Introduction
Blockade of the brachial plexus effectively provides anesthesia to the upper limb from the shoulder to the fingertips. Approaches to blocking the brachial plexus depend on the indication, planned surgery or procedure, patient-specific body habitus, medical comorbidities, and individual anatomical variants. This review addresses the indications, ultrasound probe placement, and sonoanatomy for the ultrasound-guided interscalene block, superior trunk block, supraclavicular brachial plexus block, infraclavicular brachial plexus block, and axillary brachial plexus block.[1][2][3]
It is well established that brachial plexus blocks provide superior postoperative pain management compared to general anesthesia alone. Using catheter-based continuous infusions for brachial plexus blocks is superior to single-injection brachial plexus blocks for decreasing perioperative pain scores and opioid consumption requirements for various upper extremity surgeries.[4][5] Intraoperative intra-articular shoulder infiltration is generally less effective than preoperative brachial plexus blocks.[6]
While there may be some cost-saving aspects to using brachial plexus blocks as the sole anesthetic compared to general anesthesia, this is only true if there is no need to utilize general anesthesia as a rescue technique. This emphasizes the supreme importance of successful block placement and management in maintaining cost-efficient practices.[7]
Exact needle placement is vital for successful block delivery. The choice and placement of the ultrasound probe are key factors in successfully using brachial plexus blocks. In addition, proper anatomic recognition is essential for successful ultrasound-guided brachial plexus blockade and patient safety.[8] Ultrasound-guided interscalene block requires a high-frequency linear transducer placed on the posterolateral aspect of the neck at an angle parallel to the skin surface, between the anterior and middle scalene muscles. A low-frequency curvilinear transducer can guide a supraclavicular block, while a curved array transducer can be used for infraclavicular and axillary blocks.
The anatomy of the brachial plexus comprises six anatomical structures: nerve roots, trunks, divisions, cords, and terminal branches.[9] The nerve roots are superimposed on the vertebral bodies in the posterior triangle, and their visualization depends upon proper probe positioning. When scanned in short axis orientation, the nerve appears hyperechoic with a hypoechoic background. The nerves are encased in connective tissue sheaths, which appear hypoechoic on ultrasound imaging.[10] These anatomical structures should be identified during an ultrasound-guided brachial plexus block procedure before injection.[11]
Identifying vascular structures, such as arterial vessels that traverse through or around neurovascular bundles during brachial plexus blockade, is essential.[12] Various color Doppler techniques may help identify vascular structures before needle insertion, especially during axillary blocks with a greater possibility of traversing vessels than other approaches.
In conclusion, blockade of the brachial plexus can provide significant postoperative pain relief in upper extremity surgery compared to general anesthesia alone. However, to ensure safety and efficacy, it is essential to have accurate knowledge of sonoanatomy and select the best approach based on patient characteristics. Furthermore, careful consideration must be given to needle placement and avoidance of vascular structures.[13]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The brachial plexus is formed from the C5 to T1 nerve roots. These roots join above the clavicle to form the superior (C5, C6), middle (C7), and inferior trunks (C8, T1). The trunks pass under and in close proximity to the clavicle; they can easily be blocked at this level. Distal to the clavicle, the trunks split into the lateral (C5 to C7), posterior (C5 to T1), and medial (C8, T1) cords, found adjacent to the axillary artery. Finally, the terminal nerve branches are formed from the cords in the axilla.
The median nerve is formed from the medial and lateral cords and is usually superficial to the axillary artery. The ulnar nerve is formed from the medial cord and is generally located lateral to the axillary artery. The radial nerve is located deep and lateral to the axillary artery. The last terminal branch, the musculocutaneous nerve, branches off from the lateral cord and pierces through the coracobrachialis in the proximal axilla.
The brachial plexus can be blocked at multiple sites for varying effects. Therefore, familiarizing oneself with multiple approaches given variant patient anatomy and indications is beneficial. The various brachial plexus blocks include:
- Interscalene
- Superior trunk, a potentially phrenic nerve-sparing alternative to the interscalene approach[14]
- Supraclavicular
- Infraclavicular
- Traditional
- Retrograde approach (RAPTIR)[15]
- Axillary
The interscalene block providing shoulder, arm, and forearm anesthesia is the most commonly used brachial plexus block. It is performed by injecting local anesthetic around the brachial plexus at the level of the nerve roots, which are located between the anterior and middle scalene muscles. The needle is inserted in a cephalad direction towards the neck until it contacts the bone.[3]
The supraclavicular block provides anesthesia and analgesia to the upper extremity below the shoulder. It is an excellent choice for elbow and hand surgery. This approach involves inserting a needle into the supraclavicular fossa just lateral to the clavicle. Local anesthetic can be injected around the brachial plexus at its junction with the subclavian artery.[16]
The infraclavicular block is used for procedures involving the lower arm and hand. This approach involves inserting a needle into a depression just medial to the scapular coracoid process, where local anesthetic can be injected around the brachial plexus at its junction with the axillary artery.[17] The retrograde approach for an infraclavicular block (RAPTIR) utilizes ultrasound guidance to identify individual nerve branches within the proximal axilla; this allows selective blockade of individual nerves or combinations thereof.[18]
The traditional axillary block is used for procedures involving lower arm and hand nerves. This approach involves inserting a needle into the axilla in line with the humerus, where local anesthetic can be injected around the brachial plexus at its junction with the axillary artery.[11]
Indications
Interscalene Brachial Plexus Block
The interscalene block provides analgesia or surgical anesthesia to the upper limb from the distal end of the clavicle to the shoulder joint and proximal humerus.[12]
Superior Trunk Block
The superior trunk block is a potentially phrenic nerve-sparing modification of the interscalene block that provides analgesia to the shoulder capsule and proximal humerus.[14][19]
Supraclavicular Brachial Plexus Block
The supraclavicular block provides analgesia or surgical anesthesia from the mid-humerus to the fingertips.[20]
Infraclavicular Brachial Plexus Block
This block provides analgesia or surgical anesthesia from the mid-humerus to the fingertips but typically spares the intercostobrachial nerve. The infraclavicular block can be performed via a traditional approach with a steep needle angle or retroclavicular approach (RAPTIR).[15]
Axillary Brachial Plexus Block
The axillary block provides analgesia or surgical anesthesia from the mid-humerus to the fingertips. This block also spares the intercostobrachial nerve, although that nerve is easily blocked within the same window.[21][14][22]
Contraindications
All brachial plexus blocks are contraindicated if there is active cellulitis or an abscess at the injection site, or a known allergy to the local anesthetic.[23] Patients may always choose not to undergo the procedure. Other contraindications specific to certain blocks are noted below.
Interscalene brachial plexus blocks are contraindicated in certain pulmonary and cardiac diseases. Morbid obesity may be a relative contraindication, as respiratory insufficiency can result from hemidiaphragmatic paralysis.[24]
Superior trunk blocks have the same contraindications as interscalene blocks, although phrenic nerve palsy is felt to occur less frequently. The dorsal scapular nerve travels through the middle scalene near the typical injection site.[25]
Supraclavicular brachial plexus blocks should be used cautiously in patients with poor pulmonary reserve, as any resulting pneumothorax may significantly worsen their respiratory status. An example of this relative contraindication is known pneumonia on the contralateral side.[26]
Axillary brachial plexus blocks should not be performed if there is an inability to visualize the needle path through the highly vascular region.[16]
Equipment
The same equipment is needed for all the listed approaches to the brachial plexus block.[27] This equipment includes:
- High-frequency (more than 10 MHz) linear ultrasound probe
- Chlorhexidine 2% or povidone-iodine skin disinfectant solution
- Local anesthetic; for longer duration blocks, bupivacaine 0.5% or ropivacaine 0.5%; for shorter blocks, lidocaine 2% or mepivacaine 1.5%
- A 10 mL to 20 mL syringe with extension tubing
- Short bevel block needle (10 cm, 18 to 22 G)
- Sterile ultrasound probe cover
- Sterile ultrasound gel
- Standard vital sign monitoring equipment (noninvasive blood pressure and rhythm monitoring, with or without pulse oximetry)
Personnel
A provider trained in ultrasound-guided regional anesthesia is necessary. Additional personnel (nurse, another clinician) must actively monitor patient status and administer rescue medications if needed.
Preparation
Before performing any brachial plexus block, a description of the risks, benefits, and alternatives to the procedure before obtaining informed consent. The skin over the injection site should be cleansed with chlorhexidine 2% or povidone-iodine and allowed to dry. The sterile gel should be applied to the probe; then, a sterile probe cover should be placed with additional sterile gel on the exterior surface of the probe cover. Draw up the desired volume of local anesthetic into a syringe, then connect the extension tubing with a short bevel block needle attached. Prime the tubing and needle by ejecting all of the air from the system, as injecting air into the site will inhibit insonation.[28]
For the interscalene, superior trunk, supraclavicular, and RAPTIR infraclavicular approaches, the patient should be supine with the head and neck rotated slightly toward the contralateral side. A towel roll may be used under the ipsilateral shoulder to allow more room for needle manipulation. The ipsilateral arm should be adducted.[29]
For the traditional infraclavicular and axillary approaches, the patient should be supine with the head and neck rotated slightly toward the contralateral side. The ipsilateral shoulder may be abducted to 90 degrees with the elbow flexed to increase visualization of the axillary artery and facilitate needle passage.[3]
Technique or Treatment
Interscalene Brachial Plexus Block
- Place the ultrasound probe in the supraclavicular fossa in a transverse orientation, aimed caudad relative to the thoracic cavity, to visualize the brachial plexus near the subclavian artery. Once identified, follow the plexus cephalad; it is found in the interscalene groove.[28]
- At the interscalene groove, the plexus is typically seen as multiple anechoic circular structures with a "stoplight" appearance. Typically, the topmost structure is C5, while the middle and lower structures are both divisions of C6.
- Use the color Doppler to identify any vascular structures in the needle path.
- Insert a block needle in-plane from posterior to anterior and lateral to medial toward the interscalene groove. Be cautious not to advance the needle between any of the hypoechoic nerve roots.
- Once the needle tip is in the groove, confirm the tip is not intravascular by negative aspiration.
- Inject 1 mL to 2 mL of a local anesthetic to verify tip placement and spread of local anesthetic into the interscalene groove, causing spread around the nerve roots.
- Once the placement is confirmed, repeat incremental injection and negative aspiration until an adequate spread of local anesthetic has occurred. Typically the volume is between 10 mL to 30 mL.
Superior Trunk Block
- Place the ultrasound probe in the supraclavicular fossa in a transverse orientation, aimed caudad relative to the thoracic cavity, to visualize the brachial plexus near the subclavian artery. Once identified, follow the plexus cephalad, where it is found in the interscalene groove.[30]
- Scan caudad, following the C5 and C6 roots to where they appear joined as the superior trunk. Ideally, this location should be proximal to where the suprascapular nerve branches.
- Identify the dorsal scapular nerve as it courses through the middle scalene muscle to avoid it during needle passage.
- Use the color Doppler to identify any vascular structures in the needle path.
- Insert a block needle in-plane from posterior to anterior and lateral to medial toward the superior trunk.
- Once the needle tip is deep relative to the superior trunk, confirm it is not intravascular by negative aspiration.
- Inject 1 mL to 2 mL of a local anesthetic to verify tip placement and spread of local anesthetic adjacent to the superior trunk.
- Once the placement is confirmed, repeat incremental injection and negative aspiration until an adequate spread of local anesthetic has occurred. Typically this volume is about 10 mL.
Supraclavicular Brachial Plexus Block
- Place the ultrasound probe in the supraclavicular fossa in a transverse orientation, aimed caudad relative to the thoracic cavity, to visualize the brachial plexus near the subclavian artery.[16]
- Visualize the visceral and parietal pleurae interface, seen as "lung sliding" on ultrasound. Additionally, visualize the first rib as a hyperechoic line with a dropout artifact deep relative to itself. The plexus and subclavian artery should be visualized overlying the first rib. This allows the first rib to be used as a bony backstop, decreasing the risk of pneumothorax. Rotating the lateral edge of the probe more posteriorly may aid in obtaining this window.
- Insert a block needle in-plane from posterior to anterior and lateral to medial, aiming for the deep portion of the brachial plexus where it overlies the first rib.
- Confirm negative aspiration, then inject a small amount of local anesthetic to raise the plexus of the first rib.
- Advance the needle along the first rib to the anterior aspect of the plexus, adjacent to the subclavian artery. This is called the "corner pocket." It is essential to completely cover this area for a successful block.
- Confirm negative aspiration, then inject another 1 mL to 2 mL of the local anesthetic. Repeat until about 10 mL has been injected deep relative to the plexus.
- Retract the needle to the skin, then readvance at a shallow angle, guiding the needle to the superficial aspect of the brachial plexus.
- Confirm negative aspiration, then inject 1 mL to 2 mL of local anesthetic superficial to the plexus. Repeat until about 10mL has been injected superficially relative to the plexus.
Infraclavicular Brachial Plexus Block via the Traditional Approach
- Place the ultrasound probe in the deltopectoral groove with the probe marker facing cephalad. The probe should be just caudad to the clavicle.[31]
- Identify the axillary artery and vein deep to the pectoralis major and pectoralis minor muscles. The vein is usually found lateral to the artery and is compressible and non-pulsatile. Doppler may be used to aid in identification.
- Using the color Doppler, identify the thoracoacromial artery and cephalic vein, as these may be within the needle path.
- The brachial plexus has split at this level into the lateral, posterior, and medial cords, typically found at 9, 6, and 3 o'clock, respectively. However, they are not always visible and need not be visualized for a successful block.
- Insert a block needle in-plane from cephalad to caudad and medial to lateral, starting just the caudad to the clavicle and aiming for the lateral aspect of the axillary artery. The needle trajectory is often quite steep, which may limit needle visualization.
- Aim the needle toward the 6 o'clock position deep relative to the axillary artery.
- Confirm negative aspiration, then inject 1 mL to 2 mL of a local anesthetic to visualize the spread of the local anesthetic deep relative to the artery.
- Repeat step six until the adequate spread of local anesthetic has been achieved. This is visualized as a 'U'-shaped spread of anesthetic along the lateral, posterior, and medial aspects of the axillary artery. Typically, a volume of 20 mL to 30 mL is required.
Infraclavicular Brachial Plexus Block via the Retrograde Approach
- Proceed with steps one to three of the traditional approach above.
- Starting just cephalad and posterior to the clavicle, insert a block needle in-plane from medial to lateral with the needle trajectory parallel to the ultrasound probe. Having the superior edge of the ultrasound probe slightly overlying the clavicle may help in orientation and needle guidance.[15]
- Visualize the needle passing under the clavicle and parallel to the probe. Aim toward the 6 o'clock position deep to the axillary artery.
- Confirm negative aspiration, then inject 1 mL to 2 mL of a local anesthetic to visualize the spread of the local anesthetic deep relative to the artery.
- Repeat step 4 until the adequate spread of local anesthetic has been achieved. This is visualized as a 'U'-shaped spread of anesthetic along the lateral, posterior, and medial aspects of the axillary artery. Typically, a volume of 20 mL to 30 mL is required.
Axillary Brachial Plexus Block
- Place the ultrasound probe in a transverse orientation in the axilla at the site where the pectoralis major inserts onto the humerus.[32]
- Scan distally and proximally to visualize the axillary artery, vein, and nerves surrounding the artery.
- The ideal ultrasound window should contain the musculocutaneous nerve seen piercing coracobrachialis and the teres major fasciotendinous insertion onto the humerus seen deep in the axillary artery.
- Color Doppler should be used to identify surrounding vasculature, as this area is highly vascular.
- Insert a block needle in-plane from anterior to posterior, parallel to the ultrasound probe.
- Advance the needle toward the musculocutaneous nerve (MCN).
- Confirm negative aspiration, then repeatedly inject 1 mL to 2 mL aliquots until adequate spread around the MCN is achieved.
- Retract and redirect the needle deep relative to the axillary artery.
- Confirm negative aspiration, then repeatedly inject 1 mL to 2 mL aliquots until adequate spread around the posterior aspect of the axillary artery is achieved.
- If the spread around the artery is inadequate, advance the needle under the artery toward the medial aspect and repeat step 9.
- Retract and redirect the needle superficial to the axillary artery.
- Repeat step nine to ensure the circumferential spread of the local anesthetic.
- An optional step to block the intercostobrachial nerve is to retract the needle to the skin and readvance between the skin and the muscle/fascia layer superficial to the axillary artery and plexus.
Complications
All nerve blocks risk nerve injuries such as neuropraxia or neurotmesis due to multiple factors, including inadvertent intraneural injection, local anesthetic neurotoxic properties, hematoma formation, and physical damage from the block needle. However, a recent systematic review found no association between the type of brachial plexus block and the peripheral nerve injury incidence.[33] Local anesthetic systemic toxicity should also be considered a complication for all nerve blocks. Before placing a nerve block, ensure that the total dose of local anesthetic to be injected is less than the theoretical toxic dose for the used anesthetic. Listed below are complications unique to each approach for brachial plexus blockade.[34][35]
The interscalene brachial plexus block may cause ipsilateral phrenic nerve palsy resulting in hemidiaphragmatic paralysis, vascular injury including vertebral artery puncture, Horner syndrome, subdural block, and injury to brachial plexus.
The superior trunk block may also cause ipsilateral phrenic nerve palsy, although at a possibly lower incidence than the interscalene block. Other complications include injury to the brachial plexus, surrounding vasculature, or the dorsal scapular nerve, which typically courses through the middle scalene muscle where the superior trunk inserts.
The supraclavicular brachial plexus block carries the clinically-significant risks of pneumothorax and subclavian arterial puncture. Ipsilateral hemidiaphragmatic paralysis is a known complication, but the risk is much lower than an interscalene block. In addition, ulnar nerve sparing may occur if full anesthetic spread is not achieved between the first rib and the plexus.
Complications of the infraclavicular brachial plexus block include injury to the brachial plexus, specifically the lateral and posterior cords, and injury to axillary vessels. Sparing of the medial cord may occur with the inadequate spread of local anesthetic around the axillary artery. In addition, the thoracoacromial artery and cephalic vein may lie in the needle path of the traditional approach.
The axillary brachial plexus block has virtually no risk of causing a pneumothorax. The color Doppler is recommended to avoid an inadvertent vascular puncture and injection resulting in local anesthetic systemic toxicity.[33]
Clinical Significance
Ultrasound-guided brachial plexus blocks can provide dense analgesia and anesthesia to the upper extremity from the shoulder to the fingers, depending on the indication and approach. Ultrasound has made these blocks more accessible and safer to perform. In addition, evidence suggests that ultrasound reduces the total volume of anesthetic required, decreases complications such as pneumothorax and vascular injury, and increases block success.
Interscalene brachial plexus blockade can be used to manage acute pain in proximal humerus and clavicular fractures and manage glenohumeral dislocations. It is effective as postoperative pain control and reduces opiate use in patients recovering from shoulder surgeries; this approach has been used as the sole anesthetic in shoulder arthroscopy.[36]
When performing an interscalene block for analgesia to the shoulder, there is a high risk of causing ipsilateral hemi-diaphragmatic paralysis via phrenic nerve palsy. Other approaches, such as a superior trunk block or a combined suprascapular and axillary nerve block, should be considered if phrenic nerve palsy is a concern. The superior trunk block potentially spares the diaphragm, but further research is needed to determine its efficacy.[14]
There are multiple approaches to block the brachial plexus distal to the interscalene groove, all of which result in anesthesia to the entire upper extremity from the mid humerus to the fingertips. The chosen approach depends on many factors, including the ability to position the patient appropriately, infection over the intended injection site, coagulopathy, operator experience, and variation in adjacent structures.[13]
The combined suprascapular and axillary nerve block is an intriguing alternative to regional anesthesia for shoulder surgery.[37] In patients requiring shoulder surgery, this approach may be preferable in patients with significant pulmonary disease, obstructive sleep apnea, or morbid obesity.
Among the supraclavicular, infraclavicular, and axillary blocks, a recent meta-analysis and systematic review found that all three have an equal likelihood of anesthetic success.[38]
Enhancing Healthcare Team Outcomes
Skills
Knowing how to perform a brachial plexus block is very useful as it allows the surgeon to perform a range of procedures on the ipsilateral arm. While an anesthesiologist usually performs a brachial plexus block, the nurse's role is vital. During the block, a nurse must observe the patient's vital signs for changes. Additionally, the nurse must frequently auscultate lung sounds to ensure that air entry is bilateral and equal; these procedures can be associated with a pneumothorax.[39] After the procedure, a portable x-ray is recommended to ensure no pneumothorax or diaphragmatic elevation.[40] Adept anesthesia providers can confirm the presence or absence of pneumothorax and elevated diaphragm in real-time via ultrasound, which is both sensitive and specific and avoids delays in diagnosis.[41]
Strategy
It is most appropriate and ideal to maintain continuous closed-loop communication between all members of the perioperative care team regarding the need, technique, and potential management issues associated with the brachial plexus block utilized.
Ethics
It is necessary to obtain thorough and comprehensive informed consent from either the patient or patients without the capacity to consent from their designated and authorized decision maker before placing any brachial plexus block. It is most appropriate for all team members to feel empowered to state any concerns they might have regarding the process, as this ensures buy-in from all stakeholders and provides additional layers of review and insight into any problematic matters as soon as possible.
Responsibilities
All team members must communicate their concerns, responsibilities, and activities with all other team members contemporaneously and as indicated throughout the perioperative period, based on their professional discretion.
Interprofessional Communication
All team members should respect the free flow of information and concerns among team members without allowing or producing an environment of hostility.
Care Coordination
All interprofessional team members should consider it their duty to neither disrupt the work done by other team members nor to, through their actions or inaction, create additional issues or increase the workload for other team members. [Level 5]
Media
(Click Image to Enlarge)
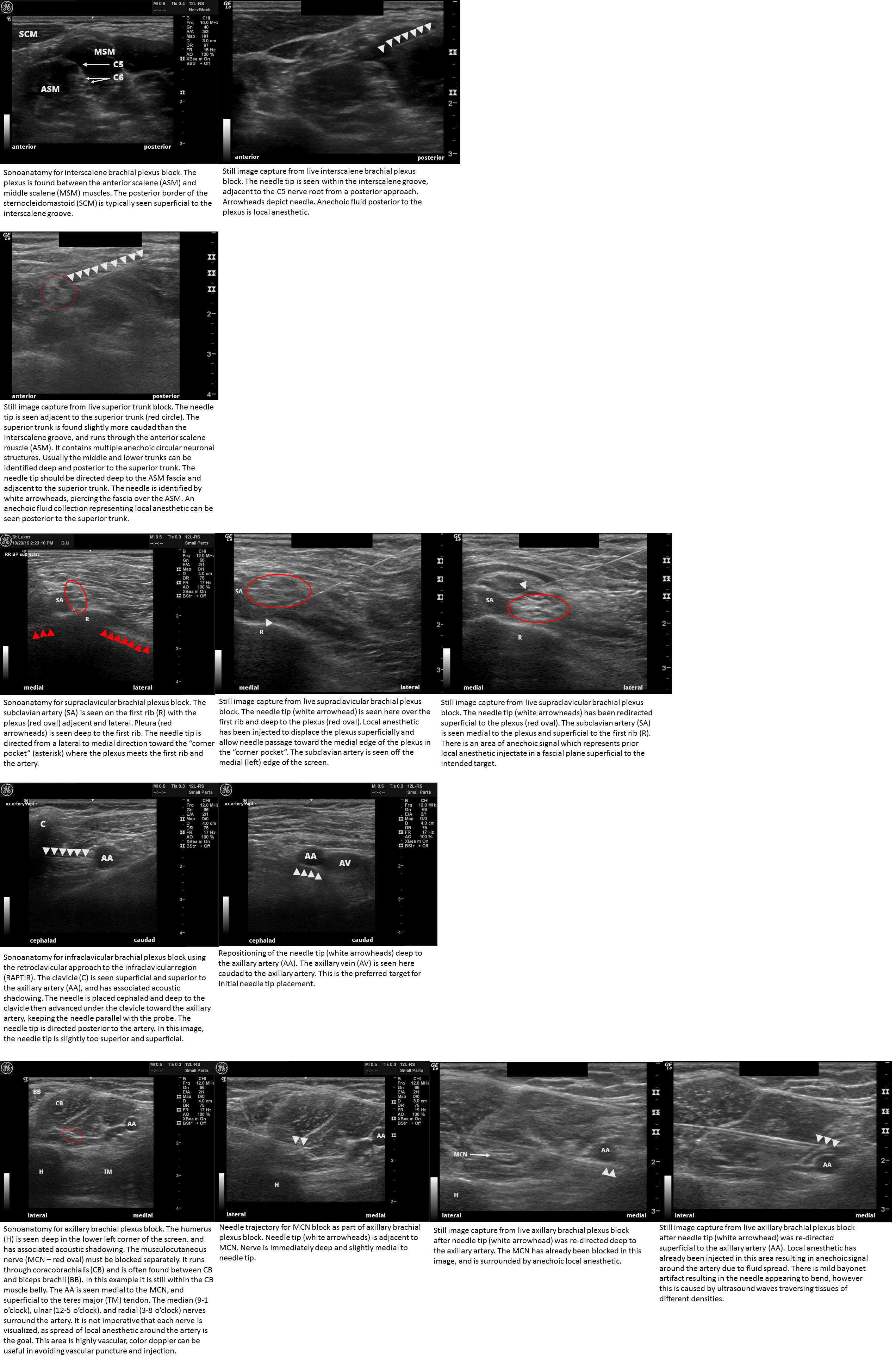
Sonoanatomy and needle placement for ultrasound guided brachial plexus blocks Includes interscalene brachial plexus block, superior trunk block, supraclavicular brachial plexus block, infraclavicular brachial plexus block (retroclavicular approach - RAPTIR), and axillary brachial plexus blocks Contributed by John Pester, DO
References
Gomide LC, Ruzi RA, Mandim BLS, Dias VADR, Freire RHD. Prospective study of ultrasound-guided peri-plexus interscalene block with continuous infusion catheter for arthroscopic rotator cuff repair and postoperative pain control. Revista brasileira de ortopedia. 2018 Nov-Dec:53(6):721-727. doi: 10.1016/j.rboe.2017.08.020. Epub 2018 Feb 3 [PubMed PMID: 30377606]
Dai W, Tang M, He K. The effect and safety of dexmedetomidine added to ropivacaine in brachial plexus block: A meta-analysis of randomized controlled trials. Medicine. 2018 Oct:97(41):e12573. doi: 10.1097/MD.0000000000012573. Epub [PubMed PMID: 30313043]
Level 1 (high-level) evidenceMojica JJ, Ocker A, Barrata J, Schwenk ES. Anesthesia for the Patient Undergoing Shoulder Surgery. Clinics in sports medicine. 2022 Apr:41(2):219-231. doi: 10.1016/j.csm.2021.11.004. Epub [PubMed PMID: 35300836]
Kalthoff A, Sanda M, Tate P, Evanson K, Pederson JM, Paranjape GS, Patel PD, Sheffels E, Miller R, Gupta A. Peripheral Nerve Blocks Outperform General Anesthesia for Pain Control in Arthroscopic Rotator Cuff Repair: A Systematic Review and Meta-analysis. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2022 May:38(5):1627-1641. doi: 10.1016/j.arthro.2021.11.054. Epub 2021 Dec 21 [PubMed PMID: 34952185]
Level 1 (high-level) evidenceBoin MA, Mehta D, Dankert J, Umeh UO, Zuckerman JD, Virk MS. Anesthesia in Total Shoulder Arthroplasty: A Systematic Review and Meta-Analysis. JBJS reviews. 2021 Nov 10:9(11):. doi: 10.2106/JBJS.RVW.21.00115. Epub 2021 Nov 10 [PubMed PMID: 34757963]
Level 1 (high-level) evidenceYung EM, Got TC, Patel N, Brull R, Abdallah FW. Intra-articular infiltration analgesia for arthroscopic shoulder surgery: a systematic review and meta-analysis. Anaesthesia. 2021 Apr:76(4):549-558. doi: 10.1111/anae.15172. Epub 2020 Jun 29 [PubMed PMID: 32596840]
Level 1 (high-level) evidenceMarhofer P, Kraus M, Marhofer D. [Regional anesthesia in daily clinical practice: an economic analysis based on case vignettes]. Der Anaesthesist. 2019 Dec:68(12):827-835. doi: 10.1007/s00101-019-00691-8. Epub 2019 Nov 5 [PubMed PMID: 31690960]
Level 3 (low-level) evidenceJones MR, Novitch MB, Sen S, Hernandez N, De Haan JB, Budish RA, Bailey CH, Ragusa J, Thakur P, Orhurhu V, Urits I, Cornett EM, Kaye AD. Upper extremity regional anesthesia techniques: A comprehensive review for clinical anesthesiologists. Best practice & research. Clinical anaesthesiology. 2020 Mar:34(1):e13-e29. doi: 10.1016/j.bpa.2019.07.005. Epub 2019 Jul 20 [PubMed PMID: 32334792]
Li J, Szabova A. Ultrasound-Guided Nerve Blocks in the Head and Neck for Chronic Pain Management: The Anatomy, Sonoanatomy, and Procedure. Pain physician. 2021 Dec:24(8):533-548 [PubMed PMID: 34793642]
Mejia J, Iohom G, Cuñat T, Flò Csefkó M, Arias M, Fervienza A, Sala-Blanch X. Accuracy of ultrasonography predicting spread location following intraneural and subparaneural injections: a scoping review. Minerva anestesiologica. 2022 Mar:88(3):166-172. doi: 10.23736/S0375-9393.21.16041-9. Epub 2022 Jan 24 [PubMed PMID: 35072434]
Level 2 (mid-level) evidenceKim TY, Hwang JT. Regional nerve blocks for relieving postoperative pain in arthroscopic rotator cuff repair. Clinics in shoulder and elbow. 2022 Dec:25(4):339-346. doi: 10.5397/cise.2022.01263. Epub 2022 Nov 24 [PubMed PMID: 36475301]
Liu Z, Li YB, Wang JH, Wu GH, Shi PC. Efficacy and adverse effects of peripheral nerve blocks and local infiltration anesthesia after arthroscopic shoulder surgery: A Bayesian network meta-analysis. Frontiers in medicine. 2022:9():1032253. doi: 10.3389/fmed.2022.1032253. Epub 2022 Nov 10 [PubMed PMID: 36438028]
Level 1 (high-level) evidenceOmura Y, Kono S, Nakayama T, Okabe M, Kadono Y. Low-Concentration Brachial Plexus Block. The Journal of hand surgery. 2022 Aug 4:():. pii: S0363-5023(22)00332-X. doi: 10.1016/j.jhsa.2022.06.006. Epub 2022 Aug 4 [PubMed PMID: 35934588]
Zisquit J, Nedeff N. Interscalene Block. StatPearls. 2023 Jan:(): [PubMed PMID: 30137775]
Luftig J, Mantuani D, Herring AA, Nagdev A. Ultrasound-guided retroclavicular approach infraclavicular brachial plexus block for upper extremity emergency procedures. The American journal of emergency medicine. 2017 May:35(5):773-777. doi: 10.1016/j.ajem.2017.01.028. Epub 2017 Jan 15 [PubMed PMID: 28126454]
Steen-Hansen C, Madsen MH, Lange KHW, Lundstrøm LH, Rothe C. Single injection combined suprascapular and axillary nerve block: A randomised controlled non-inferiority trial in healthy volunteers. Acta anaesthesiologica Scandinavica. 2023 Jan:67(1):104-111. doi: 10.1111/aas.14147. Epub 2022 Oct 1 [PubMed PMID: 36069505]
Level 1 (high-level) evidenceŞeyhanlı İ, Duran M, Yılmaz N, Nakır H, Doğukan M, Uludağ Ö. Investigation of infraclavicular block success using the perfusion index: A randomized clinical trial. Biomolecules and biomedicine. 2023 May 1:23(3):496-501. doi: 10.17305/bjbms.2022.8214. Epub 2023 May 1 [PubMed PMID: 36321618]
Level 1 (high-level) evidenceYu M, Shalaby M, Luftig J, Cooper M, Farrow R. Ultrasound-Guided Retroclavicular Approach to the Infraclavicular Region (RAPTIR) Brachial Plexus Block for Anterior Shoulder Reduction. The Journal of emergency medicine. 2022 Jul:63(1):83-87. doi: 10.1016/j.jemermed.2022.04.011. Epub 2022 Aug 4 [PubMed PMID: 35934656]
Jo Y, Oh C, Lee WY, Chung HJ, Park J, Kim YH, Ko Y, Chung W, Hong B. Randomised comparison between superior trunk and costoclavicular blocks for arthroscopic shoulder surgery: A noninferiority study. European journal of anaesthesiology. 2022 Oct 1:39(10):810-817. doi: 10.1097/EJA.0000000000001735. Epub 2022 Aug 17 [PubMed PMID: 35975762]
Level 1 (high-level) evidenceGeorgiadis PL, Vlassakov KV, Patton ME, Lirk PB, Janfaza DR, Zeballos JL, Quaye AN, Patel V, Schreiber KL. Ultrasound-guided supraclavicular vs. retroclavicular block of the brachial plexus: comparison of ipsilateral diaphragmatic function: A randomised clinical trial. European journal of anaesthesiology. 2021 Jan:38(1):64-72. doi: 10.1097/EJA.0000000000001305. Epub [PubMed PMID: 32925256]
Level 1 (high-level) evidenceChandrasoma J, Harrison TK, Ching H, Vokach-Brodsky L, Chu LF. Peripheral Nerve Blocks for Hand Procedures. The New England journal of medicine. 2018 Sep 6:379(10):e15. doi: 10.1056/NEJMvcm1400191. Epub [PubMed PMID: 30184448]
D'Souza RS, Johnson RL. Supraclavicular Block. StatPearls. 2023 Jan:(): [PubMed PMID: 30085598]
Langlois PL, Gil-Blanco AF, Jessop D, Sansoucy Y, D'Aragon F, Albert N, Echave P. Retroclavicular approach vs infraclavicular approach for plexic bloc anesthesia of the upper limb: study protocol randomized controlled trial. Trials. 2017 Jul 21:18(1):346. doi: 10.1186/s13063-017-2086-1. Epub 2017 Jul 21 [PubMed PMID: 28732521]
Level 1 (high-level) evidenceNational Guideline Centre (UK). Evidence review for anaesthesia for shoulder replacement: Joint replacement (primary): hip, knee and shoulder: Evidence review F. 2020 Jun:(): [PubMed PMID: 32881468]
Frederico TN, Sakata RK, Falc O LFDR, de Sousa PCRCB, Melhmann F, Sim Es CA, Ferraro LHC. An alternative approach for blocking the superior trunk of the brachial plexus evaluated by a single arm clinical trial. Brazilian journal of anesthesiology (Elsevier). 2022 Nov-Dec:72(6):774-779. doi: 10.1016/j.bjane.2020.10.015. Epub 2021 Feb 17 [PubMed PMID: 36357056]
Tran DQ, Elgueta MF, Aliste J, Finlayson RJ. Diaphragm-Sparing Nerve Blocks for Shoulder Surgery. Regional anesthesia and pain medicine. 2017 Jan/Feb:42(1):32-38. doi: 10.1097/AAP.0000000000000529. Epub [PubMed PMID: 27941477]
Dong X, Wu CL, YaDeau JT. Clinical care pathways for ambulatory total shoulder arthroplasty. Current opinion in anaesthesiology. 2022 Oct 1:35(5):634-640. doi: 10.1097/ACO.0000000000001174. Epub 2022 Aug 9 [PubMed PMID: 35943122]
Level 3 (low-level) evidenceKim HJ, Baek JH, Park S, Yoon JU, Byeon GJ, Shin SW. Comparison of Continuous and Programmed Intermittent Bolus Infusion of 0.2% Ropivacaine after Ultrasound-Guided Continuous Interscalene Brachial Plexus Block in Arthroscopic Shoulder Surgery. Pain research & management. 2022:2022():2010224. doi: 10.1155/2022/2010224. Epub 2022 Dec 26 [PubMed PMID: 36601435]
Bian WG, Zhou RH, Liu HL, Luo HG. Elevated cervical shoulder position and traditional supine position in the ultrasound-guided brachial plexus block: A randomized controlled trial. Asian journal of surgery. 2022 Nov:45(11):2300-2301. doi: 10.1016/j.asjsur.2022.05.019. Epub 2022 May 18 [PubMed PMID: 35597746]
Level 1 (high-level) evidenceSivakumar RK, Samy W, Pakpirom J, Songthamwat B, Karmakar MK. Ultrasound-guided selective trunk block: Evaluation of ipsilateral sensorimotor block dynamics, hemidiaphragmatic function and efficacy for upper extremity surgery. A single-centre cohort study. European journal of anaesthesiology. 2022 Oct 1:39(10):801-809. doi: 10.1097/EJA.0000000000001736. Epub 2022 Aug 11 [PubMed PMID: 35950709]
Areeruk P, Karmakar MK, Reina MA, Mok LYH, Sivakumar RK, Sala-Blanch X. High-definition ultrasound imaging defines the paraneural sheath and fascial compartments surrounding the cords of the brachial plexus at the costoclavicular space and lateral infraclavicular fossa. Regional anesthesia and pain medicine. 2021 Jun:46(6):500-506. doi: 10.1136/rapm-2020-102304. Epub 2021 Apr 2 [PubMed PMID: 33811182]
Sanchez A, Chrusciel J, Cimino Y, Nguyen M, Guinot PG, Sanchez S, Bouhemad B. Evaluation of Monitored Anesthesia Care Involving Sedation and Axillary Nerve Block for Day-Case Hand Surgery. Healthcare (Basel, Switzerland). 2022 Feb 7:10(2):. doi: 10.3390/healthcare10020313. Epub 2022 Feb 7 [PubMed PMID: 35206928]
Level 3 (low-level) evidenceSilverstein ML, Tevlin R, Higgins KE, Pedreira R, Curtin C. Peripheral Nerve Injury After Upper-Extremity Surgery Performed Under Regional Anesthesia: A Systematic Review. Journal of hand surgery global online. 2022 Jul:4(4):201-207. doi: 10.1016/j.jhsg.2022.04.011. Epub 2022 Jun 4 [PubMed PMID: 35880155]
Level 1 (high-level) evidenceNelson M, Reens A, Reda L, Lee D. Profound Prolonged Bradycardia and Hypotension after Interscalene Brachial Plexus Block with Bupivacaine. The Journal of emergency medicine. 2018 Mar:54(3):e41-e43. doi: 10.1016/j.jemermed.2017.12.004. Epub 2017 Dec 30 [PubMed PMID: 29295799]
Hussain N, Goldar G, Ragina N, Banfield L, Laffey JG, Abdallah FW. Suprascapular and Interscalene Nerve Block for Shoulder Surgery: A Systematic Review and Meta-analysis. Anesthesiology. 2017 Dec:127(6):998-1013. doi: 10.1097/ALN.0000000000001894. Epub [PubMed PMID: 28968280]
Level 1 (high-level) evidenceDoğan AT, Coşarcan SK, Gürkan Y, Koyuncu Ö, Erçelen Ö, Demirhan M. Comparison of anterior suprascapular nerve block versus interscalane nerve block in terms of diaphragm paralysis in arthroscopic shoulder surgery: a prospective randomized clinical study. Acta orthopaedica et traumatologica turcica. 2022 Nov:56(6):389-394. doi: 10.5152/j.aott.2022.22044. Epub [PubMed PMID: 36567542]
Level 1 (high-level) evidenceSun C, Zhang X, Ji X, Yu P, Cai X, Yang H. Suprascapular nerve block and axillary nerve block versus interscalene nerve block for arthroscopic shoulder surgery: A meta-analysis of randomized controlled trials. Medicine. 2021 Nov 5:100(44):e27661. doi: 10.1097/MD.0000000000027661. Epub [PubMed PMID: 34871240]
Level 1 (high-level) evidenceCasas-Arroyave FD, Ramírez-Mendoza E, Ocampo-Agudelo AF. Complications associated with three brachial plexus blocking techniques: Systematic review and meta-analysis. Revista espanola de anestesiologia y reanimacion. 2021 Aug-Sep:68(7):392-407. doi: 10.1016/j.redare.2020.10.003. Epub 2021 Jul 20 [PubMed PMID: 34294596]
Level 1 (high-level) evidenceWright I. Peripheral nerve blocks in the outpatient surgery setting. AORN journal. 2011 Jul:94(1):59-74; quiz 75-7. doi: 10.1016/j.aorn.2011.02.011. Epub [PubMed PMID: 21722772]
Visoiu M, Joy LN, Grudziak JS, Chelly JE. The effectiveness of ambulatory continuous peripheral nerve blocks for postoperative pain management in children and adolescents. Paediatric anaesthesia. 2014 Nov:24(11):1141-8. doi: 10.1111/pan.12518. Epub 2014 Aug 29 [PubMed PMID: 25176318]
Level 2 (mid-level) evidenceKetelaars R, Gülpinar E, Roes T, Kuut M, van Geffen GJ. Which ultrasound transducer type is best for diagnosing pneumothorax? Critical ultrasound journal. 2018 Oct 22:10(1):27. doi: 10.1186/s13089-018-0109-0. Epub 2018 Oct 22 [PubMed PMID: 30345473]