Introduction
Torsades de Pointes is a type of polymorphic ventricular tachycardia characterized by a gradual change in amplitude and twisting of the QRS complexes around an isoelectric line on the electrocardiogram. Torsades de Pointes is associated with QTc prolongation, which is the heart rate adjusted lengthening of the QT interval. A QTc is considered long when it is greater than 450 ms in males and 460 ms in females. A QTc greater than 500 ms has been associated with a two-fold to three-fold increase in risk for Torsades de Pointes. The rhythm may terminate spontaneously or may degenerate into ventricular fibrillation.[1][2][3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Torsades de pointes is the result of QTc prolongation which can either be congenital or acquired. Acquired QTc prolongation is most often drug-related. There is an extensive list of medications that can predispose a person to torsades. The list includes but is not limited to: antiarrhythmics, antipsychotics, antiemetics, antifungals, and antimicrobials. Substances that slow the hepatic metabolism of these medications can potentiate QTc prolongation leading to an increased likelihood of torsades de pointes. Congenital prolonged QT has two genetic variants: Jervell and Lange-Nielsen and Romano-Ward syndrome. The former is associated with congenital deafness. Prolonged QTc and Torsades are also associated with certain risk factors that include: older age (older than 65), female gender, hypokalemia, hypocalcemia, hypomagnesemia, bradycardia, heart disease, and diuretic use.[4][5]
Two rare congenital long QT syndromes include Romano-Ward syndrome and Jervell and Lange Nielsen syndrome.
Epidemiology
The prevalence of congenital prolonged QT is largely unknown. Figures estimate between 1:2000 and 1:20,000 have the genetic mutation for QT prolongation. Clinically more males than females exhibit the trait. Little is also known about the prevalence or incidence of drug-induced torsades de pointes. This is mainly because the arrhythmia is often transient, and an accurate diagnosis requires an ECG to be recorded during the event. Several European centers estimate that the annual reporting rate of drug-induced Torsades de Pointes is between 0.8 and 1.2 per million person-years. The incidence of drug-induced Torsades de Pointes also varies based on the drug in question and the population being studied.[6][7][8]
Pathophysiology
The proposed mechanism for Torsades de Pointes involves inhibition of the delayed rectifier potassium current. This leads to an excess of positive ions within the cellular membrane causing a prolonged repolarization phase. If an ectopic beat is generated during this prolonged repolarization phase, known as an R on T phenomenon, this can result in Torsades de Pointes. Both congenital and drug-induced QT prolongation affect the cellular membrane in similar fashions by blocking the potassium channel. Torsades de Pointes is slightly different from ventricular fibrillation in that it can spontaneously resolve. However, Torsades de Pointes can ultimately progress into venticular fibrillation if left untreated.[9]
History and Physical
Around 50% of patients with Torsades de Pointes are asymptomatic. The most common symptoms reported are syncope, palpitations, and dizziness. However, cardiac death is the presenting symptom in up to 10% of patients.
Patients with Jervell and Lange Nielsen syndrome may have a history of deafness.
Today one needs to be aware that drug-induced long QT syndrome is common and hence, a thorough medication history must be obtained.
Patients with torsade may be hypotensive, have a rapid pulse and have loss of consciousness.
Evaluation
An electrocardiogram is paramount in the diagnosis of Torsades de Pointes. The characteristic finding is a twisting of the QRS complexes around an isoelectric line. Torsades de Pointes is triggered by a PVC occurring on a preceding T wave. The onset of Torsades de Pointes is often preceded by a run of short-long-short R-R intervals. A QT nomogram can provide a sensitive and specific assessment of the risk of Torsades de Pointes in drug-induced QTc prolongation. Any value plotted above the line on the nomogram puts the patient at risk of Torsades de Pointes.[10][11]
Treatment / Management
The first step in managing Torsades de Pointes is preventing its onset by targeting modifiable risk factors. This includes discontinuing any QT prolonging drugs and optimizing a patient’s electrolyte profile. Correcting hypokalemia, hypomagnesemia, and hypocalcemia can all help to prevent the onset of torsades. There are a small number of studies that show a possible prophylactic benefit of oral or IV magnesium for those patients with drug-induced prolonged QT. However, the overall benefit is not well established, and there is little evidence that magnesium has any effect on the actual QT interval. The management of Torsades de Pointes begins with assessing if the patient is hemodynamically stable. Most episodes of torsades are self-limiting. However, the danger lies in those patients who go on to develop ventricular fibrillation. For those patients with hypotension or in cardiac arrest from Torsades de Pointes, electrical cardioversion should be performed. Synchronized cardioversion should be performed on a hemodynamically unstable patient in torsades who has a pulse, (100J monophasic, 50J Biphasic). Pulseless torsades should be defibrillated. Intravenous magnesium is the first-line pharmacologic therapy in Torsades de Pointes. Magnesium has been shown to stabilize the cardiac membrane, though the exact mechanism is unknown. The recommended initial dose of magnesium is a slow 2 g IV push. An infusion of 1 gm to 4 gm/hr should be started to keep the magnesium levels greater than 2 mmol/L. Once the magnesium level is greater than 3 mmol/L, the infusion can be stopped. Severe magnesium toxicity is seen with levels greater than 3.5 mmol/L and can present as confusion, respiratory depression, coma, and cardiac arrest. It is important to remember to correct any hypokalemia as well. Serum potassium should be maintained between 4.5 mmol/L and 5 mmol/L when treating Torsades de Pointes.
For a patient that continues to have intermittent runs of Torsades de Pointes, despite treatment with magnesium, increasing the heart rate may also help. This can be done pharmacologically with medications such as isoproterenol. Isoproterenol has been shown to help prevent Torsades de Pointes in patients with prolonged QT that is refractory to magnesium. It is a non-selective beta agonist, which increases the heart rate and shortens the QT interval. This lowers the likelihood of an R-on-T phenomenon that can lead to TdP. Isoproterenol can be given as an IV push of 10 mcg to 20mcg or an infusion titrated to maintain a heart rate of 100 bpm. Isoproterenol is, however, contraindicated in patients with congenital prolonged QT, because it can paradoxically lengthen the QT interval. A final option for terminating torsades is overdrive pacing. There are limited studies on the success of pacing for treatment of Torsades de Pointes; however, there are numerous case reports that show it is a viable option. Overdrive pacing can be used in the setting of both frequent runs of torsades and Torsades de Pointes that is refractory to magnesium. The rate must be set to overcome the patient’s intrinsic rate of ectopy. Ventricular rates of 90 bpm to 110 bpm are usually sufficient to overcome the arrhythmia, however occasionally rates up to 140 bpm have been required for some patients. Overdrive pacing is recommended for both drug and chemical induced Torsades de Pointes.[12][7][13](A1)
Differential Diagnosis
- Ventricular tachycardia/fibrillation
- Dialysis-related complications
- Syncope
- Drug toxicity- antihistamines, antiarrhythmics
Complications
- Ventricular fibrillation
- Sudden cardiac death
Consultations
- Electrophysiologist
- Cardiologist
- Geneticist if the patient has congenital long QT syndrome
Enhancing Healthcare Team Outcomes
Torsade is a rare arrhythmia, but it can quickly be fatal if not diagnosed and treated. Patients may present with a range of symptoms but it is the ECG that is diagnostic. While the arrhythmia is managed by physicians, all nurses should recognize this arrhythmia and consult with the cardiologist. Those who have a congenital disorder causing prolonged QT interval should be told to refrain from exercise. The pharmacist should educate the patient on medication compliance to prevent recurrence. Close follow up is required because the risk of sudden death is present. The pharmacist must be aware of all drugs the patient is taking and ensure that he or she is not on any medications that prolonged the QT interval. Finally, the nurse should teach all patients how to monitor their pulses and note for the presence of any adverse effects from the medications. In addition, the family should be taught basic life support. [14][15][16](Level V)
Outcomes
For patients with congenital long QT syndromes, the mortality for untreated patients is more than 50% over 5 years. With intervention, the mortality rates can be decreased to single digits. In patients with acquired long QT syndrome, the prognosis is good as long as the trigger medication or factor has been identified and discontinued. [17][18](Level V)
Media
(Click Image to Enlarge)
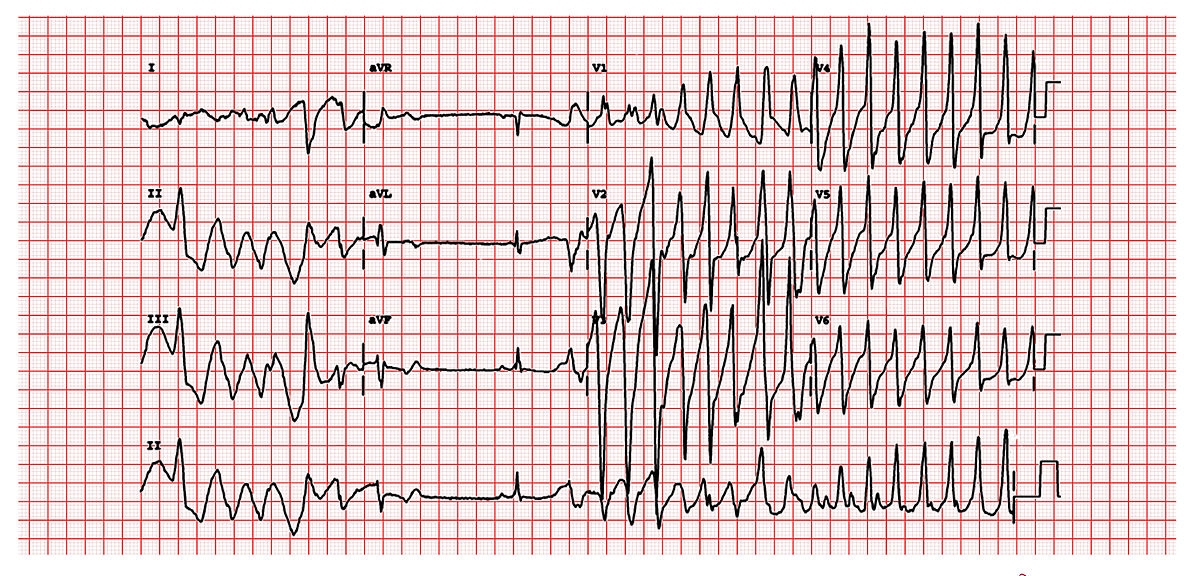
This is a classic 12 lead EKG of a patient with Torsade de Pointes. It shows the polymorphic nature of the tachycardia, the long QT interval and the initiation of the tachycardia with a late coupled P.V.C. Contributed by Michael Rosengarten BEng, MD.McGill (CC BY-SA 3.0 https://creativecommons.org/licenses/by-sa/3.0/deed.en)
References
Van Laecke S. Hypomagnesemia and hypermagnesemia. Acta clinica Belgica. 2019 Feb:74(1):41-47. doi: 10.1080/17843286.2018.1516173. Epub 2018 Sep 17 [PubMed PMID: 30220246]
Wilders R, Verkerk AO. Long QT Syndrome and Sinus Bradycardia-A Mini Review. Frontiers in cardiovascular medicine. 2018:5():106. doi: 10.3389/fcvm.2018.00106. Epub 2018 Aug 3 [PubMed PMID: 30123799]
Khan Q, Ismail M, Haider I. High prevalence of the risk factors for QT interval prolongation and associated drug-drug interactions in coronary care units. Postgraduate medicine. 2018 Nov:130(8):660-665. doi: 10.1080/00325481.2018.1516106. Epub 2018 Sep 5 [PubMed PMID: 30145917]
De Vecchis R, Ariano C, Di Biase G, Noutsias M. Acquired drug-induced long QTc: new insights coming from a retrospective study. European journal of clinical pharmacology. 2018 Dec:74(12):1645-1651. doi: 10.1007/s00228-018-2537-y. Epub 2018 Aug 15 [PubMed PMID: 30112668]
Level 2 (mid-level) evidenceSalem JE, Dureau P, Bachelot A, Germain M, Voiriot P, Lebourgeois B, Trégouët DA, Hulot JS, Funck-Brentano C. Association of Oral Contraceptives With Drug-Induced QT Interval Prolongation in Healthy Nonmenopausal Women. JAMA cardiology. 2018 Sep 1:3(9):877-882. doi: 10.1001/jamacardio.2018.2251. Epub [PubMed PMID: 30073300]
Salem M, Reichlin T, Fasel D, Leuppi-Taegtmeyer A. Torsade de pointes and systemic azole antifungal agents: Analysis of global spontaneous safety reports. Global cardiology science & practice. 2017 Jun 30:2017(2):11. doi: 10.21542/gcsp.2017.11. Epub 2017 Jun 30 [PubMed PMID: 29644223]
Porta-Sánchez A, Gilbert C, Spears D, Amir E, Chan J, Nanthakumar K, Thavendiranathan P. Incidence, Diagnosis, and Management of QT Prolongation Induced by Cancer Therapies: A Systematic Review. Journal of the American Heart Association. 2017 Dec 7:6(12):. doi: 10.1161/JAHA.117.007724. Epub 2017 Dec 7 [PubMed PMID: 29217664]
Level 1 (high-level) evidenceHeemskerk CPM, Pereboom M, van Stralen K, Berger FA, van den Bemt PMLA, Kuijper AFM, van der Hoeven RTM, Mantel-Teeuwisse AK, Becker ML. Risk factors for QTc interval prolongation. European journal of clinical pharmacology. 2018 Feb:74(2):183-191. doi: 10.1007/s00228-017-2381-5. Epub 2017 Nov 22 [PubMed PMID: 29167918]
Baldzizhar A, Manuylova E, Marchenko R, Kryvalap Y, Carey MG. Ventricular Tachycardias: Characteristics and Management. Critical care nursing clinics of North America. 2016 Sep:28(3):317-29. doi: 10.1016/j.cnc.2016.04.004. Epub 2016 Jun 22 [PubMed PMID: 27484660]
Adam MP, Feldman J, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, Groffen AJ, Bikker H, Christiaans I. Long QT Syndrome Overview. GeneReviews(®). 1993:(): [PubMed PMID: 20301308]
Turner JR, Rodriguez I, Mantovani E, Gintant G, Kowey PR, Klotzbaugh RJ, Prasad K, Sager PT, Stockbridge N, Strnadova C, Cardiac Safety Research Consortium. Drug-induced Proarrhythmia and Torsade de Pointes: A Primer for Students and Practitioners of Medicine and Pharmacy. Journal of clinical pharmacology. 2018 Aug:58(8):997-1012. doi: 10.1002/jcph.1129. Epub 2018 Apr 19 [PubMed PMID: 29672845]
de Lemos ML, Kung C, Kletas V, Badry N, Kang I. Approach to initiating QT-prolonging oncology drugs in the ambulatory setting. Journal of oncology pharmacy practice : official publication of the International Society of Oncology Pharmacy Practitioners. 2019 Jan:25(1):198-204. doi: 10.1177/1078155217748735. Epub 2018 Jan 3 [PubMed PMID: 29298624]
Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, Deal BJ, Dickfeld T, Field ME, Fonarow GC, Gillis AM, Granger CB, Hammill SC, Hlatky MA, Joglar JA, Kay GN, Matlock DD, Myerburg RJ, Page RL. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Executive summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart rhythm. 2018 Oct:15(10):e190-e252. doi: 10.1016/j.hrthm.2017.10.035. Epub 2017 Oct 30 [PubMed PMID: 29097320]
Level 1 (high-level) evidenceCrimmins S, Vashit S, Doyle L, Harman C, Turan O, Turan S. A multidisciplinary approach to prenatal treatment of congenital long QT syndrome. Journal of clinical ultrasound : JCU. 2017 Mar 4:45(3):168-170. doi: 10.1002/jcu.22386. Epub 2016 Aug 5 [PubMed PMID: 27492745]
Shulman M, Miller A, Misher J, Tentler A. Managing cardiovascular disease risk in patients treated with antipsychotics: a multidisciplinary approach. Journal of multidisciplinary healthcare. 2014:7():489-501. doi: 10.2147/JMDH.S49817. Epub 2014 Oct 31 [PubMed PMID: 25382979]
van Aerde KJ, Kalverdijk LJ, Reimer AG, Widdershoven JA. [QT interval prolongation and psychotropic drugs in children and adolescents: proposed guideline]. Nederlands tijdschrift voor geneeskunde. 2008 Aug 9:152(32):1765-70 [PubMed PMID: 18754307]
Tse G, Gong M, Meng L, Wong CW, Bazoukis G, Chan MTV, Wong MCS, Letsas KP, Baranchuk A, Yan GX, Liu T, Wu WKK. Predictive Value of T (peak) - T (end) Indices for Adverse Outcomes in Acquired QT Prolongation: A Meta-Analysis. Frontiers in physiology. 2018:9():1226. doi: 10.3389/fphys.2018.01226. Epub 2018 Sep 3 [PubMed PMID: 30233403]
Level 1 (high-level) evidenceRamalho D, Freitas J. Drug-induced life-threatening arrhythmias and sudden cardiac death: A clinical perspective of long QT, short QT and Brugada syndromes. Revista portuguesa de cardiologia. 2018 May:37(5):435-446. doi: 10.1016/j.repc.2017.07.010. Epub 2018 Apr 7 [PubMed PMID: 29636202]
Level 3 (low-level) evidence