Introduction
The spinal cord study is one of the most complex yet quite a fascinating part of the nervous system. Its complex connections, the development defects, the lesions, and clinical presentation are quite overwhelming and warrants a better understanding of its anatomical and physiological nature. This topic has received extensive study and revealed many minute details. But it quite acknowledgeable that still a lot is unknown, and discussing these details is beyond this article.
The spinal cord is an integral aspect of the central nervous system, which is cylindrical and elongated in structure. It is one of the most important contents of the vertebral canal. It presents as an extension of the lower part of the brain stem, i.e., the medulla oblongata. It begins at the first cervical vertebra level and ends at the first lumbar vertebra in an adult.[1] But in the case of young children, the spinal cord is relatively longer relative to the length of the vertebral column. Here it usually ends much lower at the level of the upper border of the third lumbar vertebrae.
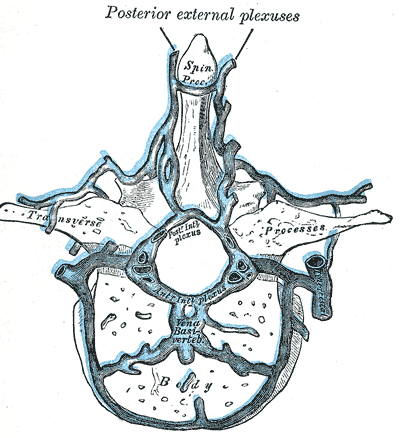
Like the brain, the very delicate and sensitive spinal cord has strong protection from a strong bony-cage formed by the vertebral arch and body of the vertebras. Together they form a long spinal column (spinal cavity) within which the spinal cord will be present. The spinal cord houses millions of neurons, and their bundled fibers are running as tracts that are either ascending or descending.[2] The three meninges completely cover the spinal cord - the dura mater, arachnoid mater, and pia mater (from outside to inside). Further protection and the cushioning effect is provided by the presence of the cerebrospinal fluid (CSF) present within the subarachnoid space,
The spinal cord gives rise to 31 pairs of spinal nerves, which supply mainly the trunk and the limbs. These spinal nerves are mixed nerves having a motor component that helps control all the limbs' voluntary muscles and trunk. They also have a sensory component that helps in receiving the sensory information from these areas. Hence, it is crucial to understand the basic anatomy for better interpretation of the clinical presentation and its pathology in any spinal cord lesion.[3]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
External Features
The spinal cord is a long cylindrical extension of the central nervous system within the vertebral column's cavity. It is approximately 42.3 cm in length in males and 38.9 cm in females.[1] Even though the spinal cord is almost symmetrical, it is enlarged in a fusiform shape in two regions in the form of cervical and lumbosacral enlargements. In the cervical area, this fusiform enlargement is due to the exit of many nerves forming a plexus (the brachial plexus) supplying the upper limb's muscles. This enlargement spreads from the fourth cervical segment to the second thoracic segment. The maximum transverse diameter is present at the level of the C5 segment.[4] Similarly, the lower thoracolumbar enlargement gives rise to a plexus of nerves supplying the lower limb muscles in the form of the lumbosacral plexus. This second enlargement extends from the second lumbar segment to the third sacral segment of the spinal cord.
The lowermost part of the spinal cord tapers in a cone-like fashion and is thus termed the conus medullaris. From the apex of this conus medullaris, an extension of the pia mater, i.e., the filum terminale, descends and gets attached to the coccyx's posterior surface. In midline anteriorly, the cord shows the presence of a deep longitudinal cleft, which is the anterior median fissure. This fissure is the site of the presence of the anterior spinal artery. Similarly, the posterior surface demonstrates a shallow furrow in the midline, the posterior median sulcus. In combination, the anterior median fissure and the posterior median sulcus will divide the whole of the spinal cord into two symmetrical halves - the right and left half, which one can better appreciate in a transverse section.
Further, we can appreciate the shallow depressions on either side as anterolateral and posterolateral sulci. The anterolateral sulcus will be the site of exit of the ventral (motor) roots of the spinal cord. The posterolateral sulcus will be the site for the entry of dorsal (sensory) roots of the spinal cord.
Transverse Section of the Spinal Cord
On sectioning a spinal cord, two distinct areas are evident with the naked eyes, an inner grey matter, and an outer white matter. The grey matter indicates the collection of cell bodies of neurons. The white matter is the collection of the fibers running through the spinal cord.
Grey Matter: When taking a transverse section of the spinal cord, in the middle is the grey matter, which appears roughly in the form of an H (butterfly) shaped mass. The grey matter is divisible on each half of the cord into a larger ventral mass – ventral grey column (anterior/ventral horn) and an elongated dorsal grey column (posterior/dorsal horn). In some parts of the cord (thoracic and upper lumbar regions), a small lateral projection of a grey mater is present between the ventral and dorsal columns. This structure is a lateral grey column (lateral horn). The cells in the anterior horn are called anterior horn cells. The grey matter on both the left and right halves connect by the grey commissure, which contains the central canal. This canal communicates above into the fourth ventricle. The central canal expands at the lower end in the conus medullaris to form the terminal ventricle. The central canal contains CSF and is lined by ependymal cells.[5] For experimental purposes, the grey matter divides into ten laminae. The laminae I to VI occupy the posterior grey column.[6] The lamina VII is in the intermediate region, lamina VIII remains confined to the medial part of the anterior grey column, and lamina IX occupies the lateral part of the anterior grey column. The area around the central canal is distinguished as lamina X.[7] Each of these laminae has unique connections and functions.
White Matter: Surrounding the grey mater superficially, we find the white matter. On either side, the white matter, which is medial to the posterior grey column, forms the dorsal (posterior) funiculus. The white matter that is medial and ventral to the ventral (anterior) grey column forms the ventral (anterior) funiculus. While the white matter lateral to the anterior and posterior grey column forms the lateral funiculus. Each of these areas contains bundles of nerves in tracts that can be ascending or descending.[8] This region is called white because it looks pale due to the presence of myelinated nerve fibers.
There is variation in the amount of the areas occupied by the white and grey matter in different spinal cord levels. The space occupied by the grey matter increases progressively, and the region for white matter decreases as we go craniocaudally.
Even the arrangement of fibers in each funiculus of the white matter is unique. When observing a transverse section of the spinal cord, we find that the posterior funiculus will have ascending sensory fibers arranged into two regions called fasciculus gracilis and fasciculus cuneatus. The anterior funiculus will contain descending motor fibers of olivospinal, tectospinal, lateral vestibulospinal, medial vestibulospinal, anterior corticospinal, anterior spinothalamic, spino-olivary, spino-tectal, and reticulospinal tracts. The lateral funiculi will contain anterior and posterior spinocerebellar, lateral spinothalamic, spino-reticular, lateral corticospinal, rubrospinal, and lateral reticulospinal tracts.
Arrangement of the Spinal Nerves and Segments
The spinal cord gives rise to a series of spinal nerves on either side. The spinal nerves are mixed nerves and have two roots, an anterior and posterior root. Sometimes they are also termed as ventral and dorsal root, respectively. The anterior or ventral root is motor in nature and gives efferent fibers to skeletal muscles. Sometimes they also contain preganglionic autonomic fibers to blood vessels and internal organs. The posterior or dorsal root is sensory and contains afferent fibers from peripheral receptors from the skin, bones, joints, muscles, and internal organs. Researchers discovered this in the 19th century, and it is known as Bell-Magendie Law.[9]
Each root is an aggregation of the number of rootlets arising from a part of the spinal cord, and that area is called the spinal segment. The spinal nerves are 31 pairs – 8 pairs of cervical, 12 pairs of thoracic, five pairs of lumbar, five pairs of sacral, and one pair of coccygeal nerves.[10] Thus there are 31 pairs of spinal segments. The dorsal nerve roots enter the spinal cord along the postero-lateral sulcus and ventral roots along the anterolateral sulcus. The dorsal root shows a swelling called dorsal nerve root ganglion (spinal ganglion). This ganglion contains cell bodies of pseudounipolar sensory neurons.
Due to the vertebral column and spinal cord's developmental differences, spinal segments do not lie opposite their corresponding vertebrae. The length and obliquity of the spinal nerves increase progressively caudally before their exit through the intervertebral foramina. This knowledge is vital in laminectomy to relieve spinal cord compression due to traumas and tumors. At the conus medullaris, these roots of nerves in pairs coming from the lower lumbar, sacral, and coccygeal nerves form a bundle of nerves that resembles the tail of a horse and is thus known as cauda equina.
Covering of Spinal Cord
Three meninges surround the spinal cord. From outside inwards, they are the dura mater (thick fibrous membrane), the arachnoid mater, and the pia mater. The space present between the dura and the vertebral canal wall is called the extradural (epidural) space. The space between the dura and arachnoid mater is said to be subdural space. Subarachnoid space is present between the pia mater and arachnoid mater. This space is filled with cerebrospinal fluid. The pia mater is adherent to the spinal cord and extends along with the cord up to the lower border of the L1 vertebra where the spinal cord end. But dura and arachnoid mater extend up to the second sacral vertebra. Between these two vertebral levels, subarachnoid space has spinal nerve roots forming cauda equina. One should remember that the pia mater does not end at L1 but extends beyond this as the thin midline structure called filum terminale, and finally attached to the posterior surface of the coccyx.
The spinal cord's most important function is to receive, integrate, associate the input, and produce a reflex response.
Embryology
The ectoderm of a trilaminar staged embryo will thicken at the midline to be called the neural plate. This plate depresses to form a neural groove whose ends later fuse to convert it into a neural tube. This tube enlarges at the cranial end and remains tubular at the caudal part. The cranial part forms the brain. The spinal cord develops from the caudal tubular part of this neural tube.[11][12] Maternal dietary supplement of foliate plays a vital role in the closure of the neural tube in the early stages.[13] The neural tube differentiates itself into the ependymal, mantle, and marginal layers from inside out. The mantle proliferates rapidly to form the gray matter, divided into a ventral basal lamina and dorsal alar lamina by the sulcus limitans. The basal lamina develops into the motor area, giving rise to anterior and lateral horns and all the neurons within. The alar lamina develops as a sensory area that gives rise to the posterior horn and all the neurons within it. The cavity within will narrow down to form the central canal. The neural crest cells help in the formation of the ventral sympathetic ganglion and dorsal root ganglion.
The axons of the neuron start occupying the marginal zone during the fourth week of gestation. The axons now bundle up to form ascending and descending tracts within the marginal zone, further subdividing this region into anterior, posterior, and lateral white columns. With the development of limb buds, there is a simultaneous development of the cervical and lumbar enlargement at the fifth to sixth weeks of gestation. The tracts start forming during the third month, and the corticospinal tract appears by the fifth month of intra-uterine life. The myelination begins at the fourth month of embryonic life from short intersegmental tracts of the spinal cord and continues up to two to three years after birth till the child starts walking.
The vertebral bodies and the muscles surrounding the spinal cord develop from the surrounding dermatomes. The incomplete development of vertebras leads to several congenital anomalies that this article describes in clinical significance. The length of the spinal cord and the vertebral column are equal in size up to the third month of fetal life. Later the vertebral column develops rapidly in comparison to the spinal cord. Thus the spinal cord ends at a higher level within the vertebral canal. It has receded to the third lumbar vertebra at birth and reaches the first lumbar vertebra by puberty. Thus the spinal nerves arise from the spinal cord at a much higher level than their exit outside through the intervertebral foramina.
Many studies indicate a crucial role of some critical signaling factors in developing the spinal cord, like retinoic acid, bone morphogenetic proteins, Wnt, fibroblast growth factors, and Hedgehog proteins.[14][15] It is now known whether vascular endothelial growth factors (VEGFs) play a significant role in developing the vessels supplying the spinal cord.[16]
Blood Supply and Lymphatics
Arterial Supply of the Spinal Cord
The spinal cord receives its blood supply from three longitudinal channels that extend along the length of the spinal cord, i.e., one anterior spinal artery and two posterior spinal arteries. The anterior spinal artery runs along the anterior median fissure, and the smaller two posterior spinal arteries pass through the posterolateral sulcus on either side. The vertebral arteries are the main source from where these spinal arteries branch. But it should be remembered that the blood coming from the vertebral arteries supply only the cord's cervical segments. In the lower down region, the spinal arteries receive blood through radicular arteries that reach the cord and the roots of the spinal nerves. The radicular arteries are actually branches from many arteries like the vertebral, cervical, intercostal, lumbar, and even sacral arteries. The largest radicular feeder from the left posterior intercostal artery to the anterior spinal artery is between T9 and T12, called the artery of Adamkewicz. All the radicular and spinal arteries anastomose with each other to form an anastomotic pial plexus called vasocorona.[17] But the better part of the spinal cord is supplied by the anterior spinal artery and its branches.
Veinous Drainage of the Spinal Cord
The veins draining the spinal cord are arranged in the form of a network of six longitudinal channels, i.e., an anteromedian vein, a posteromedian vein, and a pair of anterolateral and posterolateral veins.[17] As the name indicates, the anteromedian and posteromedian channels will be present in the midline anteriorly and posteriorly, respectively, relative to the spinal cord. The anterolateral and posterolateral channels are paired and lie as per their names on either side of the spinal cord. All these channels are interconnected to form a plexus of veins of venous vasocorona. The venous blood from these veins drains into radicular veins. These radicular veins finally drain into the segmental veins.
Nerves
Spinal Nerves
The nerves are of two types based on their origin - the cranial and spinal nerves. Those nerves which begin in the cerebrum or the brain stem are called cranial nerves. There are twelve pairs of cranial nerves. The nerves coming from the spinal cord are called the spinal nerves. There are 31 pairs of spinal nerves coming from the spinal cord and spread on either side of the vertebral column. They are classified into cervical, thoracic, lumbar, sacral, and coccygeal nerves. The cervical nerves are in eight pairs; the thoracic are twelve pairs, the lumbar and sacral nerves are in five pairs, and one pair of coccygeal nerves.
Spinal Tracts
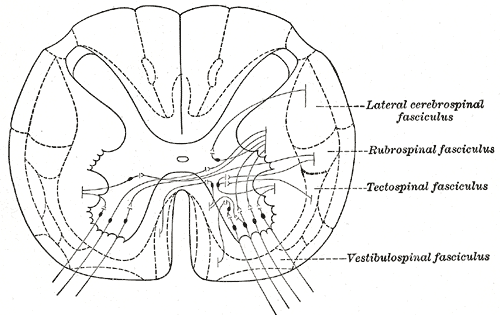
When we study the transverse section of a spinal cord, we can appreciate many spinal tracts within the white matter. They are categorized into two types - ascending and descending tracts. The descending tracks are mainly motor, and the ascending tracks are sensory.
Some of the most essential descending (motor) tracts passing through the spinal cord are as follows:
- Cortico-spinal tract (This is also known as the pyramidal tract, which is the most important of the motor tracts)
- Tectospinal tract
- Rubrospinal tract
- Vestibulospinal tract
- Reticulospinal tracts
- Olivospinal tract
Some of the most important ascending (sensory) tracts are as follows:
- Lateral spinothalamic tract (spinal lemniscus)
- Anterior spinothalamic tract (medial lemniscus)
- Trigeminal lemniscus
- Lateral lemniscus
- Spinotectal tract
- Spino-olivary tract
- Ventral spinocerebellar tract
- Dorsal spinocerebellar tract
- Dorsolateral tract (of Lissauer)
- Spino-cervico-thalamic tract
Here we will explain one descending tract in detail to better understand the whole course.
The cortico-spinal tract arises mainly from the motor area of the cerebral cortex (area 4) with some contribution from the premotor area (area 6), somatosensory area (area 3, 2, 1), and parietal cortex (area 5). The fibers run through the internal capsule's posterior limb and then occupy the middle part of the midbrain's crus cerebri. The tract then occupies the ventral part of the pons and descends through the pyramids in the medulla. At the lower end of the medulla, almost 70 to 80% of the fibers cross to the opposite side of the spinal cord, called the pyramidal (motor) decussation. These crossed fibers enter the lateral funiculus of the spinal cord and continue as the lateral corticospinal tract. They end at various levels of the spinal cord's grey matter by synapsing with internuncial neurons of dorsal and ventral columns. The remaining 20 to 30% of the corticospinal tract fibers, which have not crossed, will descend within the anterior funiculus as the anterior corticospinal tract. Finally, these anterior corticospinal tract fibers too cross to the opposite side at the appropriate levels. Thus all fibers of the corticospinal tract eventually cross to the opposite side and connect the cerebral cortex of one side with the ventral horn cells of the opposite part of the spinal cord. These fibers are called upper motor neurons. The fibers starting in the ventral horn cells and descending downwards will be called lower motor neurons. This knowledge is vital as the clinical presentation of upper and motor neuron lesions are quite different.[18] Any minor injury of these fibers will lead to widespread paralysis of the muscles supplied.
Spinal Cord Lesions
Lesions of the spinal cord fall into the following categories:
- Lesions of the afferent system:
- Dorsal nerve roots
- Spinothalamic tract
- Posterior white funiculus
- Syringomyelia
- Lesions of the efferent system:
- Upper motor neuron lesions
- Lower motor neuron lesions
- Lesions involving upper and lower motor neurons:
- Lesions involving posterior and lateral funiculi
- Thrombosis of the spinal artery
- Hemisections (Brown-Sequard syndrome)
- Transections
- Hereditary diseases: Friedreich ataxia
Details of some of these lesions will be discussed in the section of Clinical Significance.
Physiologic Variants
The neurotransmitters essential in the modulation of motor and sensory function are serotonin, noradrenaline, and dopamine. These have been observed to decrease spinal cord injuries depending on their incomplete damage to complete spinal injuries.[19]
Surgical Considerations
Lumbar Puncture: This is a clinical procedure by which the CSF is drawn from the subarachnoid space for diagnostic and therapeutic purposes.[20] Here the needle is introduced from the area between the second and third lumbar vertebra into subarachnoid space, and CSF is drawn (in the case of adults). In the case of children, it will be much more below between the third and fourth lumbar space. Even during the age of imaging, the CSF analysis remains consistent in the diagnosis of many significant neurological disorders like Alzheimer's disease, subarachnoid hemorrhage, and others. It also remains the most practical method to differentiate between bacterial and viral meningitis.[20]
Epidural Injections: Epidural anesthesia is a technique where a needle is passed into the epidural to give an analgesic into this space. This method is commonly used to relieve pain in certain conditions like cesarian sections, major abdominal surgeries, thoracotomy, and other conditions.[21][22]
Subdural Injections: It is an observation the injections intended for the epidural space often go unintentionally into the subdural space and lead to many complications.[23]
Paravertebral Block: This is a technique where the nerves are blocked at their roots or plexuses surrounded by the dura mater within the epidural space. These are similar to epidural blocks and done at the cervical, thoracic, lumbar, and sacral regions.[24]
Clinical Significance
Any spinal cord lesion can generally be localized quite easily by understanding the anatomy. There is usually impairment or sensory or motor functions in the lower extremities. It is always important to identify the motor or sensory level to determine the lesion's exact site. In general, the best imaging modality for any suspected spinal cord lesion is magnetic resonance imaging(MRI).
- Meningitis: It is the infection of meninges (coverings) of the brain. It can be bacterial or viral. Some of the most common being:
- Bacterial meningitis: It can be because of bacterias' infection such as Streptococcus pneumoniae, Neisseria meningitides, Listeria monocytogenes, E. coli, Pseudomonas aeruginosa, Klebsiella, Enterobacter, Staphylococcus aureus, and Staphylococcus albus. Streptococcus pneumoniae and Neisseria meningitides are known to be the most common.[25]
- Tubercular meningitis: It is due to infection by Mycobacterium tuberculosis. It presents with typical features like a stiff neck, fever, increased intracranial pressure, and headache. The CSF shows increased proteins and decreased glucose levels.[26] It is common in children with primary tuberculosis, patients with malnourishment, and immunodeficiencies like HIV and cancer. Even though rare compared to bacterial meningitis, this can lead to high morbidity and mortality if not detected early and treated.[27]
- Traumatic injuries of the spinal cord: It is the commonest, accounting for almost 90% of all spinal cord injuries. It frequently results from road traffic accidents, falls, and sports injuries. They can have devastating effects on the life of a person. Lesions in the lower thoracic region lead to paraplegia, and that in the cervical area leads to quadriplegia.[28]
- Compression: It can be due to intervertebral disc herniation or the vertebras' dislocation leading to compression of the spinal cord. Symptoms due to compression can be paresis to paralysis.
- Hemisection: Traumatic injuries can lead to an incomplete section of a part of the spinal cord. A classical presentation of a hemisection is the Brown-Sequard syndrome. There is ipsilateral motor loss below the section in this syndrome, contralateral loss of pain, and temperature sensations, with no loss of ipsilateral light touch sensations.
- Complete section: It is a condition where there is the absence of sacral sparing with no sensation in the segment of S4-5 or the lack of voluntary contraction of the anal sphincter.[29]
- Vascular injuries of the spinal cord:
- Anterior cord syndrome: When the anterior spinal artery is blocked, it results in ischemia of the anterior two-thirds of the spinal cord's area supplied by this artery. This ischemia is the commonest cause of spinal cord infarction, often occurs due to aortic manipulation or dissection. The commonest site is the mid-thoracic level due to the best supplies from the origin from the vertebral artery and the artery of Ademkiewicz near its lower end. It presents itself as an incomplete motor paralysis below the site of the lesion. Also seen is the sensory loss relative to pain and temperature; this is called anterior cord syndrome.[30] It may be more easily recognized if the whole cord is affected, sparing only the dorsal columns.
- Posterior cord syndrome: It is a syndrome that develops due to ischemia of the posterior spinal artery, affecting the area of the spinal cord supplied by it. It presents itself with an absence of proprioception and vibration sensation, hypotonia, ataxic gait, positive Romberg sign, and the lack of deep tendon reflexes.[31]
- Central cord syndrome: This is a non-vascular injury of the spinal cord, especially seen in a hyperextended neck after a road traffic accident. It is said to be the most common among the incomplete spinal cord injuries. It presents itself with severe sensory and motor function loss in the case of the upper limbs compared with the lower limbs.[32]
- Development anomalies of the spinal cord:
- Spina bifida: It is a developmental anomaly of the vertebrates where the laminae fail to fuse with the spinal process. It is said to be one of the most frequent developmental defects of the neural tube.[33] It is usually seen in the lumbosacral region and is identifiable by a tuft of hairs in this region. No other external visible abnormality is visible.
- Meningocele: In this condition, too, laminae fail to cover the spinal cord leading to protruding of arachnoid and pia mater as a cystic swelling in this region covered by skin.
- Meningomyelocele: This is an extension of meningocele where the cystic swelling will contain a part of the spinal cord with relevant nerves.
- Syringo-myelocele: Further to the above, here we see distension of the central canal.
- Rachischisis: It is a condition where the neural tube fails to close or incompletely closed. This anomaly can develop both in the brain and spinal cord. When it affects the brain, it is called anencephalus, and when the spinal cord, then it is myelocele.
- Herniation: Herniation of the spinal cord is less frequent and usually misdiagnosed for other conditions.[34]
- Malignancy: They can present themselves as ependymomas, astrocytomas, and hemangioblastomas. Others include lipomas, lymphomas, germ cell tumors, gangliogliomas, and germinomas.[35] They can also rarely metastases from different parts of the body like breast, bone, etc.
- Syringomyelia: It is a condition where there is a fluid-filled cavity within the spinal cord. This condition can be due to a disturbance of CSF flow, an intramedullary tumor, or spinal cord tethering.[36]
- Subacute combined degeneration: It is a rare condition arising due to the deficiency of vitamin B12. It leads to neurological complications with demyelination of the lateral and dorsal spinal cord.[37] Similar pathological findings can also be found in patients with copper deficiency, zinc excess, or HIV infection with myelopathy.
- Tabes dorsalis: this is selective pathology affecting only the dorsal columns as a late manifestation of neurosyphilis.
- Transverse myelitis: this is a condition caused by inflammation of the spinal cord. It presents with variable involvement of all functional modalities at and below the site of inflammation. It can occur by itself as an immune-mediated post-infectious problem. It is also commonly involved by an acute relapse of multiple sclerosis. Other inflammatory diseases may also affect the spinal cord, such as Sjogren disease, Behcet's disease, or neuromyelitis optica spectrum disorder.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
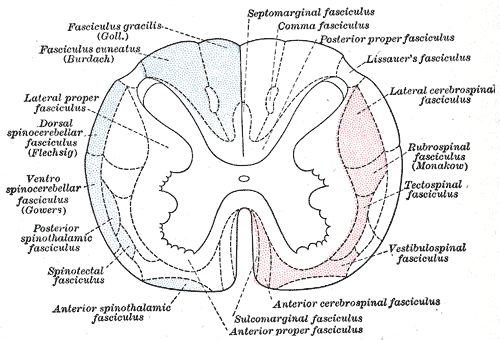
Spinal Cord Fasciculi. The illustration depicts the principal fasciculi of the spinal cord.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
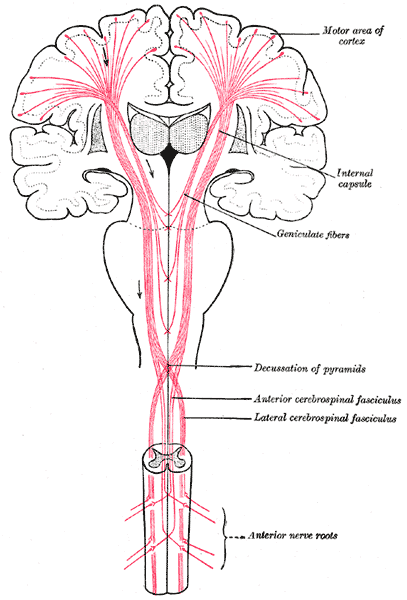
Pathways From the Brain to the Spinal Cord. The figure shows the motor tract, anterior nerve roots, anterior and lateral cerebrospinal fasciculus, decussation of pyramids, geniculate fibers, internal capsule, and motor area of cortex.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)

Types of Spina Bifida. Meningocele is a type of neural tube defect (NTD) that occurs when the meninges, the protective membranes around the spinal cord, protrude through a spinal defect, forming a sac filled with cerebrospinal fluid (CSF). Meningoceles are typically covered by skin and usually present without neurological symptoms.
Centers for Disease Control and Prevention, Public Domain, via Wikimedia Commons
References
Boonpirak N, Apinhasmit W. Length and caudal level of termination of the spinal cord in Thai adults. Acta anatomica. 1994:149(1):74-8 [PubMed PMID: 8184662]
Bhat AR, Kirmani AR, Wani MA, Bhat MH. Incidence, histopathology, and surgical outcome of tumors of spinal cord, nerve roots, meninges, and vertebral column - Data based on single institutional (Sher-i-Kashmir Institute of Medical Sciences) experience. Journal of neurosciences in rural practice. 2016 Jul-Sep:7(3):381-91. doi: 10.4103/0976-3147.181489. Epub [PubMed PMID: 27365955]
Bican O, Minagar A, Pruitt AA. The spinal cord: a review of functional neuroanatomy. Neurologic clinics. 2013 Feb:31(1):1-18. doi: 10.1016/j.ncl.2012.09.009. Epub [PubMed PMID: 23186894]
Ko HY, Park JH, Shin YB, Baek SY. Gross quantitative measurements of spinal cord segments in human. Spinal cord. 2004 Jan:42(1):35-40 [PubMed PMID: 14713942]
Mercadante AA, Tadi P. Neuroanatomy, Gray Matter. StatPearls. 2025 Jan:(): [PubMed PMID: 31990494]
Petkó M, Antal M. Propriospinal pathways in the dorsal horn (laminae I-IV) of the rat lumbar spinal cord. Brain research bulletin. 2012 Oct 1:89(1-2):41-9. doi: 10.1016/j.brainresbull.2012.06.005. Epub 2012 Jun 23 [PubMed PMID: 22732529]
Level 3 (low-level) evidenceKrotov V, Tokhtamysh A, Kopach O, Dromaretsky A, Sheremet Y, Belan P, Voitenko N. Functional Characterization of Lamina X Neurons in ex-Vivo Spinal Cord Preparation. Frontiers in cellular neuroscience. 2017:11():342. doi: 10.3389/fncel.2017.00342. Epub 2017 Nov 1 [PubMed PMID: 29163053]
Cho TA. Spinal cord functional anatomy. Continuum (Minneapolis, Minn.). 2015 Feb:21(1 Spinal Cord Disorders):13-35. doi: 10.1212/01.CON.0000461082.25876.4a. Epub [PubMed PMID: 25651215]
Berkowitz C. DEFINING A DISCOVERY: PRIORITY AND METHODOLOGICAL CONTROVERSY IN EARLY NINETEENTH-CENTURY ANATOMY. Notes and records of the Royal Society of London. 2014 Dec 20:68(4):357-72 [PubMed PMID: 27494015]
Level 3 (low-level) evidenceFrostell A, Hakim R, Thelin EP, Mattsson P, Svensson M. A Review of the Segmental Diameter of the Healthy Human Spinal Cord. Frontiers in neurology. 2016:7():238. doi: 10.3389/fneur.2016.00238. Epub 2016 Dec 23 [PubMed PMID: 28066322]
Darnell D, Gilbert SF. Neuroembryology. Wiley interdisciplinary reviews. Developmental biology. 2017 Jan:6(1):. doi: 10.1002/wdev.215. Epub 2016 Dec 1 [PubMed PMID: 27906497]
Lai HC, Seal RP, Johnson JE. Making sense out of spinal cord somatosensory development. Development (Cambridge, England). 2016 Oct 1:143(19):3434-3448 [PubMed PMID: 27702783]
Ami N, Bernstein M, Boucher F, Rieder M, Parker L, Canadian Paediatric Society, Drug Therapy and Hazardous Substances Committee. Folate and neural tube defects: The role of supplements and food fortification. Paediatrics & child health. 2016 Apr:21(3):145-54 [PubMed PMID: 27398055]
Lara-Ramírez R, Zieger E, Schubert M. Retinoic acid signaling in spinal cord development. The international journal of biochemistry & cell biology. 2013 Jul:45(7):1302-13. doi: 10.1016/j.biocel.2013.04.002. Epub 2013 Apr 8 [PubMed PMID: 23579094]
Level 3 (low-level) evidenceMelton KR, Iulianella A, Trainor PA. Gene expression and regulation of hindbrain and spinal cord development. Frontiers in bioscience : a journal and virtual library. 2004 Jan 1:9():117-38 [PubMed PMID: 14766352]
Level 3 (low-level) evidenceTakahashi T, Takase Y, Yoshino T, Saito D, Tadokoro R, Takahashi Y. Angiogenesis in the developing spinal cord: blood vessel exclusion from neural progenitor region is mediated by VEGF and its antagonists. PloS one. 2015:10(1):e0116119. doi: 10.1371/journal.pone.0116119. Epub 2015 Jan 13 [PubMed PMID: 25585380]
Level 3 (low-level) evidenceSinescu C, Popa F, Grigorean VT, Onose G, Sandu AM, Popescu M, Burnei G, Strambu V, Popa C. Molecular basis of vascular events following spinal cord injury. Journal of medicine and life. 2010 Jul-Sep:3(3):254-61 [PubMed PMID: 20945816]
Statland JM, Barohn RJ, McVey AL, Katz JS, Dimachkie MM. Patterns of Weakness, Classification of Motor Neuron Disease, and Clinical Diagnosis of Sporadic Amyotrophic Lateral Sclerosis. Neurologic clinics. 2015 Nov:33(4):735-48. doi: 10.1016/j.ncl.2015.07.006. Epub 2015 Sep 8 [PubMed PMID: 26515618]
Azam B, Wienecke J, Jensen DB, Azam A, Zhang M. Spinal Cord Hemisection Facilitates Aromatic L-Amino Acid Decarboxylase Cells to Produce Serotonin in the Subchronic but Not the Chronic Phase. Neural plasticity. 2015:2015():549671. doi: 10.1155/2015/549671. Epub 2015 Oct 4 [PubMed PMID: 26504602]
Engelborghs S, Niemantsverdriet E, Struyfs H, Blennow K, Brouns R, Comabella M, Dujmovic I, van der Flier W, Frölich L, Galimberti D, Gnanapavan S, Hemmer B, Hoff E, Hort J, Iacobaeus E, Ingelsson M, Jan de Jong F, Jonsson M, Khalil M, Kuhle J, Lleó A, de Mendonça A, Molinuevo JL, Nagels G, Paquet C, Parnetti L, Roks G, Rosa-Neto P, Scheltens P, Skårsgard C, Stomrud E, Tumani H, Visser PJ, Wallin A, Winblad B, Zetterberg H, Duits F, Teunissen CE. Consensus guidelines for lumbar puncture in patients with neurological diseases. Alzheimer's & dementia (Amsterdam, Netherlands). 2017:8():111-126. doi: 10.1016/j.dadm.2017.04.007. Epub 2017 May 18 [PubMed PMID: 28603768]
Level 3 (low-level) evidenceBos EME, Hollmann MW, Lirk P. Safety and efficacy of epidural analgesia. Current opinion in anaesthesiology. 2017 Dec:30(6):736-742. doi: 10.1097/ACO.0000000000000516. Epub [PubMed PMID: 28938298]
Level 3 (low-level) evidenceElsharkawy H, Sonny A, Chin KJ. Localization of epidural space: A review of available technologies. Journal of anaesthesiology, clinical pharmacology. 2017 Jan-Mar:33(1):16-27. doi: 10.4103/0970-9185.202184. Epub [PubMed PMID: 28413269]
Hogan QH, Mark L. Subdural injection: what's the gold standard? Regional anesthesia and pain medicine. 2009 Jan-Feb:34(1):10-1. doi: 10.1097/AAP.0b013e31819268a0. Epub [PubMed PMID: 19258981]
Boezaart AP, Lucas SD, Elliott CE. Paravertebral block: cervical, thoracic, lumbar, and sacral. Current opinion in anaesthesiology. 2009 Oct:22(5):637-43. doi: 10.1097/ACO.0b013e32832f3277. Epub [PubMed PMID: 19680122]
Level 3 (low-level) evidenceHoffman O, Weber RJ. Pathophysiology and treatment of bacterial meningitis. Therapeutic advances in neurological disorders. 2009 Nov:2(6):1-7. doi: 10.1177/1756285609337975. Epub [PubMed PMID: 21180625]
Level 3 (low-level) evidenceLuo M, Wang W, Zeng Q, Luo Y, Yang H, Yang X. Tuberculous meningitis diagnosis and treatment in adults: A series of 189 suspected cases. Experimental and therapeutic medicine. 2018 Sep:16(3):2770-2776. doi: 10.3892/etm.2018.6496. Epub 2018 Jul 20 [PubMed PMID: 30210618]
Level 3 (low-level) evidenceMarx GE, Chan ED. Tuberculous meningitis: diagnosis and treatment overview. Tuberculosis research and treatment. 2011:2011():798764. doi: 10.1155/2011/798764. Epub 2011 Dec 21 [PubMed PMID: 22567269]
Level 3 (low-level) evidenceAlizadeh A, Dyck SM, Karimi-Abdolrezaee S. Traumatic Spinal Cord Injury: An Overview of Pathophysiology, Models and Acute Injury Mechanisms. Frontiers in neurology. 2019:10():282. doi: 10.3389/fneur.2019.00282. Epub 2019 Mar 22 [PubMed PMID: 30967837]
Level 3 (low-level) evidenceMalhotra M, Bhatoe HS, Sudambrekar SM. Spinal Cord Injuries. Medical journal, Armed Forces India. 2010 Oct:66(4):325-8. doi: 10.1016/S0377-1237(10)80009-7. Epub 2011 Jul 21 [PubMed PMID: 27365735]
Klakeel M, Thompson J, Srinivasan R, McDonald F. Anterior spinal cord syndrome of unknown etiology. Proceedings (Baylor University. Medical Center). 2015 Jan:28(1):85-7 [PubMed PMID: 25552812]
Level 3 (low-level) evidenceSilva Macedo Y, Dos Santos Mota A, Morais Monteiro P, Carvalho AC, Fernandes Diniz B, Gemal Lanzieri P, Carneiro Ramos R, Mocarzel LO, Gismondi RA. Posterior Cord Syndrome and Trace Elements Deficiency as an Uncommon Presentation of Common Variable Immunodeficiency. Case reports in medicine. 2017:2017():9870305. doi: 10.1155/2017/9870305. Epub 2017 Mar 5 [PubMed PMID: 28356913]
Level 3 (low-level) evidenceDivi SN, Schroeder GD, Mangan JJ, Tadley M, Ramey WL, Badhiwala JH, Fehlings MG, Oner FC, Kandziora F, Benneker LM, Vialle EN, Rajasekaran S, Chapman JR, Vaccaro AR. Management of Acute Traumatic Central Cord Syndrome: A Narrative Review. Global spine journal. 2019 May:9(1 Suppl):89S-97S. doi: 10.1177/2192568219830943. Epub 2019 May 8 [PubMed PMID: 31157150]
Level 3 (low-level) evidenceWang C, Zhao JJ, Lu CL, Han XD, An LS, Ma X. Polycomb group proteins are essential for spinal cord development. Frontiers in bioscience (Landmark edition). 2010 Jun 1:15(3):1018-22 [PubMed PMID: 20515739]
Level 3 (low-level) evidenceDarbar A, Krishnamurthy S, Holsapple JW, Hodge CJ Jr. Ventral thoracic spinal cord herniation: frequently misdiagnosed entity. Spine. 2006 Aug 1:31(17):E600-5 [PubMed PMID: 16924199]
Level 3 (low-level) evidenceDavidson CL, Das JM, Mesfin FB. Intramedullary Spinal Cord Tumors. StatPearls. 2025 Jan:(): [PubMed PMID: 28723060]
Klekamp J. How Should Syringomyelia be Defined and Diagnosed? World neurosurgery. 2018 Mar:111():e729-e745. doi: 10.1016/j.wneu.2017.12.156. Epub 2018 Jan 6 [PubMed PMID: 29317358]
Gürsoy AE, Kolukısa M, Babacan-Yıldız G, Celebi A. Subacute Combined Degeneration of the Spinal Cord due to Different Etiologies and Improvement of MRI Findings. Case reports in neurological medicine. 2013:2013():159649. doi: 10.1155/2013/159649. Epub 2013 Mar 27 [PubMed PMID: 23607009]
Level 3 (low-level) evidenceOlakorede I, Bögli SY, Czosnyka Z, Czosnyka M, Smielewski P. CSF production rate, resistance to reabsorption, and intracranial pressure: a systematic review and meta-analysis. Brain communications. 2025:7(1):fcaf044. doi: 10.1093/braincomms/fcaf044. Epub 2025 Jan 30 [PubMed PMID: 39949404]
Level 1 (high-level) evidenceYuan Y, An ZJ, Gao F, Li ZH, Xu WL, Sun Y. Hidden cause of paralysis: tight filum terminale in spinal cord injury without radiographic abnormality. Frontiers in pediatrics. 2024:12():1528007. doi: 10.3389/fped.2024.1528007. Epub 2025 Jan 22 [PubMed PMID: 39911771]
Darwazeh R, Smaili HY, Schuhmann MU. Intraoperative High-Resolution Color-Coded Ultrasound to Identify the Posterior Median Sulcus for Midline Myelotomy in Intramedullary Spinal Cord Surgery. World neurosurgery. 2024 Apr:184():185-187. doi: 10.1016/j.wneu.2024.01.141. Epub 2024 Feb 1 [PubMed PMID: 38309651]
Ma J, Wu H, Ma Z, Wu Z. Bacterial and host factors involved in zoonotic Streptococcal meningitis. Microbes and infection. 2025 Jan:27(1):105335. doi: 10.1016/j.micinf.2024.105335. Epub 2024 Apr 4 [PubMed PMID: 38582147]
Yassen SS, Al-Badri SG, Aldarawsha AN, Elazab MS, Alawad A, Hameedi AD, Hamid AK, Hasan HM, Al-Fatlawi N, Asghar HA. Nasopharyngeal carcinoma with unusual metastatic spread to the spine and meninges: a case report with literature review. Journal of surgical case reports. 2025 Jan:2025(1):rjaf022. doi: 10.1093/jscr/rjaf022. Epub 2025 Jan 23 [PubMed PMID: 39850619]
Level 3 (low-level) evidencevan Staalduinen EK, Massoud TF. Imaging Anatomy of the Cerebrospinal Fluid Spaces. Neuroimaging clinics of North America. 2025 Feb:35(1):1-13. doi: 10.1016/j.nic.2024.08.001. Epub 2024 Sep 23 [PubMed PMID: 39521518]
Wahid ATA, Abdulghani ZM, Al-Fatlawi N, Al-Badri SG. Lumbosacral posterior meningocele in adult patient: a case report. Journal of surgical case reports. 2025 Jan:2025(1):rjaf018. doi: 10.1093/jscr/rjaf018. Epub 2025 Jan 23 [PubMed PMID: 39867984]
Level 3 (low-level) evidenceWalling I, Baumgartner S, Patel M, Crone SA. Electrical stimulation of the sciatic nerve restores inspiratory diaphragm function in mice after spinal cord injury. Frontiers in neural circuits. 2024:18():1480291. doi: 10.3389/fncir.2024.1480291. Epub 2025 Jan 22 [PubMed PMID: 39911754]
Tyagi G, A R P, Bhat DI, Rao MB, Devi BI. Duplication of Ventral Dura as a Cause of Ventral Herniation of Spinal Cord-A Report of Two Cases and Review of the Literature. World neurosurgery. 2019 Jun:126():346-353. doi: 10.1016/j.wneu.2019.02.143. Epub 2019 Mar 6 [PubMed PMID: 30851464]
Level 3 (low-level) evidenceSuleman M, Rabiel H, Vaughan K, Shadrack M, Ndibalema G, Lodhia R, Lodhia J. A Large Thoracolumbosacral Meningomyelocele From Northern Tanzania: A Case Report. Case reports in surgery. 2025:2025():5662565. doi: 10.1155/cris/5662565. Epub 2025 Jan 9 [PubMed PMID: 39835283]
Level 3 (low-level) evidenceGupta A, Khare C, Choudhury S, Dora AK. Iniencephaly with Craniospinal Rachischisis: A Rare Severe Neural Tube Defect. Journal of obstetrics and gynaecology Canada : JOGC = Journal d'obstetrique et gynecologie du Canada : JOGC. 2024 Dec 24:47(2):102752. doi: 10.1016/j.jogc.2024.102752. Epub 2024 Dec 24 [PubMed PMID: 39725026]
O'Reilly SA, Toffol GJ. Adult Arnold-Chiari malformation: a postpartum case presentation. The Journal of the American Osteopathic Association. 1995 Oct:95(10):607-9 [PubMed PMID: 8557551]
Bloch N, Brugger F, Notter J. Tabes dorsalis: a rare presentation of neurosyphilis in Western Europe. BMJ case reports. 2025 Feb 3:18(2):. doi: 10.1136/bcr-2024-262492. Epub 2025 Feb 3 [PubMed PMID: 39900398]
Level 3 (low-level) evidenceKaraja S, Kazkz W. Acute Transverse Myelitis as an Uncommon Presentation of Neurobrucellosis: A Case Report. Clinical case reports. 2025 Jan:13(1):e70060. doi: 10.1002/ccr3.70060. Epub 2025 Jan 2 [PubMed PMID: 39759187]
Level 3 (low-level) evidence