Introduction
Scapholunate advanced collapse (SLAC) describes a characteristic degenerative clinical wrist condition of progressive instability, deformity, and arthritis affecting the radiocarpal and midcarpal joints of the wrist.[1] The characteristic pattern of arthritic deformity and progressive instability occurs secondary to a long-term, chronic dissociation between the lunate and the scaphoid carpal bones.[2] SLAC of the wrist is often the terminal and end-stage result of an untreated scapholunate interosseous ligament (SLIL) injury. Radiographic, computerized tomography and magnetic resonance imaging often demonstrate widening of the scapholunate interval, degenerative changes of the affected carpal bones, and proximal migration of the capitate.[3] A 4-stage categorization to grade arthrosis is often used.[4]
Treatment most commonly includes 4-corner arthrodesis, capitolunate arthrodesis, radial styloidectomy, proximal row carpectomy, and scaphoidectomy.[5] This condition was first described by Watson and Bellet when they reviewed 4000 wrist radiographs and discovered the common pattern of wrist bone involving arthritis in 210 wrists.[6]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Chronic SLIL injuries often result secondary to trauma, although they can also occur in association with other degenerative or inflammatory arthritic conditions of the wrist.[7][8] SLAC wrist can occur bilaterally even without a preceding history of trauma and has been described in association with chronic pseudogout.[9] Many clinical presentations are either initially under-appreciated or may be acutely diagnosed as a "wrist sprain." Football linemen are particularly prone to "acute on chronic" repetitive SLIL injuries as these athletes are subject to high-impact, forced wrist dorsiflexion movements over many years.[10] These injuries change the biomechanics of the wrist joint, leading to wrist arthritis. As SLAC arthritis progresses and untreated SLIL injury worsens, the scaphoid changes shape and position. This increases the capitate's mechanical burden, migrating between the lunate and scaphoid over time.
Epidemiology
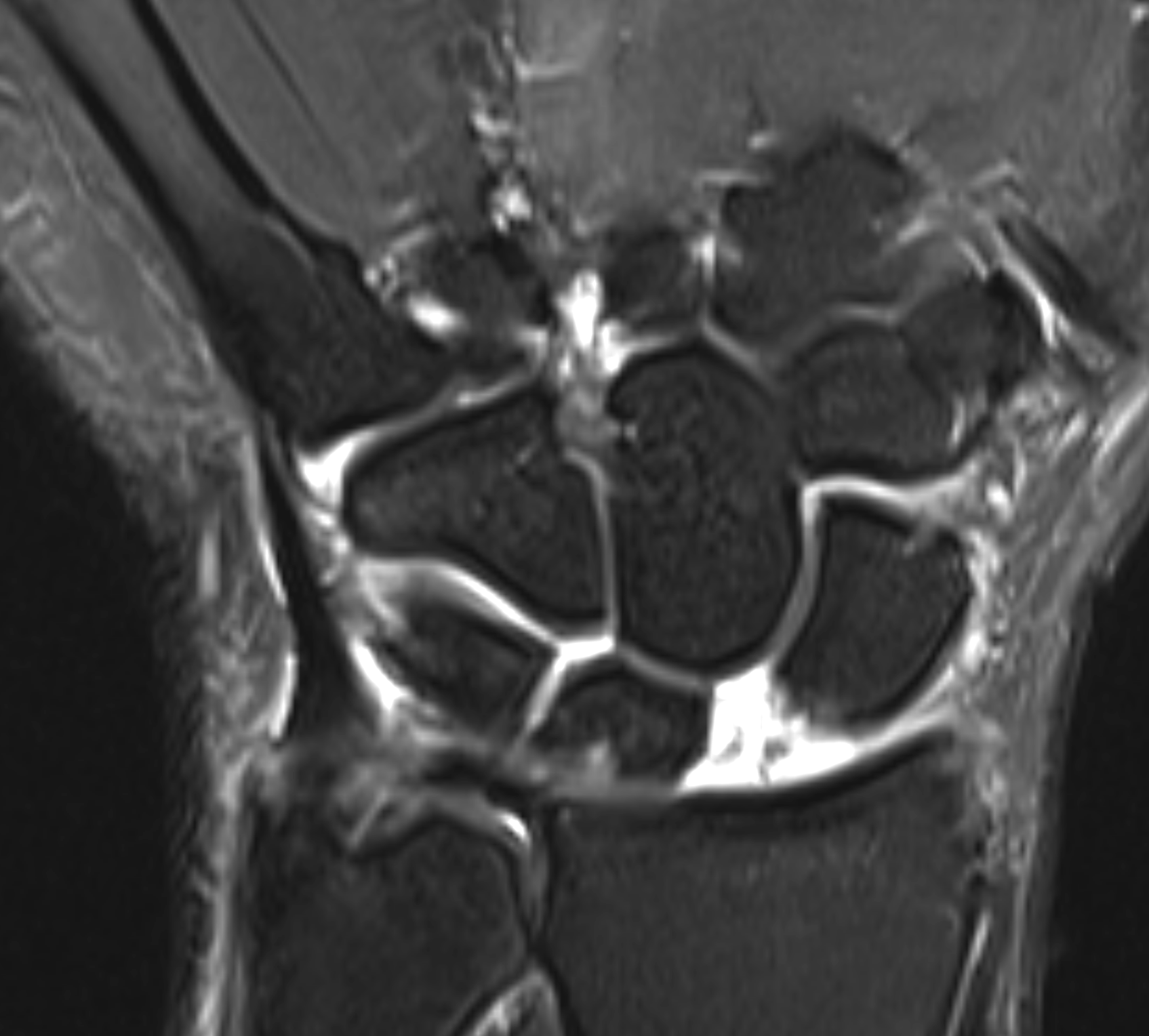
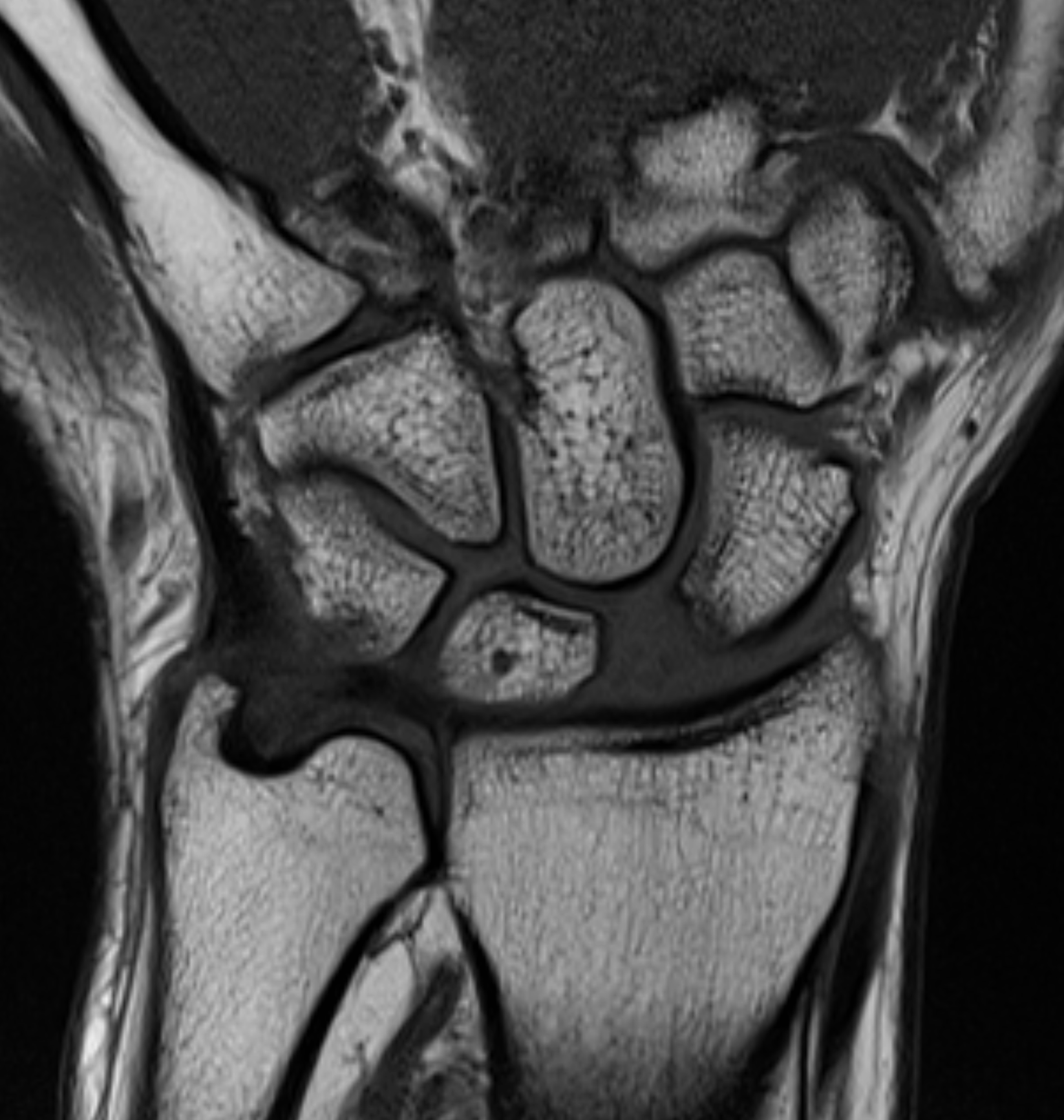
SLAC is the most common degenerative condition of the wrist.[11] Acute injury to the scapholunate ligament occurs in approximately 10% to 30% of intra-articular distal radius fractures (see Image 1, Scapholunate Ligament Tear T1 Sequence, and Image 2, Scapholunate Ligament Tear T2 Sequence).[12] Results from a study evaluating the epidemiology of SLAC of the wrist noted that patients with SLAC were more often males, had a history of wrist trauma, engaged in a manual job, and were often younger when compared to patients presenting with carpometacarpal osteoarthrosis.[13]
Pathophysiology
There is a well-established and recognized pathologic sequential algorithm for SLIL and SLAC of the wrist. The SLIL is a key wrist stabilizer and intercalating stabilizer to ensure regular, physiologic motion of the carpal bones, specifically the scaphoid and lunate bones.[14]
As the normal opposing forces at the scapholunate interval are lost, the scaphoid assumes an abnormally flexed position while the lunate pathologically deviates into extension.[15] This condition results in a dorsal intercalated segment instability (DISI deformity) pattern. The scapholunate angle increases to greater than 70° while the lunate is extended to greater than 10° past neutral. These abnormal flexion and extension positions alter the distribution of forces across the midcarpal and radiocarpal joints. Eventually, cartilage degeneration occurs, beginning with the radioscaphoid joint (recognized on radiographs at the radial styloid).
The pathologic cascade continues in an ulnar-based direction, with the final iteration yielding the collapse of the capitate proximally between a widened scapholunate interval (known as the "Terry Thomas sign"), and end-stage patterns include capitolunate arthritis.[16] Notably, the radiolunate joint remains spared in the SLAC pattern of degenerative deformity.
Histopathology
The SLIL consists of 3 regions: dorsal, proximal, and palmar. The dorsal and palmar regions histologically represent true capsular ligaments. The proximal region is made of fibrocartilage with occasional collagen fascicles. The dorsal region is histologically composed of transversely oriented collagen fascicles and is surrounded by connective tissue containing neurovascular bundles.[17]
History and Physical
When a patient presents after a fall on an outstretched hand, the clinician should consider the possibility of a SLIL injury. These injuries can be seen in isolation without fractures, but they can be present in association with distal radius or scaphoid fractures. Up to 30% of distal radius fractures have some degree of injury to the SL region. Aside from wrist trauma, SLIL secondary injuries may occur from other falls on the ipsilateral extremity (eg, a fall on the elbow), SLIL compromise secondary to underlying inflammatory arthritis, or SLIL iatrogenic compromise that may occur following excessive capsular excision when removing dorsal ganglion cysts.[18][9]
Patients will likely present with some degree of pain, although not all SLAC wrists are symptomatic. Pain is common, may be aggravated by heavy use, and is sometimes associated with a clunking sensation during movement.[15] There will usually be a decreased range of motion in the wrist and weakness in grip strength.
The external appearance of scapholunate instabilities may not be evident. Even in the acute phase, swelling may be moderate. When the patient presents with scapholunate advanced collapse, however, pain with provocative movements will usually be present. A scaphoid shift test is the passive mobilization of the dysfunctional scapholunate joint. This test is valuable in determining the presence of abnormal radioscaphoid subluxation, reproducing the patient's pain, and the reason they are presenting to the clinician.[19] A positive scaphoid shift test is said to be diagnostic of scapholunate instability.
To perform the scaphoid shift (eg, Watson) test, firm pressure is applied to the palmar tuberosity of the scaphoid while the wrist is moved from ulnar to radial deviation. In normal wrists, the scaphoid cannot flex because of the external pressure from the examiner's thumb. A positive test is seen in a patient with a scapholunate tear or a lax wrist. When pressure on the scaphoid is removed, the scaphoid returns to position, and a characteristic "snapping" occurs.
A scapholunate ballottement test can also be performed.[20] The lunate is firmly stabilized with one hand's thumb and index finger, while the scaphoid, held with the other hand, is displaced dorsally and palmarly. A positive test elicits pain, crepitus, and excessive mobility of the scaphoid.
Evaluation
Imaging begins with standard PA and lateral wrist radiographs.[3] Bilateral clenched-fist comparison views may reveal a DISI with a relative widening of the scapholunate interval on the affected side. This radiograph should be taken and appreciated as acutely in the disease process.
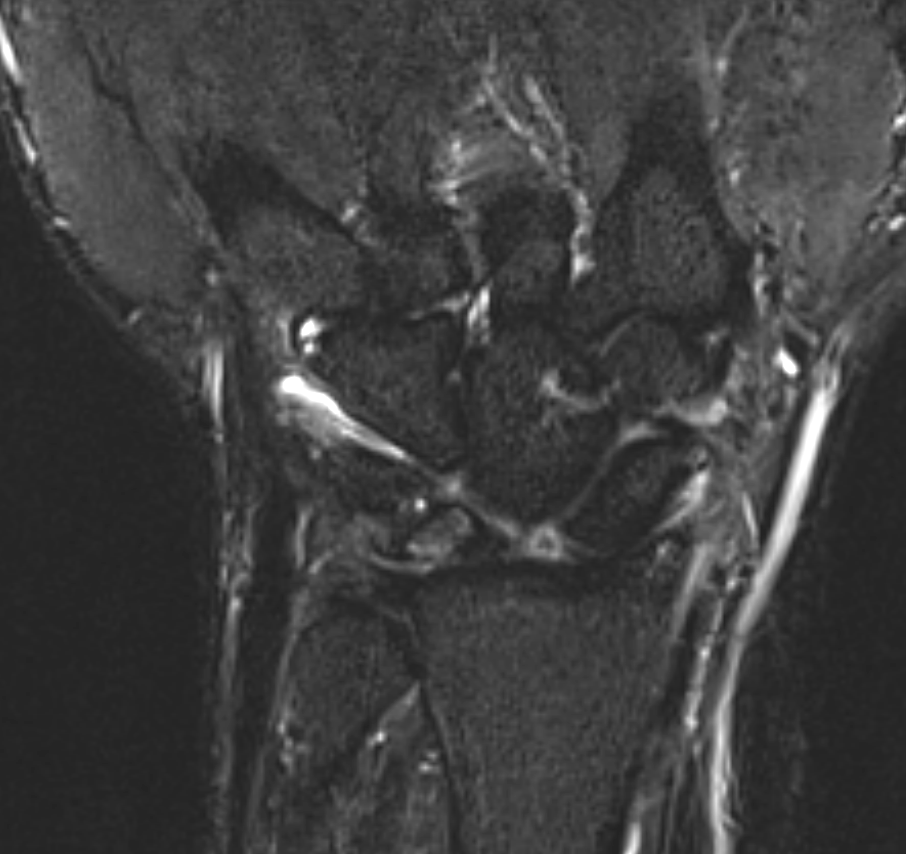
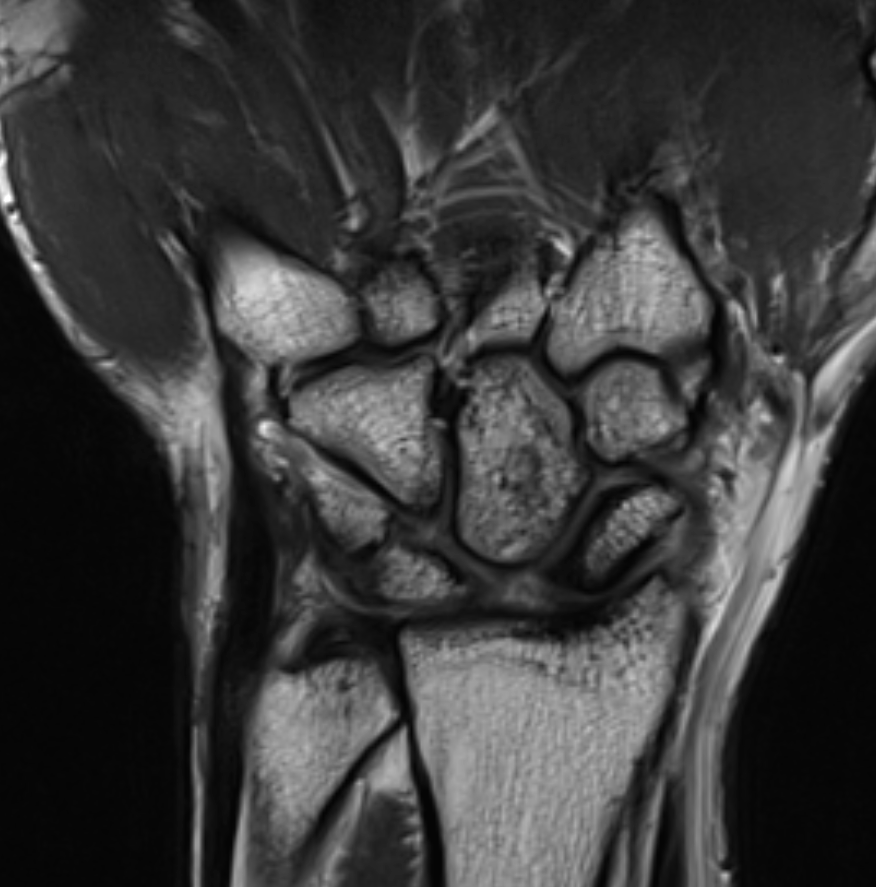
SLAC of the wrist will have an arthrosis pattern showing the progression of the injury. Watson and Ballet originally devised the classification of SLAC into 3 stages.[4] Localized arthrosis of the scaphoid fossa begins at the styloid tip (radial styloid beaking), indicative of a Stage I SLAC of the wrist. Progressive joint space narrowing and sclerosis affecting the entire scaphoid fossa of the distal radius is indicative of Stage II SLAC of the wrist. Stage III SLAC of the wrist entails sclerosis and narrowing the joint space between the lunate and capitate. Eventually, the capitate will migrate proximally into the space created by the scapholunate dissociation (see Image 3, Scapholunate Advanced Collapse T1 Sequence; Image 4, Scapholunate Advanced Collapse T2 Sequence; and Image 5, Scapholunate Advanced Collapse X-ray). Stage III SLAC of the wrist is synonymous with the "Terry Thomas sign." The lunate may fall into dorsiflexion (dorsal intercalated segment instability) and the scaphoid into flexion, but the integrity of the radiolunate articulation is preserved until late in the process. As per the original description, the radiolunate joint was always reported to be uninvolved in SLAC. However, many authors later reported radiolunate involvement in up to 80% of patients with SLAC.[21] Thus, a Stage IV SLAC was described to include pancarpal arthritis.[4]
Advanced Imaging Modalities
While CT scans are often not indicated, MRI scans may facilitate diagnosis in subtle clinical presentations. However, the latter are also usually unnecessary as radiographs are often sufficient. When obtained, an MRI may reveal thinning of the articular surfaces of the proximal scaphoid. This imaging may also show synovitis of the scaphoid facet of the distal radius and capitolunate joint and the overall radiocarpal and midcarpal joints. Sagittal images can demonstrate abnormal changes in the scaphoid and lunate bones' position and radioscaphoid incongruity.
Treatment / Management
Treatment of SLAC is complex and not always predictable. Nonoperative treatment can include nonsteroidal anti-inflammatory drugs, wrist splints, and possible corticosteroid injections for mild disease. The different surgical management options include radial styloidectomy, proximal row carpectomy, scaphoid excision and four-corner fusion, total wrist arthrodesis, and wrist arthroplasty.[9]
The stage-wise surgical treatment options include the following:[22][23]
Stage I SLAC Wrist
- Radial styloidectomy and scaphoid stabilization procedures
- PIN and AIN denervation
Stage II SLAC Wrist
- Proximal row carpectomy (PRC) is indicated to treat stage II (but not stage III) SLAC wrist
- Note that a PRC procedure is contraindicated in stage III deformity as there is an element of capitolunate arthritis, and patients inevitably report inferior outcomes in this clinical scenario
Stage III SLAC Wrist
- Scaphoid excision and 4-corner fusion
- Produces reliable, positive outcomes in patients suffering from debilitating stage II or stage III SLAC wrist deformity
- Outcomes are equivalent in the long-term when comparing this procedure to a PRC in stage II SLAC wrist deformity
- Wrist fusion
- Indicated in the setting of Stage III SLAC wrist or pancarpal arthritis (Stage IV SLAC)
- Wrist fusion procedures result in positive outcomes concerning pain relief, but wrist motion is compromised compared to scaphoid excision/4-corner fusion (the latter demonstrates preserved wrist motion following surgical reconstruction via the lunate/distal radius articulation at the lunate fossa)
Various fixation options are described in the 4-corner fusion procedure, which includes K-wires, screws, staples, metal non-locked plates, metal locked plates, and radiolucent locking plates. A recent systematic review compared the clinical outcomes and union rates using different fixation methods for 4-corner fusion. The review reported no difference in union rates or meaningful clinical difference in range of motion and grip strength among the various fixation options.[24] A systematic review to evaluate the long-term outcomes of 4-corner fusion found good long-term patient satisfaction and survivorship with only 6% conversion to total wrist fusion at a mean follow-up of 11 years.[25](A1)
There has been a lack of Level 1 evidence to compare PRC with 4-corner fusion for Stage II/III SLAC wrists. However, various systematic reviews and comparative studies have found equivalent results between the procedures.[26][27] PRC may be preferred in smokers as this is free of hardware-related complications and doesn't require bone fusion.[26] Four-corner fusion may be preferred in young patients below 35 years.[28](A1)
Although PRC and 4-corner fusion have been the mainstay of surgical management for the majority of SLAC cases until now, some new motion-preserving procedures have been recently described for SLAC wrists.[29] In a cadaveric study, arthroscopic proximal carpal row replacement using semitendinosus and gracilis graft (CARPUS procedure) was described as a safe and efficient motion-preserving procedure with maintained carpal height and is proposed to be especially useful for SLAC wrists with radius or capitate arthritis.[30] Also, 3-corner fusion (ie, the fusion of capitate, hamate, and lunate with triquetrum and scaphoid excision) has been reported as an alternative treatment for SLAC stage II/III wrists [31] (B3)
as well as arthroscopic interposition of the tendon between the radius and proximal carpal row. Arthroscopic interposition tendon arthroplasty (AITA) has been described for Stage II SLAC wrists. This condition requires a volar approach for the surgery and hence may be risky. To decrease the risks involved, modification requires a dorsal approach; the one-loop arthroscopic radiocarpal tendon inter-position (1L-ARTI) procedure has been recently reported.[32] Lately, 2-corner fusion (ie, the fusion of capitate and hamate) has been popularized as a motion-preserving surgery for SLAC wrists. A recent prospective, multi-center study compared the 2-corner fusion with 4-corner fusion surgery and found that functional scores and complications were similar between the 2 procedures. However, 2-corner fusion had better wrist mobility.[33](B2)
Differential Diagnosis
The differential diagnosis for SLAC wrist and SLIL injury is broad and includes the following various causes of wrist pain:[6]
- Scaphoid fracture
- Distal radial fractures
- Dorsal ganglion cyst
- Septic arthritis
- Avascular necrosis of the scaphoid
- Gout
- Pseudogout
- Rheumatoid arthritis
- Tear of the triangular fibrocartilage complex
- Kienbock disease
- Tenosynovitis
- Lunate fracture vs dislocation
- Dorsal intercalated segmental instability
Differentials such as crystalline arthropathies, can secondarily lead to the SLAC wrist.
Staging
Classification of advanced scapholunate collapse is broken down into 4 stages
- Stage I demonstrates radial styloid degenerative changes
- Stage II is represented by degenerative changes that involve the scaphoid fossa and the styloid
- Stage III has lunocapitate degenerative changes
- Stage IV is the last, indicated by pancarpal arthritis (This is somewhat controversial because some surgeons do not believe that advanced scapholunate collapse will result in pancarpal arthritis.)
Nevertheless, per the classical description, the radiolunate facet is always spared of arthrosis in scapholunate advanced collapse.[34] However, results from recent studies have reported radiolunate arthrosis in up to 80% of patients. A stage IV SLAC has been described that includes pancarpal arthritis.[4]
Prognosis
Most cases of scapholunate advanced collapse are in the beginning stages of progressive carpal destabilization around the lunate and result from an injury involving wrist hyperextension, ulnar deviation, and midcarpal supination. The postoperative prognosis is typically good. Results from one study showed that 91% of patients were satisfied with their postoperative result and would undergo the operation again, while 80% returned to their jobs.[35]
Complications
Complications exist for operative interventions including possible infection, failure of fusion, and additional procedures. Ashmead, et al, studied 100 patients who had surgically treated SLAC of the wrist and noted an average flexion/extension arc of 53% and grip strength of 80% of the uninjured wrist.[35] A nonunion rate of 3% was noted, and all of these cases healed after bone graft revision. A meta-analysis has shown a nonunion rate of 4.3%.[36] In another systematic review, the most common complication reported was dorsal radiocarpal impingement, representing 4.4% of cases with an overall complication rate of 13.5%.
Postoperative and Rehabilitation Care
After a 4-corner fusion, patients should be immobilized in a short-arm volar splint for 2 weeks. At this point, a custom splint is worn for an additional 6 weeks or until radiographic evidence of healing is confirmed.[37] Gentle finger range of motion and strengthening are started at 2 weeks, but wrist motion and strengthening are not initiated until radiographic confirmation of union. Patients should expect a 50% motion loss in wrist range of motion compared with the contralateral side. Grip strength should return to about 80% of the unaffected side.[38]
Deterrence and Patient Education
Most cases of SLAC of the wrist involve a chronic scapholunate ligament injury that has slowly progressed to collapse. During an initial presentation, especially after diagnosing scapholunate injury with imaging, an in-depth conversation with the patient is necessary to emphasize the long-term complications, including eventual collapse.
Pearls and Other Issues
Acute traumatic SLIL injuries can often be repaired despite even the most traumatic injuries resulting in an obliterated state of ligamentous integrity. In conditions caused by underlying arthritic conditions and inflammatory arthritis, the ligamentous and other pericapsular soft tissue structures are of significantly poor quality and can compromise overall healing and patient-reported outcomes.[36]
Enhancing Healthcare Team Outcomes
Scapholunate advanced collapse requires interprofessional communication between the patient, the clinician, and the hand therapists involved in care. The operations needed to treat this process are typically complex and require hand therapy post-operatively. Managing patient expectations is also critical. Four-corner arthrodesis is a complex procedure that can have long-term implications on a patient's occupational functionality. An informed decision with knowledge of outcomes should be discussed with the patient to establish whether surgery is advisable, especially in those with significant comorbidities.
Alternative treatments should also be addressed. A preassessment that includes blood tests, an electrocardiogram, and further imaging to guide the surgical course can be obtained. An anesthetic review by an anesthesiologist or certified nurse anesthetist should also be performed in patients with comorbidities, as well as guiding pain relief as appropriate. A physical therapy assessment during recovery is also essential in the immediate and long-term postoperative course. Follow-up clinic visits also play a role in expediting the correction of postoperative complications.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Shah CM, Stern PJ. Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist arthritis. Current reviews in musculoskeletal medicine. 2013 Mar:6(1):9-17. doi: 10.1007/s12178-012-9149-4. Epub [PubMed PMID: 23325545]
Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. The Journal of hand surgery. 1984 May:9(3):358-65 [PubMed PMID: 6725894]
Tischler BT, Diaz LE, Murakami AM, Roemer FW, Goud AR, Arndt WF 3rd, Guermazi A. Scapholunate advanced collapse: a pictorial review. Insights into imaging. 2014 Aug:5(4):407-17. doi: 10.1007/s13244-014-0337-1. Epub 2014 Jun 3 [PubMed PMID: 24891066]
McLean A, Taylor F. Classifications in Brief: Watson and Ballet Classification of Scapholunate Advanced Collapse Wrist Arthritis. Clinical orthopaedics and related research. 2019 Mar:477(3):663-666. doi: 10.1097/CORR.0000000000000451. Epub [PubMed PMID: 30179931]
Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: proximal row carpectomy versus four-corner arthrodesis. The Journal of hand surgery. 1995 Nov:20(6):965-70 [PubMed PMID: 8583069]
Trehan SK, Lee SK, Wolfe SW. Scapholunate Advanced Collapse: Nomenclature and Differential Diagnosis. The Journal of hand surgery. 2015 Oct:40(10):2085-9. doi: 10.1016/j.jhsa.2015.06.110. Epub 2015 Aug 1 [PubMed PMID: 26243321]
Chen C, Chandnani VP, Kang HS, Resnick D, Sartoris DJ, Haller J. Scapholunate advanced collapse: a common wrist abnormality in calcium pyrophosphate dihydrate crystal deposition disease. Radiology. 1990 Nov:177(2):459-61 [PubMed PMID: 2217785]
Level 2 (mid-level) evidenceTaniguchi Y, Yoshida M, Tamaki T. X-ray characteristics of wrists in calcium pyrophosphate crystal deposition disease. Is pseudogout a major cause of scapholunate advanced collapse? Journal of hand surgery (Edinburgh, Scotland). 1997 Oct:22(5):659-61 [PubMed PMID: 9752927]
Strauch RJ. Scapholunate advanced collapse and scaphoid nonunion advanced collapse arthritis--update on evaluation and treatment. The Journal of hand surgery. 2011 Apr:36(4):729-35. doi: 10.1016/j.jhsa.2011.01.018. Epub [PubMed PMID: 21463735]
Brody GA. Commentary: scapholunate ligament injuries in professional football players. Hand clinics. 2012 Aug:28(3):267-8. doi: 10.1016/j.hcl.2012.05.004. Epub 2012 Jun 22 [PubMed PMID: 22883861]
Level 3 (low-level) evidenceTraverso P, Wong A, Wollstein R, Carlson L, Ashmead D, Watson HK. Ten-Year Minimum Follow-Up of 4-Corner Fusion for SLAC and SNAC Wrist. Hand (New York, N.Y.). 2017 Nov:12(6):568-572. doi: 10.1177/1558944716681949. Epub 2016 Dec 5 [PubMed PMID: 29091493]
Richards RS, Bennett JD, Roth JH, Milne K Jr. Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. The Journal of hand surgery. 1997 Sep:22(5):772-6 [PubMed PMID: 9330132]
Murphy BD, Nagarajan M, Novak CB, Roy M, McCabe SJ. The Epidemiology of Scapholunate Advanced Collapse. Hand (New York, N.Y.). 2020 Jan:15(1):23-26. doi: 10.1177/1558944718788672. Epub 2018 Jul 13 [PubMed PMID: 30003815]
Lee DJ, Elfar JC. Carpal Ligament Injuries, Pathomechanics, and Classification. Hand clinics. 2015 Aug:31(3):389-98. doi: 10.1016/j.hcl.2015.04.011. Epub [PubMed PMID: 26205700]
Konopka G, Chim H. Optimal management of scapholunate ligament injuries. Orthopedic research and reviews. 2018:10():41-54. doi: 10.2147/ORR.S129620. Epub 2018 Aug 6 [PubMed PMID: 30774459]
Stevenson M, Levis JT. Image Diagnosis: Scapholunate Dissociation. The Permanente journal. 2019:23():. pii: 18-237. doi: 10.7812/TPP/18-237. Epub [PubMed PMID: 30939288]
Berger RA. The gross and histologic anatomy of the scapholunate interosseous ligament. The Journal of hand surgery. 1996 Mar:21(2):170-8 [PubMed PMID: 8683042]
Mehdian H, McKee MD. Scapholunate instability following dorsal wrist ganglion excision: a case report. The Iowa orthopaedic journal. 2005:25():203-6 [PubMed PMID: 16089099]
Level 3 (low-level) evidenceLane LB. The scaphoid shift test. The Journal of hand surgery. 1993 Mar:18(2):366-8 [PubMed PMID: 8463609]
Omokawa S, Iida A, Kawamura K, Nakanishi Y, Shimizu T, Kira T, Onishi T, Hayami N, Tanaka Y. A Biomechanical Perspective on Distal Radioulnar Joint Instability. Journal of wrist surgery. 2017 May:6(2):88-96. doi: 10.1055/s-0037-1601367. Epub 2017 Mar 22 [PubMed PMID: 28428909]
Level 3 (low-level) evidenceZinberg EM, Chi Y. Proximal row carpectomy versus scaphoid excision and intercarpal arthrodesis: intraoperative assessment and procedure selection. The Journal of hand surgery. 2014 Jun:39(6):1055-62. doi: 10.1016/j.jhsa.2014.03.032. Epub 2014 May 5 [PubMed PMID: 24799142]
Level 2 (mid-level) evidenceYeo JH, Kim JY. Surgical Strategy for Scaphoid Nonunion Treatment. The journal of hand surgery Asian-Pacific volume. 2018 Dec:23(4):450-462. doi: 10.1142/S2424835518300049. Epub [PubMed PMID: 30428803]
Elgammal A, Deglmann CJ, Celigoj V, Lukas B. Midterm Results of Four-Corner Fusion Using Dorsal Circular Plate Fixation. Journal of wrist surgery. 2018 Jul:7(3):262-266. doi: 10.1055/s-0037-1607072. Epub 2017 Oct 16 [PubMed PMID: 29922506]
Hayes E, Cheng Y, Sauder D, Sims L. Four-Corner Arthrodesis With Differing Methods of Osteosynthesis: A Systematic Review. The Journal of hand surgery. 2022 May:47(5):477.e1-477.e9. doi: 10.1016/j.jhsa.2021.06.002. Epub 2021 Jul 10 [PubMed PMID: 34253392]
Level 1 (high-level) evidenceAndronic O, Nagy L, Burkhard MD, Casari FA, Karczewski D, Kriechling P, Schweizer A, Jud L. Long-term outcomes of the four-corner fusion of the wrist: A systematic review. World journal of orthopedics. 2022 Jan 18:13(1):112-121. doi: 10.5312/wjo.v13.i1.112. Epub 2022 Jan 18 [PubMed PMID: 35096541]
Level 1 (high-level) evidenceAhmadi AR, Duraku LS, van der Oest MJW, Hundepool CA, Selles RW, Zuidam JM. The never-ending battle between proximal row carpectomy and four corner arthrodesis: A systematic review and meta-analysis for the final verdict. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2022 Feb:75(2):711-721. doi: 10.1016/j.bjps.2021.09.076. Epub 2021 Oct 23 [PubMed PMID: 34802951]
Level 1 (high-level) evidenceAmer KM, Thomson JE, Vosbikian MM, Ahmed I. Four-Corner Arthrodesis Versus Proximal Row Carpectomy for Scapholunate Advanced Collapse: A Systematic Literature Review and Meta-analysis. Annals of plastic surgery. 2020 Dec:85(6):699-703. doi: 10.1097/SAP.0000000000002398. Epub [PubMed PMID: 32384352]
Level 1 (high-level) evidenceKruse K, Fowler JR. Scapholunate Advanced Collapse: Motion-Sparing Reconstructive Options. The Orthopedic clinics of North America. 2016 Jan:47(1):227-33. doi: 10.1016/j.ocl.2015.08.002. Epub [PubMed PMID: 26614936]
Zhang Y, Gillis JA, Moran SL. Management of scapholunate advanced collapse and scaphoid nonunion advanced collapse without proximal row carpectomy or four corner fusion. The Journal of hand surgery, European volume. 2021 Jan:46(1):50-57. doi: 10.1177/1753193420973322. Epub 2020 Nov 17 [PubMed PMID: 33202162]
Artuso M, Protais M, Soubeyrand M. Arthroscopic proximal carpal row replacement by semitendinosus and gracilis graft (CArpus Row Plasty Using the Semitendinosus: CARPUS procedure). An anatomical study of 16 cases. Orthopaedics & traumatology, surgery & research : OTSR. 2022 Nov:108(7):103124. doi: 10.1016/j.otsr.2021.103124. Epub 2021 Oct 23 [PubMed PMID: 34700056]
Level 3 (low-level) evidenceColman M, El Kazzi W, Salvia P, Feipel V, Schuind F. Three-Corner Arthrodesis (lunate - hamate - capitate) : clinical and kinematical evaluation. Acta orthopaedica Belgica. 2020 Dec:86(4):717-723 [PubMed PMID: 33861922]
DE Villeneuve Bargemon JB, Merlini L, Mathoulin C, Levadoux M. Arthroscopic Radiocarpal Tendinous Inter-Position for Grade 2 Scapholunate Advanced Collapse - Surgical Technique. The journal of hand surgery Asian-Pacific volume. 2022 Oct:27(5):889-894. doi: 10.1142/S2424835522710035. Epub 2022 Sep 28 [PubMed PMID: 36184255]
Duraku LS, Hundepool CA, Hoogendam L, Selles RW, van der Heijden BEPA, Colaris JW, Hovius SER, Zuidam JM, Hand-Wrist Study Group. Two-Corner Fusion or Four-Corner Fusion of the Wrist for Midcarpal Osteoarthritis? A Multicenter Prospective Comparative Cohort Study. Plastic and reconstructive surgery. 2022 Jun 1:149(6):1130e-1139e. doi: 10.1097/PRS.0000000000009116. Epub 2022 Apr 11 [PubMed PMID: 35404339]
Level 2 (mid-level) evidenceChahla J, Schon JM, Olleac R, Senes S, Arroquy D, Dean CS, Clembosky G, Muratore A. Stage III Advanced Wrist Collapse Treatment Options: A Cadaveric Study. Journal of wrist surgery. 2016 Nov:5(4):265-272 [PubMed PMID: 27777816]
Ashmead D 4th, Watson HK, Damon C, Herber S, Paly W. Scapholunate advanced collapse wrist salvage. The Journal of hand surgery. 1994 Sep:19(5):741-50 [PubMed PMID: 7806794]
Level 2 (mid-level) evidenceSiegel JM, Ruby LK. A critical look at intercarpal arthrodesis: review of the literature. The Journal of hand surgery. 1996 Jul:21(4):717-23 [PubMed PMID: 8842977]
Lamas Gomez C, Proubasta Renart I, Llusa Perez M. Relationship Between Wrist Motion and Capitolunate Reduction in Four-Corner Arthrodesis. Orthopedics. 2015 Nov:38(11):e1040-5. doi: 10.3928/01477447-20151020-14. Epub [PubMed PMID: 26558669]
Trail IA, Murali R, Stanley JK, Hayton MJ, Talwalkar S, Sreekumar R, Birch A. The long-term outcome of four-corner fusion. Journal of wrist surgery. 2015 May:4(2):128-33. doi: 10.1055/s-0035-1549277. Epub [PubMed PMID: 25945298]