Introduction
Hamate fractures are rare and underreported. These injuries are usually misdiagnosed or confused with simple wrist sprains. Delayed diagnosis is not uncommon.[1]
The hamate is a triangular-shaped bone that forms part of the distal carpal row, articulating with the capitate (radially), triquetrum (proximally), and fifth and fourth metacarpals (distally).
Considering its unique anatomy (Figure 1), hamate fractures usually get subdivided into two broad groups: hook fractures and body fractures.[2][3]
Classification of hamate fractures:
- Type 1: Hook of the hamate fracture
- Type 2: Body of the hamate fracture
- 2a: Coronal (may be dorsal oblique or splitting fracture)
- 2b: Transverse fracture
Associated hook fracture injuries:
- Ulnar artery injury
- Ulnar nerve injury
Associated body fracture Injuries:
- Fourth and fifth metacarpal fracture-dislocation
- Greater arc perilunate fracture-dislocation
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The hook of hamate fracture frequently occurs in sports where a firm grip is required, such as tennis, baseball, and golf.[2] Body of the hamate fractures are related to higher energy trauma such as a punch and may be associated with concomitant carpal fractures and carpometacarpal dislocations. Body fractures are less common.[4][5]
Epidemiology
Hamate fractures are unfrequent injuries, accounting for 2 to 4% of carpal fractures.[6][7][8][9] Distal carpal row fractures are less common than first row fractures. Hamate fractures (hook and body) tend to occur in young, active patients. They are unusual in children.
Pathophysiology
The hook of hamate injuries are mainly due to repeated impact, usually, a sporting activity (racket, club, bat) exerting a direct force against the hamate.[10][11][12] The hook of the hamate is always at risk because of its peculiar anatomy, protruding from its body into the ulnar aspect of the palm. Avulsion fractures of the hook may also occur, taking into account that this portion of the hamate serves as an attachment point for three tendons (opponens digiti minimi, flexor digiti minimi, and flexor carpi ulnaris).[13]
The body of the hamate fracture is a consequence of a direct blow over the hypothenar eminence or a considerably strong dorsopalmar compression.[3][14] A body fracture may also accompany high energy trauma resulting in wrist fracture dislocations.[15] Body fractures can lead to axial carpal instability.
History and Physical
Though clinical findings may be vague and unspecific, there are some tests that are useful if a hamate fracture is suspected.
Suspicion should be high in young athletes with chronic pain along the ulnar aspect of the wrist. Chronic wrist pain is common with a hook of the hamate fracture, with tenderness and exquisite pain over the hypothenar area. Paresthesias along the ring and small finger are relatively common in chronic disease.[16] Delayed medical consultation is not uncommon.
Because of its relation to higher energy trauma and associated injuries, the body of the hamate fracture diagnosis tends to be acute. Swelling and tenderness over the dorsal ulnar wrist frequently present in hamate body fractures.
Weakened grip strength is typical. Grasp maneuvers provoke pain along the ulnar side of the wrist. Fourth and fifth metacarpal pain is related to hamate injuries; even metacarpal deformity may be an indirect sign of the body of the hamate fracture.
Pull test: in the hook of the hamate fractures, active flexion of distal interphalangeal joints of the ring and small finger may cause pain. This phenomenon is the result of flexor tendons deforming forces attached at the fracture site.[17][18]
Evaluation
Initial radiographs include anteroposterior and lateral wrist views. The overlapping of the hook of the hamate and its body is known as the "ring sign," a normal finding in the anteroposterior view. In some hook fractures, the so-called "ring sign" may be disrupted. Other signs that are visible in the anteroposterior view are loss of cortical density at the base of the hook and even absence of the hook.[19] Body fractures are usually visible in standard lateral projection or on CT scan.
Nevertheless, standard radiographs possess a high rate of false negatives, with a 70% sensitivity.[20][21] Specific views include carpal tunnel projection and semisupine oblique radially deviated projection.[22] CT scan is often necessary to reach a proper diagnosis (100% sensitivity).[20] MRI scan is only necessary for chronic disease (avascular necrosis)
If a surgical procedure is required, routine blood work should be performed based on the patient's history and physical exam. The complexity of the surgical procedure is also a required element for which the surgeon must account.
Treatment / Management
Surgical indications: displaced fractures, nonunion, ulnar nerve compression, median nerve compression, ulnar artery compression, tendon rupture, and metacarpal subluxation.
- Hook fractures:
- Acute, nondisplaced: Immobilization, ulnar gutter cast for six weeks. There is still debate whether patients may profit from initial surgical treatment in this type of fracture. Sport players will usually benefit from early surgical management, returning to sports activities in three months.
- Acute, displaced: Excision of a bony fragment is the gold standard procedure. Open reduction and internal fixation (screws or Kirschner wires) is another proven treatment. Both alternatives showed similar clinical results.[23]
- Chronic pain, nonunion: These signs require fracture pinning with bone grafting.
Surgical tech tips:
- The motor branch of the ulnar nerve must be clearly spotted and retracted before hook excision or drilling.
-
After fractured fragment excision, periosteum closure should be over the base of the remaining body to protect the ulnar nerve and tendons.
Differential Diagnosis
Ulnar flexor carpi tendinitis and triangular fibrocartilage complex injuries are a common misdiagnosis.[11] A hamate fracture accompanies a small percentage (1 to 2%) of distal radius fracture.[26]
Other differential diagnoses include:
- Bipartite hamate
- Scaphoid fracture
- Capitate fracture
- Triquetrum fracture
- Pisiform fracture
- Ligamentous injuries (without fracture)
- Carpal bone dislocations
Prognosis
Fractures treated conservatively should generally heal in 8 weeks. Non-displaced hook fractures treated conservatively have a 50% rate of nonunion. Symptomatic nonunion will require further surgical treatment. Surgical treatment (fragment excision or ORIF) provides a more rapid return to daily activities and sports.[27]
Complications
- Nonunion
- Posttraumatic arthritis
- Avascular necrosis in proximal pole (body fractures)
- Ulnar nerve compression (Guyon's canal)
- Carpal tunnel syndrome
- Flexor digitorum profundus tendon rupture
- Ulnar artery thrombosis (hypothenar hammer syndrome)
- Ulnar artery compression
- Residual instability of fourth and/or fifth metacarpals
Postoperative and Rehabilitation Care
Physical therapy is mandatory. In the case of conservative treatment, occupational therapy should beg¡n right after cast removal. If ORIF is the preferred method, therapy should begin after a 3-week immobilization protocol. Hook excisions may start early therapy. Rehabilitation protocol should last 4 to 6 weeks.
Deterrence and Patient Education
Patients should be aware of chronic pain and osteoarthritis as common consequences of hamate fractures. Smoking cessation is always a recommendation for fracture healing.
Enhancing Healthcare Team Outcomes
Radiologic knowledge of these infrequent injuries is crucial to reach a proper diagnosis. General practitioners, including nurse practitioners and PAs, should be aware of the high rate of misdiagnoses. Orthopedic surgeons should provide information regarding specific X-ray views and physical examinations. This approach leads to interprofessional teamwork. Patients must receive counsel for further treatment options, especially those involved in sports.
When diagnosing and managing hamate fractures, the entire interprofessional team has to communicate across disciplinary lines for the patient's benefit. Clinicians, including GPs, NPs, and PAs will most likely diagnose the injury specialists to include orthopedists and radiologists will often guide diagnosis and treatment plans. Nursing will assist in surgery and prep the patient. Initially, pain management may be an issue, and pharmacists can recommend optimal pharmaceutical therapy to decrease pain while avoiding opioid overuse. The pharmacists can also report back to nursing or the managing clinician regarding potential interactions and side effects. Post-surgery, the physical and/or occupational therapist will guide rehab, and report back to the other members of the team as to the progress or stagnation/regression of the rehabilitation process. All these disciplines must collaborate across interprofessional lines for optimal patient treatment. [Level 5]
Media
(Click Image to Enlarge)
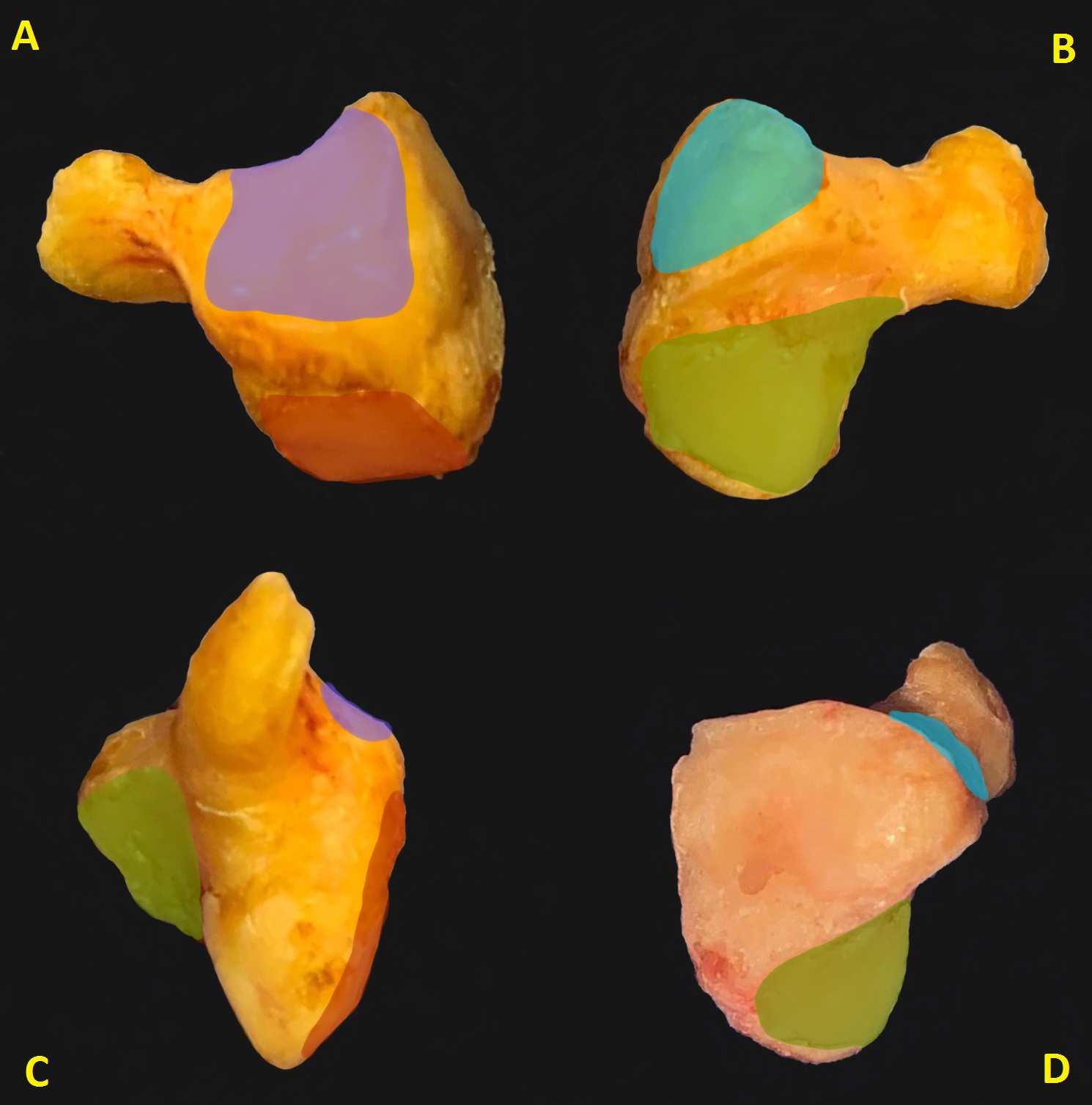
Figure 1. Fresh hamate bone dissection. Radial view (A) with articular surface for fourth metacarpal (violet) and capitate bone (red). Ulnar view (B) showing fifth metacarpal articular surface (light blue) and triquetrum (green). Volar view (C). Dorsal view (D). Anatomical dissection by Mariano O. Abrego
References
Bishop AT, Beckenbaugh RD. Fracture of the hamate hook. The Journal of hand surgery. 1988 Jan:13(1):135-9 [PubMed PMID: 3351218]
Level 2 (mid-level) evidenceArora S, Goyal A, Mittal S, Singh A, Sural S, Dhal A. Combined intraarticular fracture of the body and the hook of hamate: an unusual injury pattern. Journal of hand and microsurgery. 2013 Dec:5(2):92-5. doi: 10.1007/s12593-012-0070-2. Epub 2012 Jun 14 [PubMed PMID: 24426686]
Level 3 (low-level) evidenceHirano K, Inoue G. Classification and treatment of hamate fractures. Hand surgery : an international journal devoted to hand and upper limb surgery and related research : journal of the Asia-Pacific Federation of Societies for Surgery of the Hand. 2005:10(2-3):151-7 [PubMed PMID: 16568508]
Level 3 (low-level) evidenceYalcinkaya M, Azar N, Dogan A. A rare wrist injury: simultaneous fractures of the hamate body and scaphoid waist. Orthopedics. 2009 Aug:32(8):. pii: orthosupersite.com/view.asp?rID=41930. doi: 10.3928/01477447-20090624-23. Epub [PubMed PMID: 19708624]
Level 3 (low-level) evidenceGella S, Borse V, Rutten E. Coronal fractures of the hamate: are they rare or rarely spotted? The Journal of hand surgery, European volume. 2007 Dec:32(6):721-2 [PubMed PMID: 17993445]
Level 3 (low-level) evidenceAldridge JM 3rd, Mallon WJ. Hook of the hamate fractures in competitive golfers: results of treatment by excision of the fractured hook of the hamate. Orthopedics. 2003 Jul:26(7):717-9 [PubMed PMID: 12875568]
Boulas HJ, Milek MA. Hook of the hamate fractures. Diagnosis, treatment, and complications. Orthopaedic review. 1990 Jun:19(6):518-29 [PubMed PMID: 2367145]
Level 3 (low-level) evidenceUrch EY, Lee SK. Carpal fractures other than scaphoid. Clinics in sports medicine. 2015 Jan:34(1):51-67. doi: 10.1016/j.csm.2014.09.006. Epub 2014 Oct 11 [PubMed PMID: 25455396]
Devers BN, Douglas KC, Naik RD, Lee DH, Watson JT, Weikert DR. Outcomes of hook of hamate fracture excision in high-level amateur athletes. The Journal of hand surgery. 2013 Jan:38(1):72-6. doi: 10.1016/j.jhsa.2012.10.011. Epub 2012 Nov 30 [PubMed PMID: 23200952]
Level 2 (mid-level) evidenceBachoura A, Wroblewski A, Jacoby SM, Osterman AL, Culp RW. Hook of hamate fractures in competitive baseball players. Hand (New York, N.Y.). 2013 Sep:8(3):302-7. doi: 10.1007/s11552-013-9527-4. Epub [PubMed PMID: 24426938]
Wharton DM, Casaletto JA, Choa R, Brown DJ. Outcome following coronal fractures of the hamate. The Journal of hand surgery, European volume. 2010 Feb:35(2):146-9. doi: 10.1177/1753193408098907. Epub 2009 Mar 12 [PubMed PMID: 19282405]
Scheufler O, Kamusella P, Tadda L, Radmer S, Russo SG, Andresen R. High incidence of hamate hook fractures in underwater rugby players: diagnostic and therapeutic implications. Hand surgery : an international journal devoted to hand and upper limb surgery and related research : journal of the Asia-Pacific Federation of Societies for Surgery of the Hand. 2013:18(3):357-63. doi: 10.1142/S0218810413500391. Epub [PubMed PMID: 24156578]
Level 2 (mid-level) evidenceBlum AG, Zabel JP, Kohlmann R, Batch T, Barbara K, Zhu X, Dautel G, Dap F. Pathologic conditions of the hypothenar eminence: evaluation with multidetector CT and MR imaging. Radiographics : a review publication of the Radiological Society of North America, Inc. 2006 Jul-Aug:26(4):1021-44 [PubMed PMID: 16844930]
Chen NC, Jupiter JB, Jebson PJ. Sports-related wrist injuries in adults. Sports health. 2009 Nov:1(6):469-77 [PubMed PMID: 23015908]
Walsh JJ 4th, Bishop AT. Diagnosis and management of hamate hook fractures. Hand clinics. 2000 Aug:16(3):397-403, viii [PubMed PMID: 10955213]
Mouzopoulos G, Vlachos C, Karantzalis L, Vlachos K. Fractures of hamate: a clinical overview. Musculoskeletal surgery. 2019 Apr:103(1):15-21. doi: 10.1007/s12306-018-0543-y. Epub 2018 May 29 [PubMed PMID: 29845407]
Level 3 (low-level) evidenceO'Shea K, Weiland AJ. Fractures of the hamate and pisiform bones. Hand clinics. 2012 Aug:28(3):287-300, viii. doi: 10.1016/j.hcl.2012.05.010. Epub [PubMed PMID: 22883867]
Xiong G, Dai L, Zheng W, Sun Y, Tian G. Clinical classification and treatment strategy of hamate hook fracture. Journal of Huazhong University of Science and Technology. Medical sciences = Hua zhong ke ji da xue xue bao. Yi xue Ying De wen ban = Huazhong keji daxue xuebao. Yixue Yingdewen ban. 2010 Dec:30(6):762-6. doi: 10.1007/s11596-010-0654-7. Epub 2010 Dec 22 [PubMed PMID: 21181368]
Level 2 (mid-level) evidenceCockenpot E, Lefebvre G, Demondion X, Chantelot C, Cotten A. Imaging of Sports-related Hand and Wrist Injuries: Sports Imaging Series. Radiology. 2016 Jun:279(3):674-92. doi: 10.1148/radiol.2016150995. Epub [PubMed PMID: 27183404]
Andresen R, Radmer S, Sparmann M, Bogusch G, Banzer D. Imaging of hamate bone fractures in conventional X-rays and high-resolution computed tomography. An in vitro study. Investigative radiology. 1999 Jan:34(1):46-50 [PubMed PMID: 9888053]
Suh N, Ek ET, Wolfe SW. Carpal fractures. The Journal of hand surgery. 2014 Apr:39(4):785-91; quiz 791. doi: 10.1016/j.jhsa.2013.10.030. Epub [PubMed PMID: 24679911]
Andresen R, Radmer S, Scheufler O, Adam C, Bogusch G. [Optimization of conventional X-ray images for the detection of hook of hamate fractures]. Rontgenpraxis; Zeitschrift fur radiologische Technik. 2006:56(2):59-65 [PubMed PMID: 16733997]
Stark HH, Chao EK, Zemel NP, Rickard TA, Ashworth CR. Fracture of the hook of the hamate. The Journal of bone and joint surgery. American volume. 1989 Sep:71(8):1202-7 [PubMed PMID: 2777848]
Whalen JL, Bishop AT, Linscheid RL. Nonoperative treatment of acute hamate hook fractures. The Journal of hand surgery. 1992 May:17(3):507-11 [PubMed PMID: 1613233]
Eder C, Scheller A, Schwab N, Krapohl BD. Hamate's coronal fracture: diagnostic and therapeutic approaches based on a long-term follow-up. GMS Interdisciplinary plastic and reconstructive surgery DGPW. 2019:8():Doc05. doi: 10.3205/iprs000131. Epub 2019 Mar 29 [PubMed PMID: 30984513]
Heo YM, Kim SB, Yi JW, Lee JB, Park CY, Yoon JY, Kim DH. Evaluation of associated carpal bone fractures in distal radial fractures. Clinics in orthopedic surgery. 2013 Jun:5(2):98-104. doi: 10.4055/cios.2013.5.2.98. Epub 2013 May 15 [PubMed PMID: 23730472]
Level 2 (mid-level) evidenceTolat AR, Humphrey JA, McGovern PD, Compson J. Surgical excision of ununited hook of hamate fractures via the carpal tunnel approach. Injury. 2014 Oct:45(10):1554-6. doi: 10.1016/j.injury.2014.05.008. Epub 2014 May 17 [PubMed PMID: 24933442]
Wu WB,Du YF,Wang HX,Liang F, Bennett fracture combined with hamate fracture: carpometacarpal joint [PubMed PMID: 37301961]