12178-022-09774-3. Epub 2022 Jul 9 [PubMed PMID: 35804260]
Indino C, D'Ambrosi R, Usuelli FG. Biologics in the Treatment of Achilles Tendon Pathologies. Foot and ankle clinics. 2019 Sep:24(3):471-493. doi: 10.1016/j.fcl.2019.04.009. Epub 2019 May 21 [PubMed PMID: 31370998]
Bachir RM, Zaia IM, Santos GS, Fonseca LFD, Boni G, Guercia RF, Ferreira GF, Lana JFSD. Bone Marrow Aspirate Concentrate Improves Outcomes in Adults With Osteochondral Dissecans of the Talus and Achilles Rupture. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2023 Mar:39(3):881-886. doi: 10.1016/j.arthro.2022.11.034. Epub 2022 Dec 8 [PubMed PMID: 36543662]
Stein BE, Stroh DA, Schon LC. Outcomes of acute Achilles tendon rupture repair with bone marrow aspirate concentrate augmentation. International orthopaedics. 2015 May:39(5):901-5. doi: 10.1007/s00264-015-2725-7. Epub 2015 Mar 22 [PubMed PMID: 25795246]
Level 2 (mid-level) evidenceLantto I, Heikkinen J, Flinkkila T, Ohtonen P, Siira P, Laine V, Leppilahti J. A Prospective Randomized Trial Comparing Surgical and Nonsurgical Treatments of Acute Achilles Tendon Ruptures. The American journal of sports medicine. 2016 Sep:44(9):2406-14. doi: 10.1177/0363546516651060. Epub 2016 Jun 15 [PubMed PMID: 27307495]
Level 1 (high-level) evidencePark SH, Lee HS, Young KW, Seo SG. Treatment of Acute Achilles Tendon Rupture. Clinics in orthopedic surgery. 2020 Mar:12(1):1-8. doi: 10.4055/cios.2020.12.1.1. Epub 2020 Feb 13 [PubMed PMID: 32117532]
Saxena A, Giai Via A, Grävare Silbernagel K, Walther M, Anderson R, Gerdesmeyer L, Maffulli N. Current Consensus for Rehabilitation Protocols of the Surgically Repaired Acute Mid-Substance Achilles Rupture: A Systematic Review and Recommendations From the "GAIT" Study Group. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2022 Jul-Aug:61(4):855-861. doi: 10.1053/j.jfas.2021.12.008. Epub 2021 Dec 10 [PubMed PMID: 35120805]
Level 3 (low-level) evidenceYang X, Meng H, Quan Q, Peng J, Lu S, Wang A. Management of acute Achilles tendon ruptures: A review. Bone & joint research. 2018 Oct:7(10):561-569. doi: 10.1302/2046-3758.710.BJR-2018-0004.R2. Epub 2018 Nov 3 [PubMed PMID: 30464836]
Glazebrook M, Rubinger D. Functional Rehabilitation for Nonsurgical Treatment of Acute Achilles Tendon Rupture. Foot and ankle clinics. 2019 Sep:24(3):387-398. doi: 10.1016/j.fcl.2019.05.001. Epub 2019 Jun 22 [PubMed PMID: 31370992]
Gould HP, Bano JM, Akman JL, Fillar AL. Postoperative Rehabilitation Following Achilles Tendon Repair: A Systematic Review. Sports medicine and arthroscopy review. 2021 Jun 1:29(2):130-145. doi: 10.1097/JSA.0000000000000309. Epub [PubMed PMID: 33972490]
Level 1 (high-level) evidenceTrofa DP, Miller JC, Jang ES, Woode DR, Greisberg JK, Vosseller JT. Professional Athletes' Return to Play and Performance After Operative Repair of an Achilles Tendon Rupture. The American journal of sports medicine. 2017 Oct:45(12):2864-2871. doi: 10.1177/0363546517713001. Epub 2017 Jun 23 [PubMed PMID: 28644678]
Dams OC, van den Akker-Scheek I, Diercks RL, Wendt KW, Zwerver J, Reininga IHF. Surveying the management of Achilles tendon ruptures in the Netherlands: lack of consensus and need for treatment guidelines. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2019 Sep:27(9):2754-2764. doi: 10.1007/s00167-018-5049-5. Epub 2018 Jul 3 [PubMed PMID: 29971520]
Level 3 (low-level) evidenceHertel G, Götz J, Grifka J, Willers J. [Achilles tendon rupture : Current diagnostic and therapeutic standards]. Der Orthopade. 2016 Aug:45(8):709-20. doi: 10.1007/s00132-016-3287-0. Epub [PubMed PMID: 27405457]
Song YJ, Chen G, Jia SH, Xu WB, Hua YH. Good outcomes at mid-term following the reconstruction of chronic Achilles tendon rupture with semitendinosus allograft. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2020 May:28(5):1619-1624. doi: 10.1007/s00167-018-5113-1. Epub 2018 Aug 20 [PubMed PMID: 30128686]
Westin O, Nilsson Helander K, Grävare Silbernagel K, Samuelsson K, Brorsson A, Karlsson J. Patients with an Achilles tendon re-rupture have long-term functional deficits and worse patient-reported outcome than primary ruptures. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2018 Oct:26(10):3063-3072. doi: 10.1007/s00167-018-4952-0. Epub 2018 Apr 24 [PubMed PMID: 29691618]
Becher C, Donner S, Brucker J, Daniilidis K, Thermann H. Outcome after operative treatment for chronic versus acute Achilles tendon rupture - A comparative analysis. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2018 Apr:24(2):110-114. doi: 10.1016/j.fas.2016.12.003. Epub 2017 Jan 4 [PubMed PMID: 29409231]
Level 2 (mid-level) evidence