Introduction
The saphenous nerve block has wide use in both the emergency department and perioperative settings for procedural anesthesia and post-procedural pain management. This regional anesthesia procedure is often used to block pain from the medial leg and ankle and can be performed with ultrasound guidance.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
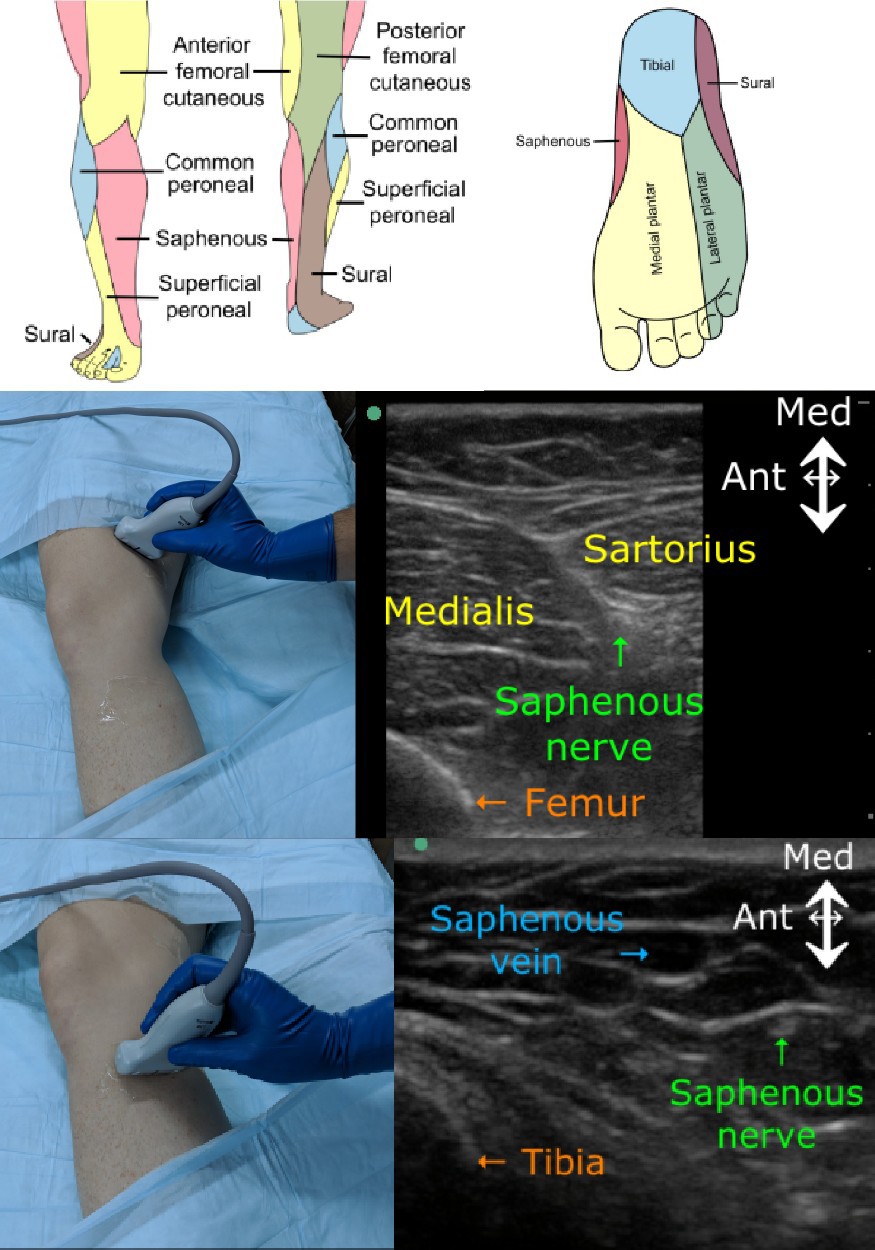
The saphenous nerve originates from the L3-L4 nerve roots and is a terminal branch of the femoral nerve. This purely sensory nerve innervates the medial, anteromedial, and posteromedial lower leg, ankle, and foot (Figure 1 and Figure 2).[1] It separates from the femoral nerve in the proximal third of the thigh, descends lateral to the femoral sheath in the adductor canal (a.k.a. subsartorial canal, Hunter canal), and crosses anteromedial to the femoral artery to emerge from the canal with the saphenous branch of the descending genicular artery.
After the saphenous nerve leaves the adductor canal, it pierces the fascia lata between the tendons of the gracilis and sartorius muscles to become subcutaneous. During this course, the nerve divides into the infrapatellar branch and the sartorial branch before dividing into multiple small subcutaneous branches. It travels laterally to the great saphenous vein as it descends the medial aspect of the lower leg, dividing into multiple small subcutaneous branches that provide sensory innervation to the medial aspect of the lower leg, ankle, and forefoot[2][3][4][5]
Indications
The saphenous nerve block is indicated whenever the need exists for anesthesia of the lower leg or foot along its neural distribution. It is most commonly used in conjunction with a popliteal sciatic nerve block to provide complete anesthesia of the lower leg for various surgical and nonsurgical procedures. These include saphenous vein stripping or harvesting, wound repair or exploration, ankle fracture or dislocation reduction, abscess drainage, and foreign body removal.
Contraindications
Absolute contraindications to the saphenous nerve block include allergy to anesthetic solution or additives, infection at the injection site, and patient refusal. Relative contraindications include coagulopathy, systemic infection, and pre-existing neurologic deficit in the distribution of the block.
Equipment
The necessary equipment includes the following:
- Antiseptic solution (povidone iodine or chlorhexidine gluconate)
- Sterile gloves
- Sterile drape
- Face mask with eye shield
- A linear ultrasound transducer (8-14 MHz) with sterile probe cover and gel
- Local anesthetic, lidocaine 1%, for superficial numbing
- Regional block local anesthetic, bupivacaine 0.5% or ropivacaine 0.5%
- 10 mL syringe
- 50-mm, 22-gauge short-bevel block needle
Personnel
A medical professional with training in ultrasound guidance for regional anesthesia should perform the block.
Preparation
The provider obtains informed consent in accordance with hospital policy. The patient should also undergo neurovascular and musculoskeletal examinations prior to the procedure.
Technique or Treatment
The saphenous nerve block can be performed at the mid-thigh in the adductor canal or just below the knee depending upon the desired area of anesthesia. Although these locations are identifiable anatomically, ultrasound visualization has become the standard of practice.
The adductor canal approach to saphenous nerve blockade provides anesthesia at the level of the mid-thigh. Patient placement is in the supine position with the leg abducted and externally rotated to allow access to the medial thigh. The patient is prepared in a standard sterile fashion. A linear ultrasound transducer is placed perpendicular to the long axis of the lower limb, approximately 5 to 7 cm proximal to the popliteal crease, and slid proximally until the hyperechoic appearance of the vastoadductor membrane fades, and the femoral artery is identified. The saphenous nerve is identified as a hyperechoic circle anterolateral to the femoral artery. After negative aspiration, an in-plane approach is used to inject 5 to 10 mL of local anesthetic deep to the sartorius muscle and lateral to the artery.[3][6][7]
The saphenous nerve can be blocked below the knee for anesthesia of the lower leg and foot. The patient is positioned supine with the leg straight. After standard sterile preparation, a linear ultrasound transducer is placed at the level of the tibial tuberosity. A short-axis view of the saphenous vein and fascia lata is obtained, and local anesthetic is infiltrated between these two landmarks[8]
Saphenous nerve blockade may also be achieved more distally at the ankle, although the nerve is often not visible with ultrasound at this level. For this reason, a landmark based approach is more reliable but may require higher volumes of local anesthetic. After palpating the medial malleolus and great saphenous vein, local anesthetic is infiltrated approximately 2 cm anterior and posterior to the saphenous vein just superior to the medial malleolus. Ultrasound guidance is helpful if the saphenous vein cannot be visualized or palpated on exam. However, the saphenous nerve usually is not visible on ultrasound at this level[9]
Complications
Complications related to saphenous nerve block may include pain on injection, infection at injection site, bleeding, nerve injury, allergic reaction, and local anesthetic systemic toxicity. There is some controversy as to whether or not adductor canal blocks may result in quadriceps muscle weakness as a result of secondary blockade of the vastus medialis nerve.[10] However, several studies have reported that the adductor canal block results in little or no quadriceps muscle weakness, particularly when compared with the femoral nerve block.[7][11][12][13][14] Ultrasound visualization minimizes the likelihood of nerve injury, local toxicity, and vessel puncture.
Complications must be recognized and treated early to avoid long-term morbidity. Patients with suspected systemic toxicity should immediately receive intravenous lipid emulsion (Intralipid) therapy. The dose is 20% lipid emulsion as a 1.5 mL/kg bolus over 2 to 3 minutes, followed by a 0.25 mL/kg/min infusion. Consider consulting your poison control center for guidance.
Clinical Significance
The saphenous nerve provides pure sensory innervation to the anteromedial aspect of the lower leg. Blockade of the saphenous nerve, particularly when performed under ultrasound guidance, offers a safe and reliable option for anesthesia of the lower extremity and may help reduce utilization of systemic therapy, such as opioids.
Enhancing Healthcare Team Outcomes
Performance of the saphenous nerve block requires interprofessional collaboration between the proceduralist, nursing staff, and clinical pharmacist. The patient should be on continuous hemodynamic monitoring and emergency airway equipment, supplemental oxygen, and resuscitation drugs (including lipid emulsion) kept immediately available. All team members should know the early symptoms of local anesthetic systemic toxicity (i.e., tinnitus, circumoral numbness, and metallic taste) and awake patients advised to report them. Early recognition and treatment are vital to avoid more severe complications including seizures and cardiovascular collapse. Providers should calculate the maximum weight-based dose of local before the start of the procedure and should use the lowest effective dosing to minimize the risk of systemic toxicity; this should include the clinician pharmacist in a collaborative effort. Nursing will assist in the procedure and provide patient monitoring, informing the clinician of any concerns that may arise. With an interprofessional approach to a saphenous nerve block, outcomes will be optimized.
Media
References
Marsland D, Dray A, Little NJ, Solan MC. The saphenous nerve in foot and ankle surgery: its variable anatomy and relevance. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2013 Jun:19(2):76-9. doi: 10.1016/j.fas.2012.10.007. Epub 2012 Dec 27 [PubMed PMID: 23548446]
Horn JL, Pitsch T, Salinas F, Benninger B. Anatomic basis to the ultrasound-guided approach for saphenous nerve blockade. Regional anesthesia and pain medicine. 2009 Sep-Oct:34(5):486-9. doi: 10.1097/AAP.0b013e3181ae11af. Epub [PubMed PMID: 19920424]
Level 2 (mid-level) evidenceMarian AA, Ranganath Y, Bayman EO, Senasu J, Brennan TJ. A Comparison of 2 Ultrasound-Guided Approaches to the Saphenous Nerve Block: Adductor Canal Versus Distal Transsartorial: A Prospective, Randomized, Blinded, Noninferiority Trial. Regional anesthesia and pain medicine. 2015 Sep-Oct:40(5):623-30. doi: 10.1097/AAP.0000000000000277. Epub [PubMed PMID: 26110441]
Level 1 (high-level) evidenceManickam B, Perlas A, Duggan E, Brull R, Chan VW, Ramlogan R. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Regional anesthesia and pain medicine. 2009 Nov-Dec:34(6):578-80 [PubMed PMID: 19916251]
Level 2 (mid-level) evidenceWalter WR, Burke CJ, Adler RS. Ultrasound-guided therapeutic injections for neural pathology about the foot and ankle: a 4 year retrospective review. Skeletal radiology. 2017 Jun:46(6):795-803. doi: 10.1007/s00256-017-2624-7. Epub 2017 Mar 16 [PubMed PMID: 28303298]
Level 2 (mid-level) evidenceKrombach J, Gray AT. Sonography for saphenous nerve block near the adductor canal. Regional anesthesia and pain medicine. 2007 Jul-Aug:32(4):369-70 [PubMed PMID: 17720129]
Level 3 (low-level) evidenceSaranteas T, Anagnostis G, Paraskeuopoulos T, Koulalis D, Kokkalis Z, Nakou M, Anagnostopoulou S, Kostopanagiotou G. Anatomy and clinical implications of the ultrasound-guided subsartorial saphenous nerve block. Regional anesthesia and pain medicine. 2011 Jul-Aug:36(4):399-402. doi: 10.1097/AAP.0b013e318220f172. Epub [PubMed PMID: 21697687]
Gray AT, Collins AB. Ultrasound-guided saphenous nerve block. Regional anesthesia and pain medicine. 2003 Mar-Apr:28(2):148; author reply 148 [PubMed PMID: 12677627]
Level 3 (low-level) evidenceFredrickson MJ, White R, Danesh-Clough TK. Low-volume ultrasound-guided nerve block provides inferior postoperative analgesia compared to a higher-volume landmark technique. Regional anesthesia and pain medicine. 2011 Jul-Aug:36(4):393-8. doi: 10.1097/AAP.0b013e31821e2fb7. Epub [PubMed PMID: 21610557]
Level 1 (high-level) evidenceThiranagama R. Nerve supply of the human vastus medialis muscle. Journal of anatomy. 1990 Jun:170():193-8 [PubMed PMID: 2254163]
Abdallah FW, Whelan DB, Chan VW, Prasad GA, Endersby RV, Theodoropolous J, Oldfield S, Oh J, Brull R. Adductor Canal Block Provides Noninferior Analgesia and Superior Quadriceps Strength Compared with Femoral Nerve Block in Anterior Cruciate Ligament Reconstruction. Anesthesiology. 2016 May:124(5):1053-64. doi: 10.1097/ALN.0000000000001045. Epub [PubMed PMID: 26938989]
Davis JJ, Bond TS, Swenson JD. Adductor canal block: more than just the saphenous nerve? Regional anesthesia and pain medicine. 2009 Nov-Dec:34(6):618-9. doi: 10.1097/AAP.0b013e3181bfbf00. Epub [PubMed PMID: 19901788]
Level 3 (low-level) evidenceJaeger P, Nielsen ZJ, Henningsen MH, Hilsted KL, Mathiesen O, Dahl JB. Adductor canal block versus femoral nerve block and quadriceps strength: a randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. Anesthesiology. 2013 Feb:118(2):409-15. doi: 10.1097/ALN.0b013e318279fa0b. Epub [PubMed PMID: 23241723]
Level 1 (high-level) evidenceKwofie MK, Shastri UD, Gadsden JC, Sinha SK, Abrams JH, Xu D, Salviz EA. The effects of ultrasound-guided adductor canal block versus femoral nerve block on quadriceps strength and fall risk: a blinded, randomized trial of volunteers. Regional anesthesia and pain medicine. 2013 Jul-Aug:38(4):321-5. doi: 10.1097/AAP.0b013e318295df80. Epub [PubMed PMID: 23788068]
Level 1 (high-level) evidence