Introduction
Galactorrhea is milk production from the breast unrelated to pregnancy or lactation. Milk production one year after cessation of breastfeeding is non-lactational and is considered galactorrhea. Various hormones including prolactin, estrogens, thyrotropin-releasing hormone (TRH) can affect the production of milk.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The various causes of galactorrhea broadly divide into hypothalamic-pituitary causes and non-hypothalamic-pituitary causes.
Hypothalamic-pituitary causes:
- Prolactinomas: Prolactinomas are prolactin-secreting tumors and are the commonest hormone-secreting tumors of the pituitary glands. Prolactinomas which are less than 1 cm in size are known as microprolactinomas, whereas those greater than 1 cm in size are known as macroprolactinomas. Prolactin levels correlate well with the size of the tumor with microprolactinomas having prolactin levels of >200 ng/ml and macroprolactinomas having higher prolactin levels of >1000 ng/ml.
- Non-prolactin-secreting pituitary tumor and infiltrative disorders of the pituitary stalk/hypothalamus: These tumors can cause hyperprolactinemia by disrupting the flow of dopamine from the hypothalamus to the anterior pituitary by compressing the pituitary stalk. This disruption results in decreased inhibition of prolactin and results in mild hyperprolactinemia, usually less than 200 ng/ml.[2]
Non-hypothalamic-pituitary causes:
- Hypothyroidism: Elevated levels of TRH in hypothyroidism can stimulate the lactotrophs resulting in hyperprolactinemia and galactorrhea.
- Medications: Several medications can cause hyperprolactinemia and galactorrhea. In most instances, the level of prolactin is less than 200 ng/ml; however, atypical antipsychotics like risperidone carry associations with prolactin levels of >200 ng/ml, which can be confused for a microprolactinoma. Atypical antipsychotics act on the D2 receptors in the hypothalamic tuberoinfundibular areas to cause hyperprolactinemia. Risperidone is a combined dopamine serotonin antagonist which can significantly raise the prolactin levels. Clozapine, olanzapine, and aripiprazole have both agonist and antagonist properties on the D2 receptor and only transiently raise the prolactin levels. Metoclopramide and domperidone, which are used in the treatment of vomiting, are D2 receptor blockers and cause hyperprolactinemia. Tricyclic antidepressants (especially clomipramine) and monoamine-oxidase inhibitors have been associated with mild hyperprolactinemia. The mechanisms by which these medications cause hyperprolactinemia is unknown. Opioids by acting through the µ receptors decrease the release of hypothalamic dopamine and can elevate prolactin levels. Verapamil has also been associated with hyperprolactinemia by decreasing the production of hypothalamic dopamine.[3]
- Renal failure: Hyperprolactinemia in renal failure is due to the failure of the kidneys to clear prolactin. Prolactin levels of >1000 mcg/liter have been reported with renal failure. Post-kidney transplant the hyperprolactinemia resolves rapidly within a few days.
- Chest wall lesions: Various chest wall lesions including burns, surgeries, herpes zoster have associations with hyperprolactinemia. The hypothesis is that the pain signals transmit to the hypothalamus via the spinal cord which results in decreased dopamine release and causes hyperprolactinemia.
- Idiopathic hyperprolactinemia: Occasionally hyperprolactinemia with no known cause has been reported. These could be secondary to small undiagnosed microprolactinomas. The hyperprolactinemia self resolves in 1/3rd patients and remains stable in half of the patients.[2]
Epidemiology
Hyperprolactinemia is more common in women. The prevalence of hyperprolactinemia ranges from 0.4% in an unselected normal adult population to as high as 9 to 17% in women with reproductive disorders. Its prevalence was found to be as high as 17% among women with polycystic ovary syndrome. [4]
Pathophysiology
Prolactin is responsible for the synthesis and secretion of milk. Prolactin is secreted by the lactotroph cells in the anterior pituitary. Dopamine secreted from the hypothalamus inhibits the secretion of prolactin. TRH and vasoactive intestinal polypeptide can stimulate prolactin secretion. Also, nipple stimulation, renal failure, chest wall lesions, and medications can cause hyperprolactinemia.[1][5]
Estrogens cause hyperprolactinemia by inhibiting hypothalamic dopamine as well as stimulating lactotrophs directly. In pregnancy, the high levels of estrogen cause lactotroph hyperplasia and can even result in the growth of a preexisting prolactinoma. Excess secretion of estrogen from ovaries in ovarian hyperstimulation syndrome has also been associated with hyperprolactinemia.[6][7]
History and Physical
Careful assessment of hyperprolactinemic related symptoms menstrual irregularities, decreased libido, galactorrhea, erectile dysfunction, infertility, and gynecomastia should be performed. Detailed medication history is important when considering medication induced hyperprolactinemia. If a pituitary lesion is suspected then evaluation for headaches, and visual deficits are in order.
For assessing galactorrhea on physical exam, the patient needs to be sitting and leaning forward. The areola needs to be squeezed in the direction of the nipple. The galactorrhea is usually bilateral and can be white or green. Bloody discharge could be due to breast tumors and will need further workup in that direction. A Sudan IV stain for fat droplets can confirm whether the discharge is milk or not.[2]
Evaluation
Prolactin levels need to be taken at least once in the evaluation of hyperprolactinemia. Prolactin levels are measured using a sandwich ELISA assay where a prolactin molecule needs to bind to a capture as well as a detection antibody to be measured. Rarely the “hook effect” may be seen in large prolactinomas with an extremely high prolactin level. Due to the extremely high prolactin levels, the number of prolactin molecules binding to both the capture and detection antibody is actually low. Dilution of the sample to a 1:100 concentration and remeasuring shows a paradoxical increase in the prolactin level. The “hook effect” needs to be considered in large pituitary adenomas which present with galactorrhea, hypogonadism but only mildly elevated levels of prolactin.[8][9]
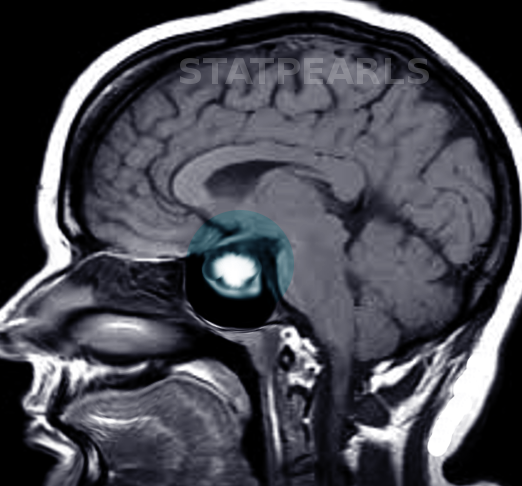
Hormonal assessment of other pituitary hormones should be taken as indicated by the clinical history and exam. Magnetic resonance imaging (MRI) of the pituitary gland may reveal lesions of the pituitary gland responsible for hyperprolactinemia. Visual field assessment needs to be performed when the tumor is in contact with the optic chiasma on MRI.[2]
Treatment / Management
After ruling out breast pathologies, therapy direction is towards the cause of hyperprolactinemia. Hyperprolactinemia is treated if there is a pituitary lesion or hypogonadism with problematic galactorrhea; if not troublesome, it can be monitored without therapy.
The mainstay of hyperprolactinemia is treatment with bromocriptine or cabergoline. These are dopamine agonists which act on the D2 receptors present on the lactotrophs and inhibit prolactin production. The doses for bromocriptine and cabergoline are 2.5-15 mg once daily and cabergoline 0.25-1 mg twice weekly, respectively. They are effective at normalizing prolactin levels as well as shrinking the size of the tumor. Side effects include nausea, vomiting, orthostatic hypotension, drowsiness, and headaches. Cardiac valvulopathy has been reported with high doses of cabergoline, and it is recommended to get an annual echocardiogram in patients on more than 3.5 mg/week.
In cases of medication-induced hyperprolactinemia, the offending medication should be stopped or changed to a different class. Use of dopamine agonists in these instances has associations with a slight risk of exacerbating the psychiatric disorder.
Normoprolactinemic galactorrhea occurs when the galactorrhea accompanies normal prolactin levels. If symptomatic with troublesome galactorrhea or menstrual cycle irregularities it can be treated with dopamine agonists to obtain symptomatic relief. The treatment is tapered off once the galactorrhea has resolved.[2][1](A1)
Differential Diagnosis
- Acromegaly
- Breast stimulation
- Bronchogenic carcinoma
- Burns
- Breast surgery
- Craniopharyngioma
- Cushing's disease
- Chest wall irritation
- Hypothyroidism
- Idiopathic
- Lymphoma
- Molar pregnancy
- Meds and herbs
- Pituitary adenomas
- Renal failure
- Sarcoid
- TB
Enhancing Healthcare Team Outcomes
Galactorrhea is nonlactational production of milk. Prolactin, estrogens, and TRH all play a role in the production of milk from the breast. The condition is often managed by an interprofessional team that consists of a radiologist, endocrinologist, neurosurgeon, neurologist, and an internist. The galactorrhea associated with hyperprolactinemia is often associated with symptoms of hypogonadism (decreased libido, erectile dysfunction, and menstrual irregularities) and thus a thorough medical history and physical exam are needed. Serosanguinous discharge from the breast should prompt further evaluation for breast pathologies. Inquiring of the patient about their current medications is vital. In most cases, treatment with dopamine agonists (cabergoline or bromocriptine) normalizes prolactin levels and results in shrinkage of the tumor. (Level V)
Media
References
Huang W, Molitch ME. Evaluation and management of galactorrhea. American family physician. 2012 Jun 1:85(11):1073-80 [PubMed PMID: 22962879]
Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA, Wass JA, Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. The Journal of clinical endocrinology and metabolism. 2011 Feb:96(2):273-88. doi: 10.1210/jc.2010-1692. Epub [PubMed PMID: 21296991]
Level 1 (high-level) evidenceMolitch ME. Drugs and prolactin. Pituitary. 2008:11(2):209-18. doi: 10.1007/s11102-008-0106-6. Epub [PubMed PMID: 18404390]
Level 3 (low-level) evidenceVroonen L, Daly AF, Beckers A. Epidemiology and Management Challenges in Prolactinomas. Neuroendocrinology. 2019:109(1):20-27. doi: 10.1159/000497746. Epub 2019 Feb 7 [PubMed PMID: 30731464]
Freeman ME, Kanyicska B, Lerant A, Nagy G. Prolactin: structure, function, and regulation of secretion. Physiological reviews. 2000 Oct:80(4):1523-631 [PubMed PMID: 11015620]
Level 3 (low-level) evidenceChristin-Maître S, Delemer B, Touraine P, Young J. Prolactinoma and estrogens: pregnancy, contraception and hormonal replacement therapy. Annales d'endocrinologie. 2007 Jun:68(2-3):106-12 [PubMed PMID: 17540335]
Morel GR, Carón RW, Cónsole GM, Soaje M, Sosa YE, Rodríguez SS, Jahn GA, Goya RG. Estrogen inhibits tuberoinfundibular dopaminergic neurons but does not cause irreversible damage. Brain research bulletin. 2009 Dec 16:80(6):347-52. doi: 10.1016/j.brainresbull.2009.08.026. Epub 2009 Sep 8 [PubMed PMID: 19744546]
Level 3 (low-level) evidenceBarkan AL, Chandler WF. Giant pituitary prolactinoma with falsely low serum prolactin: the pitfall of the "high-dose hook effect": case report. Neurosurgery. 1998 Apr:42(4):913-5; discussion 915-6 [PubMed PMID: 9574657]
Level 3 (low-level) evidenceChahal J, Schlechte J. Hyperprolactinemia. Pituitary. 2008:11(2):141-6. doi: 10.1007/s11102-008-0107-5. Epub [PubMed PMID: 18404389]