Anatomy, Bony Pelvis and Lower Limb: Posterior Thigh Muscles
Anatomy, Bony Pelvis and Lower Limb: Posterior Thigh Muscles
Introduction
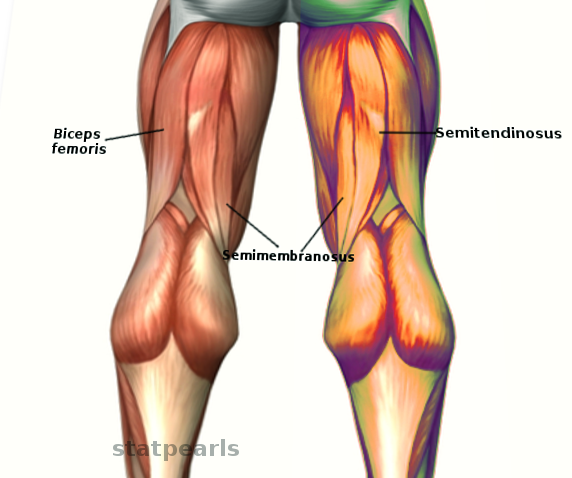
The muscles composing the posterior thigh compartment are collectively, and more commonly, known as the hamstring muscles. These three major muscles, consisting of the biceps femoris (short and long head), semitendinosus, and semimembranosus, play significant roles in everyday life as they participate in the complex actions of standing, walking, and running.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Except for the short head of the biceps femoris, the other posterior thigh muscles span the length of the femur and coss, both the hip and knee joints. Spanning from the posterior pelvis to the proximal tibia and fibula, the posterior thigh muscles provide motion to both the femoroacetabular joint (hip joint) and tibiofemoral joint (knee joint). The long head of the biceps femoris, semitendinosus, and semimembranosus originate from the ischial tuberosity of the pelvis extending distally on the posterior side of the femur, eventually crossing the knee — the biceps femoris crossing laterally while semimembranosus and semitendinosus cross medially.[1] The short head of the biceps femoris originates independently from the lateral linea aspera of the posterior femur before joining with the long head of the biceps femoris to span the knee.
The superior or proximal borders of the popliteal fossa, posterior to the knee, are created by the hamstring muscles descending and crossing the joint.[2] The superior-lateral border of the popliteal fossa is created by the biceps femoris, while the superior medial border forms from the semimembranosus and semitendinosus.
As a group of muscles, the hamstring muscles primarily work to extend the hip (movement of the femur directly posteriorly) and flex the knee (movement of the tibia and fibula directly posteriorly). These actions are significant components of the multi-joint movements of standing up from a seated position and normal gait. The ability to remain stable while standing is also largely attributed to the actions of the hamstring muscles, which allow the body to remain erect above the lower extremities by securely fixing the hip joint. The hamstrings additionally provide minor rotation pull on the lower extremity based on their lateral or medial insertion points distally (biceps femoris provides external rotation, semitendinosus/semimembranosus provides internal rotation).
Embryology
The entire human body initially derives from the embryonic ectoderm, mesoderm, or endoderm. Muscles, connective tissue, bones, blood vessels, and more form from the mesoderm. The posterior muscles of the thigh are no exception to this rule and can be traced back embryologically to their origin from the mesoderm. Specifically, the posterior thigh muscles derive from the paraxial mesoderm (somites) of the lower limb buds (L3 to L5) on the anterior surface of each bud. Around weeks 7 to 8 of gestation, the lower limbs begin to rotate medially to their final position resulting in the posterior location of these muscles.
Blood Supply and Lymphatics
The posterior thigh compartment, deep to the fascia lata, where the hamstring muscles reside, drains through lymphatic vessels to the deep inguinal lymph nodes along with the popliteal nodes, which drain some additional areas of the distal lower limb. The deep inguinal nodes continue to drain into the external iliac nodes, then to the common iliac nodes, eventually draining into the cisterna chyli/thoracic duct.[3]
Nerves
The sciatic nerve exits the pelvis via the greater sciatic foramen before coursing into and through the posterior thigh, deep to the long head of biceps femoris, before bifurcating at the superior border of the popliteal fossa into the tibial and common peroneal nerve.
The posterior femoral cutaneous nerve also exits the pelvis through the greater sciatic foramen. However, the posterior femoral cutaneous nerve travels superficially to the long head of the biceps femoris before traveling down the midline of the posterior thigh deep to the fascia lata until it reaches the popliteal fossa.[3]
Muscles
Biceps Femoris Long Head
- Origin: Common (conjoint) tendon from the superior medial quadrant of the posterior ischial tuberosity (with semitendinosus)
- Insertion: Majority onto the fibular head; also the lateral collateral ligament of the knee and lateral tibial condyle
- Action: Flexion of the knee and lateral rotation of the tibia; extension of the hip joint
- Innervation: Tibial nerve (a portion of the sciatic nerve)
- Arterial Supply: Perforating (muscular) branches of profunda femoris artery, inferior gluteal artery, and the superior muscular branches of the popliteal artery[3]
Biceps Femoris Short Head
- Origin: Lateral lip of linea aspera, the lateral intermuscular septum of the thigh, and lateral supracondylar ridge of femur
- Insertion: Mostly on the fibular head; lateral collateral ligament of the knee, and the lateral tibial condyle
- Action: Flexion of the knee and lateral rotation of the tibia
- Innervation: Common peroneal nerve (a portion of the sciatic nerve)
- Arterial Supply: Perforating (muscular) branches of profunda femoris artery, inferior gluteal artery, and the superior muscular branches of the popliteal artery[3]
Semimembranosus
- Origin: Superior lateral aspect of the ischial tuberosity
- Insertion: The posterior surface of the medial tibial condyle
- Action: Extension of the hip, flexion of the knee, and medial rotation of the tibia (specifically with knee flexion)
- Innervation: Tibial nerve (a portion of the sciatic nerve)
- Arterial Supply: Perforating (muscular) branches of profunda femoris artery, inferior gluteal artery, and the superior muscular branches of the popliteal artery[3]
Semitendinosus
- Origin: The common (conjoint) tendon from the superior medial quadrant of the posterior ischial tuberosity (with biceps femoris long head)
- Insertion: Superior aspect of the medial tibial shaft (into the distal portion of the pes anserinus along with the gracilus and sartorius muscles)
- Action: Extension of the hip and flexion of the knee, medial rotation of the tibia (specifically with knee flexion)
- Innervation: Tibial nerve (a portion of the sciatic nerve)
- Arterial Supply: Perforating (muscular) branches of profunda femoris artery, inferior gluteal artery, and the superior muscular branches of the popliteal artery[1]
Physiologic Variants
Variations in hamstring muscles and their attachments are rare. One variation noted in current research is the distinct origination of the biceps femoris long head and semitendinosus from separate tendons attached to the ischial tuberosity as opposed to their more common shared origination from the common (conjoint) tendon to the ischial tuberosity.[4][5]
Additional isolated variations have appeared through cadaver dissections. Of note on one cadaver was the lack of union between the short and long head of the biceps femoris while still inserting into the fibular head. On another, two anomalous muscles, one arising as a “third head of biceps femoris” and another as an independent muscle inserting into semitendinosus, were seen on post-mortem dissection.[6]
Surgical Considerations
Surgical treatments involving the hamstring muscles are rare, as conservative treatment for injuries is the preferred first-line management. Patients may present with ecchymosis over the posterior thigh and a stiff-legged gait to avoid flexion at the hip and knee. Patients with avulsion injuries of the proximal hamstring muscles from their origin may benefit from surgical treatment of their injuries regarding pain levels and functional outcomes, particularly if they are young and active. Surgical procedures have been shown to have better results when used in treating more severe avulsion injuries, as well as being performed on more acute injuries compared to chronic avulsion injuries.[7] The decision to indicate a patient for surgery depends on the distance that the tendon has retracted and the chronicity of symptoms.
Other surgical considerations regarding the hamstring muscles include autografting hamstring tendons to reconstruct the ACL in patients with tears. Removal of the semitendinosus and sometimes gracilus tendons from their insertion site into the pes anserinus for use in ACL repairs has been shown to have advantages over other autograft methods (such as using the patellar tendon) with less post-operative knee pain and an overall easier recovery following surgery.[8]
Clinical Significance
Hamstring muscle injuries are currently one of the most common injuries suffered by athletes. Patients largely report strains due to quick changes in speed and excessive lengthening of the hamstrings due to a particular inciting event or experiencing proximal tendinopathy resulting from excessive use over long periods. Two types of acute hamstring strains appear in the current literature. Type 1, involving mainly the proximal tendon muscle junction of the biceps femoris, results during the terminal deceleration of the swing phase of running as the patient prepares to plant their foot resulting in eccentric muscle contraction.[9] Type 2 hamstring strains result from extensive muscle lengthening, resulting in overstretching and injury to the proximal tendon area of the semimembranosus muscle. These types of injuries most commonly occur during actions involving flexion of the hip with an extension of the knee.[10] Of these two types of injuries, type 2 has been shown to require more time to fully heal and return to sports compared to type 1.[11]
Clinically, patients typically describe hamstring muscle strains as beginning acutely during physical activities involving the lower body with a sharp or stabbing pain in the proximal posterior thigh with increasing pain with active extension of the hip or flexion of the knee. A possible pop and/or delayed appearance of ecchymosis around the area of pain presents in more extreme cases.[12] On physical exam, patients generally exhibit pain in the posterior thigh with passive stretching of the hamstring muscles and activating or using the hamstring muscles. Plain radiographs of the pelvis may show a small avulsion fracture from the ischial tuberosity; however, an MRI is necessary if the radiographs are negative and a high index of suspicion exists.[13]
Treatment for hamstring injuries largely revolves around decreasing inflammation and damage near the time of injury with resting of the muscles, NSAIDs, and icing. Following initial treatment of the injury, varying progressions of physical therapy are used to progress patients back to full use of their hamstrings while avoiding re-injury, a very common occurrence with hamstring injuries.[14][15] Researchers have explored additional treatment modalities in pursuit of faster recovery, including the use of intramuscular corticosteroid injections and administration of platelet-rich plasma (PRP), all with varying results and efficacy at this time.[16][17]
Media
References
Mathew K, Pillarisetty LS. Anatomy, Bony Pelvis and Lower Limb: Thigh Semitendinosus Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30969684]
Hyland S, Sinkler MA, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Popliteal Region. StatPearls. 2023 Jan:(): [PubMed PMID: 30422486]
Rodgers CD, Raja A. Anatomy, Bony Pelvis and Lower Limb, Hamstring Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 31536294]
Koulouris G, Connell D. Hamstring muscle complex: an imaging review. Radiographics : a review publication of the Radiological Society of North America, Inc. 2005 May-Jun:25(3):571-86 [PubMed PMID: 15888610]
Azzopardi C, Almeer G, Kho J, Beale D, James SL, Botchu R. Hamstring origin-anatomy, angle of origin and its possible clinical implications. Journal of clinical orthopaedics and trauma. 2021 Feb:13():50-52. doi: 10.1016/j.jcot.2020.08.021. Epub 2020 Sep 17 [PubMed PMID: 33717874]
Chakravarthi K. Unusual unilateral multiple muscular variations of back of thigh. Annals of medical and health sciences research. 2013 Nov:3(Suppl 1):S1-2. doi: 10.4103/2141-9248.121206. Epub [PubMed PMID: 24349835]
Level 3 (low-level) evidenceBodendorfer BM, Curley AJ, Kotler JA, Ryan JM, Jejurikar NS, Kumar A, Postma WF. Outcomes After Operative and Nonoperative Treatment of Proximal Hamstring Avulsions: A Systematic Review and Meta-analysis. The American journal of sports medicine. 2018 Sep:46(11):2798-2808. doi: 10.1177/0363546517732526. Epub 2017 Oct 10 [PubMed PMID: 29016194]
Level 1 (high-level) evidenceFrank RM, Hamamoto JT, Bernardoni E, Cvetanovich G, Bach BR Jr, Verma NN, Bush-Joseph CA. ACL Reconstruction Basics: Quadruple (4-Strand) Hamstring Autograft Harvest. Arthroscopy techniques. 2017 Aug:6(4):e1309-e1313. doi: 10.1016/j.eats.2017.05.024. Epub 2017 Aug 14 [PubMed PMID: 29354434]
Chu SK, Rho ME. Hamstring Injuries in the Athlete: Diagnosis, Treatment, and Return to Play. Current sports medicine reports. 2016 May-Jun:15(3):184-90. doi: 10.1249/JSR.0000000000000264. Epub [PubMed PMID: 27172083]
Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during slow-speed stretching: clinical, magnetic resonance imaging, and recovery characteristics. The American journal of sports medicine. 2007 Oct:35(10):1716-24 [PubMed PMID: 17567821]
Level 3 (low-level) evidenceAskling C, Saartok T, Thorstensson A. Type of acute hamstring strain affects flexibility, strength, and time to return to pre-injury level. British journal of sports medicine. 2006 Jan:40(1):40-4 [PubMed PMID: 16371489]
Ali K, Leland JM. Hamstring strains and tears in the athlete. Clinics in sports medicine. 2012 Apr:31(2):263-72. doi: 10.1016/j.csm.2011.11.001. Epub 2011 Dec 21 [PubMed PMID: 22341016]
Koulouris G, Connell D. Imaging of hamstring injuries: therapeutic implications. European radiology. 2006 Jul:16(7):1478-87 [PubMed PMID: 16514470]
Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. The Journal of orthopaedic and sports physical therapy. 2010 Feb:40(2):67-81. doi: 10.2519/jospt.2010.3047. Epub [PubMed PMID: 20118524]
Sherry MA, Johnston TS, Heiderscheit BC. Rehabilitation of acute hamstring strain injuries. Clinics in sports medicine. 2015 Apr:34(2):263-84. doi: 10.1016/j.csm.2014.12.009. Epub 2015 Jan 28 [PubMed PMID: 25818713]
Levine WN, Bergfeld JA, Tessendorf W, Moorman CT 3rd. Intramuscular corticosteroid injection for hamstring injuries. A 13-year experience in the National Football League. The American journal of sports medicine. 2000 May-Jun:28(3):297-300 [PubMed PMID: 10843118]
Level 2 (mid-level) evidenceHamid MS, Yusof A, Mohamed Ali MR. Platelet-rich plasma (PRP) for acute muscle injury: a systematic review. PloS one. 2014:9(2):e90538. doi: 10.1371/journal.pone.0090538. Epub 2014 Feb 28 [PubMed PMID: 24587389]
Level 3 (low-level) evidence