Introduction
The anterior pituitary, also known as adenohypophysis, is one of the two lobes of the pituitary gland located in the sella turcica and controlled by the hypothalamus. The anterior pituitary secretes a number of peptide and glycoprotein hormones that regulate various cellular processes including growth, metabolism, reproduction, and response to stress or trauma. By acting directly on their respective target cells or by stimulating other endocrine organs to release hormones, anterior pituitary regulates various aspects of body function. It is important to emphasize that the majority are produced in a pulsatile fashion and dependant on the releasing hormone generators.[1][2][3][4][5]
Cellular Level
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Cellular Level
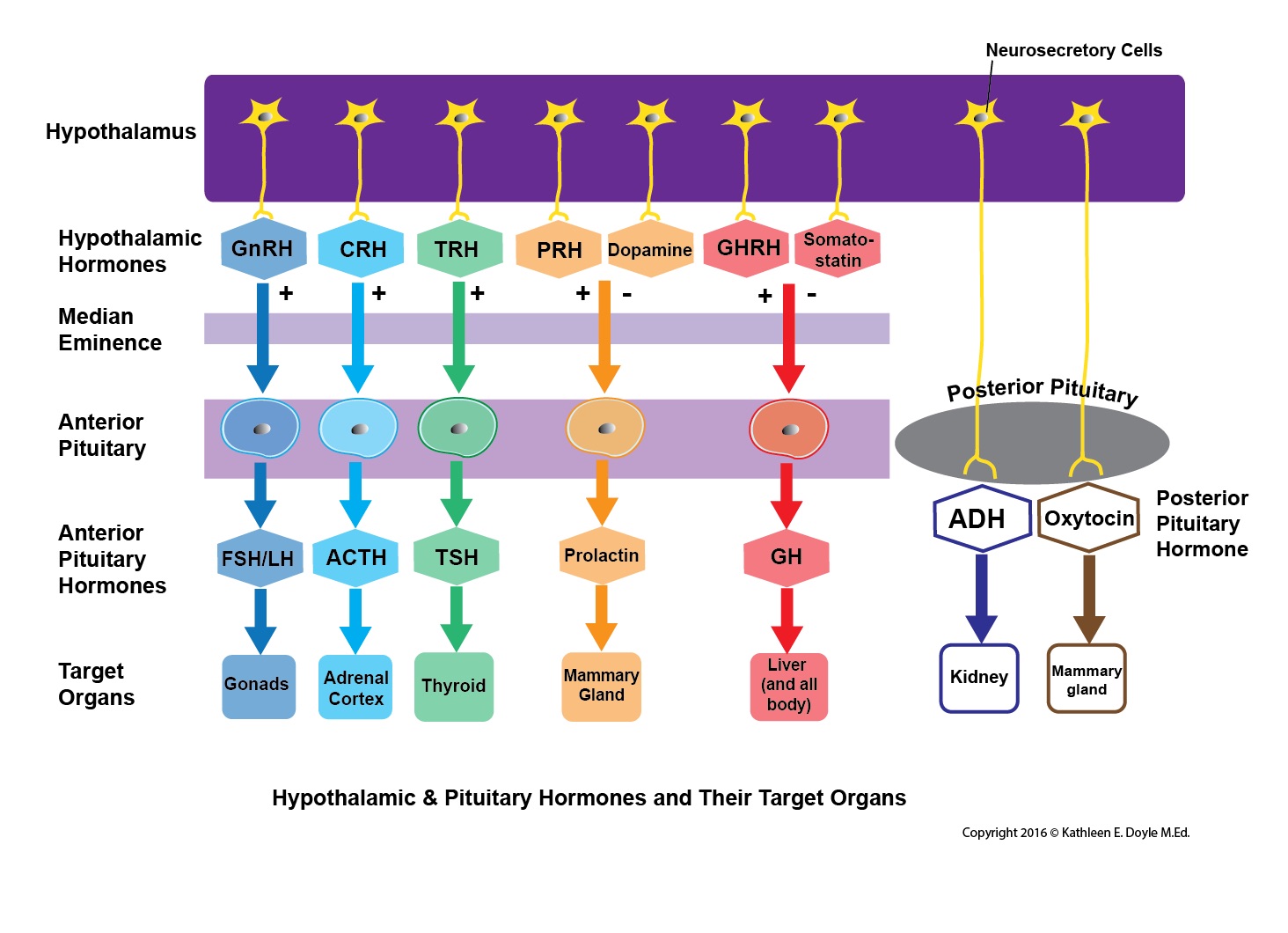
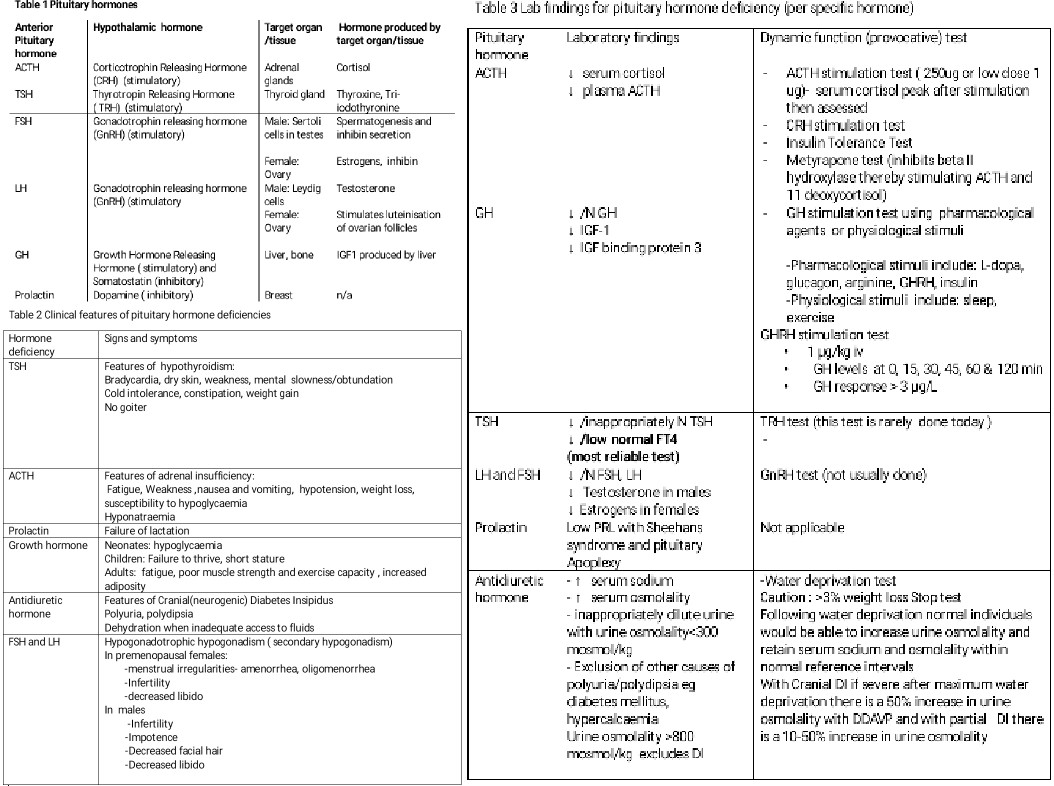
The anterior pituitary gland is composed of cell clusters that produce six anterior pituitary hormones and release them into the circulation. Corticotrophs produce the adrenocorticotrophic hormone (ACTH), thyrotrophs produce the thyroid-stimulating hormone (TSH), somatotrophs produce the growth hormone (GH), gonadotrophs produce both follicle-stimulating hormone (FSH) and luteinizing hormone (LH), and lactotrophs produce prolactin (PRL). The clusters of cells that produce the six anterior pituitary hormones are under hypothalamic control. Unlike the posterior pituitary which basically stores hormones produced by the hypothalamus, the hypothalamus regulates the anterior pituitary via secreting “releasing hormones," somatostatin and dopamine. These hormones are secreted directly into the hypophyseal portal circulation that supplies blood to the anterior pituitary. Once reaching their target cell cluster in the anterior pituitary, the releasing hormones either stimulate or inhibit the synthesis and secretion of anterior pituitary hormones.
Development
The pituitary gland is an ectodermal origin. At approximately 36 days of gestation, an upward growth from the ectodermal roof of the primordial oral cavity called the hypophyseal diverticulum or Rathke pouch gives rise to the anterior lobe of the pituitary gland. By eight weeks of gestation, the hypophyseal diverticulum loses its connection with the oral cavity and comes into contact with the infundibulum and posterior pituitary. The proliferation of the hypophyseal diverticulum produces the cells that make up the adenohypophysis or anterior pituitary.[6][7][8]
Organ Systems Involved
Hypothalamic-Pituitary Axis
The corticotrophin-releasing hormone (CRH) of the hypothalamus stimulates the corticotrophs in the anterior pituitary to secrete corticotrophin or ACTH, the thyrotropin-releasing hormone stimulates the thyrotrophs to secrete TSH, growth hormone-releasing hormone stimulates the somatotrophs to secrete growth hormone (GH), luteinizing hormone-releasing hormone stimulates gonadotrophs to secrete FSH and LH. Unlike the other releasing hormones that induce secretion of anterior pituitary hormones, dopamine inhibits the production of prolactin by lactotrophs. Likewise, somatostatin inhibits the production of GH.
The pituitary gland is located inferior to the hypothalamus and is connected to the hypothalamus by a stalk. Hormonal secretion by the anterior pituitary is controlled by hypothalamic-releasing hormones that reach their target endocrine tissues in the anterior pituitary via the pituitary stalk. Any damage to the pituitary stalk due to trauma can result in low production of ACTH, TSH, FSH, LH, and GH but can cause increased production of PRL due to the absence of tonic inhibitory effect of dopamine on prolactin.
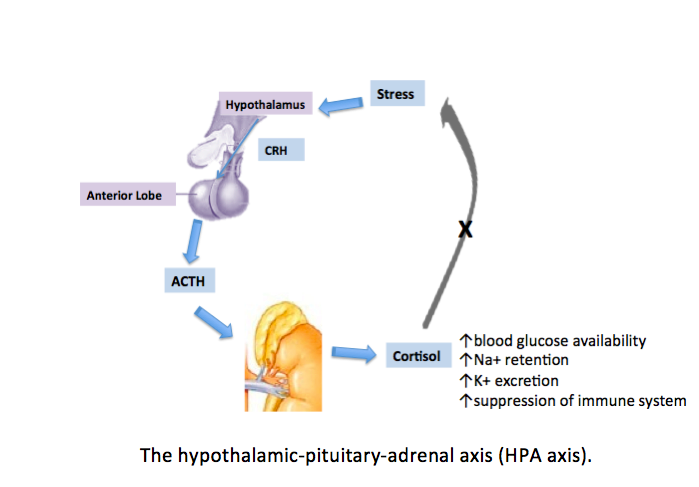
Hypothalamic-Pituitary-Adrenal Axis
Hypothalamic-pituitary-adrenal axis describes the interactions between the hypothalamus, anterior pituitary, and the adrenal cortex, involving stimulatory effects of hypothalamus on corticotrophs of the anterior pituitary and anterior pituitary on adrenal cortex as well as negative feedback actions of the end product hormone on the hypothalamus or anterior pituitary. Hypothalamus produces CRH that stimulates the corticotrophs in the anterior pituitary to secrete corticotrophin or ACTH into the bloodstream. ACTH is carried in the circulation to the adrenal cortex where it stimulates the zona fasciculata (middle layer of adrenal cortex) and zona reticularis (inner layer of the adrenal cortex) which produce the glucocorticoids cortisol and androgen dehydroepiandrosterone (DHEA). Increased amounts of glucocorticoids in the circulation cause negative feedback actions on the anterior pituitary to reduce the production of ACTH and on the hypothalamus to reduce the production of CRH. Both negative feedback actions inhibit the amount of ACTH produced by the anterior pituitary and hence reduce the stimulatory effects of ACTH on the adrenal cortex. This axis of CRH-ACTH can be over-ridden by stress.
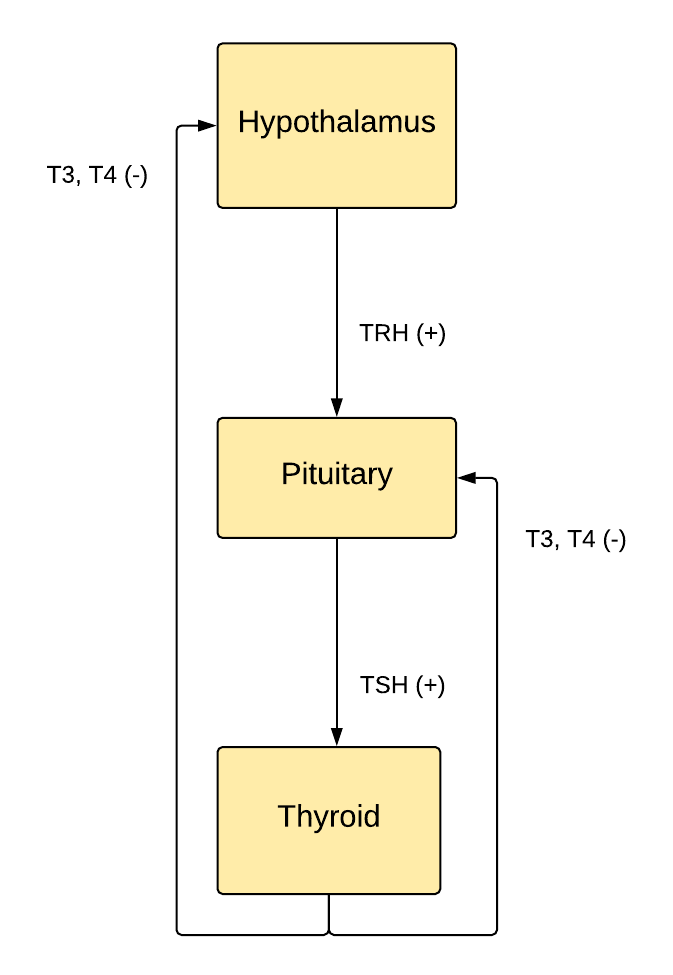
Hypothalamic-Pituitary-Thyroid Axis
The production of thyroid hormones begins with the hypothalamus producing TRH that stimulates the thyrotrophs in the anterior pituitary to secrete TSH. However, somatostatin produced by the hypothalamus causes an inhibitory effect on the anterior pituitary to produce TSH. TSH binds to its receptors found in the follicular cells of the thyroid to produce T3 and T4. The increased amount of thyroid hormones in the circulation causes negative feedback by inhibiting the anterior pituitary to secrete TSH as well as inhibiting the hypothalamic production of TRH which in turn causes the reduction of TSH and thyroid hormones. When circulating levels of T3 and T4 decline, their negative feedback on the hypothalamus and anterior pituitary decrease, leading to the rise in TSH and hence increase thyroid hormones. T3 is the major hormone that inhibits TSH and TRH secretion.
Hypothalamic-Pituitary-GH Axis
Growth hormone production from the anterior pituitary is regulated by the stimulatory and inhibitory control of the hypothalamus. Hypothalamus produces growth hormone-releasing hormone that stimulates the somatotrophs of the anterior pituitary to secrete growth hormone. Somatostatin produced by the hypothalamus inhibits the secretion of growth hormone from the anterior pituitary. Once released into the circulation, growth hormone increases the expression of the insulin-like growth factor 1 (IGF-1) gene to a greater extent in the liver compared to other tissues. IGF-1 mediates the effects of GH on growth etc
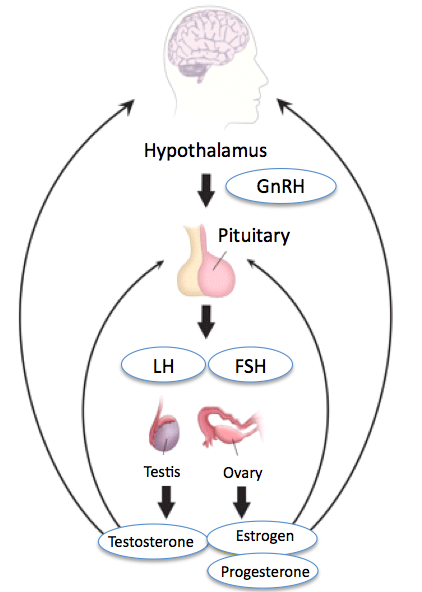
Hypothalamic-Pituitary-Gonadal Axis
GnRH produced by the hypothalamus stimulates the production of both LH and FSH.FSH functions by stimulating ovarian follicular development in females and regulating spermatogenesis in males. LH induces ovulation and corpus luteum formation in the ovaries. It also stimulates the ovaries to produce estrogen and progesterone. In males, LH induces testosterone production. Inhibin produced by the gonads inhibits FSH in the Pituitary.
Function
ACTH stimulates the adrenal cortex to produce glucocorticoids and adrenal androgens. Glucocorticoids, such as cortisol, function by maintaining blood glucose levels during fasting, preparing the body during physical and emotional stress, preventing inflammation, and suppressing the immune system. TSH stimulates receptors found in the follicular cells of the thyroid gland to produce thyroid hormones T4 and T3. In turn, the thyroid hormones regulate the body’s basal metabolic rate, produce heat, and promote the development of the central nervous system. TSH is also necessary to maintain the size of the thyroid follicles and their continued ability to produce thyroid hormones. GH influences the normal rate of body growth during childhood and adolescence. It also regulates triglyceride lipolysis and controls the action of insulin on carbohydrate and lipid metabolism. Both LH and FSH are important for the menstrual cycle in females, including ovulation, and male gonadal function.
Pathophysiology
Both hypofunction and hyperfunction can result. Measurement of pituitary hormones and target hormones can help define the defects. In Cushing disease, there is an increase in both ACTH and Cortisol. In Prolactinomas, there are very high PRL levels, generally greater than 200 ng/mL. In Acromegaly IGF-1 levels are increased, and GH fails to suppress during an oral GTT. In hypopituitarism, there is decreased GH, IGF-1, LH FSH, testosterone in males, ACTH, cortisol T4 and TSH levels and PRL in Sheehan Syndrome.[9][10]
Clinical Significance
Hypothalamic-releasing hormones can be synthetically produced and used for the treatment of endocrine disorders. GnRH can be used to treat patients with hypogonadotropic hypogonadism and restore fertility. GHRH can be of value to treat short stature.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Gurung P, Yetiskul E, Jialal I. Physiology, Male Reproductive System. StatPearls. 2025 Jan:(): [PubMed PMID: 30860700]
O'Toole TJ, Sharma S. Physiology, Somatostatin. StatPearls. 2025 Jan:(): [PubMed PMID: 30855911]
Bello MO, Garla VV. Gigantism and Acromegaly. StatPearls. 2025 Jan:(): [PubMed PMID: 30855849]
Thau L,Gandhi J,Sharma S, Physiology, Cortisol StatPearls. 2021 Jan [PubMed PMID: 30855827]
Thapa S, Bhusal K. Hyperprolactinemia. StatPearls. 2025 Jan:(): [PubMed PMID: 30726016]
Orlowski M, Sarao MS. Physiology, Follicle Stimulating Hormone. StatPearls. 2025 Jan:(): [PubMed PMID: 30571063]
Shahid Z, Asuka E, Singh G. Physiology, Hypothalamus. StatPearls. 2025 Jan:(): [PubMed PMID: 30571001]
Sizar O, Leslie SW, Schwartz J. Male Hypogonadism. StatPearls. 2025 Jan:(): [PubMed PMID: 30422528]
Bear MH, Reddy V, Bollu PC. Neuroanatomy, Hypothalamus. StatPearls. 2025 Jan:(): [PubMed PMID: 30252249]
Pirahanchi Y, Tariq MA, Jialal I. Physiology, Thyroid. StatPearls. 2025 Jan:(): [PubMed PMID: 30137850]